Published online Nov 18, 2021. doi: 10.5312/wjo.v12.i11.920
Peer-review started: April 21, 2021
First decision: July 28, 2021
Revised: August 6, 2021
Accepted: October 8, 2021
Article in press: October 8, 2021
Published online: November 18, 2021
Processing time: 209 Days and 3.5 Hours
Infection at the pin tract is a frequent and feared complication of external fixators (EF). The type of pin material and coatings have been regarded as possibly influencing infection rates. Over the last 20 years, few prospective clinical studies and systematic reviews addressed the role of coated pins on the rate of pin site infection in human clinical studies.
To assess the EF literature over the past 20 years on the clinical benefits of pins manufactured from varied materials and coating systems and their possible role in pin tract infection rates.
We performed a systematic review according to the PRISMA and PICOS guidelines using four scientific platforms: PubMed, LiLacs, SciELO, and Cochrane. We searched the literature for related publications over the past 20 years.
A literature search yielded 29 articles, among which seven met the inclusion criteria. These studies compared stainless-steel pins and pins coated with hydroxyapatite (HA), titanium and silver. The pin tract infection definitions were arbitrary and not standardized among studies. Most studies included a low number of patients in the analysis and used a short follow-up time. Three meta-analyses were carried out, comparing stainless steel vs silver pins, stainless steel vs HA-coated pins, and titanium vs HA-coated pins. None of this analysis resulted in statistically significant differences in pin tract infection rates.
Currently, no clinical evidence supports the advantage of EF pins manufactured with materials other than stainless steel or coated over uncoated pins in reducing the rates of pin tract infections. A standardized definition of pin tract infection in external fixation is still lacking.
Core Tip: There is no consensus in the literature that different materials or pin coatings of external fixators can interfere with the infection rates. This is the first manuscript that evaluates related publications over the last 20 years and develops a meta-analysis evaluating three different types of metallic coatings.
- Citation: Stoffel C, Eltz B, Salles MJ. Role of coatings and materials of external fixation pins on the rates of pin tract infection: A systematic review and meta-analysis. World J Orthop 2021; 12(11): 920-930
- URL: https://www.wjgnet.com/2218-5836/full/v12/i11/920.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i11.920
External fixators (EF) are used for bone stabilization using minimally invasive percutaneous insertion of pins, thin and olive wires, interconnected by threaded shafts, bars, and metal rings. These devices provide robust support in the management of fractures and cases of long bone nonunions, malunions, infections, and serious limb malalignment deformities[1]. At the same time, pins are a pathway of contact between the external environment and the skin, subcutaneous tissue, muscle, and bone. Consequently, infection is one of the main complications[1,2]. When infection is superficial, clinical treatment entails local measures and orally administered antibiotics for control. Cases where the infection progresses from the skin and soft tissues into bones and consequently results in pin loosening usually require pin removal or replacement and long-term intravenous antibiotic therapy for chronic osteomyelitis, increasing the cost and complexity of treatment[3].
Infections associated with implants are usually caused by microorganisms that grow in biofilms attached to the implant surface, which is also the case with pin tract infections. A biofilm is a well-controlled and protected environment favoring sessile microorganisms to develop a multi-factorial tolerance to antibiotics and host defenses. This tolerance has been attributed to restricted penetration of the antibiotics, restricted growth at low-oxygen tension, expression of biofilm-specific genes and the presence of non-dividing microorganisms[4]. The formation of biofilms is a major contributor to the clinical challenges encountered in treating pin tract infections.
Therefore, previous studies have assessed different measures to control infectious pin complications, from pin base local care protocols to nonmetallic (ceramic) manufactured pins and coating systems to avoid biofilm formation[5-8]. Clinical benefits regarding infection and loosening of coated vs. uncoated pins have yet to be well defined[9,10]. Indeed, many published articles failed to reach definitive conclusions regarding the impact of different pin materials and coatings on the reduction of pin tract infections[11]. In a 2005 clinical review on hydroxyapatite-coated pins, Moroni et al[12] concluded that this type of coating system could reduce the rate of post-operative complications, including infections. Nevertheless, current research assessing the real clinical benefits of tapered pins coated with hydroxyapatite is still lacking. A 2010 systematic review by Saithna et al[11] that included only four randomized controlled trials failed to show a clear clinical benefit of using hydro
A few types of pin materials have been assessed in previous published clinical studies, including ceramic and metallic (stainless steel and titanium), and also coatings such as hydroxyapatite (HA), HA plus fibroblast growth factor 2 (FGF-2), silver coating and iodine-coated systems[6,11,13-15]. Even though HA coating is one of the most studied coating systems, whether this and other products can effectively reduce the number of infections remains unclear[11,15-18]. Indeed, over the last 20 years, few prospective clinical studies and only two systematic reviews addressed the role of coated pins on the rate of pin site infection in human clinical studies. Moreover, only a hydroxyapatite coating system was assessed in these published reviews. Considering the advances in materials and surfaces in recent years, we aimed at assessing the clinical benefits and rates of infectious complications of EF pins manufactured from varied materials with different coating systems. This systematic review and meta-analysis compiled comparative data on superficial and deep infectious complications found in different types of external fixation pin materials and coatings in human clinical studies.
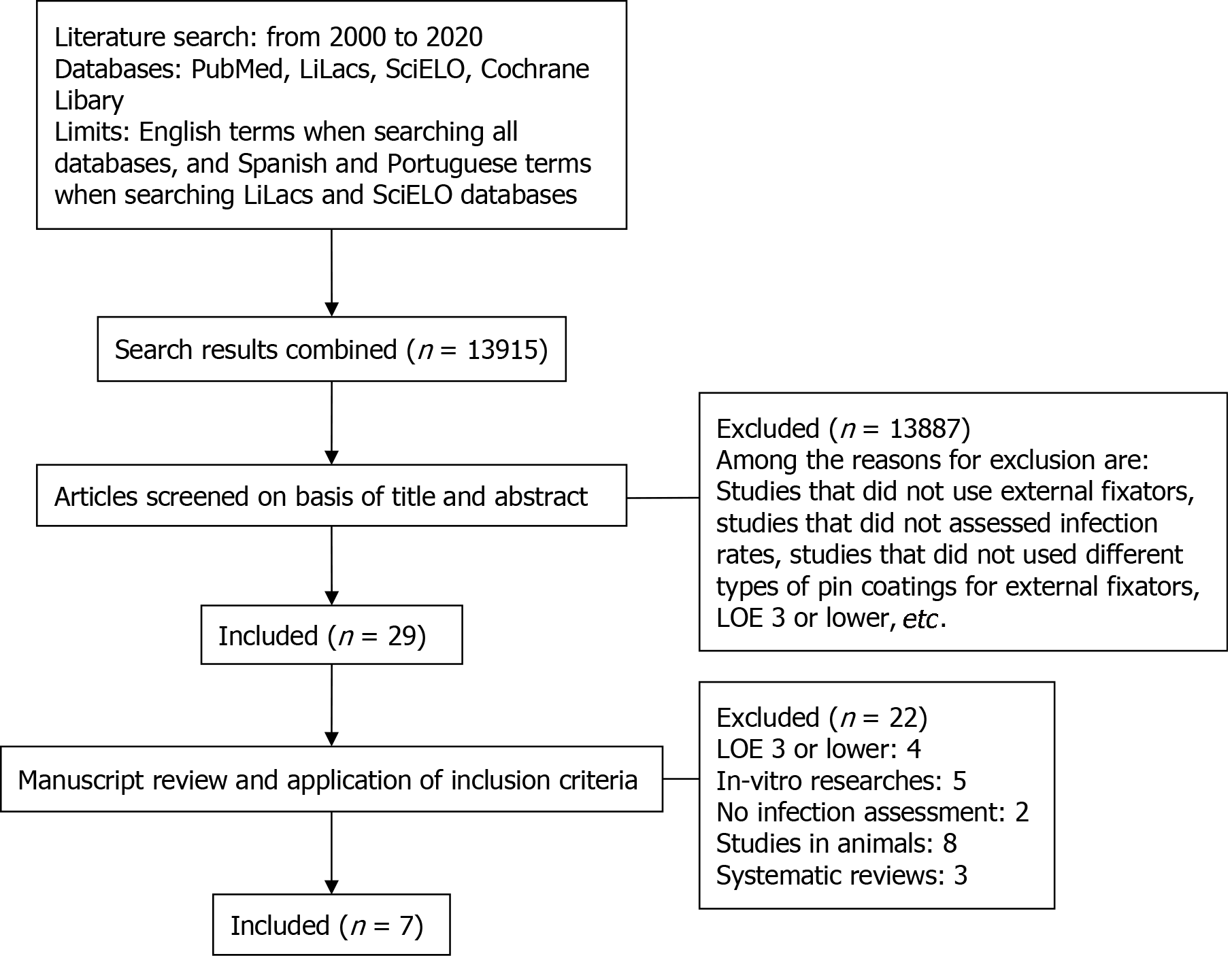
A systematic review was carried out according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines in the following databases: PubMed, LiLacs, SciELO and Cochrane. The search period spanned from January 2000 to December 2020, encompassing all relevant articles published in the last 20 years. The search was performed using key words related to the subject: “External Fixators”, “Fixation Devices, External”, “Pin Site”, “Pin Tract”, “Coated Pin”, “Hydroxyapatite Coated”, “Stainless Steel Pin” and “Hydroxyapatite-coated”. We used English terms when searching all databases and Spanish and Portuguese terms when searching the LiLacs and SciELO databases.
In the search, the population subject of this review is defined as any human being, regardless of sex or age, who has undergone any type of external fixator device procedure for the treatment of any pathology. In these studies, an objective assessment of pin tract infection rates should be made. One or more types of pin materials and coatings may be studied besides steel pins. We included clinical studies with a level of evidence of 1-2. In vitro, basic science, animal studies and previous systematic reviews are exclusion criteria. Also, studies with a level of evidence of 3-5 are excluded. The main objective of this study is to assess whether different materials and coatings, in addition to stainless steel, play a role in reducing the infection rate of the pin site, using the body of available clinical literature and its level of evidence. The quality of published literature was assessed. Whenever possible, a meta-analysis was performed to assess the effectiveness of coating systems and materials at reducing the rates of pin infection.
Two reviewers (CS, MJCS) independently selected the relevant articles based on reading the abstracts. Articles containing only scientific information on different infection rates and comparisons of the different types of pin materials and coatings were selected. All relevant texts, tables and figures have been revised for data extraction. If additional information was needed, the corresponding authors of the articles would be contacted, but it was not necessary. Discrepancies between the two reviewers were resolved by consensus discussion.
We used the Cochrane Risk of Bias Tool to calculate the risk of bias, as shown in Table 1. Among the 29 articles selected for the study, seven studies classified as clinical trials were selected for the article, all of these articles presented a low risk of bias for the randomization sequence generation category (Coester, 2006; Masse, 2000; Morone, 2001; Pieske, 2010; Pieske, 2011; Pizà, 2004; Pommer, 2002). Five described how allocation secrecy was carried out to reduce the risk of bias (Morone, 2001; Pieske, 2010; Pieske, 2011; Pizà, 2004; Pommer, 2002). Only two studies blinded patients (Pieske, 2010; Pieske, 2011), and three articles blinded the evaluators (Pieske, 2010; Pieske, 2011; Pommer, 2002). All seven articles presented the follow-up losses of study participants and presented a low risk of bias for the selective outcome reporting category (Coester, 2006; Masse, 2000; Morone, 2001; Pieske, 2010; Pieske, 2011; Pizà, 2004; Pommer, 2002).
| Study | Random sequence generation | Allocation concealment | Blinding of patients, personnel | Blinding of outcome assessor | Incomplete outcome data | Selective outcome reporting | Other |
| Coester, 2006 | Low | Low | Unclear | Low | Low | Low | Low |
| Masse, 2000 | Low | Unclear | Unclear | Unclear | Low | Low | Low |
| Morone, 2001 | Low | Low | Unclear | Unclear | Low | Low | Low |
| Pieske, 2010 | Low | Low | Low | Low | Low | Low | Low |
| Pieske, 2011 | Low | Low | Low | Low | Low | Low | Low |
| Pizà, 2004 | Low | Low | Unclear | Unclear | Low | Low | Low |
| Pommer, 2002 | Low | Low | Unclear | Low | Low | Low | Low |
The meta-analysis was performed using the Mantel-Haenszel statistical method. The model used was of random effects and the measurement of the effect through the relative risk. An alpha value of 0.05 and a 95% confidence interval were considered statistically significant. The statistical heterogeneity of the treatment effects between the studies was assessed by the Cochran Q test. Inconsistency was assessed by the I2 test, in which values between 25% and 50% were considered to indicate moderate heterogeneity and high heterogeneity was shown by values greater than 50%. All analyses were performed using Review Manager software version 5.4 (Cochrane Collaboration).
A total of 13951 articles were initially retrieved from different platforms. The abstracts of these articles were downloaded to the EndNote Clarivate™ analytics platform. After analyzing the abstracts of all 13951 articles retrieved from the search platform, both reviewers defined the same group of 29 articles for inclusion in the systematic review.
After the initial selection stage, further screening was carried out in which the 29 articles were read in full, and their contents discussed to reach a consensus on their inclusion in the final results of the study. The final group of articles comprised only clinical studies that focused on infection rates associated with the different external fixator pin materials and coatings in humans within the aforementioned inclusion criteria. Seven of the 29 articles contained data on infection rates involving the different pin materials and coatings in humans.
All stages of search, selection and exclusion of the articles listed in this study, as the 2009 PRISMA guide recommends, are shown as a diagram in Figure 1.
A total of seven scientific articles were selected as consistent scientific sources for inclusion in the systematic review. The selection results, showing the different types of materials and coatings studied and their results with respect to infection rates in the pin tract, are described below. It was possible to perform three meta-analyses comparing the following coatings: silver-steel, HA-titanium, and HA-steel.
In 2001, Moroni et al[12] conducted a prospective randomized study comparing infection rates in 20 patients with wrist fractures treated with external fixators divided into two groups. One of the groups used steel pins, and the other one used pins coated with hydroxyapatite. The Checketts-Otterburn classification was used as a criterion for infection, and the patients were followed for 6 wk. There were no reports of infection in both groups[19].
In 2004, Pizà et al[14] conducted a prospective randomized clinical study, comparing infection rates between pins coated with hydroxyapatite and steel pins. Overall, 23 patients were evaluated in which 56 external fixators were used, with a follow-up of 530 d. Infection rates between pins were assessed using the Checketts-Otterburn classification and found to be similar, with 30.4% for hydroxyapatite pins and 30.7% for steel pins[14].
In 2010, Pieske et al[20] published a prospective randomized study comparing the clinical benefits of traditional stainless-steel pins to hydroxyapatite-coated pins for the treatment of wrist fractures with external fixators. The authors assessed rates of pin tract infection and loosening based on bespoke criteria defining infection. A short period of follow-up (6 wk) was used until EF removal in both groups. Overall, 40 patients were assessed and divided into two groups of 20 patients each. Hydro
In 2002, Pommer et al[21] published a randomized clinical trial comparing pins coated with hydroxyapatite and titanium pins. In this study, 46 patients submitted to bone transport or tibial bone lengthening with external fixators were evaluated, divided into two groups according to the type of materials. The follow-up was 38 wk, and the infection criterion used was that of Mahan et al[22] (1991). The infection rates found were 0% in the group with pins coated with hydroxyapatite and 13% in the group with titanium pins, showing a statistically significant difference in infection rates[21].
In 2011, Pieske et al[20] published a prospective controlled cohort study comparing hydroxyapatite-coated pins with titanium alloy pins for the treatment of wrist fractures using external fixators. As in their 2010 study described above, the authors assessed pin infection and loosening rates and employed bespoke criteria for defining pin tract infection. The follow-up time was 6 wk until the removal of fixators in both groups. They also assessed 40 patients divided into two groups, each comprising of 20 patients. The results proved comparable to those of the previous study by the same authors, revealing only a tendency of hydroxyapatite-coated pins to yield lower rates of loosening and infection, although this difference did not reach statistical significance[21].
Two articles compared infection rates in silver pins with steel pins. In 2000, Masse published a prospective randomized study in which they evaluated 24 patients, comparing, among other variables, the infection rates between silver and steel pins. The infection criterion was based upon Mahan et al[22], and the follow-up for the silver and steel groups was 109 d and 113 d, respectively. The infection rate was 30% for silver pins and 42.9% for steel pins, but the difference was not statistically significant. In addition, they observed an increase in serum silver levels in some patients who received silver pins, and as a conclusion, they advised against the use of silver pins[23].
In 2006, Coester et al[24] carried out a randomized clinical trial comparing silver pins with steel pins. They evaluated 19 patients over an average period of 16.7 wk. As an infection criterion, they used a bespoke evaluation and found an infection rate of 30% in silver pins against 21% in steel pins, with no statistically significant difference between the two[24].
It is worth mentioning that all selected studies compared only two types of pin materials and coating systems. None included more than two different types of coating for comparison. Additionally, information such as the reasons for external fixator indications and classification for the severity of fractures or deformities were not necessarily mentioned in the studies. Nevertheless, the selected articles met the inclusion criteria and the desired literary quality.
The main characteristics of all selected studies are shown in Table 2.
| Author | Year | Level of evidence | Number of patient (n) | Coatings | Follow-up | Infection criteria | Infection rate | Conclusion |
| Masse | 2000 | 2 | 24 | Silver vs Steel | 109 d vs 113 d | Mahan et al[22] criteria | 30% vs 42.9% | No statistical difference |
| Moroni | 2001 | 1 | 20 | Hydroxyapatite vs Steel | 6 wk | Checketts-Otterburn | 0 | No statistical difference |
| Pommer | 2002 | 1 | 16 | Hydroxyapatite vs Titanium | 38 wk | Mahan et al[22] criteria | 0% vs 13% | Statistically significant |
| Pizá | 2004 | 1 | 23 | Hydroxyapatite vs Steel | 530 d | Checketts-Otterburn | 30.4% vs 30.7% | No statistical difference |
| Coaster | 2006 | 1 | 19 | Silver vs Steel | 16,7 wk | Bespoke | 30% vs 21% | No statistical difference |
| Pieske | 2010 | 2 | 20 vs 20 | Steel vs Hydroxyapatite | 65 d | Bespoke | 5.3% vs 2.6% | No statistical difference |
| Pieske | 2011 | 2 | 20 vs 20 | Titanium vs Hydroxyapatite | 56 d | Bespoke | 0% vs 10% | No statistical difference |
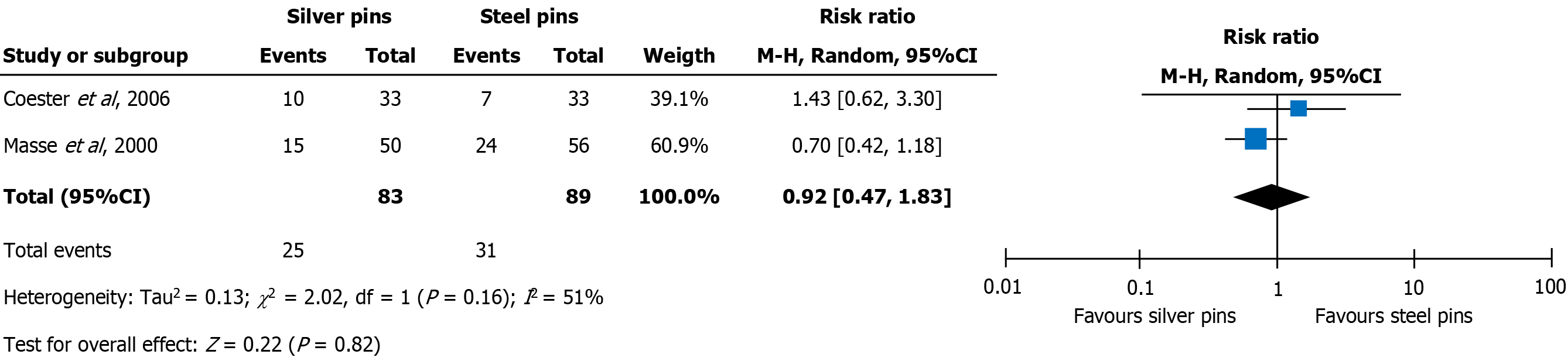
Two studies compared the infection rate between silver pins vs. steel pins[23,24]. The use of silver pins did not show any significant difference (0.92; 95%CI: 0.47 to 1.83; I2 = 51%; P = 0.82) in the infection rate compared to steel pins, as shown in Figure 2. The meta-analysis showed high heterogeneity and can be explained by the methodological difference in assessing the infection rate, according to criteria described by different authors. Both articles showed good methodological quality.
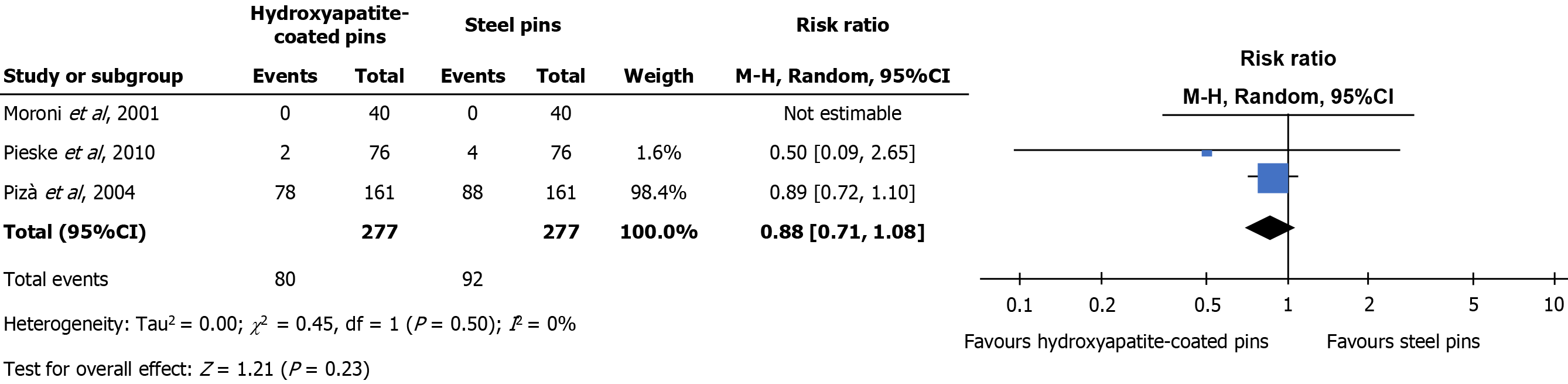
Three articles compared pin tract infection rates between HA-coated pins vs. stainless steel pins[10,14,19]. No statistically significant difference was found in the rate of infection when comparing HA-coated with stainless steel pins (0.88; 95%CI: 0.71 to 1.08; I2 = 0%, P = 0, 23), as shown in Figure 3.
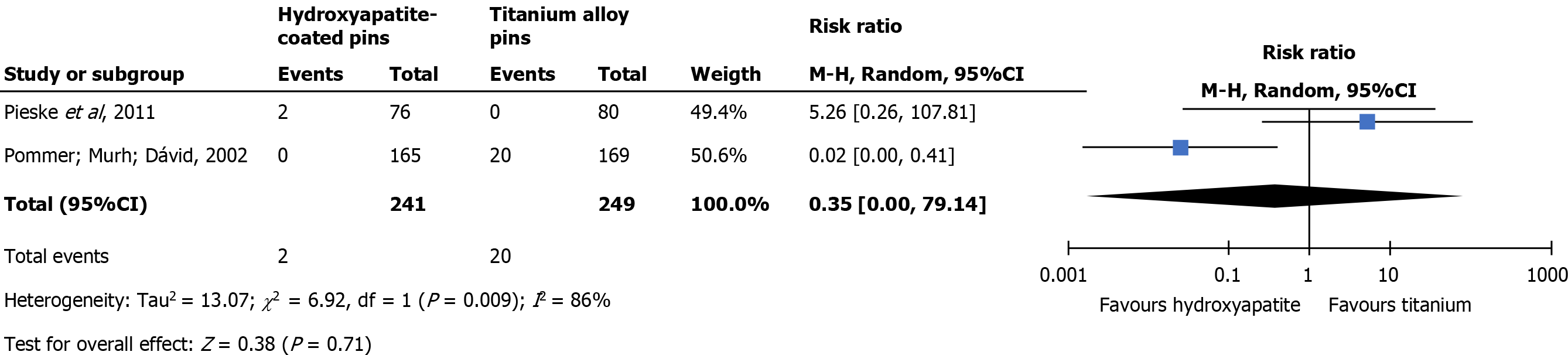
Two studies compared the infection rate between HA-coated pins vs. titanium pins[20,21]. The use of HA-coated pins had no significant difference in the rate of infection compared to titanium pins (0.35; 95%CI: 0.00 to 79.17; I2 = 86%, P = 0, 71), as shown in Figure 4. The heterogeneity of this meta-analysis is characterized as high, possibly because these articles evaluate the rates of infection using different scales. Both articles have good methodological quality.
The following coatings and materials were studied in addition to steel in the studies selected for analysis according to our inclusion criteria: (1) Silver: Known for its antimicrobial and bacteriostatic activity, is used in medical equipment such as special dressings and urinary catheters. Its potential antimicrobial mechanisms are the production of reactive oxygen species with direct effects on DNA and cell membranes. Bacterial resistance to silver is rare[25]; and (2) Hydroxyapatite: A molecule composed of calcium and phosphate, is the main mineral component of human bone and is used on a large scale in orthopedic surgery. It has osteoconductive properties and has been used in an attempt to decrease infection and loosening rates in the pins of external fixators[11,26].
Titanium has anti-corrosion and mechanical properties that favor its use in external fixators. With exposure to oxygen, a spontaneous stable oxide layer forms and leads to biocompatibility[27].
We also found studies evaluating other materials that did not meet the inclusion criteria: ceramic pins, pins with bisphosphonate coating, titanium pins with iodine coating, and pins with FGF-2-apatite coating.
Ceramic pins produced low interference in the MRI signal, an advantage over metal pins in the event that CNS imaging assessment is required. However, rates of infection and aseptic loosening of ceramic pins were significantly higher than for titanium alloy pins. The infection rate in ceramic pins was 27.3% (12/44) vs 13.3% (35/263) in titanium pins (P = 0.031). Hence, the advantage of lesser interference in MRI for ceramic pins was outweighed by their higher complication rates. The study was not included due to its low level of evidence (LoE)[28].
Bisphosphonate-coated pins have been shown to increase adherence to bone in dental implants. In a randomized clinical trial published in 2013, the possibility of decreasing the rates of loosening of pins in human diaphyseal bone was evaluated. This study was not included because it did not aim to evaluate infection rates between different coatings[16].
Iodine-coated titanium pins were studied in a prospective cohort study published in 2014 that assessed the infection rates in iodine-coated titanium pins in 39 external fixators involving 38 patients. The infection rate was 3.6% (17/476 pins), and all cases were superficial. After comparing with other published studies, the authors concluded that coating titanium with iodine reduced infection rates in external fixator pins. The study was not included due to its low LoE[2].
FGF-2-apatite coating was evaluated in a prospective controlled study comparing titanium pins with and without FGF-2-apatite coating published in 2018. Overall, no significant difference between groups for pin tract infection or loosening was found. The study results concluded that pins coated with FGF-2-apatite were safe, and no severe pin tract infections were observed[29].
In addition to the materials and coatings discussed above, a review study published in 2013 by Jennison et al[30] commented on the possible effect of other materials and coatings such as copper, nitric oxide, chitosan and antibiotics, concluding that at that time, none of them had shown a reduction in infection rates in human clinical trials[30].
Only seven relevant publications with LoE 2 or more were available comparing different pin materials and coating systems with rates of infections in human clinical studies over the past 20 years. The main complications investigated were pin tract infections, torque force for pin removal and loosening rates. The results revealed a lack of standardized criteria established to define and classify pin tract infection. Overall, among the seven studies reviewed, only four systematically adopted a published pin infection classification system, such as the Checketts-Otterburn or the Mahan classification. The other three studies used the authors’ own criteria to classify the degree of infection, potentially leading to disparities between evaluators[10,21,24]. The data retrieved from these studies warranted three meta-analyses, in which two studies compared silver with steel pins[23,24], three studies compared steel pins with HA-coated pins[10,14,19] and two studies compared titanium pins with HA-coated pins[20,21]. Interestingly, none showed a statistically significant impact on the outcome of pin tract infection, which corroborated and confirmed the information shown by other systematic reviews and studies previously carried out[11,12,30].
Despite the limited number of clinical studies addressing new materials and coated pins proposed to prevent infections, some modern strategies have been developed[31]. However, outcomes often depend on coating systems that use different antibiotic compounds, polymers or antibiotic film peptides, silver or nitric ions, nanoparticles or even antiseptics such as chlorhexidine or silver sulfadiazine[1,5,31]. Unfortunately, none of these materials have progressed to clinical trials.
In conclusion, a small number of clinical studies assessing the impact of different coatings and materials on the EF pin tract infection rates have been published over the last 20 years. Currently, there are no standardized methods of defining and classifying pin tract infections. The lack of a clear and universal definition renders existing studies difficult to evaluate and compare. We identified seven quality clinical trials, comparing three different types of coatings, that enabled us to carry out three meta-analyses. The meta-analysis showed high heterogeneity, and none of the coating systems and materials was superior at reducing the pin tract infection rates. Under these circumstances, no scientific evidence supports materials other than steel pins to control infection rates of EF pins. Prospective multicenter clinical trials involving modern pin materials and new coating systems are very much welcomed to find a way to reduce infection rates, which are considerable in the use of EF.
Few clinical studies assessed the impact of pin materials and coating systems on infection rates over the last 20 years.
Few studies identified significant differences between pin materials in the rate of infection. There has been a lack of standardized criteria for defining and grading pin tract infection of external fixators.
Search the literature of the last 20 years for evidence on the influence of coating systems and different materials of external fixator pins on infection rates.
A systematic review was carried out, over the last 20 years, according to the preferred reporting items for systematic reviews and meta-analyses guidelines in the following databases: PubMed, LiLacs, SciELO and Cochrane.
Seven studies met the inclusion criteria and allowed for three different meta-analyses between similar coating systems and materials used. Due to the heterogeneity of the studies, it was not possible to carry out a meta-analysis that encompassed all selected works.
Currently, no significant clinical benefit to control infection rates has been achieved with our coating pins systems.
Prospective multicenter clinical trials involving pin materials and new coating systems should be carried out.
We would like to thank Ciconelli R and Zanini SCC for technical and support in the systematic review process.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Orthopedics
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Faur C S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Bliven EK, Greinwald M, Hackl S, Augat P. External fixation of the lower extremities: Biomechanical perspective and recent innovations. Injury. 2019;50 Suppl 1:S10-S17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 2. | Shirai T, Watanabe K, Matsubara H, Nomura I, Fujiwara H, Arai Y, Ikoma K, Terauchi R, Kubo T, Tsuchiya H. Prevention of pin tract infection with iodine-supported titanium pins. J Orthop Sci. 2014;19:598-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Sisk TD. External fixation. Historic review, advantages, disadvantages, complications, and indications. Clin Orthop Relat Res. 1983;15-22. [DOI] [Full Text] |
| 4. | Ciofu O, Rojo-Molinero E, Macià MD, Oliver A. Antibiotic treatment of biofilm infections. APMIS. 2017;125:304-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 275] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 5. | Ferreira N, Marais LC. Prevention and management of external fixator pin tract sepsis. Strategies Trauma Limb Reconstr. 2012;7:67-72. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Grant S, Kerr D, Wallis M, Pitchford D. Comparison of povidone-iodine solution and soft white paraffin ointment in the management of skeletal pin-sites: a pilot study. J Orthop Nurs. 2005;9:218-25. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (2)] |
| 7. | W-Dahl A, Toksvig-Larsen S, Lindstrand A. No difference between daily and weekly pin site care: a randomized study of 50 patients with external fixation. Acta Orthop Scand. 2003;74:704-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Lethaby A, Temple J, Santy J. Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database Syst Rev. 2008;CD004551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Goodman SB, Yao Z, Keeney M, Yang F. The future of biologic coatings for orthopaedic implants. Biomaterials. 2013;34:3174-3183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 568] [Cited by in RCA: 445] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 10. | Pieske O, Kaltenhauser F, Pichlmaier L, Schramm N, Trentzsch H, Löffler T, Greiner A, Piltz S. Clinical benefit of hydroxyapatite-coated pins compared with stainless steel in external fixation at the wrist: a randomized prospective study. Injury. 2010;41:1031-1036. [RCA] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Saithna A. The influence of hydroxyapatite coating of external fixator pins on pin loosening and pin tract infection: a systematic review. Injury. 2010;41:128-132. [RCA] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Moroni A, Pegreffi AMF, Cadossi M, Hoang-Kim A, Lio V, Giannini S. Hydroxyapatite-coated external fixation pins. Expert Rev Med Devices. 2005;2:465-471. [RCA] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Britten S, Ghoz A, Duffield B, Giannoudis PV. Ilizarov fixator pin site care: the role of crusts in the prevention of infection. Injury. 2013;44:1275-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Pizà G, Caja VL, Gonzáles-Viejo MA, Navarro A. Hydroxyapatite-coated external-fixation pins. The effect on pin loosening and pin-tract infection in leg lengthening for short stature. J Bone Joint Surg Br. 2004;86:892-897. [RCA] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Nakamura H, Matsuno T, Hashimoto Y, Nakamura T, Mataga I. Comparison of a hydroxyapatite-coated and an anodic oxidized titanium implant for experimentally induced peri-implantitis: macroscopic and novel radiographic evaluations in a canine model. J Hard Tissue Biol. 2015;24:347-355. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Toksvig-Larsen S, Aspenberg P. Bisphosphonate-coated external fixation pins appear similar to hydroxyapatite-coated pins in the tibial metaphysis and to uncoated pins in the shaft. Acta Orthop. 2013;84:314-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Kazmers NH, Fragomen AT, Rozbruch SR. Prevention of pin site infection in external fixation: a review of the literature. Strategies Trauma Limb Reconstr. 2016;11:75-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 111] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 18. | Arciola CR, Montanaro L, Moroni A, Giordano M, Pizzoferrato A, Donati ME. Hydroxyapatite-coated orthopaedic screws as infection resistant materials: in vitro study. Biomaterials. 1999;20:323-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Moroni A, Faldini C, Marchetti S, Manca M, Consoli V, Giannini S. Improvement of the bone-pin interface strength in osteoporotic bone with use of hydroxyapatite-coated tapered external-fixation pins. A prospective, randomized clinical study of wrist fractures. J Bone Joint Surg Am. 2001;83:717-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 75] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Pieske O, Pichlmaier L, Kaltenhauser F, Schramm N, Rubenbauer B, Greiner A, Piltz S. Hydroxyapatite-coated pins vs titanium alloy pins in external fixation at the wrist: a controlled cohort study. J Trauma. 2011;70:845-851. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Pommer A, Muhr G, Dávid A. Hydroxyapatite-coated Schanz pins in external fixators used for distraction osteogenesis : a randomized, controlled trial. J Bone Joint Surg Am. 2002;84:1162-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Mahan J, Seligson D, Henry SL, Hynes P, Dobbins J. Factors in pin tract infections. Orthopedics. 1991;14:305-308. [PubMed] |
| 23. | Massè A, Bruno A, Bosetti M, Biasibetti A, Cannas M, Gallinaro P. Prevention of pin track infection in external fixation with silver coated pins: clinical and microbiological results. J Biomed Mater Res. 2000;53:600-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Coester LM, Nepola JV, Allen J, Marsh JL. The effects of silver coated external fixation pins. Iowa Orthop J. 2006;26:48-53. [PubMed] |
| 25. | Chaloupka K, Malam Y, Seifalian AM. Nanosilver as a new generation of nanoproduct in biomedical applications. Trends Biotechnol. 2010;28:580-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 988] [Cited by in RCA: 806] [Article Influence: 53.7] [Reference Citation Analysis (0)] |
| 26. | Shepperd JA, Apthorp H. A contemporary snapshot of the use of hydroxyapatite coating in orthopaedic surgery. J Bone Joint Surg Br. 2005;87:1046-1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Neoh KG, Hu X, Zheng D, Kang ET. Balancing osteoblast functions and bacterial adhesion on functionalized titanium surfaces. Biomaterials. 2012;33:2813-2822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 217] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 28. | Kraemer P, Lee MB, Englehardt H, Chapman JR, Bransford RJ. Infectious pin complication rates in halo vest fixators using ceramic vs metallic pins. J Spinal Disord Tech. 2010;23:e, 59-62. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Yanagisawa Y, Ito A, Hara Y, Mutsuzaki H, Murai S, Fujii K, Sogo Y, Hirose M, Oyane A, Kobayashi F, Yamazaki M. Initial clinical trial of pins coated with fibroblast growth factor-2-apatite composite layer in external fixation of distal radius fractures. J Orthop. 2019;16:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Jennison T, McNally M, Pandit H. Prevention of infection in external fixator pin sites. Acta Biomater. 2014;10:595-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 31. | Gil D, Shuvaev S, Frank-Kamenetskii A, Reukov V, Gross C, Vertegel A. Novel Antibacterial Coating on Orthopedic Wires To Eliminate Pin Tract Infections. Antimicrob Agents Chemother. 2017;61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |