Published online Nov 18, 2020. doi: 10.5312/wjo.v11.i11.523
Peer-review started: April 12, 2020
First decision: August 23, 2020
Revised: September 7, 2020
Accepted: October 5, 2020
Article in press: October 5, 2020
Published online: November 18, 2020
Processing time: 216 Days and 5.5 Hours
The correction surgery for severely multidimensional spinal deformity in neurofibromatosis type I is very difficult and it is still a very big challenge for spine surgeons.
A 44-year-old woman presented with progressive kyphosis for more than 10 years and low back pain for 2 years. She had been diagnosed with neurofibromatosis at a local hospital many years ago. Conservative treatments had been applied, but the symptoms got worse rather than alleviated. Therefore, surgery was required.
For this patient with severe deformity, the correction treatment of Ponte osteotomy followed by satellite rod technique in the region of the apical vertebra and the technique of pedicle screws and dual iliac screws had been applied, and successful clinical outcomes were achieved.
Core Tip: The neurofibromatosis type I (NF-I) dystrophic spinal deformity can be very severe. Thus, sufficient and exquisite preoperative assessment is significantly important for the correction surgery. In this study, we creatively performed a modified surgery for a patient with NF-I dystrophic spinal deformity.
- Citation: Shi Y, Li YH, Guan ZP, Huang YC, Yu BS. Modified surgical treatment for a patient with neurofibromatosis scoliosis: A case report. World J Orthop 2020; 11(11): 523-527
- URL: https://www.wjgnet.com/2218-5836/full/v11/i11/523.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i11.523
Neurofibromatosis is one of the most common single-gene disorders and it is autosomal dominant. According to its clinical manifestations and genetic location, neurofibromatosis can be divided into neurofibromatosis type I (NF-I), neurofibroma-tosis type II, and schwannomatosis. NF-I is frequently associated with orthopaedic disorders such as scoliosis, in which severe wedging and rotation of the vertebral body, vertebral subluxation, penciling of ribs, spindling of transverse processes, enlargement of nerve root canal, and pedicle defects are often seen[1,2]. The correction surgery for this severely multidimensional spinal deformity is very difficult and is still a very big challenge for spine surgeons. Importantly, personalized treatment is required. Herein, we report a new treatment for a patient with neurofibromatosis scoliosis.
A 44-year-old woman presented with progressive kyphosis for more than 10 years and low back pain in the past 2 years.
It had been about 10 years since she suffered from kyphosis, just after she gave birth. After long standing and fatigue, she began to feel low back pain, and her height became shorter after getting up in the morning, but she had not been diagnosed and treated. She suffered from severe inferiority due to deformity as well. In the last 2 years, her pain was gradually aggravated. Neurofibromatosis was diagnosed at a local hospital many years ago.
The patient had no previous medical history.
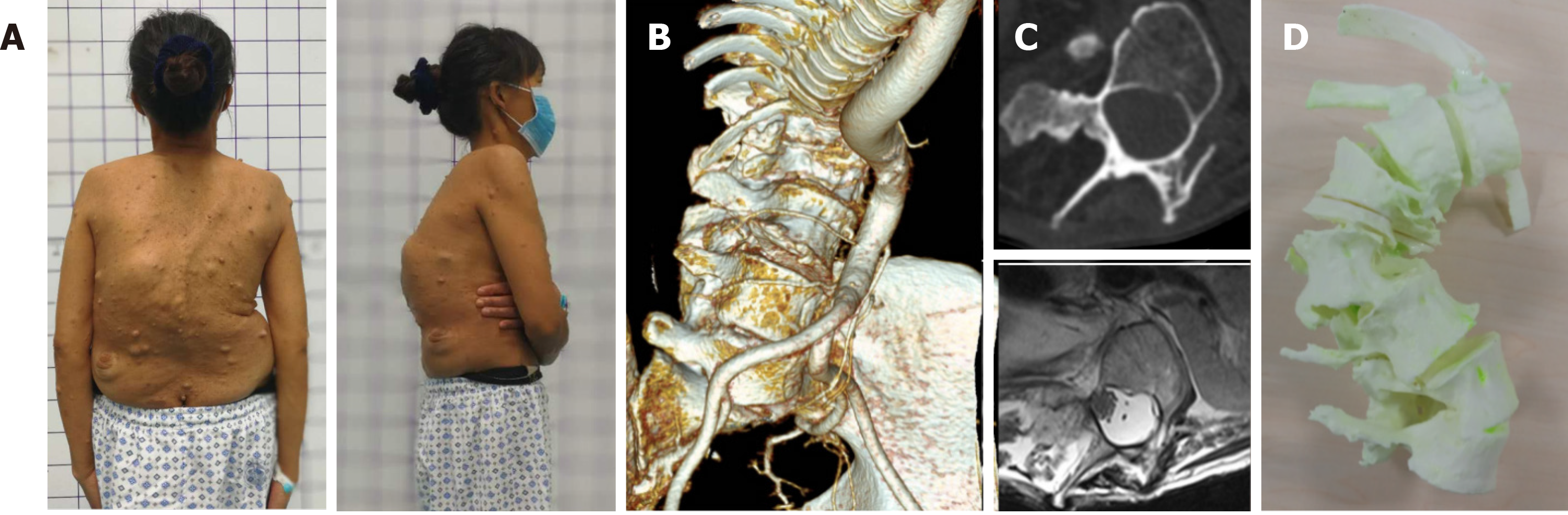
The patient was 144 cm in height and had a weight of 40 kg. A mass of café-au-lait spots and neurofibromas can be found over her body. She presented thoracolumbar angular kyphosis, but no spinal cord damage or neurological dysfunction (Figure 1).
The bone mineral density is as follows: Femoral neck, 0.747 g/cm2; and T-score: -1.8. The bone mass of the femur decreased.
Preoperative computerized tomography (CT) and magnetic resonance imaging examinations showed rotatory subluxation of L2 vertebra, spontaneous fusion of T12-L4 vertebrae, thin pedicles of L1-L5, expansion of dural ectasia, and spinal cord located in the concave side (right) (Figure 2).
NF-I dystrophic spinal deformity.
After the patient received conservative treatment for a few days, the pain was not alleviated. Thus, we decided to take surgical treatment.
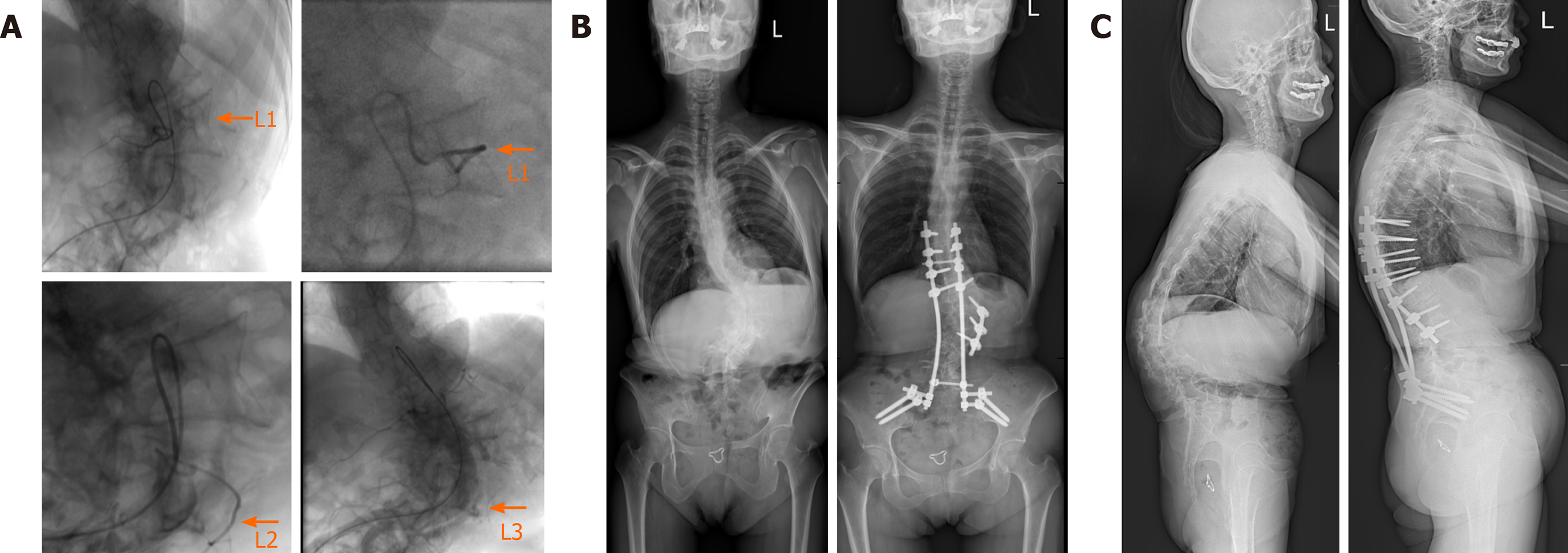
Forty-eight hours before operation, L1-L3 segmental artery embolization was performed under digital subtraction angiography to reduce the intraoperative hemorrhage. With the patient lying prone on a Jackson table, because the pedicles of L1-L5 are too thin to be implanted with pedicle screws, a total of eight pedicle screws were placed in T9-T12 under navigation, and internal fixation with dual iliac screws was performed at the same time. Potent osteotomy was performed at L1/L2 and L2/L3, the bone was loosened to the anterior osteophyte along the intervertebral space, and the intervertebral space was filled with bone graft.
The transvertebra screw and satellite rod were placed in L1-L3 on the convex side of the apical vertebra. The convex side of the apical vertebra was compressed for the local correction and the main bending angle of the scoliosis was reduced.
Finally, the full-length orthopedic rod stretching out the concave side was placed and then the maximum correction effect was achieved by clasping the convex side. After decortication of posterior bony element of the spine, autologous bone chips and allograft bone chips were implanted. The whole procedures were monitored by motor evoked potential and somatosensory evoked potential. The duration of operation was 5 h with a blood loss of 500 mL. After the deformity correction surgery, thoracic-lumbo-sacral orthosis was applied for 3 mo in order to protect excessive strains and to prevent dislodgement of the implants.
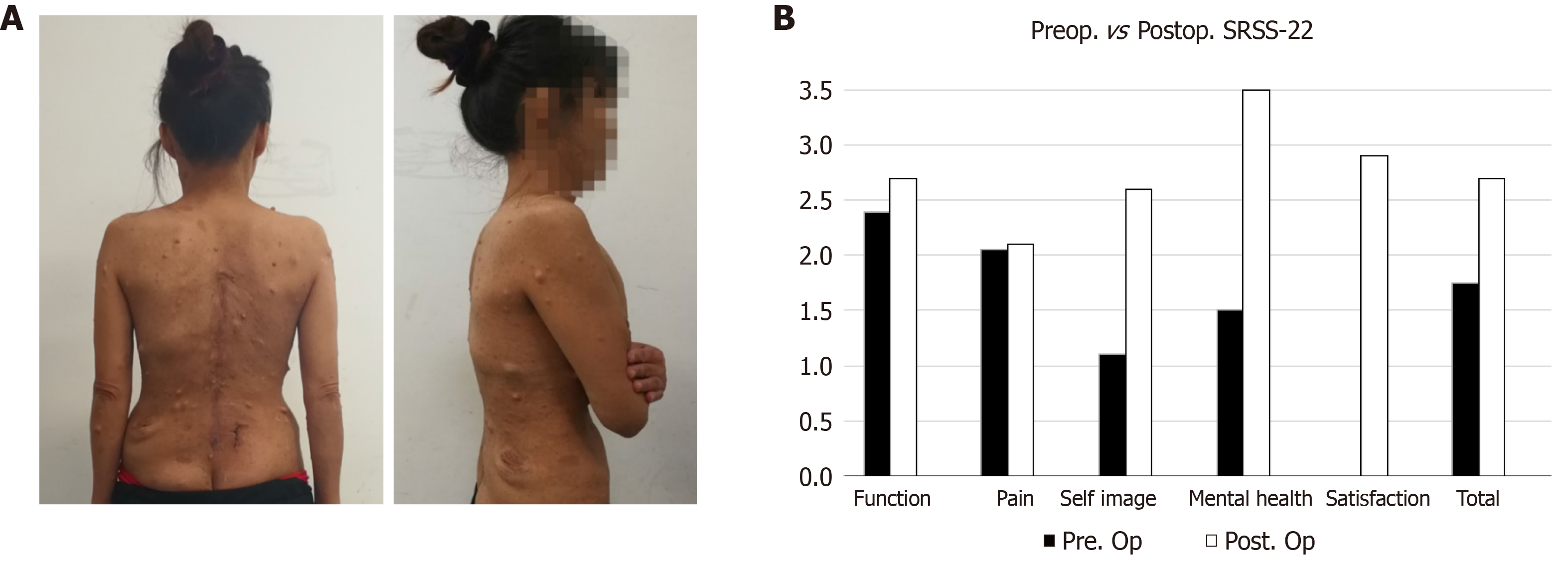
The patient’s height became 153 cm postoperatively. Corrected spinal curve and height were well preserved during a 2-year follow-up period with solid fusion without neurologic deficit (Figure 3A). At the final follow-up, her Scoliosis Research Society-22r score was significantly improved compared to preoperative score (Figure 3B).
The surgical treatment for NF-I dystrophic spinal deformity is still a challenge for spine surgeons. Because of the presence of paraspinal neurofibroma and plexiform veins surrounding the spinal soft tissue, the surgery can cause massive blood loss. Therefore, the segmental artery interventional embolization is routinely adopted during the total vertebra resection, and the embolization of L1-L3 bilateral segmental arteries effectively reduced the intraoperative hemorrhage and shortened the operation time.
For patients with severe rigid deformity, although three-column osteotomy is good for deformity correction, the high-risk complications during the perioperative period, postoperative internal fixation failure, pseudarthrosis formation, and the loss of correction cannot be ignored. It was reported that the incidence of neurologic complications after three-column osteotomy is 9.9%-21.9% while the incidence of rod breaking is as high as 16.7%[3]. For this patient, after careful inquiry of her history, we found that the kyphosis would partially recover after lying down at night, and the kyphosis would gradually increase after the physiological load in the morning. We believed that the surgical goal for the patient was to stabilize the spine and to prevent spinal cord injury caused by further progression of deformities; hence, it was not necessary to pursue complete reduction.
If the apical vertebra could be fully released, kyphosis can be effectively corrected and strong fixation can be maintained. Different from three-column osteotomy, Ponte osteotomy only removes the articular process and part of the lamina, which is less invasive and much safer for patients and easier for surgeons. Meanwhile, the preoperative CT demonstrated that the anterior vertebral body had formed osseous fusion. During the operation, for further loosening, an ultrasonic bone knife was used to cut off the bone bridge of the anterior edge of the vertebral body through the intervertebral space, which improved the correction of severe scoliosis.
The finite elements analysis reveals that the satellite rod was able to enhance the strength of the internal fixation remarkably and disperse the stress of the main rod effectively so as to decrease the incidence of the main rod fracture[4]. The use of Ponte osteotomy combined with satellite rod sequential orthopedic technology obtained better correction in the treatment of severe rigid thoracic scoliosis, and during the long-term follow-up there was less loss of correction[3,4]. Hence, it is a safe and effective surgical strategy. In this case, the screw could not be placed because of the thin pedicle of the lumbar vertebra. In order to strength the fixation of the osteotomy region, we innovatively designed a new approach to insert the vertebral nails on the side of the vertebral body together with the satellite rod at the same time. Finally, very satisfying outcomes were achieved.
Biomechanical testing has confirmed that the anti-compression and anti-torsion ability of dual iliac screws is higher than that of single iliac screw and the stability is the same as that of the initial state[5-7]. For this patient, the dual iliac screw was necessary; even if the patient is short, patients with NF-I malnutrition have varying degrees of osteoporosis. Therefore, strong anchoring should be performed to improve the stability of long segment fixation and fusion, so as to ensure the safety of the surrounding osteotomy area before stable bone fusion.
Although no neurologic cardiopulmonary complication was seen during the surgery and follow-up period in this case, we still need to pay attention to this issue. Ponte osteotomy may cause nerve injury and the major mechanisms include stretching or mechanical trauma of the spinal cord and nerve roots; thus, regional cord ischemia from vascular insufficiency may occur. However, based on the existing literature, it is not easy to assess the true rate of neurologic complications in patients after the treatment of Ponte osteotomy[8,9]. This issue remains further investigations.
Preoperative three-dimensional printing model, intraoperative spinal nerve monitoring, and accurate intraoperative navigation are the important guarantees of safe operation for NF-I dystrophic spinal deformity. Most of the cases of NF-I dystrophy were thoracic scoliosis and it was for the first time that lumbar subluxation with all lumbar pedicle mutation was found. For this severe deformity, local correction was performed with Ponte osteotomy in the apex region combined with vertebral screw satellite rod technique, followed by the fixation using long segment transpedicular screws and dual iliac screws. This modified technique is safe and effective for NF-I dystrophic spinal deformity.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Caboclo JF, Hashimoto N S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Kim WB, Park YS, Park JH, Hyun SJ. Posterior Spinal Reconstruction with Pedicle Screws, Multiple Iliac Screws and Wisconsin Spinal Wires in a Patient with Neurofibromatosis Scoliosis: A Case Report. Korean J Spine. 2015;12:181-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Zhao CM, Zhang WJ, Huang AB, Chen Q, He YL, Zhang W, Yang HL. Coexistence of multiple rare spinal abnormalities in type 1 neurofibromatosis: a case report and literature review. Int J Clin Exp Med. 2015;8:17289-17294. [PubMed] |
| 3. | Li Y, Shi BL, Liu Z, Sun X, Wang B, Zhu ZZ, Qiu Y. Ponte osteotomy followed by sequential correction technique with satellite rods in severe rigid thoracic scoliosis. Zhonghua Guke Zazhi. 2019;39:1357-1364. [DOI] [Full Text] |
| 4. | Seyed Vosoughi A, Joukar A, Kiapour A, Parajuli D, Agarwal AK, Goel VK, Zavatsky J. Optimal satellite rod constructs to mitigate rod failure following pedicle subtraction osteotomy (PSO): a finite element study. Spine J. 2019;19:931-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 5. | Yu BS, Zhuang XM, Zheng ZM, Li ZM, Wang TP, Lu WW. Biomechanical advantages of dual over single iliac screws in lumbo-iliac fixation construct. Eur Spine J. 2010;19:1121-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Bourghli A, Boissiere L, Obeid I. Dual iliac screws in spinopelvic fixation: a systematic review. Eur Spine J. 2019;28:2053-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Yu BS, Zheng ZM, Zhuang XM, Li ZM, Lv WJ. Biomechanical advantage of iliac dual screws in lumbo-iliac reconstruction. Zhonghua Guke ZaZhi. 2010;30:589-593. [DOI] [Full Text] |
| 8. | Shah SA, Dhawale AA, Oda JE, Yorgova P, Neiss GI, Holmes L Jr, Gabos PG. Ponte Osteotomies With Pedicle Screw Instrumentation in the Treatment of Adolescent Idiopathic Scoliosis. Spine Deform. 2013;1:196-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Buckland AJ, Moon JY, Betz RR, Lonner BS, Newton PO, Shufflebarger HL, Errico TJ; Harms Study Group. Ponte Osteotomies Increase the Risk of Neuromonitoring Alerts in Adolescent Idiopathic Scoliosis Correction Surgery. Spine. 44:E175-E180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |