Published online Dec 18, 2021. doi: 10.5312/wjo.v12.i12.983
Peer-review started: March 21, 2021
First decision: May 3, 2021
Revised: May 30, 2021
Accepted: October 27, 2021
Article in press: October 27, 2021
Published online: December 18, 2021
Processing time: 267 Days and 16.6 Hours
Arthroscopic procedures are commonly performed for rotator cuff pathology. Repair of rotator cuff tears is a commonly performed procedure. The intraoperative evaluation of the tear size and pattern contributes to the choice and completion of the technique and the prognosis of the repair.
To compare the arthroscopic and open measurements with the real dimensions of three different patterns of simulated rotator cuff tears of known size using a plastic shoulder model.
We created three sizes and patterns of simulated supraspinatus tears on a plastic shoulder model (small and large U-shaped, oval-shaped). Six orthopaedic surgeons with three levels of experience measured the dimensions of the tears arthroscopically, using a 5 mm probe, repeating the procedure three times, and then using a ruler (open technique). Arthroscopic, open and computerized measurements were compared.
A constant underestimation of specific dimensions of the tears was found when measured with an arthroscope, compared to both the open and computerized measurements (mean differences up to -7.5 ± 5.8 mm, P < 0.001). No differences were observed between the open and computerized measurements (mean difference -0.4 ± 1.6 mm). The accuracy of arthroscopic and open measurements was 90.5% and 98.5%, respectively. When comparing between levels of experience, senior residents reported smaller tear dimensions when compared both to staff surgeons and fellows.
This study suggests that arthroscopic measurements of full-thickness rotator cuff tears constantly underestimate the dimensions of the tears. Development of more precise arthroscopic techniques or tools for the evaluation of the size and type of rotator cuff tears are necessary.
Core Tip: The intraoperative evaluation of the rotator cuff tear size and pattern contributes to the choice of the technique and the prognosis of the repair. The purpose of the study was to determine the accuracy of arthroscopic measurement of the tears’ size comparing them with the open technique. A constant underestimation of specific dimensions of the tears was found when measured with an arthroscopic probe compared to the open measurements.
- Citation: Kitridis D, Alaseirlis D, Malliaropoulos N, Chalidis B, McMahon P, Debski R, Givissis P. Assessing the accuracy of arthroscopic and open measurements of the size of rotator cuff tears: A simulation-based study. World J Orthop 2021; 12(12): 983-990
- URL: https://www.wjgnet.com/2218-5836/full/v12/i12/983.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i12.983
Rotator cuff (RC) tears are the most common tendon injury in adults, often resulting in debilitating symptoms related to both daily and sports activities[1-3]. After the failure of conservative regimens, these patients are usually treated with surgical repair of the tear[1]. Arthroscopy is the preferred surgical option for rotator cuff repair, giving a better intraoperative evaluation of the dynamic shoulder anatomy, preserves the muscle integrity, is associated with lower postoperative morbidity, and provides equal or better results compared to open techniques[4,5].
Repair techniques are based on many factors including patient characteristics, muscle quality, mobility of the tendons, and intraoperative evaluation of the size of the tear[4,6-9]. Therefore, accurate intraoperative measurement of the size of the rotator cuff tear is crucial. Especially in certain techniques such as superior capsule reconstruction, precise measurements of the tears’ dimensions are crucial for the correct sizing of the graft[10-12]. Previous studies have compared magnetic resonance imaging (MRI) measurements with arthroscopic evaluation, and focused on the MRIs ability to detect shoulder pathology in general, and not on the arthroscopic accuracy to evaluate the dimensions of different types of rotator cuff tears[13-15].
Our purpose was to compare the arthroscopic and open measurements with the real dimensions of three different patterns of simulated rotator cuff tears of known size using a plastic shoulder model. We utilized surgeons of three different levels of experience and compared the accuracy between them. The hypothesis of our study was that the size of a rotator cuff tear can be estimated accurately and equally with both arthroscopic and open techniques. To our knowledge, there is currently no research implementing this study design.
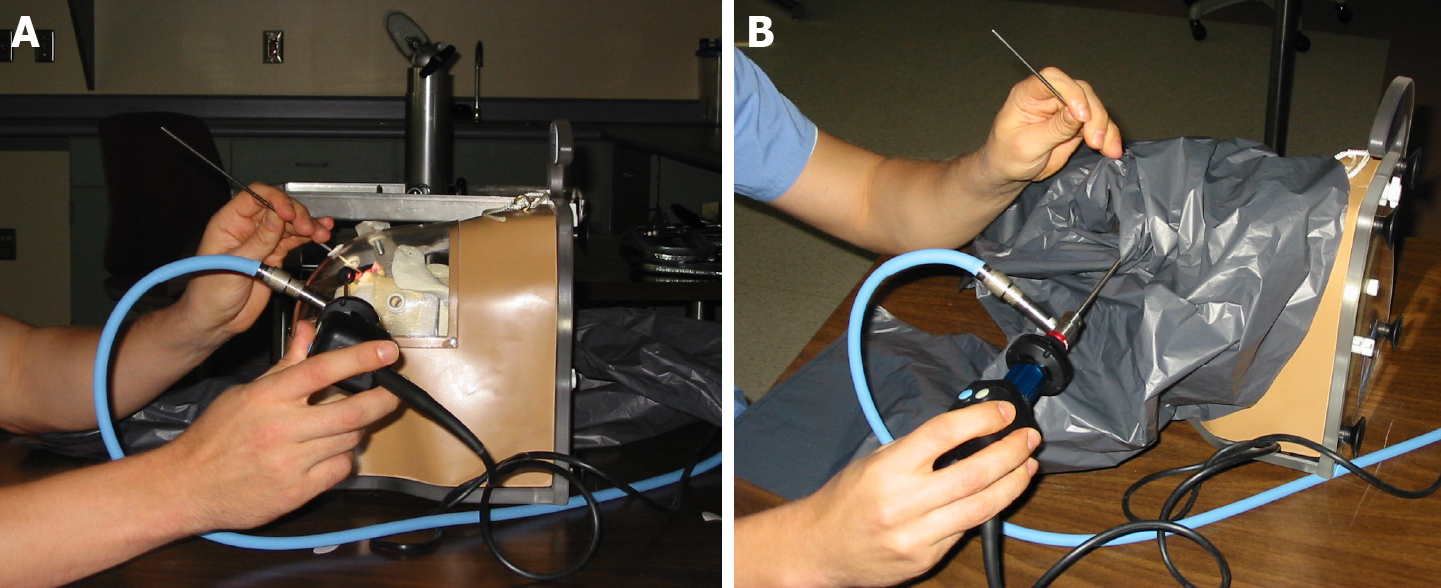
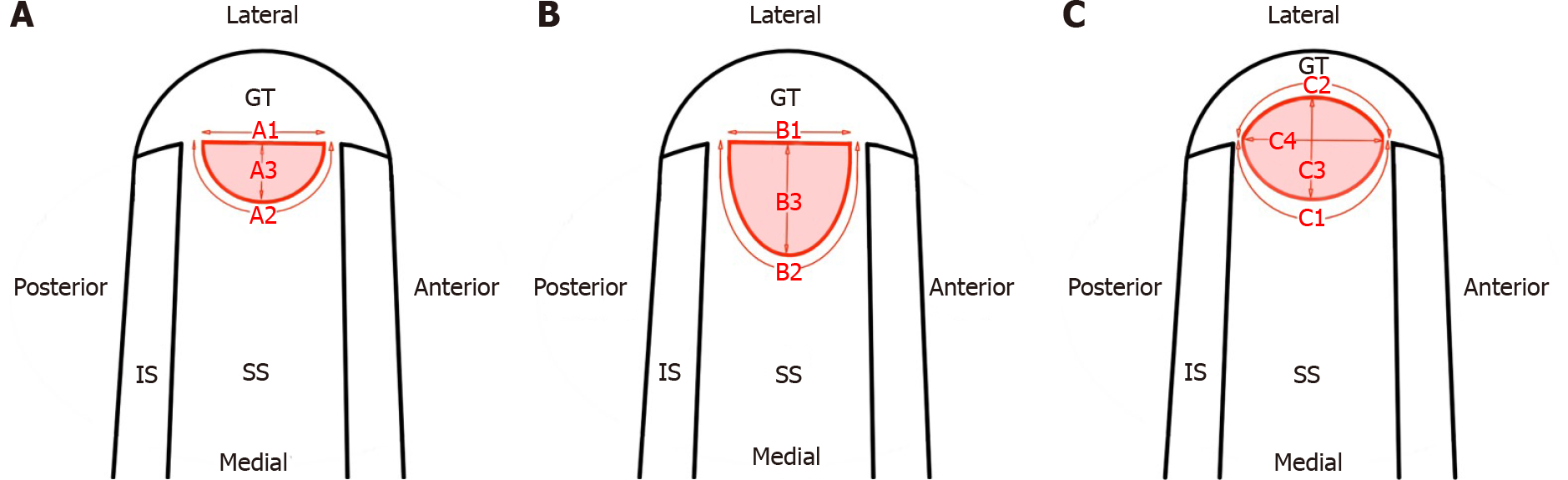
The study took place at the Musculoskeletal Research Center in Pittsburgh, PA, USA. A plastic shoulder model (ALEX shoulder model, Sawbones Inc, Vashon, WA, Figure 1), a 30-degree arthroscope (Linvatec, Largo, FL) through the posterior portal, and a high-definition video system were utilized. Three sizes and patterns of full-thickness rotator cuff tears (a small U-shaped, a larger U-shaped, and a crescent-type, Figure 2) were created using computer software. Dimensions close to the cut-off point of medium and large tears (3 cm) were chosen, according to the DeOrio and Cofield classification system (Table 1)[16]. The simulated tear patterns were printed on paper with adhesive backing and placed in the location of the soft tissue element of the model simulating the supraspinatus tears location. The simulated tears with these computerized measurements had a precision of 0.1 mm.
| ID | Description | Standardized technique | Computerized dimensions (mm) |
| A1 | Basis length | Anterior to posterior | 15.2 |
| A2 | Contour length | Anterior to posterior | 53.5 |
| A3 | Height | Medial to lateral, most distal length | 22.9 |
| B1 | Basis length | Anterior to posterior | 20.3 |
| B2 | Contour length | Anterior to posterior | 31.9 |
| B3 | Height | Medial to lateral, most distal length | 10.2 |
| C1 | Medial contour length | Upper in Figure 2 | 31.9 |
| C2 | Lateral contour length | Lower in Figure 2 | 31.6 |
| C3 | Medial to lateral height | Short height in Figure 2 | 7.6 |
| C4 | Anterior to posterior height | Long height in Figure 2 | 31.0 |
Six orthopaedic surgeons were enrolled in the study and they were blinded to the computerized measurements: two senior residents with fellowship training, two fellows and two senior staff surgeons, all of the Sports Injuries and Shoulder Surgery Department. We asked them to measure the dimensions of the tears arthroscopically, repeating the procedure three times at weekly intervals. Viewing was from the lateral portal and measuring from the lateral portal, constantly. We used a probe calibrated in 5mm intervals and with a 5 mm tip, reflecting the usual practice. During all arthroscopic measurements, the shoulder model was completely covered, so the observers could not have direct vision of the simulated tears (Figure 1B). When all arthroscopic measurements were completed, the shoulder model was uncovered and the plastic cover was also removed. Each surgeon used a surgical ruler for a single measurement to simulate the open technique.
The mean differences between the arthroscopic measurements of the tears compared to the open and computerized measurements were calculated. Comparisons between the overall mean differences between the groups in pairs, using Wilcoxon signed ranks test, with P < 0.016 as the level of significance using the Bonferroni correction were then performed.
Subsequently, the subgroups of the separate dimensions’ measurements were evaluated, using Wilcoxon signed ranks test, with P < 0.05 as the level of significance. Finally, the measurements between the surgeons with the different levels of experience were compared using Wilcoxon signed ranks test, with P < 0.016 as the level of significance using the Bonferroni correction.
The mean value of the three consecutive arthroscopic measurements were used for the analyses that was then performed with the Statistical Package for Social Sciences (SPSS, IBM) software version 24.
A statistically significant underestimation of the dimensions of the tears when measured arthroscopically was observed (P < 0.001) (Table 2). The largest mean differences of the separate measurements were -7.6 ± 5.8 mm in the contour length of the small U-shape tear, -4.5 ± 3.1 mm in the anterior to posterior height of the crescent-type tear, and -3.1 ± 3.1 mm in the contour length of the large U-shaped tear (Table 3). All mean differences were negative (Table 3), showing the constant underestimation of the dimensions. The accuracy of the arthroscopic measurements was 90.5%.
| Groups | mean difference, mm | P1 value |
| Arthroscopic vs computerized | -2.4 ± 3.2 | < 0.001 |
| Arthroscopic vs open | -2 ± 2.6 | < 0.001 |
| Open vs computerized | -0.4 ± 1.6 | 0.014 |
| Dimension | Arthroscopic vs computerized | P1 value | Arthroscopic vs open | P1 value |
| A1 | -0.5 ± 1.2 | 0.92 | -0.3 ± 1.2 | 0.92 |
| A2 | -7.6 ± 5.8 | 0.03 | -3.7 ± 4.9 | 0.12 |
| A3 | -2.1 ± 2.7 | 0.17 | -2.0 ± 2.5 | 0.14 |
| B1 | -2.3 ± 1.9 | 0.03 | -1.9 ± 1.9 | 0.04 |
| B2 | -3.1 ± 3.1 | 0.12 | -3.2 ± 2.3 | 0.04 |
| B3 | -0.7 ± 0.8 | 0.05 | -0.5 ± 0.8 | 0.20 |
| C1 | -1.8 ± 1.6 | 0.05 | -2.5 ± 2.4 | 0.05 |
| C2 | -1.8 ± 1.8 | 0.05 | -2.8 ± 2.1 | 0.03 |
| C3 | -0.1 ± 0.5 | 0.91 | -0.3 ± 0.4 | 0.18 |
| C4 | -4.5 ± 3.1 | 0.03 | -3.1 ± 3.5 | 0.06 |
The overall mean difference between arthroscopic and open measurements confirmed the trend of underestimation of the dimensions, when measured arthroscopically (P < 0.001) (Table 2). The differences between separate measurements were all negative, and some of them were statistically significant (Table 3).
The overall mean difference between open and computerized differences was smaller than between arthroscopic and computerized; -0.4 ± 1.6 mm vs -2.4 ± 3.2 mm. The difference was statistically significant for the corrected level of significance between the groups (P < 0.016), but we considered the mean value of 0.4 mm clinically insignificant for the surgical decision-making. The accuracy of the open measurements was 98.5%.
No significant differences were observed between the senior staff surgeons and the fellows (P = 0.07). On the contrary, the senior residents reported smaller tear dimensions when compared both to the staff surgeons and the fellows (P < 0.001 for both comparisons). Measurements with the open technique were precise among all surgeons (P = 0.96), showing excellent inter-observer reliability.
Surgeons of three different levels of experience were found to constantly underestimate given dimensions of simulated rotator cuff tears with the arthroscopic technique. We utilized three common patterns of rotator tears (a small U-shaped, a larger U-shaped, and a crescent-type). We observed a constant underestimation of the dimensions of the tears when measured with a standard 5 mm probe arthroscopically.
We observed mean differences up to 7.5 mm when comparing the separate measurements of the tears’ dimensions compared to the computerized measurements. The accuracy of the arthroscopic and open measurements was 90.5% and 98.5%, respectively. When comparing the different levels of experience, the senior residents reported smaller tear dimensions when compared both to the staff surgeons and the fellows. It seems that more experienced surgeons tend to be more accurate, although the underestimation is constant to all levels of experience, implicating that the instrumentation used is not suitable for precise measurements. Measurements with an open technique were both accurate and precise.
There are numerous studies considering the intraoperative evaluation of the size of the tear as a factor influencing the choice of the most indicated repair technique and the outcomes of the repair. Park et al[4] reported that large-to-massive tears (> 3 cm) repaired with double-row fixation had significantly improved outcomes in terms of functional outcomes in comparison with those repaired with single-row fixation. Duquin et al[7] analyzed data from 23 studies and found re-tearrates significantly lower for double-row repairs when compared with single-row, especially for tears greater than 5 cm. A summary of meta-analyses reported that six meta-analyses found double row repair to be superior for tears greater than 3 cm, and recent studies also report that larger tears size increases re-tear risk[9,17-19]. Of course, several other factors influence the surgeon’s decision-making of the appropriate surgical technique, including patient characteristics, muscle quality, and mobility of the tendons, as mentioned before[4,6-9]. However, recent research has shown that the rotator cuff tear size at the time of surgery significantly affects supraspinatus integrity in the long-term, thus greatly influences the prognosis of clinical and functional outcomes and patient satisfaction[20]. Moreover, in certain techniques such as superior capsule recons
In the current study, we observed a constant underestimation of the tears’ dimensions with mean differences up to 7.5 mm, when measured arthroscopically. These differences could lead to inappropriate selection of procedures during surgery and affect the patients’ outcomes and prognosis. Our results agree with Bryant et al[21], who reported arthroscopic measurements to have a 12% underestimation of the tear size compared to measurements with an open technique.
Previous studies have compared MRI measurements with the arthroscopic evaluation of rotator cuff tears and reported high sensitivity and specificity both for full and partial thickness tears[13,14]. However, Bryant et al[21] reported magnetic resonance imaging to underestimate the size of rotator cuff tears by 30%. Additionally, Eren et al[14] found significantly larger measurements during surgery when compared with MRI.
In our study, arthroscopic and open techniques were compared but the accuracy and precision were also determined. Combined with the three different levels of experience of the surgeons and the common clinical use of the 5 mm probe, our procedure is very close to daily routine surgical practice.
We used a relatively small sample size. The rationale for the sample selection was that separate measurements for ten specific tear dimensions provided a total of sixty observations in each group (arthroscopic, open, and computerized measurements), which were enough to draw conclusions. Secondly, the measurements were conducted in a plastic simulation shoulder model and not in real patients so that comparisons could be made to computerized measurements.
This study suggests that arthroscopic measurements of full-thickness rotator cuff tears constantly underestimate the dimensions of the tears. This underestimation, especially of specific dimensions (contour length of the small U-shape tear, anterior to posterior height of the crescent-type tear, and contour length of the large U-shaped tear), could lead to false documentation during surgery, unreliable prognostic suggestions, and even postoperative failures. Measurements with an open technique were accurate and precise. These observations raise the need for the development of better arthroscopic tools and techniques for the evaluation of the size of the rotator cuff tears.
Arthroscopic procedures are commonly performed for rotator cuff pathology. The intraoperative evaluation of the tear size and pattern contributes to the choice and completion of the technique and the prognosis of the repair.
The accuracy of common arthroscopic instruments to evaluate the dimensions of different types of rotator cuff tears is not yet evaluated.
The purpose of the current study was to compare the arthroscopic and open measurements with the real dimensions of three different patterns of simulated rotator cuff tears of known size using a plastic shoulder model.
Three sizes and patterns of simulated supraspinatus tears on a plastic shoulder model (small and large U-shaped, oval-shaped) were created. Six orthopaedic surgeons with three levels of experience measured the dimensions of the tears arthroscopically, using a 5 mm probe, repeating the procedure three times, and then using a ruler (open technique). Arthroscopic, open and computerized measurements were compared.
A constant underestimation of specific dimensions of the tears was found when measured with an arthroscope, compared to both the open and computerized measurements. No differences were observed between the open and computerized measurements. The accuracy of arthroscopic and open measurements was 90.5% and 98.5%, respectively. When comparing between levels of experience, senior residents reported smaller tear dimensions when compared both to staff surgeons and fellows.
This study suggests that arthroscopic measurements of full-thickness rotator cuff tears constantly underestimate the dimensions of the tears. This underestimation could lead to false documentation during surgery, unreliable prognostic suggestions, and even postoperative failures.
Development of more precise arthroscopic techniques or tools for the evaluation of the size and type of rotator cuff tears are necessary.
The support of the Musculoskeletal Research Center and the facilities of the Wet Lab in Southside Hospital of UPMC, Pittsburgh are greatly appreciated.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gantaguru A S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Sambandam SN, Khanna V, Gul A, Mounasamy V. Rotator cuff tears: An evidence based approach. World J Orthop. 2015;6:902-918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 102] [Cited by in RCA: 128] [Article Influence: 12.8] [Reference Citation Analysis (6)] |
| 2. | Eljabu W, Klinger HM, von Knoch M. The natural history of rotator cuff tears: a systematic review. Arch Orthop Trauma Surg. 2015;135:1055-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Totlis T, Kitridis D, Tsikopoulos K, Georgoulis A. A computer tablet software can quantify the deviation of scapula medial border from the thoracic wall during clinical assessment of scapula dyskinesis. Knee Surg Sports Traumatol Arthrosc. 2021;29:202-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Park JY, Lhee SH, Choi JH, Park HK, Yu JW, Seo JB. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36:1310-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 160] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 5. | Colegate-Stone T, Allom R, Tavakkolizadeh A, Sinha J. An analysis of outcome of arthroscopic versus mini-open rotator cuff repair using subjective and objective scoring tools. Knee Surg Sports Traumatol Arthrosc. 2009;17:691-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Haviv B, Dolev E, Haber M, Mayo L, Biggs D. Arthroscopic rotator cuff repair: clinical outcome of 607 patients. Knee Surg Sports Traumatol Arthrosc. 2010;18:1707-1711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? Am J Sports Med. 2010;38:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 275] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 8. | Saridakis P, Jones G. Outcomes of single-row and double-row arthroscopic rotator cuff repair: a systematic review. J Bone Joint Surg Am. 2010;92:732-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Spiegl UJ, Euler SA, Millett PJ, Hepp P. Summary of Meta-Analyses Dealing with Single-Row versus Double-Row Repair Techniques for Rotator Cuff Tears. Open Orthop J. 2016;10:330-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Mihata T, Lee TQ, Hasegawa A, Fukunishi K, Kawakami T, Fujisawa Y, Ohue M, Doi M, Neo M. Superior Capsule Reconstruction for Reinforcement of Arthroscopic Rotator Cuff Repair Improves Cuff Integrity. Am J Sports Med. 2019;47:379-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 11. | Mihata T, Lee TQ, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Kinoshita M. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 551] [Cited by in RCA: 613] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 12. | Kitridis D, Yiannakopoulos C, Sinopidis C, Givissis P, Galanis N. Superior Capsular Reconstruction of the Shoulder Using the Long Head of the Biceps Tendon: A Systematic Review of Surgical Techniques and Clinical Outcomes. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Bhatnagar A, Bhonsle S, Mehta S. Correlation between MRI and Arthroscopy in Diagnosis of Shoulder Pathology. J Clin Diagn Res. 2016;10:RC18-RC21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Eren I, Ozben H, Gunerbuyuk C, Koyuncu Ö, Aygün MS, Hatipoglu E, Aydingöz Ü, Demirhan M. Rotator cuff tear characteristics: how comparable are the pre-operative MRI findings with intra-operative measurements following debridement during arthroscopic repair? Int Orthop. 2019;43:1171-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Sharma G, Bhandary S, Khandige G, Kabra U. MR Imaging of Rotator Cuff Tears: Correlation with Arthroscopy. J Clin Diagn Res. 2017;11:TC24-TC27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563-567. [PubMed] |
| 17. | Saccomanno MF, Sircana G, Cazzato G, Donati F, Randelli P, Milano G. Prognostic factors influencing the outcome of rotator cuff repair: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:3809-3819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 117] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 18. | Lambers Heerspink FO, Dorrestijn O, van Raay JJ, Diercks RL. Specific patient-related prognostic factors for rotator cuff repair: a systematic review. J Shoulder Elbow Surg. 2014;23:1073-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 19. | Kukkonen J, Kauko T, Virolainen P, Äärimaa V. The effect of tear size on the treatment outcome of operatively treated rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:567-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Randelli PS, Menon A, Nocerino E, Aliprandi A, Feroldi FM, Mazzoleni MG, Boveri S, Ambrogi F, Cucchi D. Long-term Results of Arthroscopic Rotator Cuff Repair: Initial Tear Size Matters: A Prospective Study on Clinical and Radiological Results at a Minimum Follow-up of 10 Years. Am J Sports Med. 2019;47:2659-2669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 21. | Bryant L, Shnier R, Bryant C, Murrell GA. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elbow Surg. 2002;11:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |