Published online Mar 18, 2020. doi: 10.5312/wjo.v11.i3.197
Peer-review started: September 16, 2019
First decision: October 13, 2019
Revised: November 3, 2019
Accepted: January 13, 2020
Article in press: January 13, 2020
Published online: March 18, 2020
Processing time: 182 Days and 14.2 Hours
Bone lesions can present the multi-displinary team with a challenge by way of diagnosis as some lesions share many radiological and histological characteristics. Giant cell tumours of the bone (GCTB) are relatively common, benign bone tumours. Aneurysmal bone cysts (ABC) are less common benign osteolytic lesions that are histologically similar to GCTBs but produce blood filled cavities. Both GCTBs and ABCs are locally aggressive and are typically found on meta-epiphyseal regions of long bones with pelvic tumours being less common.
A 17-year old female presented with atraumatic right groin pain and was initially diagnosed with a GCTB on the right superior pubic ramus of the pelvis. The patient was treated successfully with a wide excision, curettage and bone graft and underwent open reduction and internal fixation of the right hemi-pelvis. Following further intra-operative histological investigations, the lesion was diagnosed as an ABC.
This patient has had an uncomplicated post-operative course, has returned to comfortable weight bearing and will be reviewed for minimum 5 yr in the out-patient setting to monitor for reoccurrence.
Core tip: We hereby present the successful management of a young female who presented with atraumatic groin pain. This patient was ultimately diagnosed with an aneurysmal bone cyst of the superior pubic ramus and underwent wide-excision, curettage, bone grafting and open reduction internal fixation of her right hemi-pelvis. This patient is currently mobilising comfortably and is being monitored in the out-patient setting for recurrence.
- Citation: Downey C, Daly A, Molloy AP, O’Daly BJ. Atraumatic groin pain secondary to an aneurysmal bone cyst: A case report and literature review. World J Orthop 2020; 11(3): 197-205
- URL: https://www.wjgnet.com/2218-5836/full/v11/i3/197.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i3.197
Giant cell tumours of the bone (GCTB) are histologically benign neoplasms that account for approximately 20% of all benign bone tumours[1]. Aneurysmal bone cyst (ABC) are less common, expansile, osteolytic lesions that can produce blood filled cavities[2]. These entities can be difficult to diagnose and require radiological and histological investigations to differentiate one from the other. Although both benign, GCTBs and ABCs can be locally aggressive. They can both affect the entire skeleton, but they are more likely to occur in the metaphysis of long bones[1,2] . ABCs may be primary neoplasms or they may occur secondary to neoplasms such as giant cell tumours, osteosarcomas and chondroblastomas[3]. Management of GCTBs and ABCs are typically surgical with a combination of either intra-lesional curettage, wide resection and bone grafting employed depending on the location and extent of the neoplasm. We report the case of a 17-year old female with, what was primarily diagnosed as a giant cell tumour of the pelvis. The patient was treated surgically with wide excision, curettage and bone graft as well as open reduction and internal fixation of the right hemi-pelvis. Following analysis of intra-operative tissue specimens, the patient was diagnosed with an ABC following specialist histopathological input.
A 17-year old female presented to her general practitioner with a 4-mo history of pain in the right groin.
This symptom was initially described by the patient as similar to a groin strain previously experienced playing sports and the patient had discomfort on ambulation. There was no history of preceding trauma or sports injury. This pain progressed in severity and began to wake the patient at night. The patient had no associated history of fevers, rigors, shortness of breath, fatigue or weight loss.
The patient had no significant history of past illness.
This young female had a normal developmental history, had received all routine vaccinations and had a typical history of childhood infections. There was no significant family history of any medical conditions/illnesses.
On examination, the patient had non-irritable, normal range of motion of both hip joints. She mobilised with an antalgic gait and the pain increased on single leg stance using the right lower limb.
This patient had routine bloods including complete blood count, basic metabolic panel, c-reactive protein and erythrocyte sedimentation rate. These results did not reveal any abnormalities.
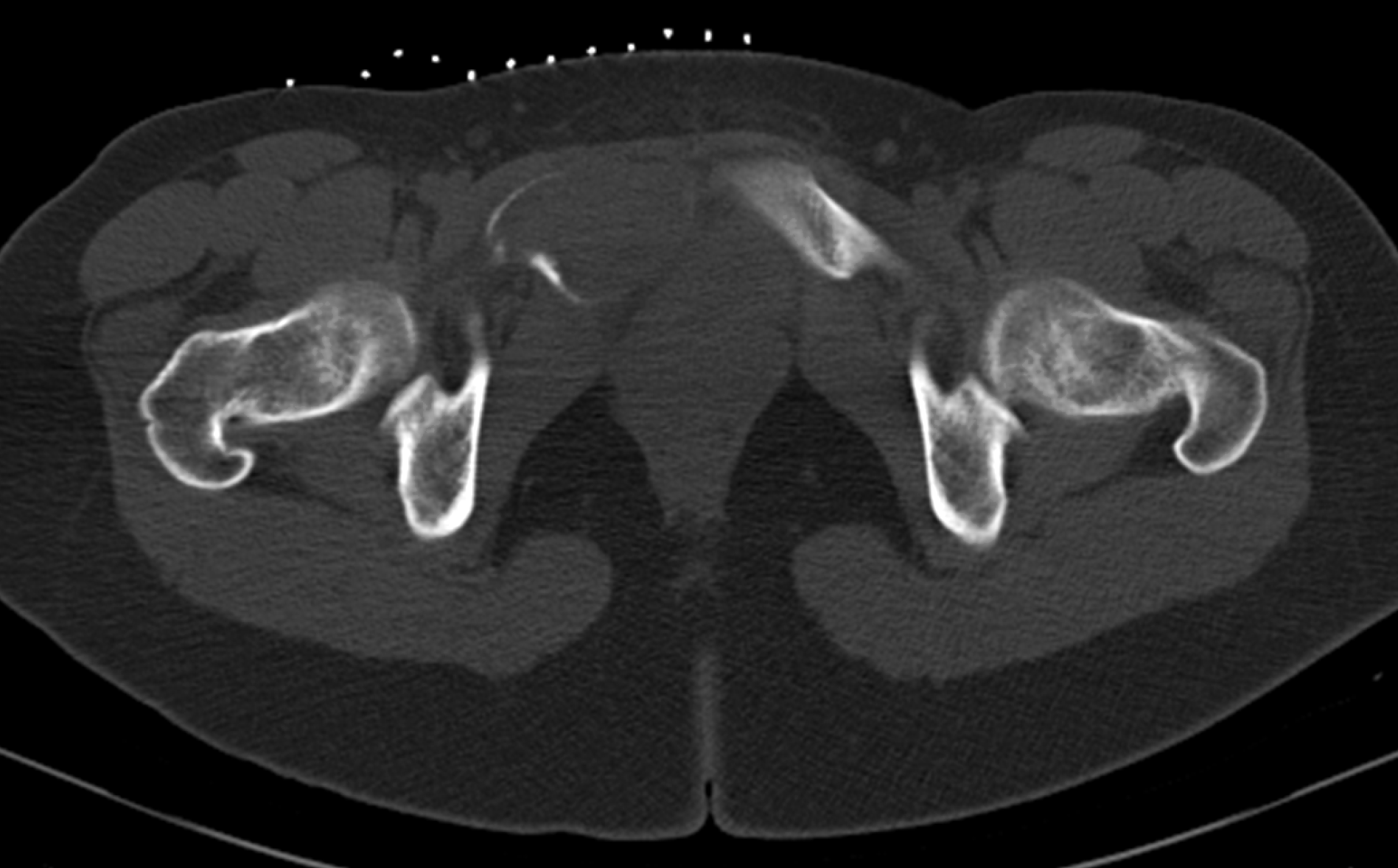
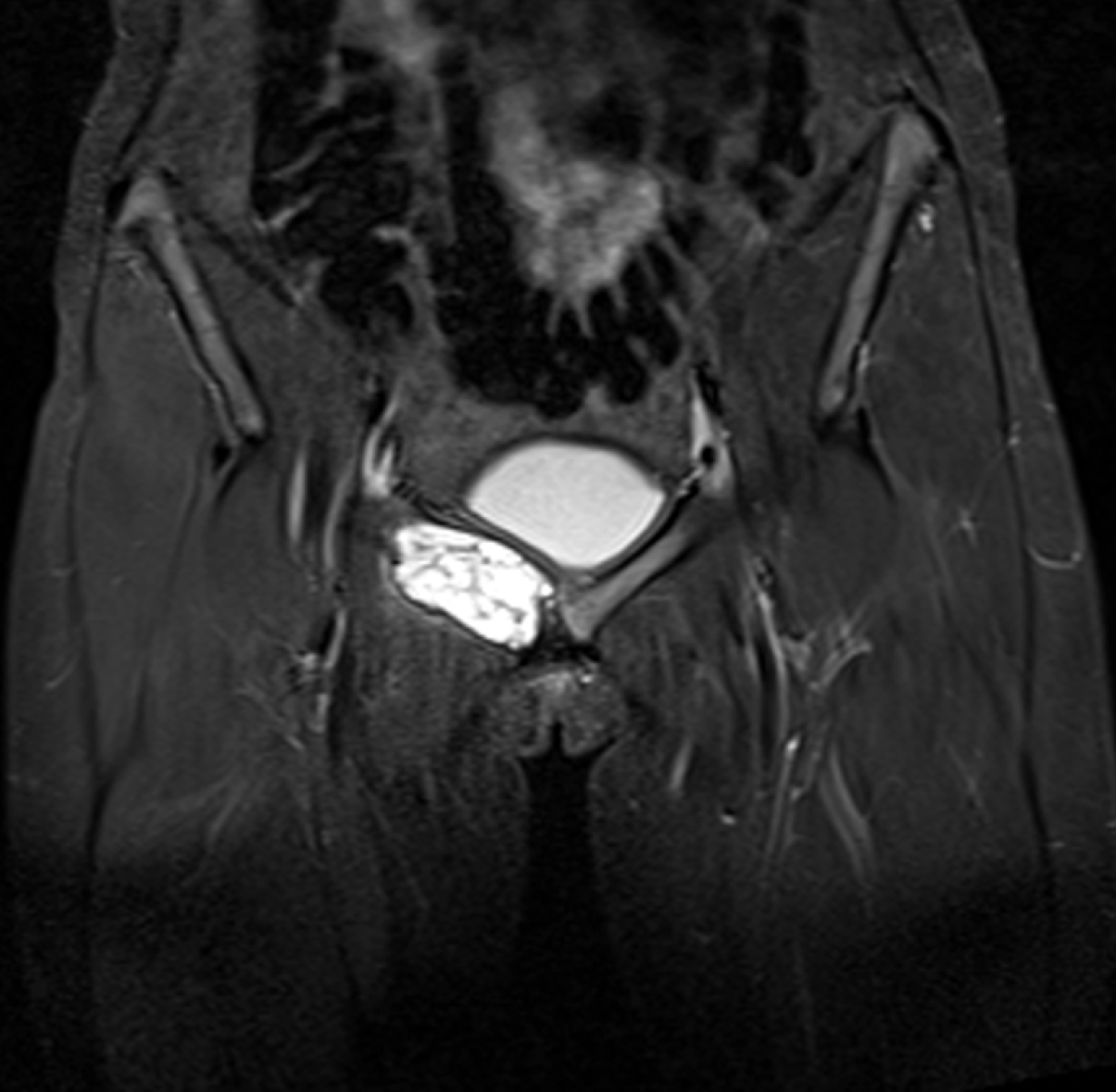
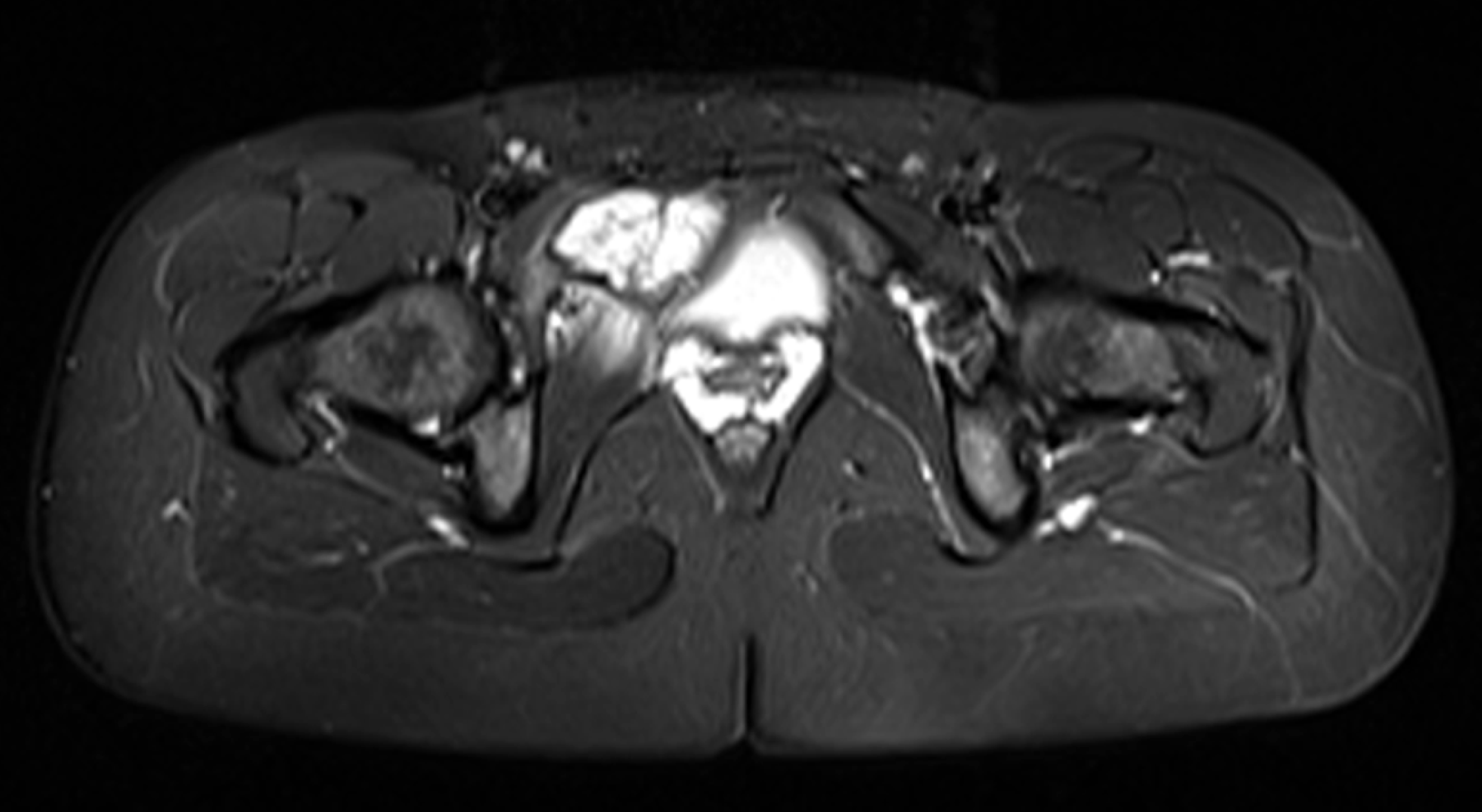
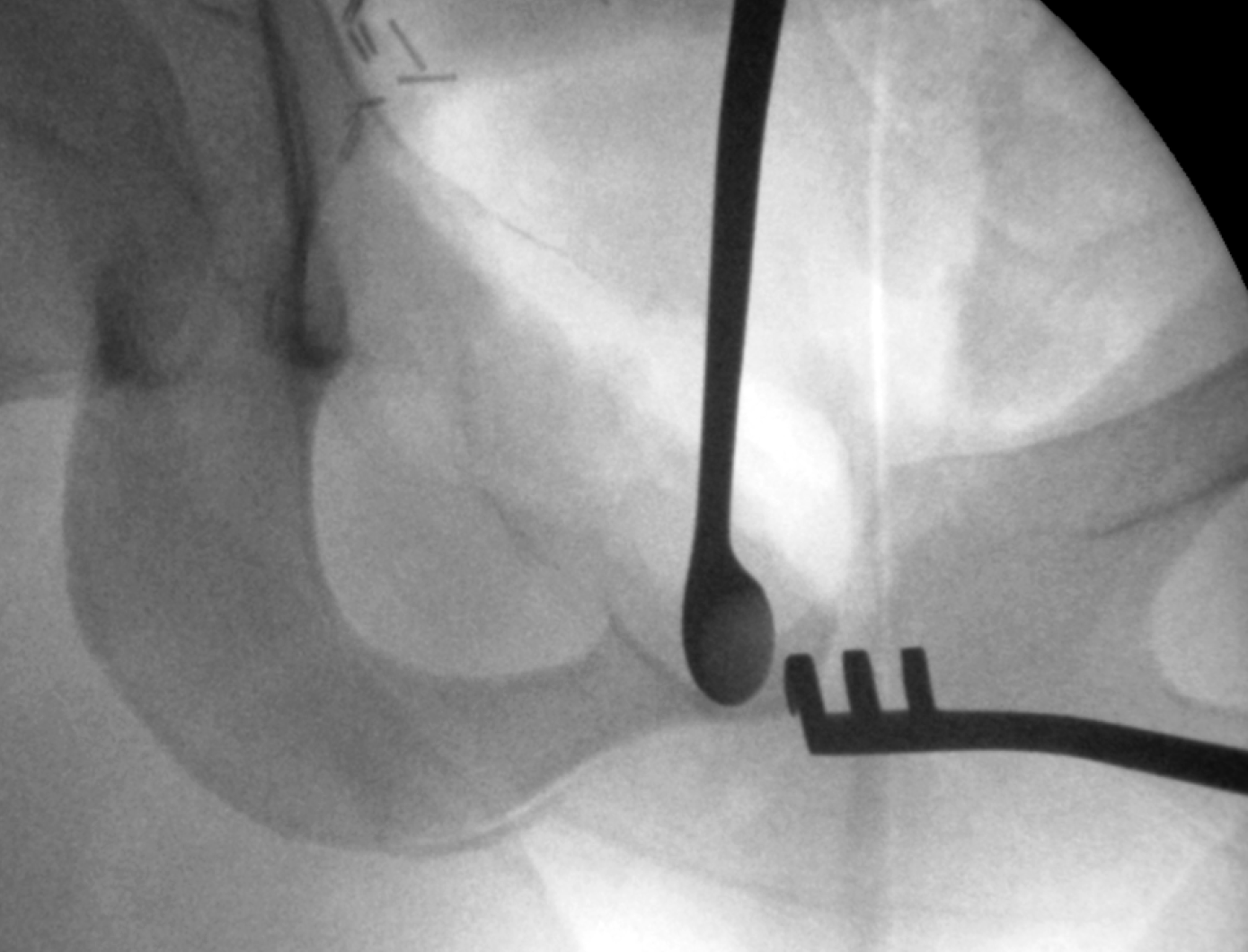
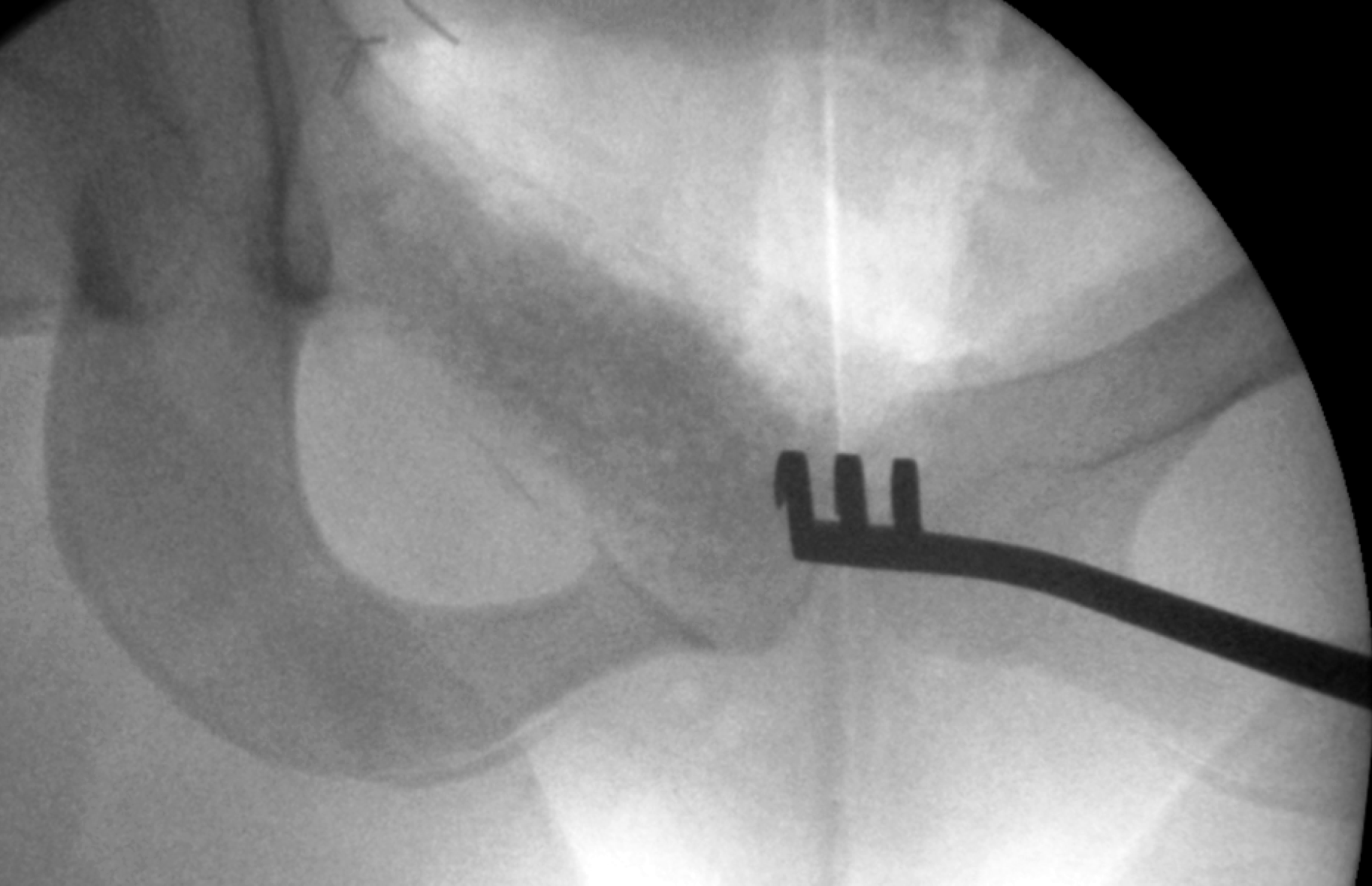
The patient had X-ray imaging of her pelvis (Figure 1, anterior osterior pelvis and Figure 2, frog-leg lateral right hip) which showed an aggressive osseous lesion in the right superior pubic ramus. The patient was referred for specialist orthopaedic opinion and a computed tomography-guided biopsy was undertaken (Figure 3). The patient subsequently had magnetic resonance imaging (Figures 4 and 5) which showed an expansile mass arising from the right parasymphyseal bone into the right superior pubic ramus. There was significant effacement and thinning of the adjacent cortex without bony destruction. Following interpretation of the above imaging and initial biopsy, the patient was preliminarily diagnosed with giant cell tumour of the right superior pubic ramus and following a multi-disciplinary team approach, the patient was scheduled for excision, curettage and grafting of the right superior pubic ramus and open reduction and internal fixation of the right hemi-pelvis.
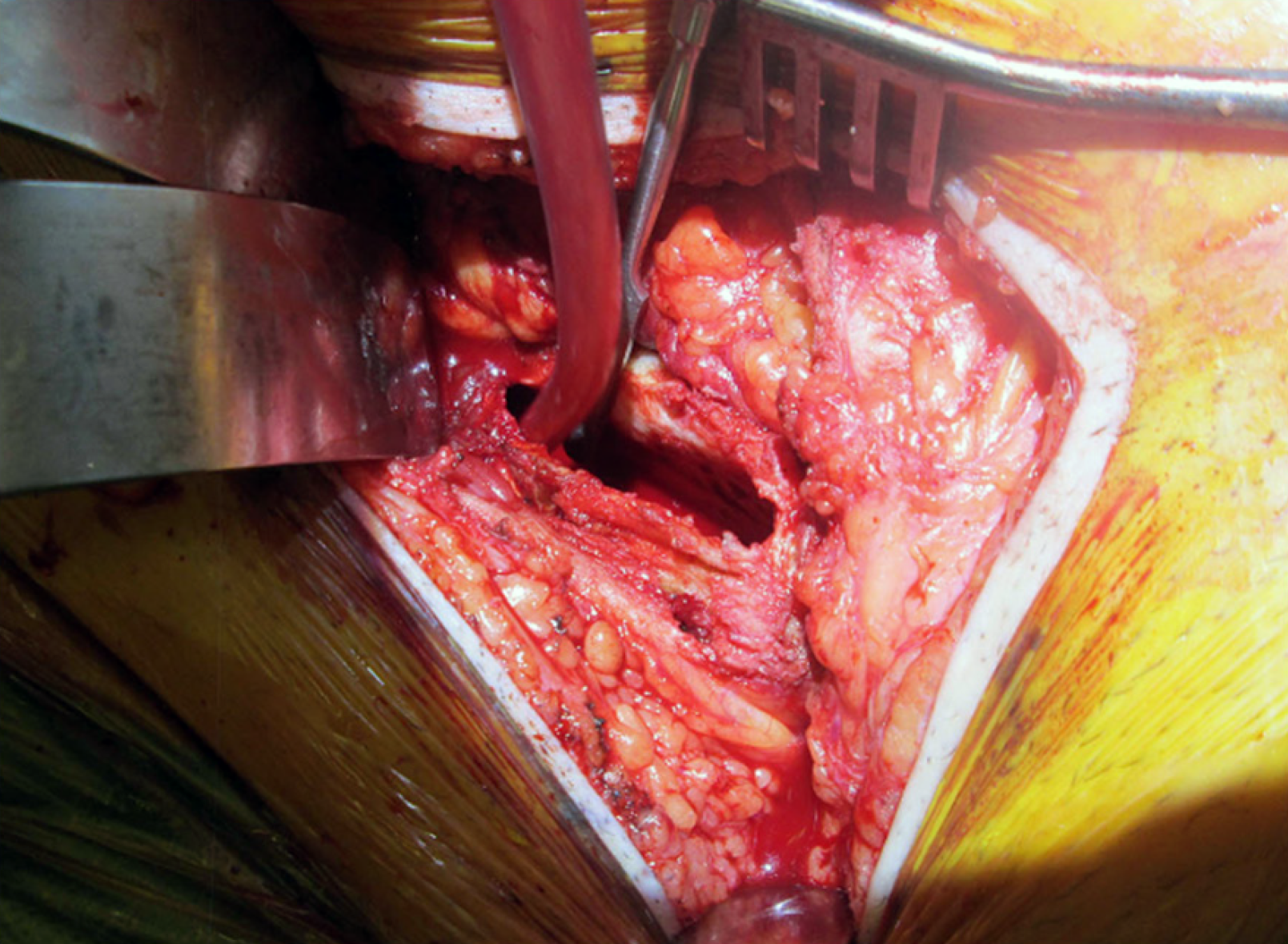
The patient was positioned supine and an approximately 10 cm Pfannenstiel incision was performed. The Anterior Intra-Pelvic approach was utilised to expose the right superior pubic ramus. The corona mortis vessel (anastomosis between the obturator and the external iliac or inferior epigastric arteries or veins) were visualised and ligated to optimise prophylactic management of haemostasis. This step assisted the surgical team in minimising intra-operative blood loss and following measurement of suction and swab weights, the estimated blood loss was < 300 ccs. The lesion was adequately exposed (Figure 6) and a window (approximately 1 cm × 5 cm) was excised to permit curettage of the right superior pubic ramus using a long curette (Figure 7). The lesion was gelatinous in texture and the periosteum surrounding the lesion was left intact. A commercially available bone graft (30 cc, Vitoss Scaffold, Stryker, USA) was packed within the periosteal sleeve (Figure 8). A 10-hole curved pelvic plate (Radius 88°, Stryker, USA) was utilised to stabilise the pelvis post excision, curettage and grafting of the patient’s lesion (Figure 9).
Local histological examination of the excised tissue failed to confirm a tissue diagnosis and a differential diagnosis of (1) GCTB; (2) ABC; (3) giant cell rich osteosarcoma; (4) “brown” tumour; and (5) non-ossifying fibroma was reported. The tissue material was forwarded to the United Kingdom’s National Sarcoma Specialist Centre (Royal National Orthopaedic Hospital, Stanmore, UK) for a second opinion. The sections showed (1) fragments of cystic osteoclast-rich tumour composed of bland mononuclear stromal cells; (2) coiled fragments of cystic wall containing fibrino-osteoid seam; (3) patches of basophilic calcified tissue; (4) numerous fragments of normal articular cartilage admixed with the tumour; and (5) the tissues were negative for K36M and G34W tumour markers. This specialist histopathology unit diagnosed the lesion as an ABC with no evidence of malignancy.
The patient was mobilised using crutches on post-operative day 1 with partial weight-bearing of her right lower limb. Following satisfactory mobilisation with physiotherapy and optimal pain control, the patient was safely discharged home on post-operative day 4. Partial weight-bearing was undertaken for 6 wk with progression to full weight-bearing following this. The patient has been followed up for 6 mo post-operatively, has progressed to full weight-bearing and is symptom free. X-rays of this patient’s pelvis (Figure 10) confirm satisfactory maturation of the bone grafted site and satisfactory position of internal fixation. The patient will be followed in the out-patient setting for next 5 yr minimum.
We presented a case of a young female patient who presented with a 4-mo history of atraumatic right groin pain and underwent a series of radiological and histological investigations. This patient was preliminarily diagnosed with a GCTB but was ultimately diagnosed as having an ABC within her right superior pubic ramus. The difficulty in achieving the final diagnoses was secondary to the fact that both GCTB and ABC share a number of overlapping features.
GCTBs are histologically benign but locally aggressive neoplasms[1] and account for approximately 20% of benign bone tumors and approximately 5% of all bone tumors (malignant and benign)[4]. GCTBs have a large biological spectrum ranging from latent benign to highly recurrent[1]. In rare cases (1%-6%), pulmonary metastasis is seen[5,6]. GCTBs have a peak onset at ages 21-40, while females have a greater incidence (male:female, 1:1.4)[7]. Pelvic GCTBs exhibit a marginally more pronounced male to female incidence ratio of 1:1.7[8]. GCTBs occur predominantly at the meta-epiphyseal area of long bones (75%-90%), with the distal femur being the most common site, followed by the proximal tibia, distal radius, sacrum and proximal humerus[1]. Atypical sites of GCTBs include the vertebral bodies, the hands, patella and talus[1]. GCTBs of the pelvis account for just 1.6%-6.1% of all GCTBs[8] and when they do occur, are most likely in the acetabular area followed by the iliac and the ischiopubic areas[8,9].
Historically, ABCs were considered to be a variant of giant cell tumours and were initially described in 1941 by Jaffe et al[10]. The microscopic appearances of the two lesions are sometimes dramatically similar, and they are occasionally indistinguishable, explaining the preliminary diagnosis of a GCTB[11]. ABCs are less common, highly vascularised, osteolytic lesions. They are largely seen in childhood and young adulthood, with 90% occurring in patients under 30[12]. ABCs, similarly to GCTBs, are typically located on the metaphysis of long bones, while pelvic ABCs constitute half of flat bone ABCs. ABCs may arise as a primary neoplasm (66%) or secondary to neoplasms (33%) such as GCTBs, osteosarcomas and chondroblastomas[3]. GCTBs are the preceding lesion of secondary ABCs in 19%-39% of cases[11]. Pathogenesis of primary ABCs is unclear although historically it was thought to result from a local circulatory disturbance leading to markedly increased venous pressure and the development of a dilated and enlarged vascular bed within the affected bone area[13]. However, more recent studies have proposed a hereditary factor[14].
Radiologically, GCTBs are characterised by (1) erratic and lytic lesions demonstrating a “soap bubble” appearance; (2) a lack of internal calcification; and (3) cortical thinning. Other features such as (4) cortical penetration; (5) periosteal reaction; and (6) pathological fractures can also be shown. ABCs can share a number of these features, therefore magnetic resonance imaging (MRI) is vital to aid diagnosis. In GCTBs, MRI typically demonstrates low to intermediate signal using T1 sequence and high signal using T2 signal intensity. Using MRI, ABCs typically demonstrate (1) an expansile appearance with multi-septated cysts; (2) fluid-fluid levels/solid components; and (3) thin-walled margins[15]. The presence of fluid-fluid levels may also be seen in giant cell tumors of the bone (GCTs), amongst other lesions[15] (chondroblastoma, simple bone cysts and telangiectatic osteosarcoma), therefore histological examination is vital.
Histologically, GCTs are determined using the following features for characterisation: (1) Numerous osteoclast-like giant cells uniformly distributed; (2) Presence of spindle and round/oval mononuclear cells; (3) Highly vascular stroma; (4) Necrosis; and (5) Vascular invasion may be present[16]. Separately, ABCs are characterised by (1) large cystic spaces filled with blood separated by fibrous septa; (2) cysts and septa bordered by histiocytes, myofibroblasts and fibroblasts; (3) variable mitotic figures/haemosiderin; (4) absent atypia; and (5) clusters of osteoclast-like multinucleated giant cells[17]. Other options are available to aid diagnosis including next generation sequencing, fluorescence in situ hybridisation analysis and other cytogenetic examinations[18].
Intralesional curettage accompanied by reconstruction of the residual defect by bone graft or cementing is an appropriate surgical procedure for ABCs. A high-power burr has been recommended to optimise the curettage and reduce the risk of recurrence[19]. This method strikes the greatest balance between tumour removal and maintenance of functionality. Recurrence rates for this method are approximately 16%-45%[20]. The use of adjuvants such as phenol, local toxins or filling with polymethylmethacrylate have been shown to reduce recurrence rates post curettage[21]. Due to their infrequent occurrence, there is no management guideline on the optimal surgical protocol for the treatment of pelvic ABCs. The tumour site has a critical influence on treatment. Complications, particularly with wide resection, are common (20%), but studies show a low overall mortality rate (3.2%)[8]. Although local recurrence of pelvic ABCs are expectedly more common in patients who undergo intralesional curettage alone[8], wide resection is primarily done where there is extensive bone destruction, joint preservation is impossible, recurrent disease or biologically more aggressive tumours[20,22]. In this case, wide resection was deemed necessary due to the extent of the bone destruction.
Due to their high level of vascularization, surgical adjuncts such as selective arterial embolism may be employed as a primary treatment of ABCs that are difficult to access such as those of the pelvis[2]. Successful embolization of an ABC has been shown to result in progressive ossification within 2-4 mo of initial embolization[11]. In one study, 61% of patients were found to require just one embolization, while 25% required two and 14% required three, making embolization an attractive treatment option for ABCs[23]. Sclerotherapy using polidocanol has also been shown to have high efficacy in the treatment of ABCs[2].
The management of this case was further complicated by the neoplasm being located on the superior pubic ramus. Surgery relating to the superior pubic ramus requires critical planning due to its proximity to corona mortis, a variant anastomosis between the external iliac artery or inferior epigastric artery and the obturator artery. This anastomosis runs along the posterior aspect of the superior pubic ramus. Significant, brisk haemorrhage may occur if it is accidentally breached and subsequent haemostasis is difficult to obtain, although this occurrence is rare[24]. Medical treatment adjuncts specific to ABCs were discussed at multi-disciplinary team meeting but were not deemed appropriate (e.g., denosumab) to optimise the management of this patient’s ABC.
Following review of the above literature and discussion at multi-disciplinary meeting, this patient successfully underwent wide excision, curettage and bone graft as well as open reduction and internal fixation of the right hemi-pelvis.
We have presented a less common case of ABC of the right superior pubic ramus in a young female and our management of this diagnosis. This case was initially diagnosed as a giant cell tumour, however, following specialist histopathological opinion of the intra-operative specimen, ABC was diagnosed. We hereby report the successful treatment of this patient with wide excision, curettage and bone graft and underwent open reduction and internal fixation of the right hemi-pelvis. This patient has had an uncomplicated post-operative course, has returned to comfortable weight bearing and will be reviewed for minimum 5 yr in the out-patient setting to monitor for reoccurrence.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Ireland
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Matcuk GR, Leung PC S-Editor: Wang LY L-Editor: A E-Editor: Liu MY
| 1. | Mavrogenis AF, Igoumenou VG, Megaloikonomos PD, Panagopoulos GN, Papagelopoulos PJ, Soucacos PN. Giant cell tumor of bone revisited. SICOT J. 2017;3:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Park HY, Yang SK, Sheppard WL, Hegde V, Zoller SD, Nelson SD, Federman N, Bernthal NM. Current management of aneurysmal bone cysts. Curr Rev Musculoskelet Med. 2016;9:435-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 135] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 3. | Tomoyuki K, Susa M, Nakayama R, Watanabe I, Horiuchi K, Toyama Y, Morioka H. Secondary aneurysmal bone cyst following chondroblastoma of the patella. Rare Tumors. 2013;5:e43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Turcotte RE. Giant Cell Tumor of Bone. Orthop Clin North Am. 2006;37:35-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 262] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 5. | Wülling M, Engels C, Jesse N, Werner M, Delling G, Kaiser E. The nature of giant cell tumor of bone. J Cancer Res Clin Oncol. 2001;127:467-474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 125] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Gupta R, Seethalakshmi V, Jambhekar NA, Prabhudesai S, Merchant N, Puri A, Agarwal M. Clinicopathologic profile of 470 giant cell tumors of bone from a cancer hospital in western India. Ann Diagn Pathol. 2008;12:239-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Verschoor AJ, Bovee JVMG, Mastboom MJL, Sander Dijkstra PD, Van De Sande MAJ, Gelderblom H. Incidence and demographics of giant cell tumor of bone in The Netherlands: First nationwide Pathology Registry Study. Acta Orthop. 2018;89:570-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Zheng K, Wang Z, Wu SJ, Ye ZM, Xu SF, Xu M, Hu YC, Yu XC. Giant cell tumor of the pelvis: a systematic review. Orthop Surg. 2015;7:102-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Magee KR. The neurologic workup by the primary care physician. Postgrad Med. 1977;61:77-80, 83-84, 86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 66] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Jaffe HL, Lichtenstein L. Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg. 1942;44:1004-1025. |
| 11. | Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. 1995;164:573-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 292] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, Kotz R. Aneurysmal bone cyst. A population based epidemiologic study and literature review. Clin Orthop Relat Res. 1999;363:176-179. [PubMed] |
| 13. | Cin PD. Bone: Aneurysmal bone cysts. Atlas of Genetics and Cytogenetics in Oncology and Haematology. 2002. Available from: http://atlasgeneticsoncology.org/Tumors/AneurBoneCystID5133.html. |
| 14. | Cottalorda J, Bourelle S. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg. 2007;127:105-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 131] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Yu X, Guo R, Fan C, Liu H, Zhang B, Nie T, Tu Y, Dai M. Aneurysmal bone cyst secondary to a giant cell tumor of the patella: A case report. Oncol Lett. 2016;11:1481-1485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Harte J, Clay MR, Zynger D. Bone - Giant Cell Tumor of Bone. Ohio State University, Wexner Medical Center, USA. Available from: http://www.pathologyoutlines.com/topic/bonegiantcelltumor.html. |
| 17. | Pernick N. Bone – Aneursymal Bone Cyst. Ohio State University, Wexner Medical Center, USA. Available from: http://www.pathologyoutlines.com/topic/boneabc.html. |
| 18. | Rehkämper J, Steinestel K, Jeiler B, Elges S, Hekeler E, Huss S, Sperveslage J, Hardes J, Streitbürger A, Gosheger G, Wardelmann E, Baumhoer D, Trautmann M, Hartmann W. Diagnostic tools in the differential diagnosis of giant cell-rich lesions of bone at biopsy. Oncotarget. 2018;9:30106-30114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Puri A, Agarwal M. Treatment of giant cell tumor of bone: Current concepts. Indian J Orthop. 2007;41:101-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Kekatpure A, Pimprikar M, Kekatpure A. Arthroscope assisted intralesional curettage of GCT. J Orthop Case Rep. 2015;5:6-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Knochentumoren A, Becker WT, Dohle J, Bernd L, Braun A, Cserhati M, Enderle A, Hovy L, Matejovsky Z, Szendroi M, Trieb K, Tunn PU. Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy. J Bone Joint Surg Am. 2008;90:1060-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 279] [Article Influence: 16.4] [Reference Citation Analysis (1)] |
| 22. | Klenke FM, Wenger DE, Inwards CY, Rose PS, Sim FH. Giant cell tumor of bone: risk factors for recurrence. Clin Orthop Relat Res. 2011;469:591-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 257] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 23. | Rossi G, Rimondi E, Bartalena T, Gerardi A, Alberghini M, Staals EL, Errani C, Bianchi G, Toscano A, Mercuri M, Vanel D. Selective arterial embolization of 36 aneurysmal bone cysts of the skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol. 2010;39:161-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 24. | Papagrigorakis E, Gkarsioudis K, Skandalakis P, Filippou D. Corona Mortis: Surgical Anatomy, Physiology and Clinical Significance. Int J New Tech and Res. 2018;4:64-66. |