Published online Dec 18, 2021. doi: 10.5312/wjo.v12.i12.1036
Peer-review started: March 18, 2021
First decision: July 18, 2021
Revised: August 1, 2021
Accepted: November 28, 2021
Article in press: November 28, 2021
Published online: December 18, 2021
Processing time: 270 Days and 21.9 Hours
Arthrodesis is the surgical fusion of a diseased joint for the purposes of obtaining pain relief and stability. There have been numerous fixation devices described in literature for foot and ankle arthrodesis, each with their own benefits and drawbacks.
To review the use of intraosseous devices in foot and ankle surgery.
There were 9 papers included in the review (6 clinical and 3 experimental studies) all evaluating arthrodesis in the foot and ankle using the IOFIX device (Extremity Medical™, Parsippany, NJ, United States). Outcome scores, union rates, as well as complications were analysed.
IOFIX appears to be safe and effective in achieving arthrodesis of the 1st metatarsophalangeal, and talonavicular joints with early rehabilitation. In comparison to plate/screw constructs there were fewer soft tissue complications and issues of metalwork prominence. Cadaveric and biomechanical studies on the use of intramedullary fixation for fusion of the tarsometatarsal and ankle joint showed decreased load to failure, cycles to failure and stiffness in comparison to traditional fusion methods using plates and screws, however IOFIX devices produced higher compressive forces at the joint.
We describe the reasons for which this biomechanical behavior of the intraosseous fixation may be favorable, until prospective and comparative studies with larger sample size and longer follow-up confirm the effectiveness and limitations of the method.
Core Tip: Numerous fixation devices have been described in literature for foot and ankle arthrodesis. This review article looked into the use of an intraosseous device IOFIX. Outcome scores, union rates, as well as complications described in 9 related publications were analysed. IOFIX appears to be safe and effective in achieving arthrodesis of the 1st metatarsophalangeal and talonavicular joints with early rehabilitation. However, cadaveric and biomechanical studies on the use in tarsometatarsal and ankle joint showed some concerns for which further clinical trials are required.
- Citation: Benjamin B, Ryan P, Chechelnitskaya Y, Bayam L, Syed T, Drampalos E. Intraosseous device for arthrodesis in foot and ankle surgery: Review of the literature and biomechanical properties. World J Orthop 2021; 12(12): 1036-1044
- URL: https://www.wjgnet.com/2218-5836/full/v12/i12/1036.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i12.1036
Arthrodesis is the surgical fusion of a diseased joint for the purposes of obtaining pain relief and stability. The fundamental principles of arthrodesis include (1) Adequate exposure and preparation of joint surfaces; (2) Coaptation of the surfaces; and (3) Rigid fixation of the surfaces until union[1,2].
Compression, rigidity and co-aptation are interrelated. With perfect co-aptation and compression, significant rigidity can be achieved. Compression neutralises the shear and bending forces. This in turn prevents separation of the surfaces. When compression is applied across an arthrodesis, the pressure is initially concentrated on the uneven areas of the cut surfaces. The resulting osteoclastic resorption brings the surfaces into closer co-aptation. Under the influence of moderate dynamic com
In foot and ankle surgery, common joints where arthrodesis is performed include ankle, subtalar (ST), talonavicular (TN), calcaneocuboid (CC), tarsometatarsal (TMT) and the 1st metatarsophalangeal (MTP) joint. There have been numerous fixation devices such as compression screws, staples, locking and nonlocking plates, as well as combined fixation of screws, staples, and/or plates described in literature each with their own benefits and drawbacks.
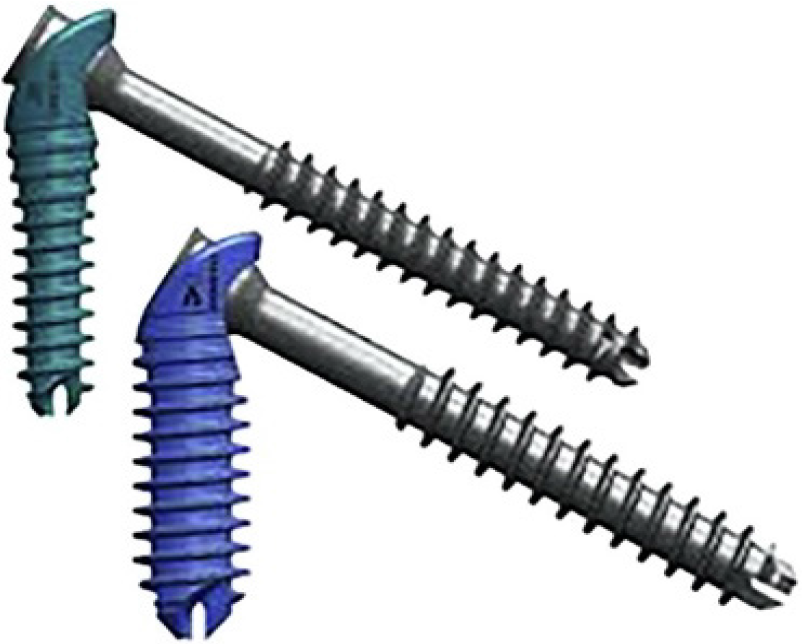
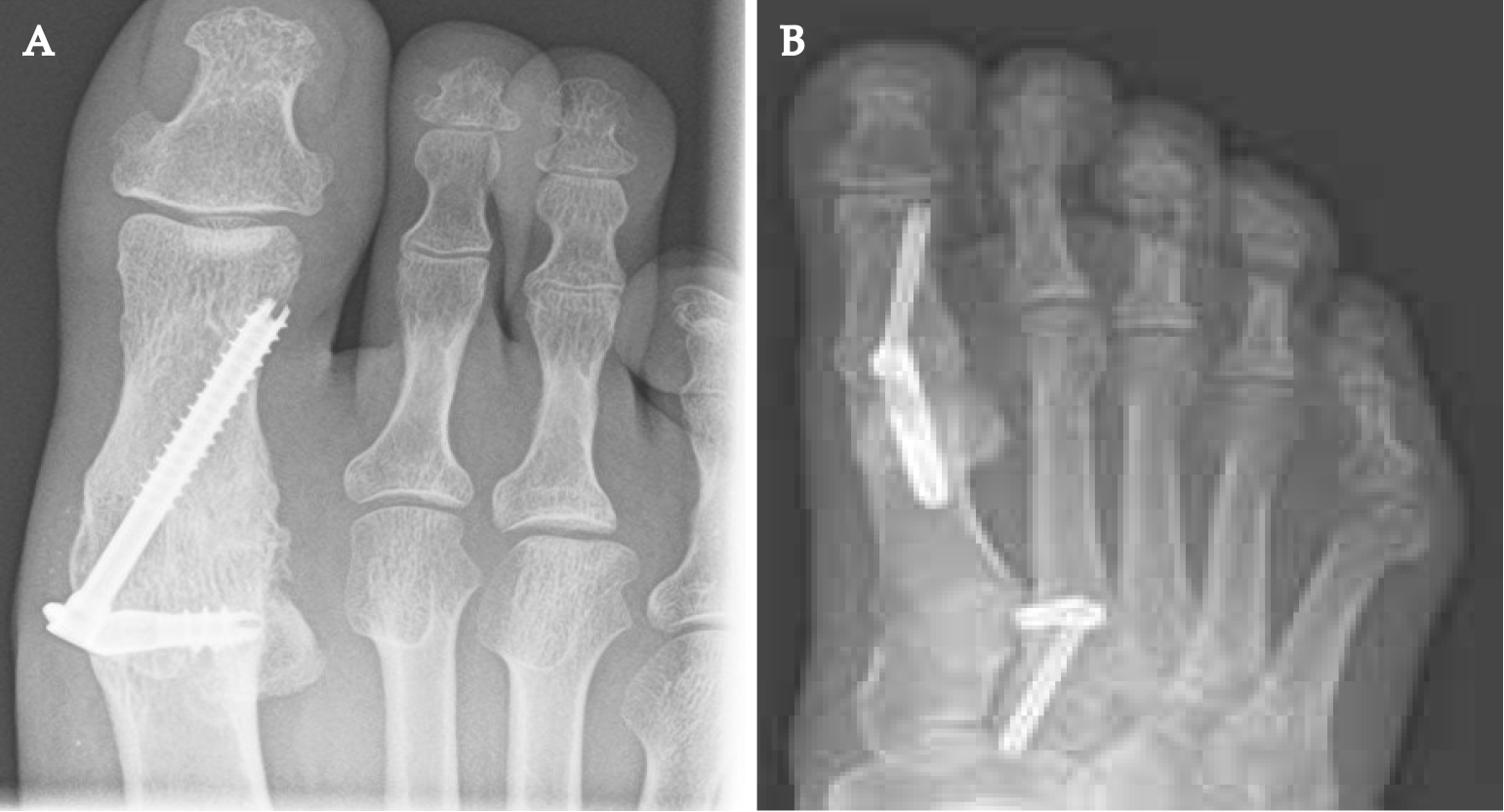
The IOFIX (an Intra-Osseous FIXation device, Extremity medical, New Jersey, United States) is a fixed angle device consisting of a “Post” and a lag screw. The “Post” is inserted parallel to the joint surface. The “post” has an eyelet in its head through which a lag screw can be passed across the arthrodesis site at a 60° angle (Figures 1 and 2A). The lag screw gets engaged in the morse taper of the eyelet resulting in a more uniform compression across the fusion site. Since the entire construct is embedded in the bone there is less risk of soft tissue irritation and prominence of metalwork. Furthermore, in comparison with a plate and screw construct there is less soft tissue damage and periosteal damage needed to prepare the articular surfaces and apply the implant.
There have been a number of publications in literature regarding the use of the Intraosseous devices in different joint arthrodesis[5-12]. The aim of this article is to review these publications, assess the overall efficacy of the device across the various joints that are commonly arthrodesed in foot and ankle surgery and correlate the results with its biomechanical properties.
A literature search was done in several databases; PubMed Central, Cochrane Central and MEDLINE. The search was restricted to articles in English language. Only fully published studies with details of the use of intra osseous devices were included. Key words used in search were “Intra osseous fixation”, “foot”, “ankle” and “arthrodesis”.
Data extracted included study design, selection criteria, population demographics, type of intervention, initial and final outcome scores, union rates, as well as complications if any. Results of all the included studies were described in a table format. Key outcomes assessed were union rates, patient reported outcome scores and complications.
There have been 9 publications on this topic[5-13] (Table 1). Six of these were clinical studies (5 on 1st MTP joint and 1 on TN joint). Two were cadaveric (1 each on ankle and TMT joint) and one was a synthetic bone study (TMT joint). All the clinical studies had patient reported outcome scores as well as arthrodesis union rates reported.
| No | Ref. | Joint arthrodesed | Number of joints | Follow up (mo) | Outcome |
| 1 | Segal et al[5], 2020 | 1st MTP joint | 30 | 36 | Mean postop AOFAS score: 80.5 |
| 2 | Patel et al[6], 2019 | 1st MTP joint | 54 | 12 | Mean MOXFQ improved from 46.4 to 18.4 |
| 3 | Singhal et al[7], 2018 | 1st MTP joint | 21 | 28 | Mean MOXFQ improved from 49.7 to 17.9 |
| 4 | Drampalos et al[8], 2017 | 1st MTP joint | 12 | 15 | Mean AOFAS score improved from 29.4 to 73.3 |
| 5 | Drampalos et al[9], 2016 | 1st MTP joint | 23 | 19 | Mean AOFAS score improved from 29 to 75.4 |
| 6 | Shymon et al[10], 2016 | Talonavicular | 12 | 12 | VAS pain level decreased from 7.3 to 2.1 |
| 7 | Parker et al[11], 2014 | Tibio talar joint | 10 cadaveric | Higher forces within the arthrodesis (3.95 kg vs 2.35 kg) in IOFIX | |
| 8 | Burchard et al[12], 2018 | 1st MTP joint | 9 synthetic | Lower load to failure and less stiffness in IOFIX | |
| 9 | Roth et al[13], 2014 | 1st MTP joint | 7 cadaveric | Lesser cycles to failure in IOFIX |
Radiographic union of the fusion site was defined by observing complete callus or trabeculation across 3 cortices. Position of fusion of the 1st MTP joint was assessed by analysing the intermetatarsal angle, hallux valgus angle (HVA), and 1st MTP joint dorsiflexion angle (DA) using weightbearing anteroposterior and lateral views of the foot.
Segal et al[5] from Tel Aviv, Israel, conducted a retrospective review on union rates following the use of IOFIX. Standard operative technique was used. The study included 30 cases with an average follow up of 36.2 ± 12.31 mo. Plain radiographic studies were taken at 6 wk, 3–6-12 mo, and at 24 mo when applicable. Clinical union was when the patients could fully bear weight on their feet without pain, and had no pain when applying external force on the 1st MTP joint. Radiographic union was obtained in 28 (93.33%) patients. None of the patients requested removal of hardware due to prominence. The mean postoperative AOFAS score[14,15] was 80.5 ± 10.87. One patient had asymptomatic nonunion. One patient underwent repeat surgery for symptomatic nonunion but still did not go on to union. There were no cases of loss of position or implant breakage.
Patel et al[6] from London, United Kingdom, analysed 54 feet for clinical and radiological union with a minimum follow up of 1 year. Patients were allowed to fully bear weight in a rigid-soled shoe with 2 crutches to assist walking immediately after surgery. Arthrodesis was achieved in 52 (96.3%) feet at a mean of 61 ± 16 d. Nonunion was observed in 2 (3.7%) feet with one person opting for repeat surgery using a dorsal plate. There were 2 (3.7%) superficial wound infections that responded to oral antibiotics without further complications. Removal of implant due to metalware impingement on soft tissues was performed in 3 (5.6%) feet after union. The mean Manchester-Oxford Foot Questionnaire score[16] improved from 46.4 ± 13.3 to 18.4 ± 9.4 (P < 0.001) at latest follow-up. There were no cases of loss of position or implant breakage.
Singhal et al[7] from Liverpool, United Kingdom, did a retrospective review of 21 patients with a mean follow up of 28 mo. Postoperatively patients were allowed to heel weight bear in a firm soled sandal with the aid of crutches. Complete fusion of the 1st MTP joint was achieved in twenty (95%) patients. One patient had a non-union and another patient developed a delayed union. The non-union was revised 14 mo after the initial procedure with a locking plate and bone graft and this has gone on to unite. The mean preoperative MOXFQ score improved from 49.7 (95% confidence interval: 46-52) to 17.9 (95% confidence interval: 12-22), P < 0.05.
Drampalos et al[8] from Manchester, United Kingdom, published their results on twelve consecutive patients operated with this method. Postoperatively, a C-slab was applied, followed by immediate heel weight bearing in stiff soled shoe. After 6–12 wk, the patients were allowed unrestricted activities provided a satisfactory progression of fusion was evident on radiographs. The mean follow up was 15 mo. Fusion of the MTP joint was obtained in 11 toes (91%). The AOFAS score improved significantly from a preoperative mean of 29.4 (range 10–54), to a postoperative mean of 73.3 (range 59–90) (P < 0.0001). The patient with nonunion had only minor improvement from the procedure with persisting symptoms but did not want a revision surgery. There was one patient diagnosed with transfer metatarsalgia who had a malalignment with a HVA of 4°. This patient had a poor improvement of the AOFAS score (from 30 preoperatively to 59 after the operation) but was still satisfied with the result.
In another series, Drampalos et al[9] from Manchester, United Kingdom, reviewed the results of arthrodesis of the 1st MTP joint in 23 patients using the IOFIX or HALUX (Extremity Medical, Parsippany NJ, a similar intramedullary device with an anchored post and a lag screw) (Figure 2B). Patients were followed up for a mean of 19 mo. The mean AOFAS score improved from 29 to 75.4 (P < 0.0001) and the mean VAS for pain improved from 8.1 to 2.4 (P < 0.0001). Twenty (86%) of the patients were satisfied with the outcome. Twenty-one (91%) of the patients achieved arthrodesis. 2 patients underwent revision surgery for failed fusion (HALUX) and infected non-union (IOFIX).
Shymon et al[10] from California, United States, investigated postoperative bony union and functional outcomes of 12 consecutive patients who underwent TN arthrodesis with the IOFIX device. Surgical indications included posttraumatic arthritis, rheumatoid arthritis, and idiopathic arthritis. Post operatively, a short leg, well-padded splint was applied. Patients were advised to be non–weight bearing. At 1 wk, they were placed in a controlled ankle movement boot and allowed to weight bear if pain allowed it. Patients were followed up for a minimum of 1 year. The VAS pain level decreased from 7.3 ± 0.9 preoperatively to 2.1 ± 0.7 postoperatively (P < 0.001) and the SF-12 physical component improved from 27.9 ± 4.2 preoperatively to 42.2 ± 3.5 postoperatively (P < 0.001). Radiographic union was achieved in all the 12 patients at 9.6 ± 0.4 wk. Three patients had a superficial wound infection that resolved with oral antibiotics for 10 d. On average, patients were able to weight bear by 3.5 wk (range 2.2-5.5 wk)
Parker et al[11] from London, United Kingdom, conducted a cadaveric experiment on 10 ankles where they compared the magnitude and distribution of force created across an ankle arthrodesis between IOFIX and traditional AO 6.5 mm cancellous partially-threaded bone screws (Figure 3). The soft tissues from the ankles were removed and the articular surfaces of the distal tibia and talus were prepared with a 2.5 cm wide saw to create uniformly flat arthrodesis cuts. The 10 ankles received both treatments in a randomized fashion in order to allow direct comparisons between repeated measurements. Compression forces were measured using a Tekscan/Iscan (Tekscan Inc. South Boston MA, United States) pressure transducer calibrated to display force in kilograms (kg) and contact area in cm2 and inserted into the arthrodesis.
The IOFIX created significantly higher median average forces within the arthrodesis (3.95 kg compared with 2.35 kg, P ≤ 0.01). The IOFIX also created a more uniform pressure across the arthrodesis as well as a higher median average uniform contact area (3.41 cm2 vs 2.42 cm2, P ≤ 0.03).
Burchard et al[12] from Witten, Germany, conducted an experimental study using 9 synthetic bones to study the use of a medial locking plate (Double bridge plate® (Konigsee Implantate GmbH, Allendorf, Germany), a plantar locking plate (PEDUS L Plantar Lapidus Plate® (Axomed GmbH, Freiburg, Germany), or an intraosseous locking device [IOFIX (Extremity Medicals, Parsippany, United States)] in 1st TMT joint arthrodesis. They looked into the difference in the initial compression of the osteosynthesis as well as loss of stability and load to failure. The highest initial compression force was provided by the IOFIX implant (131 ± 55 N), followed by the medial locking plate (87 ± 51 N) and the plantar plate (3 ± 1 N). The stiffness provided by the plantar plate was superior compared to both of the other fixation methods (vs medial plate P ≤ 0.000, vs IOFIX P ≤ 0.000). Load to failure was in the following order: (1) IOFIX (173 ± 8 N); (2) Medial plate (324 ± 24 N); and (3) Plantar plate (377 ± 41 N).
Roth et al[13] from Mainz, Germany, performed a study on 7 pairs of freshly frozen cadaveric feet to compare the intra- medullary implant IOFIX (Extremity Medical TM, Parsippany, NJ, United States) with plantar locking plate (Wright Medical Technology, Inc, Arlington, TX, United States) in osteosynthesis of the 1st TMT joint. Cycles until failure, failure load, displacement, and plantar gapping were recorded. On average the plates failed after 7517 cycles and a maxi- mum load of 167.1 N while the screw and post implants failed on average after 2946 cycles and a maximum load of 68.6 N. After 8167 cycles 50% of the plates had failed while the same failure rate was observed after 2269 cycles in the IOFIX group. Initial and final stiffness were all higher on average in the plate-treated group than in the screw and post group.
The majority of studies on the use of intraosseus fixation devices for arthrodesis involve the first MTP joint and it is considered that the type of implant used to stabilise the fusion site influences the outcome. In general literature the union rates of primary first MTP joint arthrodesis has been excellent and reported to be up to 100%[17]. Patient's satisfaction after MTP arthrodesis varies from 78% to 93%[18-20]. Larger implants have a higher rate of successful fusion but they also have higher implant removal rate, up to 30%, due to nonunion, malalignment, pain and hardware impingement of the soft tissues[21-23]. The intraosseous advantages of IOFIX include the facts that it is of “low profile” and provides uniform compression with a stable fixation[24]. In the series of studies reviewed, IOFIX appears to be safe and effective in achieving arthrodesis of the first MTPJ and immediate weightbearing can be allowed. Concerns have been raised about the cost of the IOFIX implant[5]. However, with the reduced requirement for further surgery and excellent union rates, the pros could outweigh the cons.
The TN arthrodesis study[10] suggests that the IOFIX device improves patient outcomes with a quick return to weight bearing. Historically, post-TN arthrodesis nonunion has been reported in up to 37% of cases of rheumatoid arthritis[25]. In this study, that included 3 patients with rheumatoid arthritis, there were no cases of nonunion.
The experimental study on ankle arthrodesis[11] showed that the IOFIX exhibited a more uniform contact area. The AO lag-screw and washer tended to concentrate stress nearest where it was inserted. Bone resorption in areas of high peak contact stress within an arthrodesis may lead to progressive loss of bone interdigitation, gapping and non-union at the interface. Therefore, theoretically, IOFIX has an advantage over the lag screw fixation methods. But there were no clinical studies available.
In the TMT studies[12,13], IOFIX demonstrated the highest initial compression force of the three tested implants but the load to failure, cycles to failure and stiffness were significantly lesser. The plantar locking plate showed the best overall stability and stiffer construct during cyclic weight-bearing simulation. This does not necessarily mean higher union rates when a plate is being used. In case of a fracture or a fusion there is a range of instability/rigidity which may be tolerated in different biomechanical scenarios. A fusion may be achieved despite instability (or decreased stiffness) while minimal instability may be detrimental in rigidly fixed constructs with small gaps.
The Perren’s theory of strain describes the minimum and maximum degrees of rigidity which will be tolerated leading to primary bone healing and induction of callus formation[26]. The decisive factor for tissue differentiation is deformation or strain of the repair tissue and not rigidity/mobility. While tissue strain relates with mobility, it depends even more so on the distance between the movement of the opposing surfaces. The biological parameters of damage to the blood supply and bone necrosis emphasize the importance of avoiding extensive periosteal stripping and contact of the implant with bone. A balance between rigidity, compression and co-aptation is probably more important. Primary union is seen when rigid stabilisation with perfect co-aptation and minimal interfragmentary motion is applied. Osteoclasts make up the head of a “cutting cone”, followed by capillaries and then osteoblasts which lay down the osteoid to fill the “cutting cone”. Small gaps are filled by woven bone which later remodels to lamellar bone. There is no external callus and bone strength is not restored for many months. However, in less rigidly fixed fractures, external callus is seen and bone is remodelled quicker in accordance with Wolff’s law and Perrens’s strain theory[3]. The intraosseous device offers an advantage in this regard. Further research and clinical data is necessary to study the efficacy of IOFIX in TMT fusions. The senior authors of our team have used the IOFIX device for 1st TMT joint fusions with encouraging results and is in the process of publishing them.
The limitation of this review is the few papers available on the device. There were also no clinical papers on the use of intraosseous devices in joints other than the 1st MTPJ and a single article on the talonavicular joint.
The intraosseous fixation device IOFIX reviewed in our study appears to be a safe and effective device to achieve arthrodesis with the advantages of early weight bearing. They provide good patient reported outcomes satisfaction and bone union as well as avoiding prominent hardware complications and soft tissue irritation. However, further prospective and comparative studies with larger sample size and longer follow-up are needed to confirm these findings.
Numerous fixation devices have been described in literature for foot and ankle arthrodesis. Each of these devices have their own benefits and drawbacks
This review article looked into the use of an intraosseous device IOFIX. Since the entire construct of IOFIX is embedded in the bone, there is less risk of soft tissue irritation and prominence of metalwork.
Outcome scores, union rates, as well as complications associated with the use of IOFIX was looked into.
Fully published studies with details of the use of intra osseous devices were included in the study. These were identified by a search through available English literature. Nine related publications were identified and analysed.
In comparison to plate/screw constructs there were fewer soft tissue complications and issues of metalwork prominence. It also provided adequate compression across the arthrodesis site.
IOFIX appears to be safe and effective in achieving arthrodesis of the 1st metatarsophalangeal and talonavicular joints with early rehabilitation. However, cadaveric and biomechanical studies on the use in tarsometatarsal and ankle joint showed some concerns with decreased load to failure and cycles to failure.
Further clinical trials are required. Prospective and comparative studies with larger sample size and longer follow-up could confirm the effectiveness and limitations of the method.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Mazzotti A, Vitiello R S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Charnley JC. Positive pressure in arthrodesis of the knee joint. J Bone Joint Surg Br. 1948;30B:478-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 58] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Cunningham JL, Richardson JB, Soriano RM, Kenwright J. A mechanical assessment of applied compression and healing in knee arthrodesis. Clin Orthop Relat Res. 1989;256-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Perren SM. The biomechanics and biology of internal fixation using plates and nails. Orthopedics. 1989;12:21-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Kenwright J, Goodship AE. Controlled mechanical stimulation in the treatment of tibial fractures. Clin Orthop Relat Res. 1989;36-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 69] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Segal D, Ohana N, Nyska M, Palmanovich E. Does the IOFix implant improve union rates? BMC Musculoskelet Disord. 2020;21:654. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Patel S, Garg P, Fazal MA, Ray PS. First Metatarsophalangeal Joint Arthrodesis Using an Intraosseous Post and Lag Screw With Immediate Bearing of Weight. J Foot Ankle Surg. 2019;58:1091-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Singhal R, Kwaees T, Mohamed M, Argyropoulos M, Amarasinghe P, Toh EM. Result of IOFIX (Intra Osseous FIXation) device for first metatarsophalangeal joint arthrodesis: A single surgeon's series. Foot Ankle Surg. 2018;24:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Drampalos E, Vun SH, Bayam L, Fayyaz I. Early results of an intraosseous device for arthrodesis of the hallux metatarsophalangeal joint. Indian J Orthop. 2017;51:299-303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Drampalos E, Vun SH, Fayyaz I. Intramedullary and intra-osseous arthrodesis of the hallux metatarsophalangeal joint. J Orthop Surg (Hong Kong). 2016;24:358-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Shymon SJ, Moss L, Harris TG. Case Series Using a Novel Implant and Accelerated Rehabilitation for Patients Undergoing an Isolated Talonavicular Arthrodesis. Foot Ankle Spec. 2016;9:227-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Parker L, Ray P, Grechenig S, Grechenig W. Does the IOFIX improve compression in ankle fusion? Foot Ankle Surg. 2014;20:258-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Burchard R, Massa R, Soost C, Richter W, Dietrich G, Ohrndorf A, Christ HJ, Fritzen CP, Graw JA, Schmitt J. Biomechanics of common fixation devices for first tarsometatarsal joint fusion-a comparative study with synthetic bones. J Orthop Surg Res. 2018;13:176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Roth KE, Peters J, Schmidtmann I, Maus U, Stephan D, Augat P. Intraosseous fixation compared to plantar plate fixation for first metatarsocuneiform arthrodesis: a cadaveric biomechanical analysis. Foot Ankle Int. 2014;35:1209-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Extremity Medical. IOFiX Plus intraosseous fixation—Surgical technique. [cited 8 February 2021]. Available from: http://www.extremitymedical.com/Lower-extremity/. |
| 15. | Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3199] [Cited by in RCA: 3113] [Article Influence: 100.4] [Reference Citation Analysis (0)] |
| 16. | Morley D, Jenkinson C, Doll H, Lavis G, Sharp R, Cooke P, Dawson J. The Manchester-Oxford Foot Questionnaire (MOXFQ): Development and validation of a summary index score. Bone Joint Res. 2013;2:66-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 158] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 17. | Flavin R, Stephens MM. Arthrodesis of the first metatarsophalangeal joint using a dorsal titanium contoured plate. Foot Ankle Int. 2004;25:783-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Parker L, Singh D. The principles of foot and ankle arthrodesis. Ortho Trau. 2009;23:385-394. [DOI] [Full Text] |
| 19. | Mann RA, Oates JC. Arthrodesis of the first metatarsophalangeal joint. Foot Ankle. 1980;1:159-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 141] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Maher AJ, Metcalfe SA. First MTP joint arthrodesis for the treatment of hallux rigidus: results of 29 consecutive cases using the foot health status questionnaire validated measurement tool. Foot (Edinb). 2008;18:123-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Wassink S, van den Oever M. Arthrodesis of the first metatarsophalangeal joint using a single screw: retrospective analysis of 109 feet. J Foot Ankle Surg. 2009;48:653-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Wanivenhaus F, Espinosa N, Tscholl PM, Krause F, Wirth SH. Quality of Early Union After First Metatarsophalangeal Joint Arthrodesis. J Foot Ankle Surg. 2017;56:50-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Riggs SA Jr, Johnson EW Jr. McKeever arthrodesis for the painful hallux. Foot Ankle. 1983;3:248-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Knutsen AR, Fleming JF, Ebramzadeh E, Ho NC, Warganich T, Harris TG, Sangiorgio SN. Biomechanical Comparison of Fixation Devices for First Metatarsocuneiform Joint Arthrodesis. Foot Ankle Spec. 2017;10:322-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Ljung P, Kaij J, Knutson K, Pettersson H, Rydholm U. Talonavicular arthrodesis in the rheumatoid foot. Foot Ankle. 1992;13:313-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Perren SM. [Optimizing the degree of fixation stability based on the strain theory]. Orthopade. 2010;39:132-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |