Published online Nov 18, 2021. doi: 10.5312/wjo.v12.i11.850
Peer-review started: May 24, 2021
First decision: July 16, 2021
Revised: July 28, 2021
Accepted: September 15, 2021
Article in press: September 15, 2021
Published online: November 18, 2021
Processing time: 175 Days and 10.7 Hours
Direct anterior approach (DAA) total hip arthroplasty (THA) in a supine position provides a unique opportunity to assess leg length discrepancy (LLD) intra-operatively with fluoroscopy. Reported fluoroscopic techniques are useful but are generally complicated or costly. Despite the use of multiple techniques for leg length assessment, LLD continues to be a major post-operative source of patient dissatisfaction further emphasizing the importance of near-anatomic restoration. The utility of an alternative direct measurement of LLD on an intra-operative fluoroscopic pelvic image during DAA THA has not been reported.
To determine the reliability of a novel simple intra-operative measurement of LLD using a parallel line technique on a single fluoroscopic digital image of the pelvis.
One hundred and seventy-one patients who underwent DAA THA were included for analysis. Intra-operative fluoroscopic and post-operative anterior-posterior radiographs were imported to TraumaCad and calibrated for LLD measurement. LLD was measured on each image using the right-left hip differences in lesser trochanter to pelvic reference line distances. Pelvic reference points included the teardrops and ischia. Fluoroscopic LLD was compared to the gold-standard measurement of LLD measured on a post-operative radiograph.
Mean absolute difference in teardrop referenced LLD between fluoroscopic and post-operative radiographs was 2.17 mm and based on the ischia mean absolute difference was 2.63 mm. Linear regression of fluoroscopic and post-operative radiograph LLD based on teardrop and ischia LLD found r2 values of 0.57 and 0.84, respectively. Mean absolute difference between fluoroscopic and post-operative x-ray LLD was within 5 mm in 95% of cases regardless of pelvic reference.
This study demonstrates that a single fluoroscopic view obtained during DAA THA for leg length assessment is clinically useful.
Core Tip: The direct anterior approach (DAA) for total hip arthroplasty (THA) has grown in popularity among Orthopaedic Surgeons in recent years. Despite the growth in this approach for THA, leg length discrepancy continues to be a major source of post-arthroplasty dissatisfaction in patients. Here we demonstrate that a single intra-operative fluoroscopic image for leg length assessment has clinical significance among patients undergoing DAA THA.
- Citation: Caus S, Reist H, Bernard C, Blankstein M, Nelms NJ. Reliability of a simple fluoroscopic image to assess leg length discrepancy during direct anterior approach total hip arthroplasty. World J Orthop 2021; 12(11): 850-858
- URL: https://www.wjgnet.com/2218-5836/full/v12/i11/850.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i11.850
Leg length discrepancy (LLD) is a significant source of patient dissatisfaction after total hip arthroplasty (THA). An error in achieving acceptable leg length may manifest as discomfort, nerve palsy, pelvic obliquity, compensatory lumbar scoliosis, or result in need for revision surgery[1-4]. To minimize LLD after THA, multiple techniques have been developed for intra-operative assessment of leg length. In a survey conducted by the British Hip Society, surgeons reported utilizing a median of five techniques during THA to estimate LLD[5].
The direct anterior approach (DAA) for THA with a patient in a supine position has recently grown in popularity and presents an opportunity to use fluoroscopy intra-operatively to assess component position, size, femoral offset and LLD. Use of a specialized traction table facilitates this procedure but may also increase reliance on fluoroscopically based assessment of LLD[6,7]. Reported techniques to assess LLD intra-operatively with fluoroscopy during DAA THA include printed or virtual image overlays, concurrent imaging of a radio-opaque linear marker, and computer assisted image analysis techniques to correct for image distortion[5,8]. These previously reported fluoroscopic techniques can add time, complexity, radiation exposure, or significant cost to the procedure.
The aim of this study is to determine the reliability of an alternative novel simple intra-operative measurement of LLD using a parallel line technique on a single fluoroscopic digital image of the pelvis during DAA THA.
A retrospective study was performed of DAA THA's performed by two fellowship trained adult reconstruction surgeons between January 1, 2019 and December 31, 2019. Over this period, 182 patients were identified as eligible for inclusion in this study. Eligibility criteria included THA done by DAA on a Hana table, an adequate quality appropriate intra-operative fluoroscopic image saved, and a standard post-operative pelvic radiograph available. The fluoroscopic image had to be a centered view of the pelvis such that both lesser trochanters were visible with all final THA components in place including the final femoral head. This study was approved by our institutional review board.
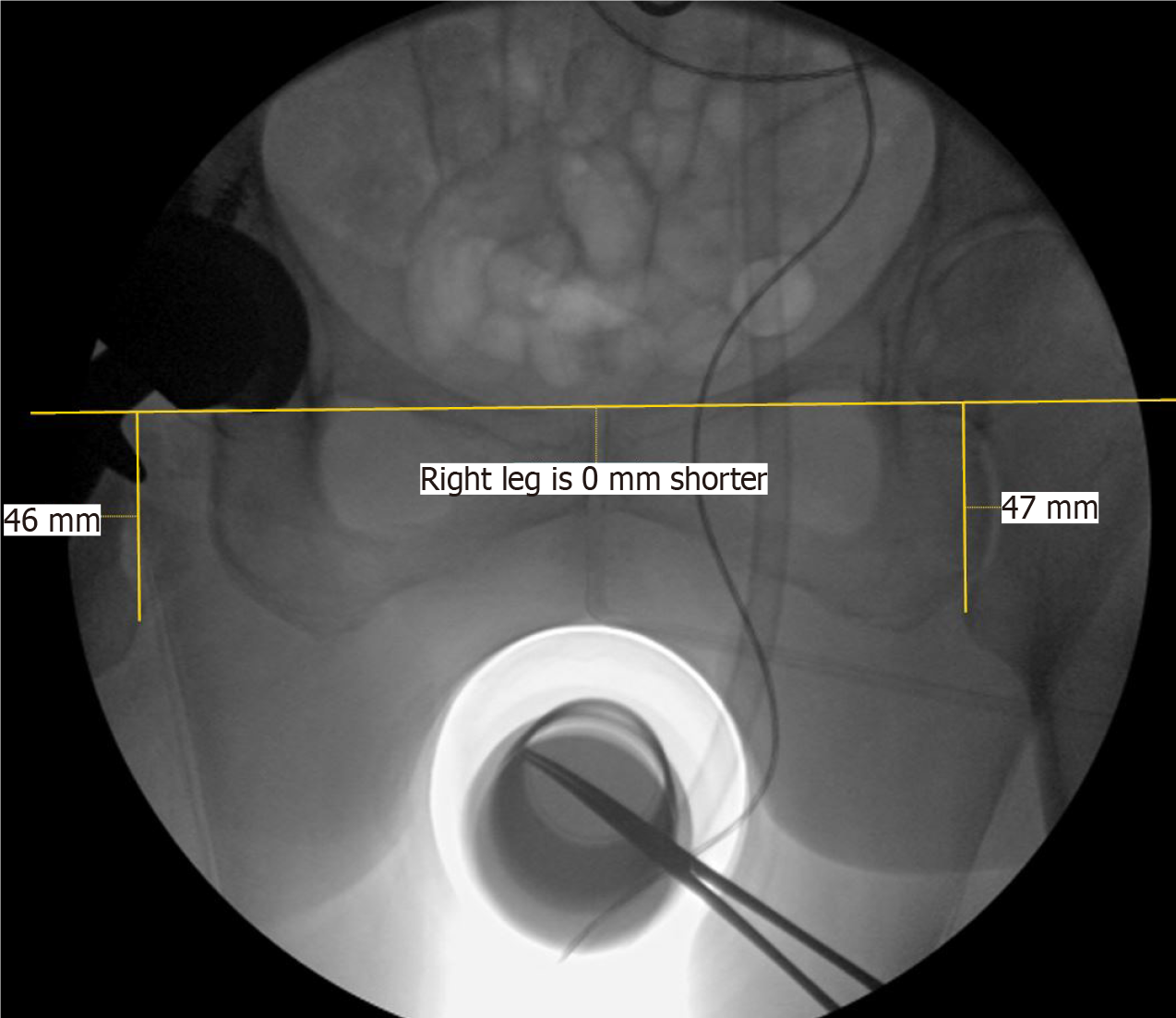
During each DAA THA, LLD was assessed after trial components were in place using a single view of the pelvis obtained with an 18-inch OEC image intensifier (GE Healthcare). The image was typically performed with each leg externally rotated 20 degrees to display the profiles of the lesser trochanters. Once an adequately centered image of the pelvis was obtained, a line was drawn between the radiographic teardrops utilizing the OEC digital measurement tool. Then a second line was drawn through the prominence of the lesser trochanters. The two lines were then visually inspected to determine how near they were to parallel. Adjustments to trial com
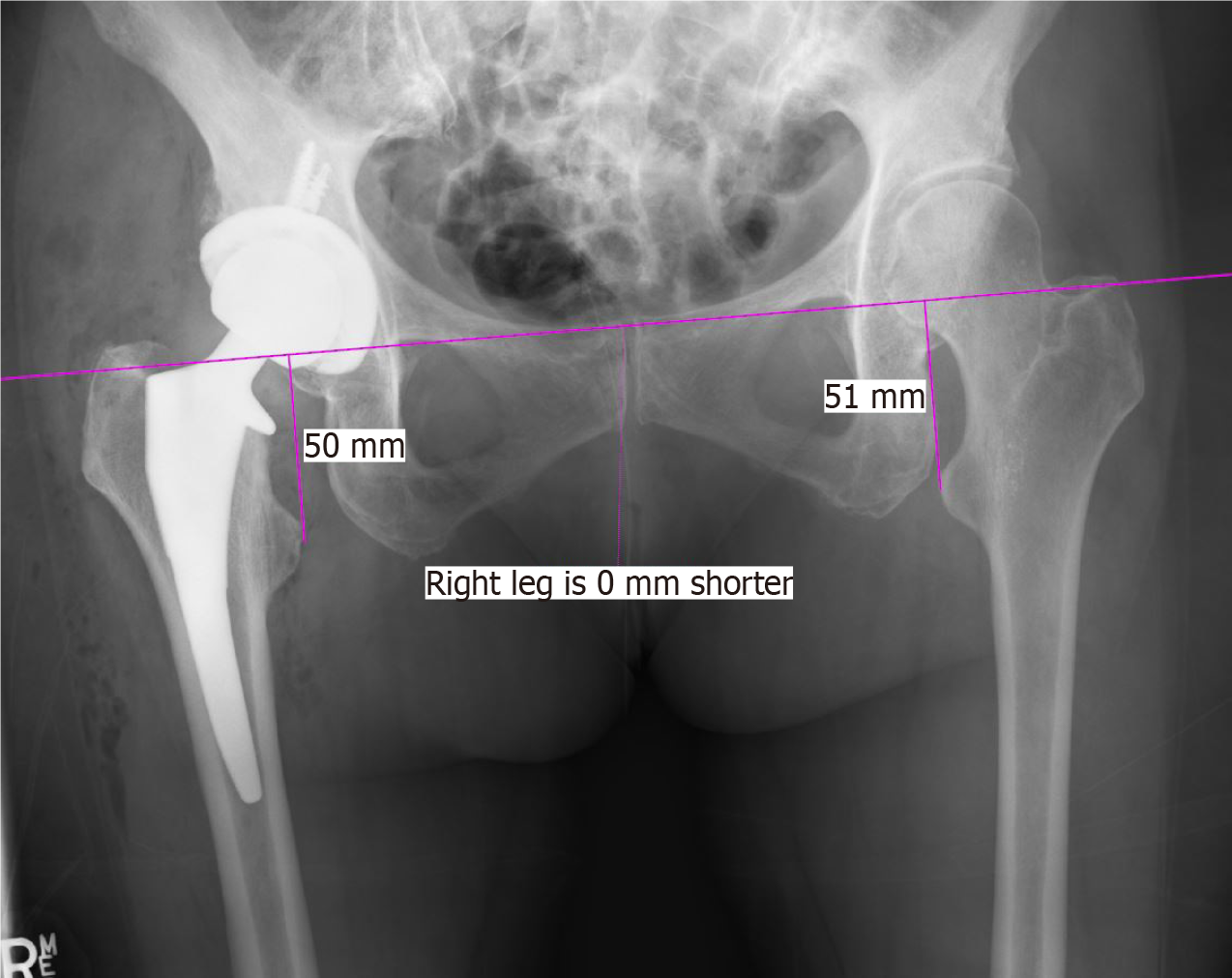
Fluoroscopic and AP radiographs each with the final components in position were imported to TraumaCad for analysis by two independent observers (Nelms NJ and Caus S). Fluoroscopic and AP radiographs were calibrated manually to adjust for image magnification by matching the circular shape of the THA femoral head to the surgical component size in millimeters as recorded in the subject’s operative note. The digital leg length comparison tool within TraumaCad was utilized to measure LLD based on teardrop and ischial pelvic reference lines (Figures 1 and 2). From each reference line a perpendicular distance was measured to the medial prominence of the right and left lesser trochanters. The left hip distance was subtracted from the right hip on both the fluoroscopic and x-ray images so that a positive or negative value represented which leg was longer. A positive value indicated a longer right leg, conversely a negative value indicated a shorter right leg. This was important to be able to define the relative LLD by side in case fluoroscopy and x-ray conflicted as to which leg was longer.
After all measurements were independently completed by two observers, cases with an inter-observer disagreement in LLD measurement of greater than 5 mm in either the intra-operative fluoroscopic images or anterior posterior radiographs were flagged for repeat measurement[8]. Repeat measurements were again performed independently to determine if the two observers could agree within 5 mm on LLD measurement. Of the initial 182 cases there were 25 cases for which two observers could not agree within 5 mm on LLD and a second independent measurement was completed. Of these 25 cases, the observers were unable to agree within 5 mm on the measured LLD in 11 cases. These 11 cases were removed from further analysis because the measurement inconsistency was attributed to poor image quality or difficult to define radiographic landmarks. This left a final count of 171 subjects for statistical analysis.
The mean, standard deviation, and maximum LLD measured on x-ray and intra-operative fluoroscopy with teardrop and ischium references were calculated (n = 171). The difference in x-ray and fluoroscopic LLD was calculated by subtraction and the absolute value taken. The mean absolute difference in x-ray and fluoroscopic LLD measurements were compared between the teardrop and ischial reference points using a paired t-test. Linear regression was performed to determine the relationship between LLD measured with fluoroscopy vs x-ray for both teardrop and ischial references.
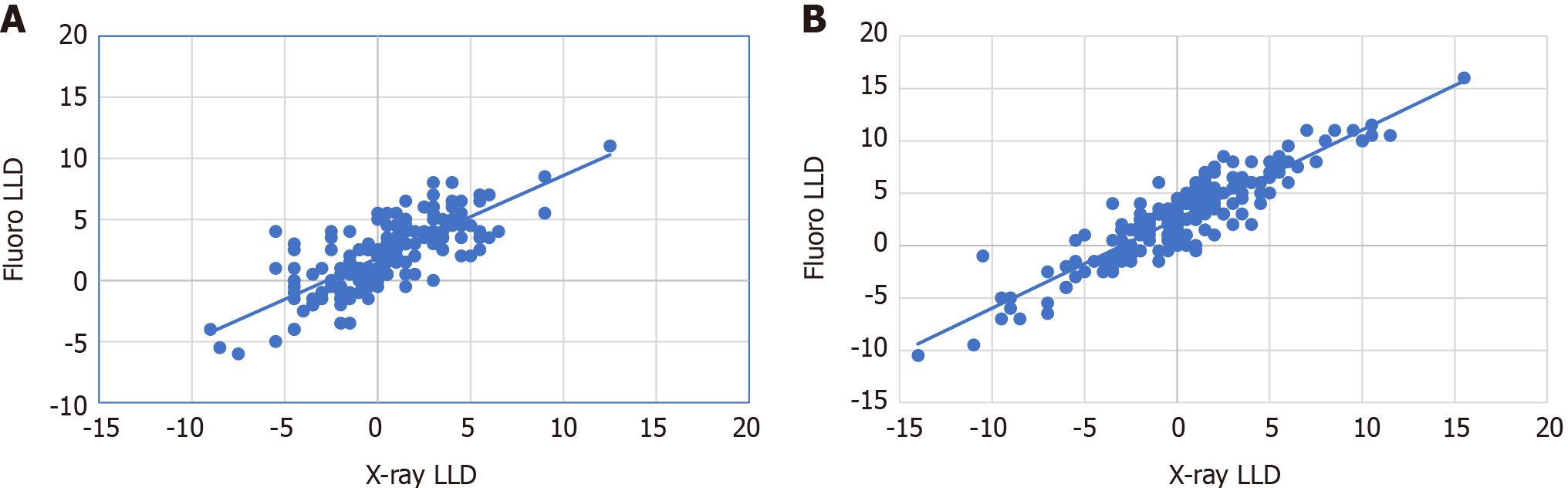
Overall mean LLD measured by the teardrops with fluoroscopy was 2.89 mm (SD = 2.07) and by x-ray 2.45 mm (SD = 2.11). Mean LLD measured by the ischia with fluoroscopy was 3.93 mm (SD = 2.95) and by x-ray 3.27 mm (SD = 3.01) (Table 1). Measurements with both teardrop and ischial landmarks demonstrated a statistically significant difference between the mean observed LLD with fluoroscopy compared with the gold standard x-ray (P = 0.007, P < 0.001). This difference included a bias toward overestimation of LLD by fluoroscopy especially when using an ischial pelvic reference.
| Fluoroscopic | X-ray | ||||||||
| Mean | SD | Min | Max | Mean | SD | Min | Max | P value | |
| LLD by Teardrops | 2.89 | 2.07 | 0.0 | 11.0 | 2.45 | 2.11 | 0.0 | 12.5 | 0.007 |
| LLD by Ischiums | 3.93 | 2.95 | 0.0 | 16.0 | 3.27 | 3.01 | 0.0 | 15.5 | < 0.001 |
Based on the teardrops, the mean absolute difference in LLD between fluoroscopic and x-ray was 2.17 mm (SD = 1.7). Referencing the ischia, the mean absolute difference in fluoroscopic and x-ray LLD was 2.63 mm (SD = 1.64) (Table 2). There was a statistically significant difference between the ischial and teardrop reference measurements of LLD, with a larger discrepancy between x-ray and fluoroscopic LLD observed using the ischial reference points (P < 0.001).
| Teardrop | Ischium | ||||||||
| Mean | SD | Min | Max | Mean | SD | Min | Max | P value | |
| Fluoro-x-ray difference | 2.17 | 1.7 | 0.0 | 9.50 | 2.63 | 1.64 | 0.0 | 9.5 | < 0.001 |
Linear regression of fluoroscopic and x-ray measurements based on the teardrops and ischia found r2 values of 0.57 and 0.84, respectively (Figure 3). Despite the observed statistical differences, the absolute difference in LLD between fluoroscopic and x-ray measurements with either landmark was within 5 mm in 95% of cases. In only 1.8% of cases were both teardrop and ischial referenced fluoroscopic LLD measurements greater than 5 mm different from the gold standard x-ray LLD. Furthermore, we achieved a LLD of < 5 mm in 88.9% of patients and of < 10 mm in 98.8% of patients as assessed on a gold-standard post-operative x-ray of the pelvis.
Direct measurement of LLD on a single fluoroscopic view of the pelvis during DAA THA provided a clinically reasonable estimation of LLD in most of our cases. Using the teardrops for pelvic reference resulted in the closest association between intra-operative fluoroscopic and post-operative x-ray LLD. Although an ischial reference had a stronger linear correlation for LLD than the teardrops, there was a greater systematic overestimation of LLD when measuring from the ischia with fluoroscopy. Nonetheless, the difference between fluoroscopic and x-ray assessment of LLD using either teardrop or ischial landmarks was typically relatively small from a clinical standpoint. The fluoroscopic measurements with either pelvic landmark were in agreement with post-operative x-ray LLD measurements by a margin of 5 mm in 95% of cases. This degree of accuracy is useful because up to a 5 mm LLD is widely considered clinically insignificant and even up to and slightly beyond 10 mm may not be clinically meaningful[8-11]. For comparison, this simple technique appears more accurate than intra-operative x-ray assessment of LLD with patients in a lateral position. One study found that taking an x-ray with a patient in a lateral position resulted in 20% of cases displaying an intra-operative LLD measurement more than 5 mm different from that measured on a post-operative supine AP pelvis x-ray[12]. It also remains unclear as to the amount of post-operative LLD that can be tolerated without impacting patient function or satisfaction post-operatively[11,13]. Some studies have shown no clinically significant detrimental outcomes in LLDs approaching or even greater than 10 mm, while others have reported significantly worse OHS scores in patients able to perceive any LLD post-operatively[14,15]. Despite evidence that some LLD can be well tolerated after THA, restoration of near anatomic leg length is an important goal. Minimizing LLD after THA is critical because patient perceived post-operative LLD can result in post-operative joint pain, early revision arthroplasty or litigation[16].
While there is growing clinical evidence in support of a DAA for THA, there is not a gold-standard technique for intra-operative LLD assessment[1,7,13,17]. Previously reported fluoroscopic techniques can add time, complexity, or cost[18-21]. One common technique is overlaying traced printed fluoroscopic images of the contralateral hip, or of the operative hip taken at the start of the procedure, with an image of the operative hip with trial implants in place. This relies heavily on accurate tracing and the surgeon may risk breaching sterility to draw on the images themselves. Also access to a fluoroscopic printer and the cost of printing supplies may prevent this from being universally available to surgeons. Another simple technique is to lay a transverse metal rod over the patient while images are taken until the rod is positioned in a way to estimate a relative LLD. Unfortunately, this usually requires multiple fluoroscopic images to achieve appropriate position of the rod. More specialized computer assisted techniques can partially automate LLD comparisons by allowing virtual image overlays, image stitching, and image correction for distortion. All of these commercial products based on advanced technology add cost.
The benefits of fluoroscopy during DAA THA are technique dependent, but fluoroscopy can provide an intra-operative assessment of leg length, offset, component size, and implant position[22-25]. Interestingly, Bingham et al[26] found no significant difference in post-operative LLD with or without use of intra-operative fluoroscopy when DAA THA was performed by very experienced surgeons with specific techniques which differ from ours. They achieved an impressive mean post-operative LLD of only 1.1 mm with fluoroscopy and 0.8 mm without. However, all DAA THA’s performed in that study without fluoroscopy were performed on a standard operating table with both legs draped to allow direct visual comparison of LLD. Potential benefits of DAA THA on a specialized traction table include improved surgical exposure and access for intra-operative fluoroscopy. Fluoroscopic assessment of LLD is particularly helpful when a specialized traction table is used for DAA THA because the patient’s feet are placed in traction boots which prevents direct clinical comparison of LLD. Even the two most commonly used intra-operative fluoroscopic measurement techniques to minimize image distortion may not result in anatomic leg length restoration. Austin et al[8] reported an average LLD measured on final post-operative x-rays relative to the teardrops of 4.8 mm using fluoroscopic tracing and 4.4 mm using a transverse metal rod technique[8]. These values are similar but surprisingly greater than our comparable average post-operative LLD of 2.45 mm LLD on post-operative x-rays. Austin et al[8] also reported that of the two fluoroscopic techniques, even the most accurate resulted in a final LLD of < 5 mm in only 59.6% of patients but of < 10 mm in 95.3%, which contrasts with our rates of 88.9% and 98.8%, respectively.
We found the assessment of LLD on a single fluoroscopic view of the pelvis to be a useful and simple technique of moderate accuracy. We suspect that by drawing lines through the teardrops or ischiums and comparing this to a line through the lesser trochanters is effective because image distortion is partially cancelled by such effects on both lines. In our clinical practice, we have achieved success by combining this parallel line fluoroscopic estimation of LLD with careful pre-operative templating and assessment of THA tension with a “shuck test” using a bone hook to feel the force necessary to distract the hip. We believe it is important to have more than one technique to estimate LLD intra-operatively. This study shows the clinical usefulness of fluoroscopy during THA on a traction table using a very simple technique.
Our study does have several limitations. In 6% of cases, our independent observers could not agree within 5 mm on the LLD measurements. This demonstrates some subjectivity in identifying radiographic landmarks despite efforts to establish consistency in these measurements between observers prior to beginning this study. We believe it was reasonable to exclude these cases so that the effects of subjective image interpretation can be diminished. We acknowledge that any measurement of LLD based on imaging of the pelvis alone may not represent discrepancy in overall leg lengths. True leg length comparison requires clinical evaluation or long leg x-rays, each of which also have their own intrinsic inaccuracies. Even so we demonstrate that combining this fluoroscopic technique with careful pre-operative templating and assessment of joint laxity resulted in minimal average post-operative LLD apparent on x-ray. And this demonstrates that the effects of intra-operative fluoroscopic image distortion do not preclude the clinical usefulness of this simple technique. Our findings are in contrast to the degree of fluoroscopic distortion observed by Carlson et al[27]. This could be because there was less electromagnetic interference in our operating suites or the use of a different model of C-arm.
An intra-operative estimation of LLD of moderate accuracy can be achieved during DAA THA by assessment of a simple AP fluoroscopic image. Assessment of LLD with this technique is achieved by comparing how parallel a digital line drawn through the radiographic teardrops is to a line drawn between corresponding points on the lesser trochanters.
The direct anterior approach (DAA) in total hip arthroplasty (THA) with a patient in the supine position has gained popularity in recent years and provides an opportunity for intra-operative fluoroscopy for assessment of leg length discrepancy (LLD), as well as other intra-operative parameters of interest to Orthopaedic surgeons. LLD remains a significant source of patient dissatisfaction post-arthroplasty and we recognize an opportunity to evaluate the reliability of a novel simple parallel line technique on a single intra-operative fluoroscopic image.
The increase in popularity of the DAA THA combined with the opportunity to utilize intra-operative fluoroscopy has made surgeons wonder about the reliability of fluoroscopy in the clinical setting. We aimed to provide an assessment of this based on a simple parallel line technique on a single intra-operative fluoroscopic image of the pelvis once final arthroplasty components had been positioned.
The primary objective of this study was to understand the accuracy and reliability of a novel simple intra-operative fluoroscopy LLD assessment technique as compared to the standard post-operative x-ray.
171 intra-operative fluoroscopic and anterior-posterior (AP) radiographs with final components in position were imported to TraumaCad for observer LLD analysis. LLD measurements were taken on each image utilizing right-left hip differences in lesser trochanters to two separate pelvic reference points. These were either the radiographic teardrops or ischia. Fluoroscopic LLD measurements were compared to the standard measurement of LLD on a post-operative AP radiograph.
Mean absolute difference between fluoroscopic and post-operative x-ray LLD was within 5 mm in 95% of cases regardless of pelvic reference point. Utilizing the simple parallel line technique on a single fluoroscopic image of the pelvis we achieved an LLD of < 5 mm in 88.9% of subjects and of < 10 mm in 98.8% of subjects as measured on the gold-standard post-operative x-ray.
We demonstrate moderate accuracy in estimation of LLD intra-operatively by assessment of a simple AP fluoroscopic image, specifically with a novel simple parallel line technique. This technique is performed by visually comparing how parallel a digital line drawn trough the radiographic teardrops is to a line drawn between corresponding points on the lesser trochanters. We acknowledge the importance of continuing to have more than one technique intra-operatively to most accurately estimate LLD.
Our study adds to a body of research investigating the clinical usefulness of intra-operative fluoroscopy in the DAA THA, specifically we demonstrate that this technique has clinical benefit in our cohort of patients. Not only do we hope this adds to the body of research and clinical understanding of fluoroscopy, but also hope it can be utilized as an additional reliable technique for assessment of intra-operative LLD.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Surgery
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bäcker HC S-Editor: Liu M L-Editor: A P-Editor: Wang LYT
| 1. | Flecher X, Ollivier M, Argenson JN. Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res. 2016;102:S9-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 153] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 2. | Fujita K, Kabata T, Kajino Y, Tsuchiya H. Optimizing leg length correction in total hip arthroplasty. Int Orthop. 2020;44:437-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Kjellberg M, Al-Amiry B, Englund E, Sjödén GO, Sayed-Noor AS. Measurement of leg length discrepancy after total hip arthroplasty. The reliability of a plain radiographic method compared to CT-scanogram. Skeletal Radiol. 2012;41:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | Ng VY, Kean JR, Glassman AH. Limb-length discrepancy after hip arthroplasty. J Bone Joint Surg Am. 2013;95:1426-1436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Loughenbury FA, McWilliams AB, Stewart TD, Redmond AC, Stone MH. Hip surgeons and leg length inequality after primary hip replacement. Hip Int. 2019;29:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Shemesh SS, Robinson J, Keswani A, Bronson MJ, Moucha CS, Chen D. The Accuracy of Digital Templating for Primary Total Hip Arthroplasty: Is There a Difference Between Direct Anterior and Posterior Approaches? J Arthroplasty. 2017;32:1884-1889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Thorne TJ, Nishioka ST, Andrews SN, Mathews KA, Nakasone CK. Comparison of Component Placement Accuracy Using Two Intraoperative Fluoroscopic Grid Technologies During Direct Anterior Total Hip Arthroplasty. J Arthroplasty. 2020;35:3601-3606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Austin DC, Dempsey BE, Kunkel ST, Torchia MT, Jevsevar DS. A comparison of radiographic leg-length and offset discrepancies between 2 intraoperative measurement techniques in anterior total hip arthroplasty. Arthroplast Today. 2019;5:181-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Sykes A, Hill J, Orr J, Humphreys P, Rooney A, Morrow E, Beverland D. Patients' perception of leg length discrepancy post total hip arthroplasty. Hip Int. 2015;25:452-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | O'Brien S, Kernohan G, Fitzpatrick C, Hill J, Beverland D. Perception of imposed leg length inequality in normal subjects. Hip Int. 2010;20:505-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Hofmann AA, Skrzynski MC. Leg-length inequality and nerve palsy in total hip arthroplasty: a lawyer awaits! Orthopedics. 2000;23:943-944. [PubMed] |
| 12. | Herisson O, Felden A, Hamadouche M, Anract P, Biau DJ. Validity and Reliability of Intraoperative Radiographs to Assess Leg Length During Total Hip Arthroplasty: Correlation and Reproducibility of Anatomic Distances. J Arthroplasty. 2016;31:2784-2788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Lecoanet P, Vargas M, Pallaro J, Thelen T, Ribes C, Fabre T. Leg length discrepancy after total hip arthroplasty: Can leg length be satisfactorily controlled via anterior approach without a traction table? Orthop Traumatol Surg Res. 2018;104:1143-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Whitehouse MR, Stefanovich-Lawbuary NS, Brunton LR, Blom AW. The impact of leg length discrepancy on patient satisfaction and functional outcome following total hip arthroplasty. J Arthroplasty. 2013;28:1408-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Keršič M, Dolinar D, Antolič V, Mavčič B. The impact of leg length discrepancy on clinical outcome of total hip arthroplasty: comparison of four measurement methods. J Arthroplasty. 2014;29:137-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Beswick A, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of Prospective studies in unselected patients. BMJ open 2012; 2: e000435. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 866] [Cited by in RCA: 1005] [Article Influence: 77.3] [Reference Citation Analysis (0)] |
| 17. | El Bitar YF, Stone JC, Jackson TJ, Lindner D, Stake CE, Domb BG. Leg-Length Discrepancy After Total Hip Arthroplasty: Comparison of Robot-Assisted Posterior, Fluoroscopy-Guided Anterior, and Conventional Posterior Approaches. Am J Orthop (Belle Mead NJ). 2015;44:265-269. [PubMed] |
| 18. | De Silva T, Punnoose J, Uneri A, Mahesh M, Goerres J, Jacobson M, Ketcha MD, Manbachi A, Vogt S, Kleinszig G, Khanna AJ, Wolinksy JP, Siewerdsen JH, Osgood G. Virtual fluoroscopy for intraoperative C-arm positioning and radiation dose reduction. J Med Imaging (Bellingham). 2018;5:015005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Goytia RN, Jones LC, Hungerford MW. Learning curve for the anterior approach total hip arthroplasty. J Surg Orthop Adv. 2012;21:78-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Masonis J, Thompson C, Odum S. Safe and accurate: learning the direct anterior total hip arthroplasty. Orthopedics. 2008;31. [PubMed] |
| 21. | Ji W, Stewart N. Fluoroscopy assessment during anterior minimally invasive hip replacement is more accurate than with the posterior approach. Int Orthop. 2016;40:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Jennings JD, Iorio J, Kleiner MT, Gaughan JP, Star AM. Intraoperative Fluoroscopy Improves Component Position During Anterior Hip Arthroplasty. Orthopedics. 2015;38:e970-e975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 23. | James CR, Peterson BE, Crim JR, Cook JL, Crist BD. The Use of Fluoroscopy During Direct Anterior Hip Arthroplasty: Powerful or Misleading? J Arthroplasty. 2018;33:1775-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Beamer BS, Morgan JH, Barr C, Weaver MJ, Vrahas MS. Does fluoroscopy improve acetabular component placement in total hip arthroplasty? Clin Orthop Relat Res. 2014;472:3953-3962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 25. | Connolly KP, Kamath AF. Direct anterior total hip arthroplasty: Comparative outcomes and contemporary results. World J Orthop. 2016;7:94-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 54] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 26. | Bingham JS, Spangehl MJ, Hines JT, Taunton MJ, Schwartz AJ. Does Intraoperative Fluoroscopy Improve Limb-Length Discrepancy and Acetabular Component Positioning During Direct Anterior Total Hip Arthroplasty? J Arthroplasty. 2018;33:2927-2931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 27. | Carlson VR, Elliott IS, DeKeyser GJ, Pelt CE, Anderson LA, Gililland JM. Are We Being Fooled by Fluoroscopy? J Arthroplasty. 2021;36:1799-1803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |