Published online Nov 18, 2020. doi: 10.5312/wjo.v11.i11.492
Peer-review started: April 10, 2020
First decision: September 18, 2020
Revised: September 30, 2020
Accepted: October 20, 2020
Article in press: October 20, 2020
Published online: November 18, 2020
Processing time: 218 Days and 12.2 Hours
Orthopedic physicians typically apply a cast to immobilize a body part that has been injured. There have been no significant structural changes or advances in synthetic casts since the development of the modern cast. The Opencast® is a recently developed type of cast that allows ventilation and direct visual inspection of the skin to avoid cast-related complications. Although this novel cast appears to have more benefits than the conventional synthetic cast, its clinical efficacy and advantages have not been established.
To investigate the clinical efficacy and advantages of the newly developed Opencast® based on patients’ perspectives in those with ankle inversion injury.
A specifically designed questionnaire consisting of 19 items was used to compare patients’ opinions and concerns of the Opencast® and the conventional synthetic cast. The items were focused on subjective patient satisfaction, discomfort, and adverse effects while wearing the cast. Patients with an ankle inversion injury diagnosed as a high-grade ankle sprain were enrolled. The subjects were randomized and instructed to fill the questionnaire after wearing a synthetic cast or an Opencast® for 2 wk. They were then required to fill the questionnaire again, after switching to the alternative type of cast for 2 more weeks.
A total of 22 subjects participated in the study. The synthetic cast appeared to be more rigid and stable than the Opencast®, but there was no significant difference in the amount of pain relief. The likelihood of adverse effects when wearing the synthetic cast was significantly higher. Patient satisfaction tended to be rated higher after wearing the Opencast®. Opencast® showed more subjective vulnerability than the synthetic cast, but there was no significant difference in the redo rate. Patients were more anxious about removal of the synthetic cast than of the Opencast®.
The results indicate that the Opencast® could replace the conventional synthetic cast as it offers increased patient satisfaction, which would in turn increase compliance to treatment.
Core Tip: A newly developed Opencast® was found to provide more convenience and satisfaction in patients with ankle sprain. The patients wearing the Opencast® could take showers and felt less anxiety during cast removal. These characteristics are expected to increase the patients’ compliance with treatment.
- Citation: Min BC, Yoon JS, Chung CY, Park MS, Sung KH, Lee KM. Patients’ perspectives on the conventional synthetic cast vs a newly developed open cast for ankle sprains. World J Orthop 2020; 11(11): 492-498
- URL: https://www.wjgnet.com/2218-5836/full/v11/i11/492.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i11.492
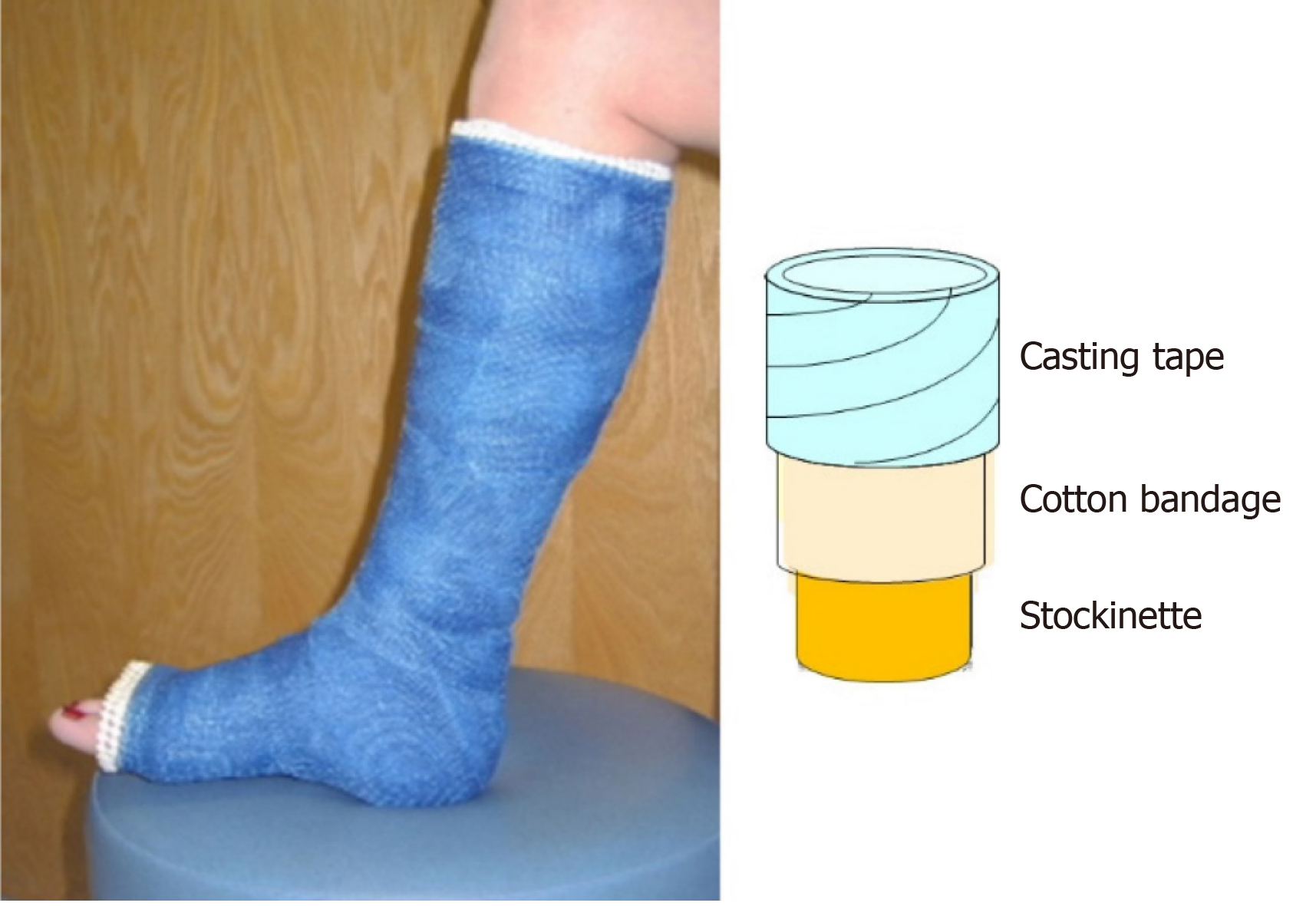
Traditionally, the first-line treatment of an ankle sprain, which is the most common sports-associated injury, involves immobilizing the joint. Orthopedic physicians typically apply a cast to immobilize an injured body part. The modern plaster cast dates back to the 1850s when a Dutch military surgeon first used cotton bandages impregnated with calcined gypsum to immobilize limb fractures. The so-called plaster of Paris cast has been used widely in the field of orthopedics ever since[1,2].
Nearly 120 years later, in the 1970s, a synthetic cast made out of fiberglass was developed and is still used worldwide[1,2]. However, this synthetic cast was developed by only changing the cast material from cotton bandage impregnated with gypsum to fiberglass. Although some improvement has been made in terms of stiffness and weight, there have been no other significant structural changes or advances in synthetic casts since the development of the modern cast 170 years ago.
Regardless of the cast material used, there have been some inevitable adverse effects, given that the cast cannot be taken off during treatment and the material is hard. Furthermore, there can be serious complications, such as tight cast syndrome, which includes skin necrosis, pressure ulcers, and nerve palsy[3,4]. Immobilizing boots are commercially available and could avoid these complications, but their efficacy and patient compliance are not guaranteed.
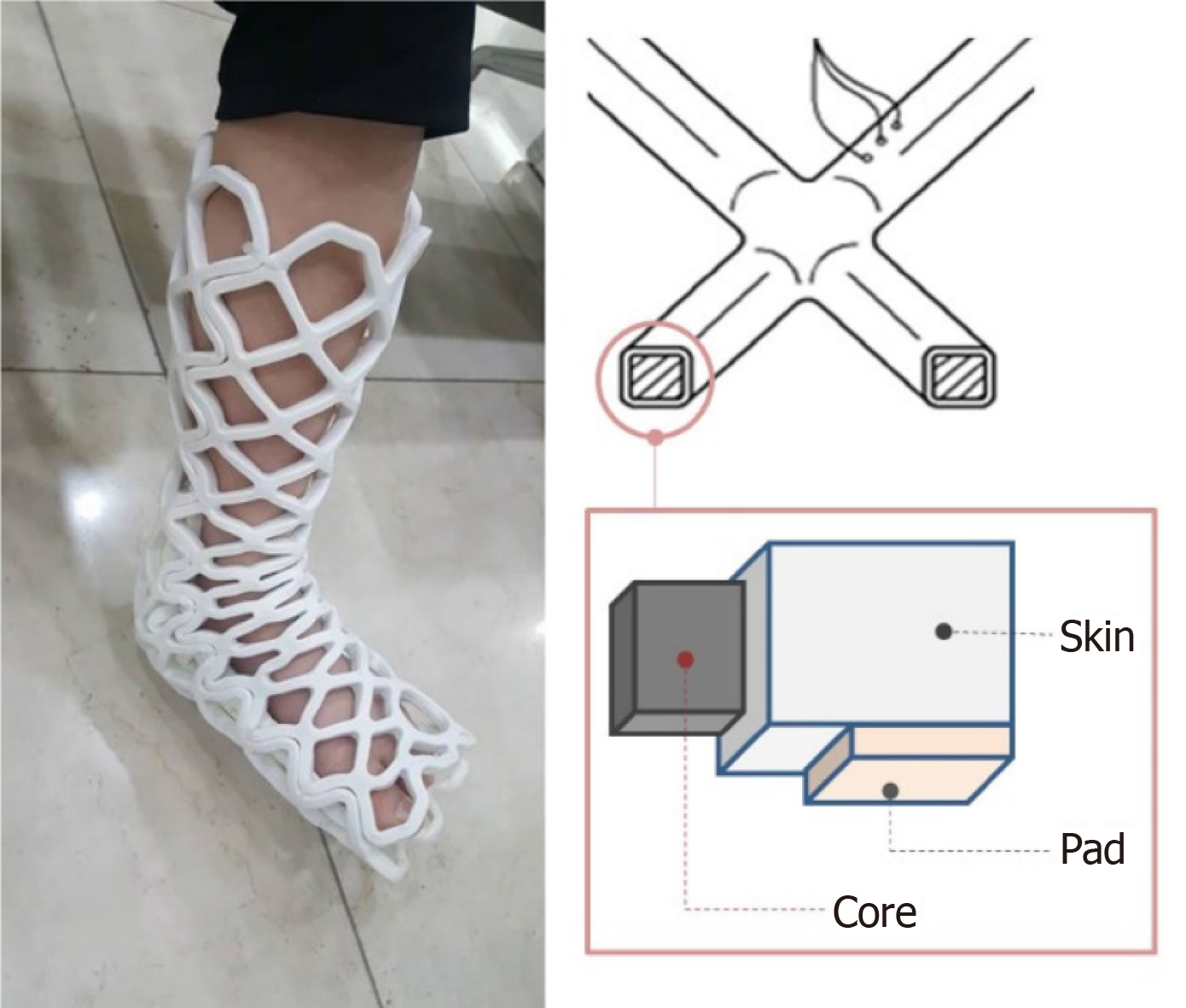
The Opencast® (OpenM, Daejeon, Korea) is a newly developed type of cast that contains multiple web-type or mesh-type open spaces that allow ventilation and direct visual inspection of the skin to avoid cast-related complications. Furthermore, the Opencast® guarantees compliance because patients cannot remove the cast themselves. Although this novel cast appears to have more benefits than the conventional synthetic cast, its clinical efficacy and advantages have not yet been established.
The aim of this study was to compare patients’ opinions of the relative clinical benefits of the Opencast® and the conventional synthetic cast using a specifically designed questionnaire.
This prospective study was approved by the institutional review board of our hospital. Informed consent was obtained from all study participants.
Before initiating the study, the questionnaire items were devised by a consensus committee consisting of three orthopedic surgeons and a research assistant specialized in questionnaire development. The items were selected from previous studies[3-5] or generated during discussions by the committee.
Emphasis was made on subjective patient satisfaction, discomfort, and adverse effects while wearing the cast. The inclusion of any item was decided by considering its content validity, which was mainly determined by consensus of the committee members. Nineteen items were chosen. The items in this questionnaire were categorized into the following domains: Function and effect, adverse effects and improvement in quality of life, and effectiveness. The function and effect domain consisted of five items that assessed the subjective response regarding immobilization after application of the cast. Ten items were included in the adverse effects and improvement in quality of life domain to test for subjective satisfaction or discomfort while wearing the cast material for 2 wk. Four items were included in the effectiveness domain and were designed to compare the cast redo rate and patient discomfort during removal of the cast. All items except the first question had a response format based on a 5-point Likert scale[6] (scored 1-5) to facilitate comparison of the two types of cast. For the first two domains, the items were carefully chosen to have acceptable reliability within the domain.
The inclusion criteria were as follows: Aged 20 years or older, an ankle inversion injury diagnosed as a high-grade ankle sprain within the previous week, attendance at our outpatient clinic (at a tertiary referral center for foot and ankle surgery), and willingness to participate in the study. Patients with ankle fractures were excluded. Patients who could not complete the questionnaire and those with a previous ankle fracture, ankle surgery, infection, tumor, neuromuscular disease, or any other condition that could change the normal anatomy of the ankle joint were also excluded.
The patients enrolled in the study were randomized to fill the questionnaire after wearing a conventional synthetic cast (Figure 1) or an Opencast® (Figure 2) for 2 wk. They were then switched to the alternative type of cast for 2 more weeks after which they were required to fill the questionnaire again. The questionnaire took a maximum of 10 min to complete.
The Opencast® contains three components. The first is the core component, which is made of carbon fiber composite plastic, melts at 80–90 °C and can be molded into any shape. When the temperature is decreased after the change in shape, the shape is then solidified and maintained. The cast maintains its rigidity at temperatures below 50 °C, which is the temperature range of normal daily living. Hot showers are allowed while wearing the cast but saunas are not. The second component is an outer skin surrounding the core and is made of an elastomer with a high melting point and a rubber-like elastic texture. When the structural core component melts at high temperatures, the outer skin component holds and protects the unique mesh structure of the Opencast® while maintaining its inherent flexibility that allows easy molding. The third component is a pad that protects the skin and is in direct contact with the cast. This pad is made from skin-friendly polyolefin foam that gives the skin a soft touch and feel.
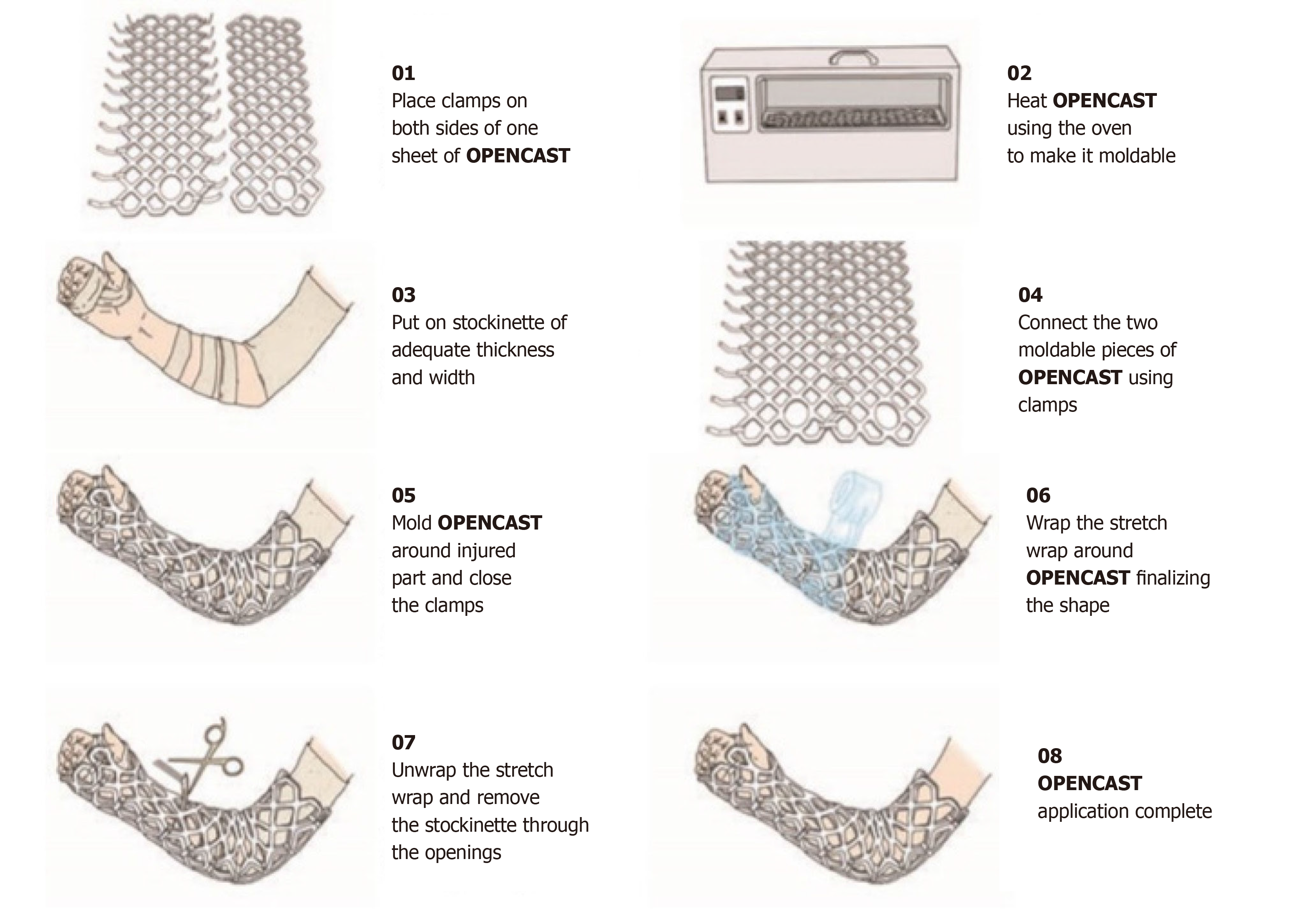
The Opencast® is applied in a way similar to that of a thermoplastic splint (Figure 3). Two appropriately sized sheets of Opencast® are preheated until soft and moldable. These sheets are then applied to the limb in a cylindrical shape using plastic clamps after covering the limb with stockinettes to prevent heat injury. After molding, the final shape is fixed using the stretch wrapping supplied with the product. Finally, all other materials, including the stockinettes and wraps, are removed through the open structure. The Opencast® is much simpler to remove than the synthetic cast. Rather than cutting it open with a saw, the plastic clamp is removed and just enough of the mesh frame is cut with a nipper to permit its removal.
This study was based on the responses of study participants to a questionnaire. It was calculated that at least 34 patients would need to be recruited to permit at least 17 patients in each matched group with an alpha error of 0.05 and a power of 0.8[7]. Anticipating a withdrawal rate of 25% during 4 wk of immobilization in a cast, each study group had to contain 23 subjects. Therefore, 23 subjects were enrolled and had their treatment alternated to constitute the matched group. During follow-up, one subject declined a follow-up visit. Therefore, 22 subjects were finally included in the data analysis.
All data are presented as mean and standard deviation. The questionnaire items were categorized according to the type of cast worn during the previous 2 wk. The responses to the synthetic cast and Opencast® questionnaires were compared using the Wilcoxon signed rank test. The reliability of the questionnaire was determined using Cronbach’s alpha. All statistical analyses were performed using SPSS software (version 25.0, IBM Corp., Armonk, NY, United States). Statistical significance was set at P < 0.05.
Of the 23 subjects initially enrolled, 1 was lost to follow up. Therefore, a total of 22 subjects were finally included in the analysis. The mean patient age was 27.0 ± 10.8 years. The reliability of the questionnaire for the first two domains was acceptable (Cronbach’s alpha, 0.71 and 0.76, respectively).
In the function and effect domain, the synthetic cast appeared to be more rigid (Q2, P < 0.001), stable (Q3, P = 0.002), and better protect the injured ankle (Q4, P = 0.001) than the Opencast®. However, there was no significant difference in the amount of pain relief offered by each type of cast (Q5, P = 0.891).
In the adverse effects and improvement in quality of life domain, the likelihood of adverse effects when wearing the synthetic cast was significantly higher in terms of tightness (Q6, P < 0.001), itchiness (Q7, P < 0.002), discomfort because of low ventilation (Q8, P < 0.001), water seeping inside the cast (Q9, P < 0.001), discomfort due to dampness (Q10, P < 0.001), bad odor (Q11, P < 0.001), inability to bathe or shower freely (Q12, P < 0.001), inability to see the skin beneath the cast (Q13, P < 0.001), and limitations to activities of daily living (Q14, P = 0.003) after casting. Patient satisfaction tended to be rated higher after wearing the Opencast® for 2 wk but this finding did not reach statistical significance (Q15, P = 0.15)
In the effectiveness domain, the Opencast® showed more subjective vulnerability than the synthetic cast (Q16, P = 0.001), but there was no significant difference in the redo rate between groups (Q17, P = 0.564). Patients were more anxious about removal of the synthetic cast than of the Opencast® (Q18, P = 0.001 and Q19, P = 0.004).
Immobilization using casts is well accepted as the first-line treatment for an ankle sprain. Although functional bracing and early rehabilitation for ankle sprains is becoming more popular nowadays, the cast still plays an important role in the treatment of this common injury[8]. In this study, we chose ankle sprain as the inclusion criterion for type of injury because it is a very common injury[9], has reports of well-established outcomes associated with ankle sprains published[10], and yields good results for immobilization of high-grade ankle sprains using casts[8-10]. The study design was set to minimize bias given that the same questionnaire was answered just 2 wk apart as part of the crossover study design.
The results for the function and effect domain show that the Opencast® provided somewhat less support than the conventional synthetic cast; however, there was no significant between-group difference in the amount of pain relief. The severity of pain experienced after an ankle sprain depended on the amount of inflammation present, which could be aggravated by movement of the injured tissues[11,12]. Therefore, this suggests that the injured ligamentous tissue was well protected and immobilized despite the patients’ subjective feelings otherwise.
The results for the adverse effects and improvement in quality of life domain were predictable for the conventional synthetic cast. The synthetic cast is less comfortable than the Opencast® because it is tight, causes itching, has limited ventilation (causing dampness), is hard to manage when water accidently seeps between the plaster and the skin, and is malodorous. The visible and open nature of the Opencast® may overcome these undesirable effects and provide satisfactory results for both patients and physicians.
Finally, in the effectiveness domain, the redo rate was similar for both types of casts despite the patients feeling more vulnerable when wearing the Opencast®. There was no evidence of a broken cast that required a redo procedure. Although the durability of the Opencast® has been controversial, its structural durability is as good as that of the conventional synthetic cast. Additionally, a patient may feel anxious when the cast is being removed. Unlike a conventional cast, the Opencast® does not require cutting by a saw to remove it. Therefore, an Opencast® would be beneficial in patients who feel anxious about the cast cutting procedure.
This study had some limitations. First, the number of study participants was small and a specific group of patients was chosen. Second, the questionnaire was subjective and did not measure any objective outcomes, such as stress radiographic examination or functional scoring. However, the purpose of this study was not to provide treatment de novo but to test the clinical application of a new type of immobilization material with the hope of improving the poor safety profile of the blind and nonwashable conventional casts. The authors assume that this new type of cast may provide adequate structural support in addition to the above-mentioned benefits.
The results of this study indicate that the Opencast® could replace the conventional synthetic cast by increasing patient satisfaction, which would in turn increase compliance to treatment. Further investigations are needed before the conventional synthetic cast can be replaced with the Opencast®. However, this small randomized controlled trial shows the potential benefit of using this novel type of cast for the treatment of ankle sprains.
Although the conventional cast has been effective in immobilizing orthopedic injuries, it has shortcomings such as foul odor, itchiness, internal moisture, inability to take a shower, etc. during its use. These could impede a patient’s compliance.
Opencast® is a recently developed mesh type of cast that allows ventilation and direct visual inspection of the skin. This cast is expected to avoid cast-related complications and discomfort. However, the advantage and efficacy of the cast have not been tested.
This study aimed to compare patients’ perspectives of the clinical benefits of the Opencast® and the conventional synthetic cast using a specifically designed questionnaire.
Patients who sustained recent ankle sprain injuries were randomly allocated to group A (initial 2 wk of conventional cast + additional 2 wk of Opencast®) and group B (initial 2 wk of Opencast® and additional 2 wk of conventional cast). Patients’ perspectives on the complications and discomfort regarding the two types of cast were compared using a specifically designed questionnaire.
A total of 22 subjects participated in the study. The conventional cast appeared to be more rigid and stable than the Opencast®. Patient satisfaction tended to be rated higher after wearing the Opencast®. Opencast® was superior to the conventional cast in the items regarding itchiness, bad odor, ability to take a shower, etc.
Opencast® was found to be appropriate for immobilization in patients with acute ankle sprains. Mechanical strength needs to be improved for this new type of cast.
Opencast® could replace the conventional synthetic cast as it offers increased patient satisfaction, which would in turn increase compliance to treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bianco L S-Editor: Zhang L L-Editor: Filipodia P-Editor: Xing YX
| 1. | DeMaio M, McHale K, Lenhart M, Garland J, McIlvaine C, Rhode M. Plaster: our orthopaedic heritage: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Philbin TM, Gittins ME. Hybrid casts: a comparison of different casting materials. J Am Osteopath Assoc. 1999;99:311-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Halanski M, Noonan KJ. Cast and splint immobilization: complications. J Am Acad Orthop Surg. 2008;16:30-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 157] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 4. | Marson BM, Keenan MA. Skin surface pressures under short leg casts. J Orthop Trauma. 1993;7:275-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Roberts A, Shaw KA, Boomsma SE, Cameron CD. Effect of Casting Material on the Cast Pressure after Sequential Cast Splitting. J Pediatr Orthop. 2017;37:74-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Sullivan GM, Artino AR Jr. Analyzing and interpreting data from likert-type scales. J Grad Med Educ. 2013;5:541-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1009] [Cited by in RCA: 970] [Article Influence: 80.8] [Reference Citation Analysis (0)] |
| 7. | Gogtay NJ. Principles of sample size calculation. Indian J Ophthalmol. 2010;58:517-518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Lamb SE, Marsh JL, Hutton JL, Nakash R, Cooke MW; Collaborative Ankle Support Trial (CAST Group). Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009;373:575-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 129] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 9. | Kannus P, Renström P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73:305-312. [PubMed] |
| 10. | van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? Am J Med. 2008;121:324-331.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 410] [Article Influence: 24.1] [Reference Citation Analysis (1)] |
| 11. | Kannus P. Immobilization or early mobilization after an acute soft-tissue injury? Phys Sportsmed. 2000;28:55-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Sommerfeldt M, Bouliane M, Otto D, Rowe BH, Beaupre L. The use of early immobilization in the management of acute soft-tissue injuries of the knee: results of a survey of emergency physicians, sports medicine physicians and orthopedic surgeons. Can J Surg. 2015;58:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |