Published online Jan 18, 2021. doi: 10.5312/wjo.v12.i1.14
Peer-review started: August 5, 2020
First decision: November 4, 2020
Revised: November 4, 2020
Accepted: November 12, 2020
Article in press: November 12, 2020
Published online: January 18, 2021
Processing time: 156 Days and 4.6 Hours
In press-fit total hip arthroplasty (THA) ceramic-on-ceramic (CoC) bearings are a potential for overcoming the wear that is seen in ceramic-on-polyethylene (CoPE) bearings, and can lead to wear-induced osteolysis, resulting in loosening of the implant. However, CoC bearings show disadvantages as well, such as squeaking sounds and being more fragile, which can cause ceramic head or liner fracture. Because comparative long-term studies are limited, the objective of this study was to determine the long-term difference in wear, identify potential predictive factors for wear, investigate radiological findings such as osteolysis, and evaluate clinical functioning and complications between these bearings.
To determine 10-year differences in wear, predictive factors for wear, and investigate radiological findings and clinical functioning between CoC and CoPE.
This observational prospective single-center cohort study with a 10-year follow-up includes a documented series of elective THAs. Primary outcome was wear measured by anteroposterior (AP) radiographs. Secondary outcomes were potential predictive factors for wear, complications during follow-up, Harris hip score (HHS), and radiological findings such as presence of radiolucency, osteolysis, atrophy, and hypertrophy around the cup. Due to the absence of wear in the CoC group, stratified analysis to identify risk factors for wear was only performed in the CoPE group by use of univariate linear regression analysis. HHS was expressed as a change from baseline and the association with bearing type was assessed by use of multivariate linear regression analysis, adjusted for potential confounders.
A total of 17 CoPE (63.0%) and 25 CoC (73.5%) cases were available for follow-up and showed a linear wear of respectively 0.130 mm/year (range 0.010; 0.350) and 0.000 mm/year (range 0.000; 0.005), which was significant (P < 0.001) between both groups. Wear always occurred in the cranial direction. Cup inclination was the only predictive factor for polyethylene (PE) wear. No dislocations, ceramic head, or liner fractures were seen. The HHS showed a mean change from baseline of 37.1 points (SD 18.5) in the CoPE group and 43.9 (SD 17.0) in the CoC group. This crude difference of 6.8 (range -5.2; 18.7) in favor of the CoC group was not significant (P = 0.26) and was not significant when adjusted for age, gender, and diagnosis either (P = 0.99). No significant differences in complications and radiological findings were seen between groups.
CoC bearing shows lower wear rates compared to CoPE at 10-year follow-up with cup inclination as a predictive factor for wear and no differences in complications, HHS, and radiological findings.
Core Tip: Polyethylene wear of the acetabular insert can cause osteolysis and aseptic loosening of the implant in total hip arthroplasty. Ceramic-on-ceramic (CoC) bearing can overcome this problem, but comparative long-term data between ceramic-on-polyethylene (CoPE) and CoC are limited. This 10-year follow-up study showed higher wear rates in CoPE with cup inclination as a predictive factor for wear. No differences in complications, radiological findings, and clinical scores were seen. To confirm the potential benefits of CoC bearing focusing on wear and survival rates of the implant, more long-term data are needed.
- Citation: van Loon J, Hoornenborg D, van der Vis HM, Sierevelt IN, Opdam KT, Kerkhoffs GM, Haverkamp D. Ceramic-on-ceramic vs ceramic-on-polyethylene, a comparative study with 10-year follow-up. World J Orthop 2021; 12(1): 14-23
- URL: https://www.wjgnet.com/2218-5836/full/v12/i1/14.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i1.14
Total hip arthroplasty (THA) is considered the operation of the century, but the search for the ideal articulation is still a point of discussion[1]. Several bearing surfaces have been developed in the past to reduce causes for revision. Polyethylene (PE) or highly cross-linked PE (HXLPE) inlay combined with a ceramic head still remains the option of choice[2]. Therefore, the use of a ceramic-on-polyethylene (CoPE) articulation increased with almost 20% in the last decade up to 63.4% of all THAs as seen in the Dutch Arthroplasty Register in 2019[3].
Wear rates of PE are widely investigated, since wear-induced osteolysis resulting in aseptic loosening still remains one of the main causes of late revision[4,5]. The threshold of 0.05 mm/year was eventually stated to eliminate osteolysis, but recent long-term results showed that even wear rates below this threshold in both PE and HXLPE are associated with osteolysis[6,7]. Ceramic-on-ceramic (CoC) bearings are a potential to overcome this problem, with lower wear rates and incidence of osteolysis than CoPE[8]. However, CoC bearings show disadvantages as well, such as a squeaking sound and being more fragile, which can cause fracture of both the head and the inlay and makes revision THA challenging[9,10].
Comparative long-term studies are needed to confirm if the aforementioned disadvantages of both bearings will be reflected in accompanying revision rates, clinical functioning, and radiological findings over time. Recent systematic reviews have shown that more data and especially more research focused on long-term are required to clarify clinical advantages of both bearings[11,12].
The objective of this study was to determine the long-term difference in wear, identify potential predictive factors for wear, investigate radiological findings such as osteolysis, and evaluate clinical functioning and complications between CoC bearing vs CoPE in THA when using the same implants with a 10 years follow-up.
Our hypotheses were that CoPE would show higher wear rates than CoC and no differences would be observed in radiological findings, clinical functioning and complications.
No ethical approval was needed for this observational prospective cohort study because this documented series was part of the normal follow-up of elective THAs. Reporting was done in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement. This research was conducted according to the Declaration of Helsinki.
This observational prospective single center cohort study with 10-year follow-up included a documented series of elective THAs performed between December 2003 and December 2004 comparing the EP-FIT PLUS press-fit cup system with ceramic insert (BIOLOX delta, Smith and Nephew) to standard PE acetabular inserts (Standard REXPOL, Smith and Nephew) with similar ceramic head (BIOLOX delta, Smith and Nephew) articulation. No randomization was performed in this study. The choice between PE or ceramic insert depended on patient characteristics and the experienced orthopedic surgeons’ preferences. All patients included were seen in a standard follow-up scheme with X-rays at baseline, 3, 12, 36, 60, and 120 mo post-operatively. After surgery, a standard postoperative rehabilitation protocol under guidance of a physical therapist consisted of immediate weightbearing and crutches for 6 wk. All outcomes were analyzed by a reviewer and checked by a second researcher who were both not involved in the selection, surgery, and follow-up process.
All indications for THA included in this study were primary osteoarthritis (OA), degeneration due to rheumatoid arthritis or other inflammatory arthritis, avascular necrosis and hip dysplasia. Patients were included after completing verbal informed consent. Patients with secondary OA due to trauma, infection of the hip, osteoporosis or a prior osteotomy or arthroplasty were excluded from this study. No a priori power analysis was performed.
All THAs were performed at Slotervaart Medical Center by experienced orthopedic surgeons using a straight lateral approach under standard antibiotic prophylaxis. The surgical approach was according to the surgical technique described by the manufacturer of the implants. The same uncemented acetabular cup (EP-FIT PLUS, Smith and Nephew) was used in all patients. This cup is an equatorial flattened press-fit cup design with an open porous titanium vacuum plasma coating to increase roughness, with initial fixation by 2%-3% oversizing. A non-cemented Zweymuller titanium rectangular tapered shape femoral stem (SL-PLUS, Smith and Nephew) was used as femur component in all cases in combination with a ceramic head articulation (BIOLOX delta, Smith and Nephew). A 32 mm and 28 mm head were respectively used in CoC and CoPE bearing. The liner being used was either a ceramic insert (BIOLOX delta, Smith and Nephew) or a standard PE acetabular insert (Standard PE, Smith and Nephew). Both the ceramic head and liner are made of a zirconia toughened alumina ceramic alloy, a fourth-generation ceramic material. The aimed leg length and femoral offset was measured accordingly to be identical to the contralateral side.
Patient demographics were recorded at baseline, including age, gender, body mass index (BMI), indication for surgery (primary OA or other diagnosis), and operation side. Information regarding the operation was recorded as well including articulation, head size, and cup inclination in degrees on direct post-operative radiographs. Perioperative and complications during follow-up like ceramic articulation fractures, squeaking and dislocations were directly registered.
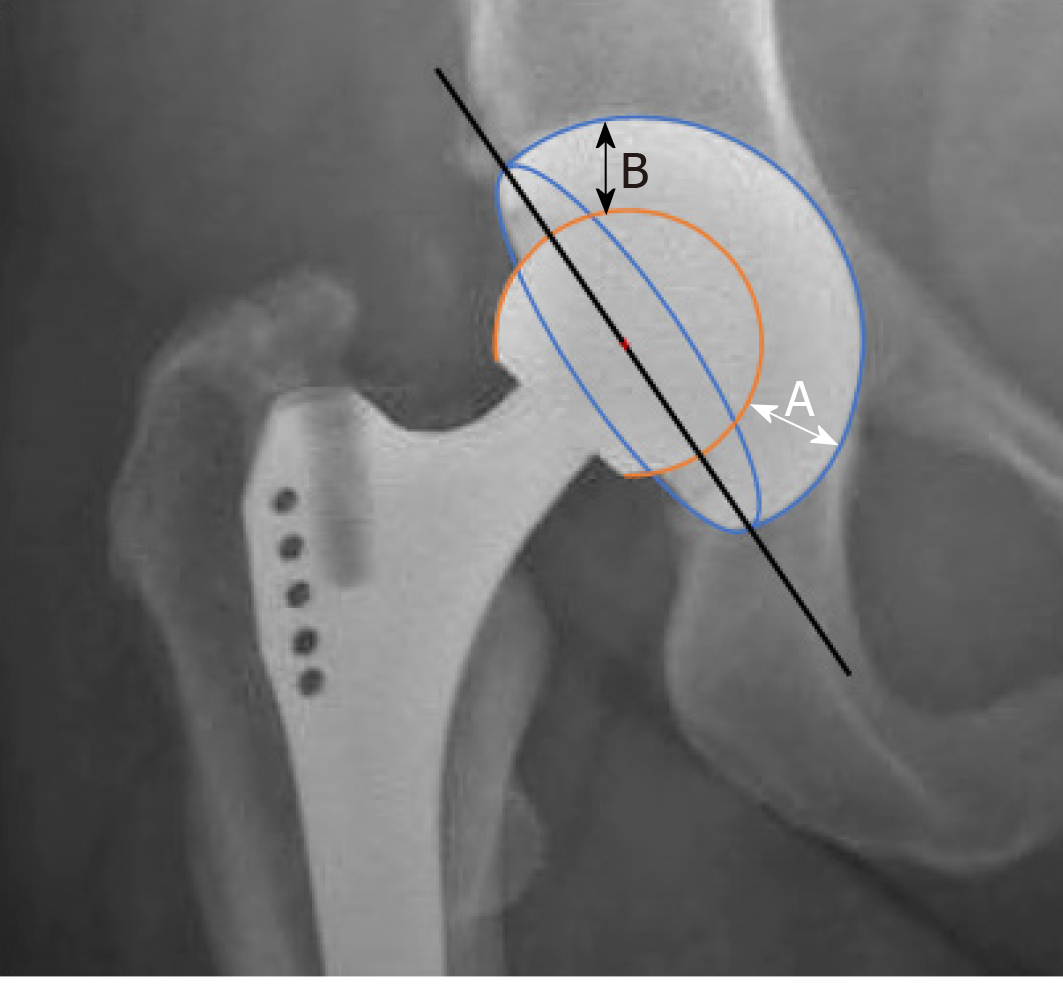
The primary outcome was wear in mm/year measured by an independent orthopedic surgeon, by consecutive radiography using standard weightbearing anterior-posterior radiographs. By using the penetration and the size of the head, the thickness of the inlay was calculated. The method being used as demonstrated in Figure 1, is widely used and first described and validated by Charnley et al[13]. The width of the narrowest part of the inlay in the proximal weightbearing region (B) was subtracted from the widest part in the distal non-weightbearing area (A) and halved. With this formula, wear = (A – B)/2, wear was calculated as cranial migration in mm. These outcomes were used to calculate linear wear rates in mm/year. As an example, if no wear occurs, the thickness of the inlay is the same in all directions. Hereby the difference between the measurement of A and B is zero, meaning that there is no cranial migration and hereby no wear. If wear increases and more cranial migration is seen, the measurement of B will become lower and A will increase due to a wider distal part, resulting in a greater difference between both values (Figure 1). As a secondary outcome, potential predictive factors for wear such as gender, age, operation side, BMI, diagnosis (primary OA vs other), cup size, and cup inclination were determined. The Harris hip score (HHS) was used as a clinical questionnaire to measure patient reported outcomes[14]. Radiographs were evaluated by two researchers to determine presence of radiolucency, osteolysis, atrophy, and hypertrophy around the cup in Zones I-III according to DeLee et al[15].
Statistical analyses were performed with Statistical Package for Social Sciences (SPSS) version 26.0 (IBM Corp., Armonk, New York, United States). Normally distributed continuous variables are stated as mean with standard deviation (SD) and tested by use of Student’s t-test. In case of non-normality medians with interquartile ranges are presented and a Mann-Whitney U test was used to asses for significant differences between both groups. Categorical data were compared by use of chi-squared tests. Due to the absence of wear in the CoC group, stratified analysis to identify risk factors for wear was only performed in the CoPE group by use of univariate linear regression analyses. HHS was expressed as a change from baseline and the association with bearing type was assessed by use of multivariate linear regression analysis, adjusted for potential confounders (i.e. age, sex, and diagnosis). Differences were stated significant if P values were less than 0.05. Complications and radiological findings were expressed as frequencies with percentage. All statistical methods in this study were done by a biomedical statistical expert (Inger N Sierevelt).
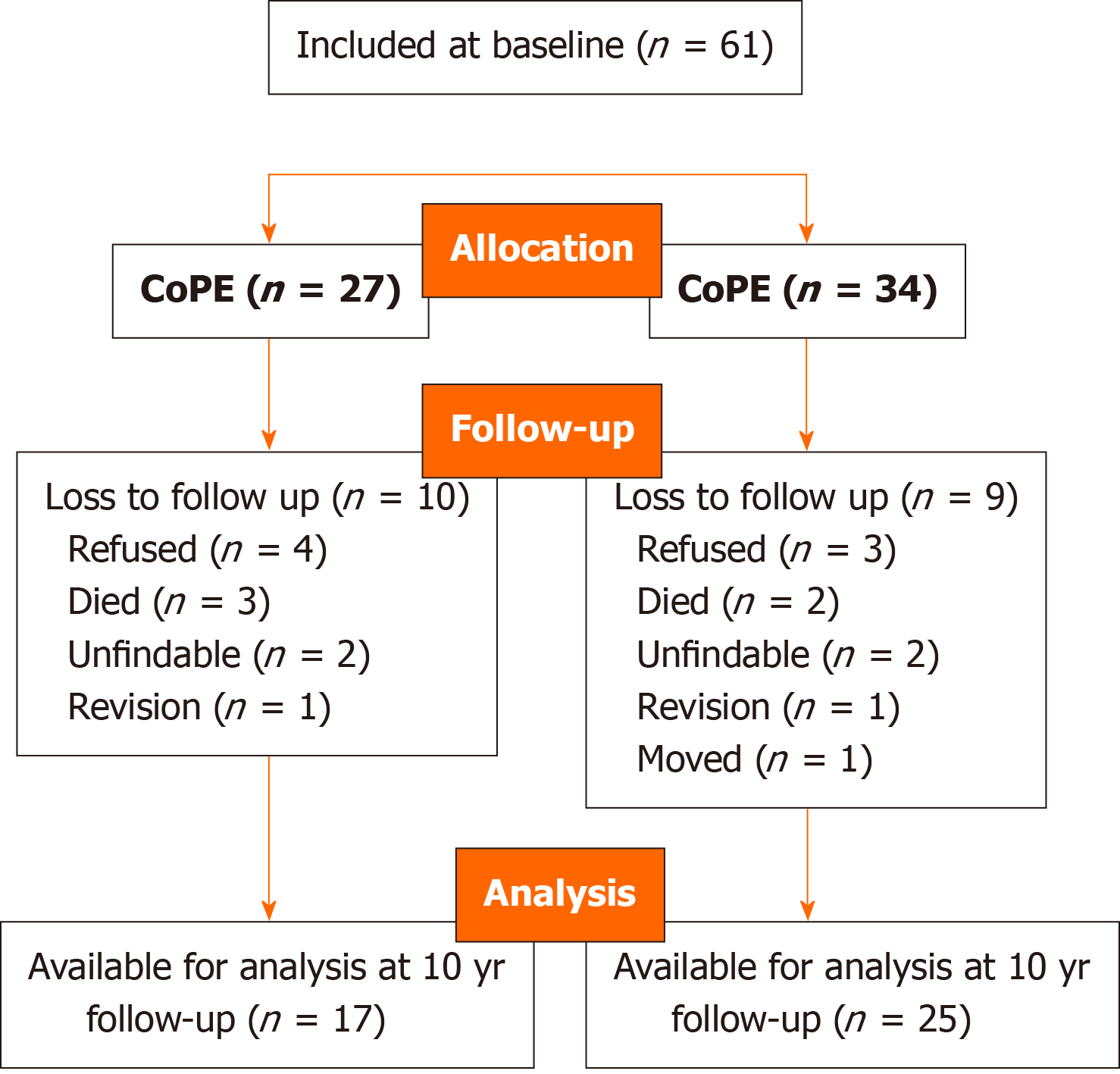
A total of 61 patients receiving THAs were included in this study at baseline (Figure 2). A significant difference in age and distribution of diagnosis (primary OA vs other) between both groups was observed (Table 1). A total of 17 CoPE (63.0%) and 25 CoC (73.5%) cases were available for 10-year follow-up. Intra-operative trochanteric fracture occurred in one case (4%) in the CoPE group and two (6%) in the CoC group, and were treated with a trochanteric wire. Delayed wound healing was seen in two (8%) and four (13%) patients in the CoPE and CoC group, respectively. Temporary peroneal nerve injury was observed in the CoPE group in two cases (7.4%). During follow-up, one periprosthetic joint infection (3%) was seen in the CoC group, which was initially treated with lavage and antibiotics; however, removal of the implant was done elsewhere after 3 years of follow-up. Femoral component loosening was the reason for one revision in both groups, treated by revision of the stem and inlay elsewhere in the CoC case and in our clinic in the CoPE patient. No dislocations, squeaking, and fracture of the ceramic liner were observed. A total of two revisions were planned in the CoPE group after the 10-year follow-up due to complaints combined with excessive wear. All complications showed no significant differences between both groups.
| CoPE, n = 27 (100%) | CoC, n = 34 (100%) | P value | |
| Female gender, n (%) | 21 (78%) | 22 (65%) | 0.27 |
| Right side, n (%) | 19 (76%) | 17 (50%) | 0.11 |
| Diagnosis, n (%) | 0.01 | ||
| Primary OA | 23 (85%) | 19 (56%) | |
| Other | 4 (15%) | 15 (44%) | |
| Age, in years, mean (SD) | 64.2 (5.3) | 55.7 (8.5) | < 0.001 |
| BMI, in kg/m2 mean (SD) | 27.6 (4.1) | 26.9 (4.1) | 0.52 |
| Cup size in mm, mean (SD) | 52.1 (3.4) | 53.6 (3.5) | 0.10 |
| Inclination cup in degrees, mean (SD) | 46.8 (6.7) | 44.6 (5.0) | 0.22 |
| HHS, mean (SD) | 50.2 (13.3) | 47.5 (13.4) | 0.44 |
After 10 years of follow-up, the median linear wear of CoPE and CoC bearing was 0.130 mm/year (range 0.010; 0.350) and 0.000 mm/year (range 0.000; 0.005), respectively. Wear always occurred in the cranial direction. In two patients in the CoC group, wear of 0.05 mm was measured, in all other cases, no wear was observed. The difference in wear between both groups was significant (P < 0.001).
The results of the stratified analysis to identify risk factors for wear in the CoPE group are shown in Table 2. Increased cup inclination was the only predictive factor for PE wear in CoPE bearing.
| Potential predictive factors for PE wear | Beta-coefficient (95%CI) | P value |
| Gender | 0.06 (-1.18; 1.29) | 0.93 |
| Age | -0.01 (-0.10; 0.08) | 0.82 |
| Operation side | -0.40 (-1.53; 0.73) | 0.46 |
| BMI | -0.05 (-0.20; 0.10) | 0.46 |
| Diagnosis, primary OA vs other | 1.10 (-0.42; 2.61) | 0.14 |
| Cup size | -0.06 (-0.23; 0.12) | 0.52 |
| Cup inclination | 0.08 (0.02; 0.15) | 0.02 |
The HHS score showed a mean change from baseline of 37.1 points (SD 18.5) in the CoPE group and 43.9 (SD 17.0) in the CoC group. This crude difference of 6.8 (range -5.2; 18.7) in favor of the CoC group was not significant (P = 0.26). When adjusted for age, gender, and diagnosis (primary OA vs other), a mean difference of -0.02 (range -14.7; 14.7) was seen, which was not significant either (P = 0.99).
The radiological findings in the periacetabular cup zones are shown in Table 3. These outcomes showed no significant differences between both groups.
| CoPE, n = 17 | CoC, n = 25 | |||||
| Zones | I | II | III | I | II | III |
| Radiolucent lines | 0 | 0 | 0 | 0 | 0 | 0 |
| Osteolysis cup | 0 | 1 (6%) | 0 | 2 (8%) | 3 (12%) | 0 |
| Atrophy | 2 (12%) | 3 (18%) | 0 | 5 (19%) | 5 (19%) | 0 |
| Hypertrophy | 0 | 0 | 0 | 0 | 0 | 0 |
The main finding of this observational prospective cohort study of 61 THAs with 17 CoPE and 25 CoC cases available for 10-year follow-up was a significantly different degree of wear between the CoPE and CoC, with values of 0.130 mm/year (range 0.010; 0.350) and 0.000 mm/year (range 0.000; 0.005), respectively in the cranial direction. Comparable significant differences in wear rates were seen in the literature in both the short and long-term[8,16]. Conventional PE inlays have been improved by cross-linking to improve wear rates, but CoC bearings still show the lowest wear rates[17-19]. Therefore, long-term follow-up is required to assess whether differences in wear will result in different survival rates. Although survival was not the focus of our study, to the best of our knowledge, the literature has only one comparative study with 12.6 years of follow-up showing no differences between CoC and CoHXLPE[18]. Studies that only focused on CoPE and CoHXLPE showed long-term survival rates of 86% and 100%, respectively, at 13 years and 88.3% and 93.8%, respectively, at 16 years[20,21]. Long-term studies that focused only on CoC showed divergent survival rates, with a 15-year follow-up study showing a survival rate of 92%, whereas another 20 years of follow-up showed a survival rate of 99.7%[22,23]. Our wear rate results combined with the revision rates in the literature indicated a possible advantage of ceramic coupling over PE, which needs to be confirmed with longer follow-up studies of at least 20 years.
The low wear and revision rates of CoC in the longer term become highly relevant since a rise in prevalence of THA and a shift to younger age is seen over the last decades[24]. Moreover, our study shows that patients receiving CoC articulation were significantly younger. Since life expectancy is still increasing worldwide, further research is needed to show if CoC can improve the longevity of THAs[25].
Our study showed that a higher inclination angle of the cup is a significant risk factor for wear. The same results are seen in the literature, with inclination angles above 45 degrees[26-28]. Since the mean angle of CoPE in our group was above this angle, it supports that acetabular positioning is highly important to reduce wear of CoPE.
In addition, inclination angles above 45 degrees are related to the higher incidence of squeaking in CoC[29,30]. In the literature, the incidence of squeaking is significantly higher in CoC than CoPE and varies between 0.5% and 20% and can influence the satisfaction of patients[11,12,31]. Although the mean angle of inclination in CoC in our study was just below the 45 degrees, no squeaking was reported.
Since the introduction of CoC, fracture of the ceramic, which was seen more often than in CoPE, was one of the greatest concerns against using this articulation[11,12]. A recent long-term meta-analysis showed that improvement of the ceramic over time led to lower fracture rates[32]. Additionally, in the literature, fourth-generation ceramic bearings showed no ceramic fracture when compared to third-generation CoC[33]. Since we used a fourth-generation ceramic bearing, this might be a reason that no head or liner fractures occurred in our study[32,33].
Another complication that influences long-term outcomes is dislocation, which can be caused by wear and malpositioning[34,35]. In the literature, a trend is seen in favor to CoC over CoPE[11,12]. Although no dislocations were seen in our study, the higher wear rate and wider angles of inclination presented in CoPE can indicate an increased risk of dislocation, which might become significant in the longer term.
In our study, no differences in radiological findings such as osteolysis were seen, which was supported by recent systematic reviews comparing CoC and CoPE[11,12]. Longer follow-up is needed to see if differences in osteolysis will occur over time.
No significant differences in clinical outcomes on the HHS were seen in our study. Since comparable scores on the HHS were seen in systematic reviews, there is no preference for one of the bearings based on functioning[11,12].
Finally, ceramic inserts are more expensive than PE, which might be an important issue in decision making in modern healthcare systems with an increasing focus on healthcare costs. Beaupre et al[36] stated that the costs of ceramic inserts were three times higher. To the best of our knowledge, no cost-analyses are performed in the literature between CoC and Co(HXL)PE. Long-term analysis needs to clarify if differences in outcomes, complication, and revision rates are cost-effective to the costs of both bearings.
A strength of our study is that we provided comparative results of a fourth-generation ceramic bearing, which are limited in the literature including wear, clinical, and radiological results. A limitation of our study was that no randomization was performed, which can have consequences for the comparability of the groups and might give indication bias. Moreover, a high loss to follow-up was seen in this study. Wear measurements were done using standard AP radiographs, which is a valid method, but is subsidiary to radiostereometric analysis (RSA)[37]. For example, we measured wear in two cases of CoC, which might be an error. Finally, no HXLPE was used, which is currently preferred when using a CoPE bearing.
In this study, higher wear rates were observed in CoPE compared to CoC bearing in THA at the 10-year follow-up, with cup inclination as a predictive factor for wear for CoPE bearing, and no differences in complications, HHS, and radiological findings. More long-term comparative studies are needed to confirm potential benefits of CoC bearing, which might be the preference in THA focused on wear and survival rates, especially in younger patients.
Ceramic-on-ceramic (CoC) bearing in total hip arthroplasty (THA) is presumed to give lower wear rates in vivo, compared to ceramic-on-polyethylene (CoPE).
More in vivo long-term studies are needed in literature, to confirm potential benefits or disadvantages of CoC over CoPE.
The objective of this study was to determine the 10-year difference in wear, identify potential predictive factors for wear, investigate radiological findings such as osteolysis, evaluate clinical functioning and complications between CoC bearing vs CoPE when using the same implants.
An observational prospective single-center cohort study with 10-year follow-up of a documented series of elective THAs was performed with either a ceramic (BIOLOX delta, Smith and Nephew) or a standard PE acetabular insert (Standard REXPOL, Smith and Nephew) with a similar ceramic head (BIOLOX delta, Smith and Nephew) articulation.
Higher wear rates were observed in CoPE compared to CoC bearing after 10-year follow-up with cup inclination as a predictive factor for wear for CoPE bearing, and no differences in complications, Harris hip score, and radiological findings.
The potential benefit of CoC over CoPE at the 10-year follow-up is less wear with cup inclination as a predictive factor for wear, without differences in clinical or radiological outcomes.
Further investigation of wear, revision, and complication rates between CoC and CoPE, especially in the long-term, should be done, to confirm potential benefits of CoC over CoPE and to prove if it can improve the longevity of THAs. In addition, long-term analysis needs to clarify if differences in outcomes, complication, and revision rates are cost-effective to the costs of both bearings.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: The Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li J S-Editor: Gao CC L-Editor: Filipodia P-Editor: Xing YX
| 1. | Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1477] [Cited by in RCA: 1790] [Article Influence: 99.4] [Reference Citation Analysis (0)] |
| 2. | Haverkamp D. The latest information on total hip arthroplasty bearing surfaces. Minerva Ortop Traumatol. 2009;60:233-240. |
| 3. | Dutch National Arthroplasty Register (LROI) Annual Report. 2019. Available from: https://www.lroi-report.nl/previous-reports/online-lroi-report-2019. |
| 4. | McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty. A randomized controlled trial. J Bone Joint Surg Am. 2009;91:773-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 152] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 5. | Mori T, Tsukamoto M. Highly cross-linked polyethylene in total hip arthroplasty, present and future. Ann Jt. 2018;3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Broomfield JA, Malak TT, Thomas GE, Palmer AJ, Taylor A, Glyn-Jones S. The Relationship Between Polyethylene Wear and Periprosthetic Osteolysis in Total Hip Arthroplasty at 12 Years in a Randomized Controlled Trial Cohort. J Arthroplasty. 2017;32:1186-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17:649-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 492] [Cited by in RCA: 430] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 8. | Hernigou P, Zilber S, Filippini P, Poignard A. Ceramic-ceramic bearing decreases osteolysis: a 20-year study versus ceramic-polyethylene on the contralateral hip. Clin Orthop Relat Res. 2009;467:2274-2280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Howard DP, Wall PDH, Fernandez MA, Parsons H, Howard PW. Ceramic-on-ceramic bearing fractures in total hip arthroplasty: an analysis of data from the National Joint Registry. Bone Joint J. 2017;99-B:1012-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 10. | Yang CC, Kim RH, Dennis DA. The squeaking hip: a cause for concern-disagrees. Orthopedics. 2007;30:739-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Dong YL, Li T, Xiao K, Bian YY, Weng XS. Ceramic on Ceramic or Ceramic-on-polyethylene for Total Hip Arthroplasty: A Systemic Review and Meta-analysis of Prospective Randomized Studies. Chin Med J (Engl). 2015;128:1223-1231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Hu D, Yang X, Tan Y, Alaidaros M, Chen L. Ceramic-on-ceramic versus ceramic-on-polyethylene bearing surfaces in total hip arthroplasty. Orthopedics. 2015;38:e331-e338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Charnley J, Halley DK. Rate of wear in total hip replacement. Clin Orthop Relat Res. 1975;(112):170-179. [PubMed] |
| 14. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [PubMed] |
| 15. | DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;(121):20-32. [PubMed] |
| 16. | Amanatullah DF, Landa J, Strauss EJ, Garino JP, Kim SH, Di Cesare PE. Comparison of surgical outcomes and implant wear between ceramic-ceramic and ceramic-polyethylene articulations in total hip arthroplasty. J Arthroplasty. 2011;26:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Callary SA, Solomon LB, Holubowycz OT, Campbell DG, Munn Z, Howie DW. Wear of highly crosslinked polyethylene acetabular components. Acta Orthop. 2015;86:159-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Kim YH, Park JW, Kulkarni SS, Kim YH. A randomised prospective evaluation of ceramic-on-ceramic and ceramic-on-highly cross-linked polyethylene bearings in the same patients with primary cementless total hip arthroplasty. Int Orthop. 2013;37:2131-2137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Lewis PM, Al-Belooshi A, Olsen M, Schemitch EH, Waddell JP. Prospective randomized trial comparing alumina ceramic-on-ceramic with ceramic-on-conventional polyethylene bearings in total hip arthroplasty. J Arthroplasty. 2010;25:392-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | de Steiger R, Lorimer M, Graves SE. Cross-Linked Polyethylene for Total Hip Arthroplasty Markedly Reduces Revision Surgery at 16 Years. J Bone Joint Surg Am. 2018;100:1281-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 21. | Hanna SA, Somerville L, McCalden RW, Naudie DD, MacDonald SJ. Highly cross-linked polyethylene decreases the rate of revision of total hip arthroplasty compared with conventional polyethylene at 13 years' follow-up. Bone Joint J. 2016;98-B:28-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 113] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 22. | Kim YH, Park JW, Kim JS. Long-Term Results of Third-Generation Ceramic-on-Ceramic Bearing Cementless Total Hip Arthroplasty in Young Patients. J Arthroplasty. 2016;31:2520-2524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Pitto R. Ceramic-on-ceramic total hip arthroplasty: long-term results in a national registry. Orthop Proceed. 2018;100-B:5-5. |
| 24. | Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am. 2015;97:1386-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 922] [Cited by in RCA: 1208] [Article Influence: 120.8] [Reference Citation Analysis (0)] |
| 25. | Roser M, Ritchie H, Ortiz-Ospina E. World Population Growth. Published online at OurWorldInDataorg 2013. Available from: https://ourworldindata.org/world-population-growth. |
| 26. | Bhaskar D, Rajpura A, Board T. Current Concepts in Acetabular Positioning in Total Hip Arthroplasty. Indian J Orthop. 2017;51:386-396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 27. | Little NJ, Busch CA, Gallagher JA, Rorabeck CH, Bourne RB. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467:2895-2900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 231] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 28. | Patil S, Bergula A, Chen PC, Colwell CW Jr, D'Lima DD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85-A Suppl 4:56-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 263] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 29. | Sariali E, Klouche S, Mamoudy P. Ceramic-on-ceramic total hip arthroplasty: is squeaking related to an inaccurate three-dimensional hip anatomy reconstruction? Orthop Traumatol Surg Res. 2014;100:437-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Walter WL, O'toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007;22:496-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 216] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 31. | Traina F, De Fine M, Di Martino A, Faldini C. Fracture of ceramic bearing surfaces following total hip replacement: a systematic review. Biomed Res Int. 2013;2013:157247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 32. | Yoon BH, Park JW, Cha YH, Won SH, Lee YK, Ha YC, Koo KH. Incidence of Ceramic Fracture in Contemporary Ceramic-on-Ceramic Total Hip Arthroplasty: A Meta-analysis of Proportions. J Arthroplasty 2020; 35: 1437-1443. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 33. | Kim SC, Lim YW, Jo WL, Park HW, Han SB, Kwon SY, Kim YS. Fourth-generation ceramic-on-ceramic THA results in improvements in midterm outcomes compared to third-generation THA but does not resolve noise problems: a cohort study of a single-hip system. BMC Musculoskelet Disord. 2019;20:263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 34. | Dargel J, Oppermann J, Brüggemann GP, Eysel P. Dislocation following total hip replacement. Dtsch Arztebl Int. 2014;111:884-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 35. | Lu Y, Xiao H, Xue F. Causes of and treatment options for dislocation following total hip arthroplasty. Exp Ther Med. 2019;18:1715-1722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 36. | Beaupre LA, Al-Houkail A, Johnston DWC. A Randomized Trial Comparing Ceramic-on-Ceramic Bearing vs Ceramic-on-Crossfire-Polyethylene Bearing Surfaces in Total Hip Arthroplasty. J Arthroplasty. 2016;31:1240-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 37. | Stilling M, Kold S, de Raedt S, Andersen NT, Rahbek O, Søballe K. Superior accuracy of model-based radiostereometric analysis for measurement of polyethylene wear: A phantom study. Bone Joint Res. 2012;1:180-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |