Published online Nov 18, 2020. doi: 10.5312/wjo.v11.i11.483
Peer-review started: June 17, 2020
First decision: July 21, 2020
Revised: July 29, 2020
Accepted: September 1, 2020
Article in press: September 1, 2020
Published online: November 18, 2020
Processing time: 150 Days and 9.4 Hours
There are few studies in the literature comparing the clinical outcomes and radiographic results of proximal femoral nail (PFN) and proximal femoral nail antirotation (PFNA) for pertrochanteric femoral fracture (PFF) in elderly patients.
To evaluate both clinical and radiographic outcomes after fixation with PFN and PFNA in an elderly patient population.
One hundred fifty-eight patients older than 65 years with PFF who underwent fixation with either PFN or PFNA were included. Seventy-three patients underwent fixation with PFN, whereas 85 were fixed with PFNA. The mean follow-up was 2.4 years (range, 1-7 years). Clinical outcome was measured in terms of operation time, postoperative function at each follow-up visit, and mortality within one year. Radiographic evaluation included reduction quality after surgery, Cleveland Index, tip-apex distance (TAD), union rate, time to union, and sliding distance of the screw or blade. Complications including nonunion, screw cutout, infection, osteonecrosis of the femoral head, and implant breakage were also investigated.
Postoperative function was more satisfactory in patients who underwent PFNA than in those who underwent PFN (P = 0.033). Radiologically, the sliding difference was greater in PFN than in PFNA patients (6.1 and 3.2 mm, respectively, P = 0.036). The rate of screw cutout was higher in the PFN group; eight for PFN (11.0%) and two for PFNA patients (2.4%, P = 0.027). There were no differences between the two groups in terms of operation time, mortality rate at one year after the operation, adequacy of reduction, Cleveland Index, TAD, union rate, time to union, nonunion, infection, osteonecrosis, or implant breakage.
Elderly patients with PFF who underwent PFNA using a helical blade demonstrated better clinical and radiographic outcomes as measured by clinical score and sliding distance compared with patients who underwent PFN.
Core Tip: There are few studies comparing the clinical outcomes and radiographic results in elderly patients with pertrochanteric femoral fracture (PFF) receiving proximal femoral nail antirotation (PFNA) and those receiving the previous-generation proximal femoral nail. PFNA using a helical blade demonstrated better clinical and radiographic outcomes in terms of clinical score, sliding distance and cutout rate in elderly patients with PFF.
- Citation: Baek SH, Baek S, Won H, Yoon JW, Jung CH, Kim SY. Does proximal femoral nail antirotation achieve better outcome than previous-generation proximal femoral nail? World J Orthop 2020; 11(11): 483-491
- URL: https://www.wjgnet.com/2218-5836/full/v11/i11/483.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i11.483
As the population continues to age, the incidence of pertrochanteric femoral fracture (PFF) has also increased[1] and surgery has been reported as a standard treatment for achieving better clinical outcomes, including shorter hospitalization, earlier return to preinjury status, and fewer complications such as bed sores, pulmonary thromboembolism, and pneumonia[2-4]. Among the numerous implants currently available for the internal fixation of PFF[5-7], proximal femoral nail (PFN; Synthes®, Solothurn, Switzerland) has been reported in the last decade to be a suitable implant for the treatment of unstable PFF in elderly patients[8-10]. However, some studies have reported several complications associated with the use of PFN, including cutout and the Z-effect[8,11,12]. To overcome these complications, a newly-designed implant, proximal femoral nail antirotation (PFNA; Synthes®, Solothurn, Switzerland), has been developed. According to a biomechanical study conducted in the laboratory setting, the PFNA blade compacts the cancellous bone, leading to increased stability and higher resistance to cutout in the osteoporotic bone[13]. However, there are few studies comparing clinical outcomes and radiographic results (including cutout after fixation) between elderly patients with PFF receiving PFNA and those receiving the previous-generation PFN. Therefore, we evaluated the clinical and radiographic outcomes after fixation with PFN and PFNA for PFF in elderly patients.
This retrospective study was approved by the institutional review board in our institution which waived informed consents. From January 2003 to December 2009, 204 patients over 65 years of age with PFF underwent fixation with either PFN or PFNA at a single institution. Among them, 46 patients were excluded because of bilateral PFF (2 patients) and loss to follow-up before radiographic follow-up at one year (44 patients). Thus, the remaining 158 patients were included. The mean duration of radiographic follow-up was 2.4 years (range, 1-7 years). Seventy-three patients underwent fixation with PFN (PFN group), whereas 85 patients were fixed with PFNA (PFNA group). The PFN group was composed of 31 men and 42 women with an average age of 76.6 ± 7.3 years. Based on the AO classification[14], fractures was categorized as 31-A1 in 14 patients, A2 in 42 patients, and A3 in 17 patients. The PFNA group consisted of 37 men and 48 women with an average age of 74.9 ± 7.2 years. Fractures were classified as 31-A1 in 19 patients, A2 in 50 patients, and A3 in 16 patients. We identified each patient’s medical history and converted it to a Charlson Comorbidity Index[15] score by deploying questionnaires at each patient’s visit to the clinic and conducting a careful review of medical records. In addition, femoral bone mineral density was also investigated. Demographic details and fracture characteristics are described in Table 1. There were no differences between the two groups (P > 0.05).
| PFN group | PFNA group | P value | |
| Number of patients | 73 | 85 | NA |
| Male:female | 31:42 | 37:48 | 0.893 |
| Age, yr | 76.6 (65-90) | 74.9 (65-92) | 0.213 |
| BMI, kg/m2 | 21.4 (18.5-31.6) | 22.8 (20.4-28.3) | 0.576 |
| Femoral BMD, T-score | -2.83 (-1.3 to -5.3) | -3.14(-1.1 to -6.1) | 0.518 |
| Charlson Comorbidity Index[15] | 13.4 (3-18) | 11.9 (4-19) | 0.536 |
| Cause of injury | 0.890 | ||
| Slip down | 56 | 65 | |
| Traffic accident | 8 | 11 | |
| Fall down | 9 | 9 | |
| AO/OTA classification | 0.750 | ||
| 31-A1 | 14 | 19 | |
| 31-A2 | 42 | 50 | |
| 31-A3 | 17 | 16 | |
| Stay before operation, d | 4.02 (1-13) | 2.84 (1-17) | 0.253 |
All operations were performed using a fracture table under the guidance of fluoroscopy. We encouraged the Q-setting exercise with an active range of motion, with wheelchair ambulation at one day after index operation. Clinical outcome was measured in terms of operation time, postoperative function according to Salvati and Wilson’s hip function rating system[16] at each patient’s visit to the clinic, and mortality rate within one year. The operation time was calculated from skin incision to closure. We searched the National Statistical Office for death certificates for patients who failed follow-up[17]. Radiographic evaluation included the reduction state after the operation, which was categorized into three groups using modified Baumgartner’s criteria[18], the Cleveland Index[19], tip-apex distance (TAD)[7], union rate, time to union and sliding distance of the screw or blade. Complications, including nonunion, screw cutout, infection, osteonecrosis of the femoral head, and implant breakage were also investigated.
The Pearson chi-square test and Student t-test were performed for statistical analysis using SPSS software version 22.0 (SPSS, Chicago, IL, United States), and differences were considered significant when the P value was < 0.05. The statistical methods used in this study were reviewed by Won Kee Lee, Professor of Biostatistics of Kyungpook National University.
In the PFN group, postoperative hip function was graded as excellent in 26 (35.6%), good in 35 (47.9%), fair in 8, and poor in 4 patients, respectively (Table 2). In the PFNA group, hip function was classified as excellent in 36 (42.4%), good in 44 (51.8%), fair in 4, and poor in 1 patient, respectively. The proportion of patients with excellent or good postoperative function was significantly higher in the PFNA group compared to the PFN group (94.1% and 83.6%, P = 0.033). Differences in operation time and mortality within one year were not significantly different between the two groups (P > 0.05).
| PFN group | PFNA group | P value | |
| Operation time, min | 67.3 | 63.2 | 0.395 |
| Salvati and Wilson score score[16] | 0.328 | ||
| Excellent (32 or more) | 26 | 36 | |
| Good (24-31) | 35 | 44 | |
| Fair (16-23) | 8 | 4 | |
| Poor (15 or less) | 4 | 1 | |
| Excellent + good | 61 (83.6%) | 80 (94.1%) | 0.033 |
| Mortality within one year | 16 (21.9%) | 20 (23.5%) | 0.629 |
The union rate was 87.7% for the PFN group (64/73) and 94.1% for the PFNA group (80/85) (P = 0.155), and the union time was 14.9 wk (range, 12-17) and 13.7 wk (range, 11-18), respectively (P = 0.156).
In the PFN group, reduction was graded as good in 34 (46.6%), normal in 31 (42.5%), and poor in 8 patients, whereas it was rated as good in 42 (49.4%), normal in 36 (42.4%), and poor in 7 patients in the PFNA group (P = 0.830; Table 3). According to Cleveland et al[19], zones 5, 6, 8, and 9 were shown in 67 (91.8%) patients with PFN, whereas those zones were demonstrated in 79 patients (92.9%) with PFNA (P = 0.218). TAD was 7.2 mm (range, 2.1-12.3) in the PFN group, whereas it was 7.9 mm (range, 3.6-14.9) on immediate postoperative radiographs in the PFNA group.
| PFN group | PFNA group | P value | |
| Reduction | 0.830 | ||
| Good, n (%) | 34 (46.6%) | 42 (49.4%), | |
| Normal, n (%) | 31 (42.5%) | 36 (42.4%) | |
| Poor | 8 | 7 | |
| Cleveland Index | 0.577 | ||
| Zone 1 | 0 | 0 | |
| Zone 2 | 1 | 0 | |
| Zone 3 | 0 | 0 | |
| Zone 4 | 2 | 2 | |
| Zone 5 | 34 | 42 | |
| Zone 6 | 11 | 15 | |
| Zone 7 | 3 | 4 | |
| Zone 8 | 14 | 19 | |
| Zone 9 | 8 | 3 | |
| Zone 5 + 6 + 8 + 9, n (%) | 67 (91.8%) | 79 (92.9%) | 0.218 |
| TAD, mm | 7.2 (2.1-12.3) | 7.9 (3.6-14.9) | 0.222 |
| Union rate, % (n) | 87.7 (64/73) | 94.1 (80/85) | 0.155 |
| Union time, wk | 14.9 (12-17) | 13.7 (11-18) | 0.156 |
| Sliding distance, mm | 6.1 (0-23.6) | 3.2 (0-18.4) | 0.036 |
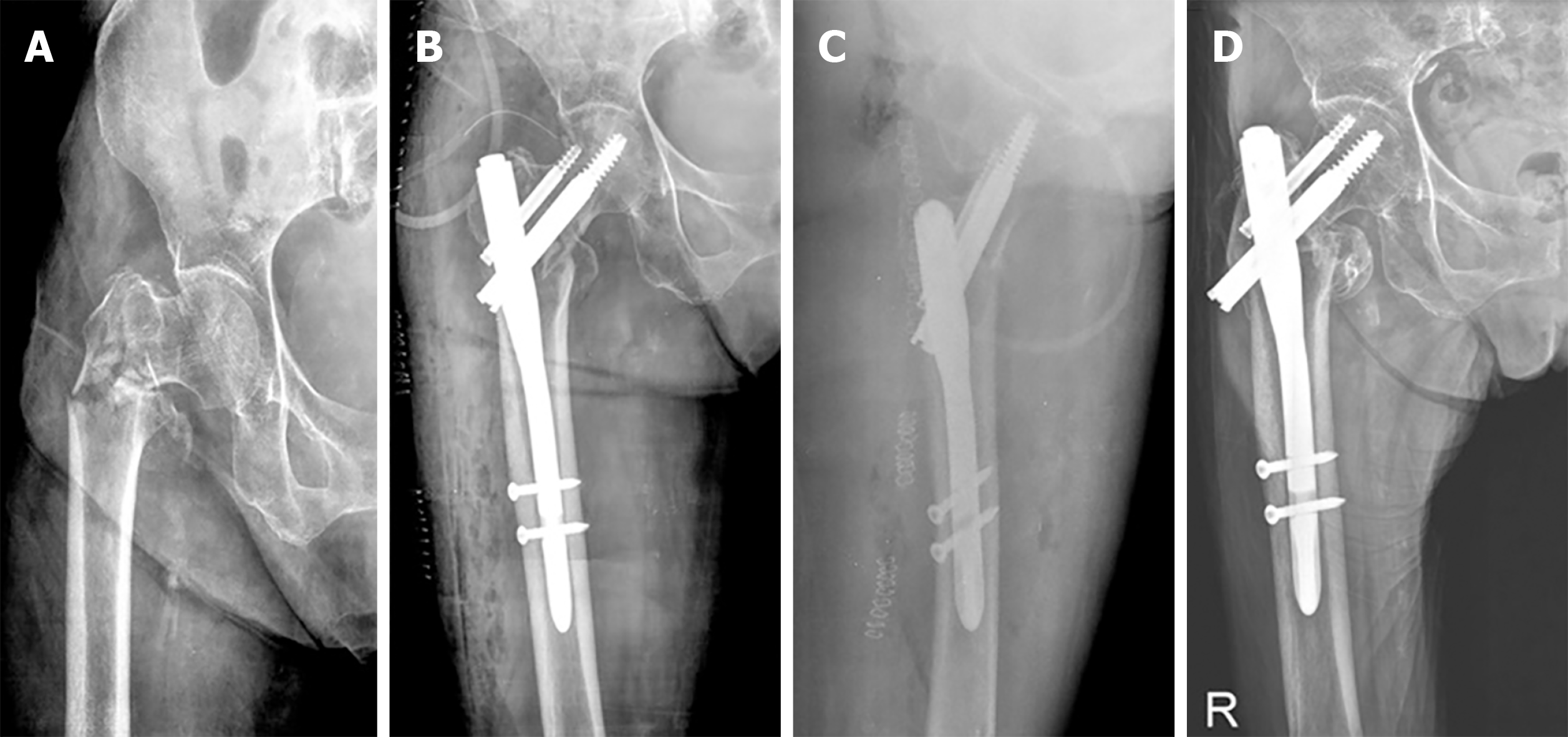
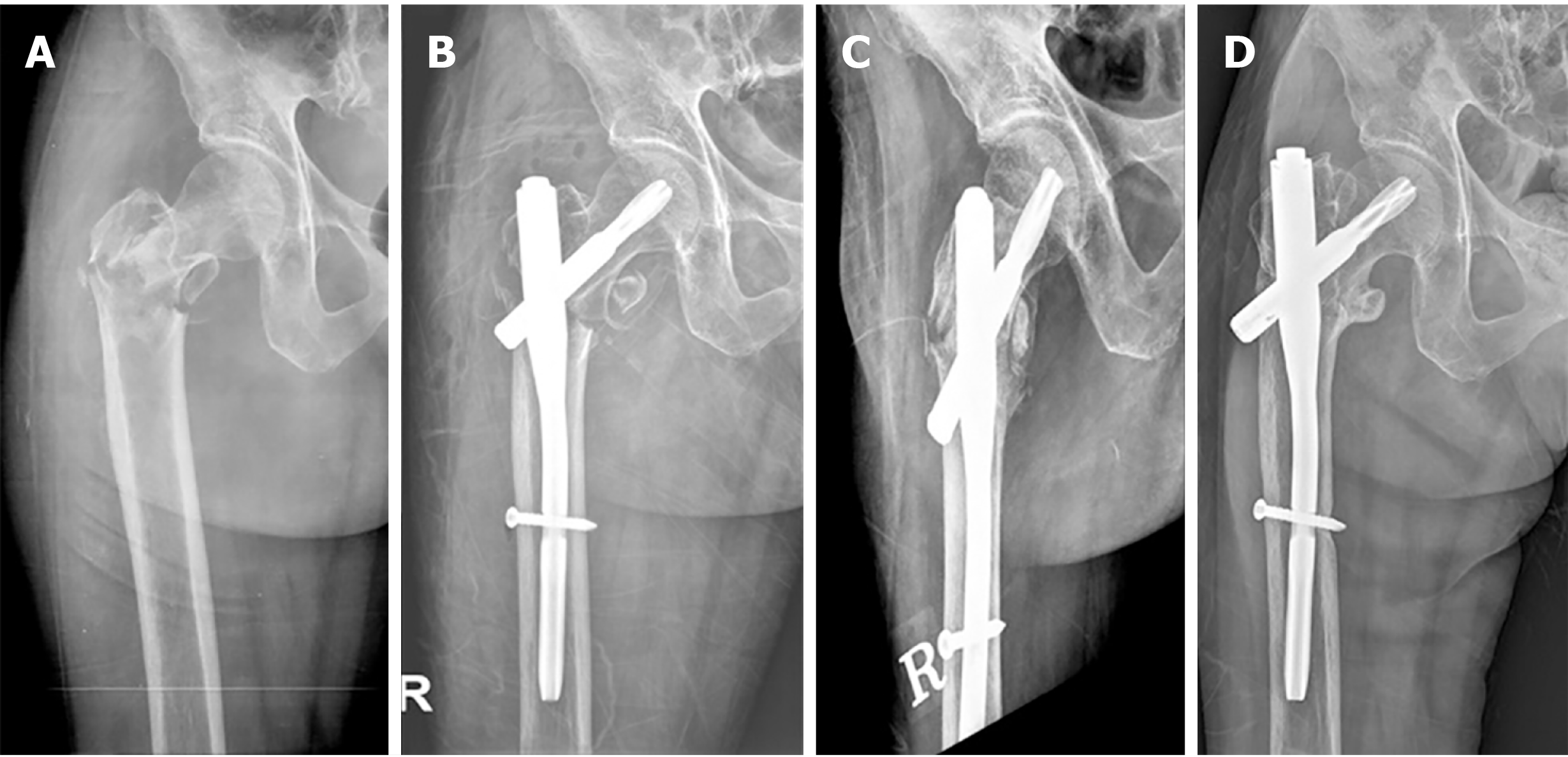
Sliding distance was 6.1 mm (range, 0-23.6 mm) in the PFN group, whereas it was 3.2 mm (range, 0-18.4 mm) in the PFNA group at final follow-up compared to radiographs taken immediately after the index operation. The sliding difference was significantly higher in the PFN group (P = 0.036). There was no difference between the two groups in terms of reduction state, Cleveland Index, TAD, union rate and time to union (Figures 1 and 2).
Screw cutout was demonstrated in eight (11.0%) patients in the PFN group and in two (2.4%) patients in the PFNA group (P = 0.027; Table 4). However, there was no statistical difference between groups in terms of nonunion, infection, osteonecrosis of the femoral head, or implant breakage.
| PFN group | PFNA group | P value | |
| Screw cutout, n (%) | 8 (11.0%) | 2 (2.4%) | 0.027 |
| Nonunion, n (%) | 9 (12.3%) | 5 (5.9%) | 0.155 |
| Infection | 2 | 1 | 0.473 |
| ONFH | 1 | 0 | 0.279 |
| Implant breakage | 1 | 0 | 0.279 |
Among the various implants used for treating proximal femur fracture, PFNA has been developed to overcome several problems of PFN, which has a similar design but uses a helical blade[8,11,12]. According to one biomechanical study, better clinical outcomes might be expected in patients undergoing PFNA than in those receiving the previous-generation PFN[13]. However, few studies have compared the clinical and radiographic outcomes, including cutout after fixation, between PFNA and PFN in elderly patients with PFF. Thus, we performed the current study. Our results indicate that PFNA is associated with better clinical outcomes and fewer complications (in terms of sliding distance and screw cutout) compared to PFN.
In our study, the group that underwent PFNA with a helical blade demonstrated less sliding distance compared to the group undergoing PFN with a conventional screw. This result is comparable with previous studies conducted in the laboratory setting, which demonstrated increased resistance of the blade to implant migration, and an increase in interlocking stability[13,20,21]. In a clinical study comparing the sliding distance between PFN and PFNA groups, Choo et al[22] reported that the sliding distance was shorter in the PFNA group than in the PFN group, which was consistent with our results.
Similar to our study, several studies comparing PFN and PFNA indicated that the PFN group had more implant-related complications[23-25]. We speculate that this result is due to the biomechanical properties of the helical blade of PFNA[13]. As reaming is not performed before blade insertion, the bone stock of the femoral head can be preserved, thereby increasing the contact area between the implant and cancellous bone of the femoral head. In addition, when the blade is inserted, the cancellous bone is compressed, which increases resistance to rotational stress and varus collapse[26]. However, Mallya et al[27] described that there was no difference in implant-related complications between the two groups. We presume that their study was conducted with a short follow-up period of 6 mo; thus, there was no difference between the two groups.
In the present study, the clinical score after surgery was significantly higher in the PFNA group than in the PFN group (P = 0.033). This result is different to previous studies that reported no difference in clinical outcomes between the two groups[22,25,27,28]. We speculate that the decrease in blade sliding had a smaller effect on native hip biomechanics, including offset and limb length, leading to less reduction in walking ability. In addition, decreased sliding might have resulted in less irritation of the iliotibial band and gluteal sling by the blade itself, leading to less pain.
Our study showed no difference in surgical time between the two groups. In contrast to our findings, several studies[22,24,27,28] reported a shortened time of operation with PFNA when compared with PFN due to the simplified surgical steps. We estimated that this discrepancy among studies might originate from the learning curve associated with the initial introduction of PFNA, which could affect operation time.
The current study is limited by its nonrandomized, retrospective nature, as well as the fact that there were no selection criteria applied for each implant. However, the analysis of demographic characteristics and data related to the operation in the two groups did not reveal any confounding factors such as selection bias. Second, our findings cannot reflect long-term clinical outcomes because of the relatively short-term follow-up. However, a high mortality rate within 5 years has been reported in the literature[29]. Lastly, the current study included a relatively small number of patients, which can weaken statistical power. Nevertheless, we believe that our findings are important as when a theoretically improved implant is introduced, comparison with previous implants of a similar design is paramount to determine the value of the new implant.
In conclusion, PFNA using a helical blade demonstrated better clinical and radiographic outcomes in terms of clinical score, cutout, and sliding distance following treatment of PFF in elderly patients. However, a randomized study with longer-term follow-up may be necessary to draw a definitive conclusion.
There are few studies comparing clinical and radiologic outcomes between proximal femoral nail antirotation (PFNA) and previous-generation proximal femoral nail (PFN) in elderly patients with pertrochanteric femoral fracture (PFF).
We evaluated the clinical and radiographic outcomes after fixation with PFN and PFNA for PFF in elderly patients.
From January 2003 to December 2009, seventy-three patients underwent fixation with PFN (PFN group), whereas 85 patients were fixed with PFNA (PFNA group). The mean duration of radiographic follow-up was 2.4 years (range, 1-7 years). The PFN group was composed of 31 men and 42 women with an average age of 76.6 ± 7.3 years. The PFNA group consisted of 37 men and 48 women with an average age of 74.9 ± 7.2 years.
We evaluated each patient’s medical history and converted it to a Charlson Comorbidity Index score and femoral bone mineral density. There was no difference in demographics between the two groups (P > 0.05). Clinical outcome was measured in terms of operation time, postoperative function according to Salvati and Wilson’s hip function rating system and mortality rate within one year. Radiographic evaluation included the reduction state after the operation, the Cleveland Index[19], tip-apex distance (TAD), union rate, time to union and sliding distance of the screw or blade. Complications, including nonunion, screw cutout, infection, osteonecrosis of the femoral head, and implant breakage were also investigated.
The proportion of patients with excellent or good postoperative function was significantly higher in the PFNA group compared to the PFN group (94.1% and 83.6%, respectively, P = 0.033). Differences in operation time and mortality within one year were not significantly different between the two groups (P > 0.05). Sliding distance was 6.1 mm (range, 0-23.6 mm) in the PFN group, and was 3.2 mm (range, 0-18.4 mm) in the PFNA group at final follow-up (P = 0.036). There was no difference between the two groups in terms of reduction state, Cleveland Index, TAD, union rate and time to union. Screw cutout was demonstrated in eight (11.0%) patients in the PFN group and in two (2.4%) patients in the PFNA group (P = 0.027).
PFNA using a helical blade demonstrated better outcomes in terms of clinical score, sliding distance and cutout rate following treatment of PFF in elderly patients than PFN.
A randomized control study with longer-term follow-up may be necessary to draw a definitive conclusion.
We thank Won Kee Lee, PhD for his valuable guidance in the statistical analysis of data, and interpretation of results.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tripathy SK S-Editor: Huang P L-Editor: Webster JR P-Editor: Xing YX
| 1. | Max W, Sinnot P, Kao C, Sung HY, Rice DP. The burden of osteoporosis in California, 1998. Osteoporos Int. 2002;13:493-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 2. | Hornby R, Evans JG, Vardon V. Operative or conservative treatment for trochanteric fractures of the femur. A randomised epidemiological trial in elderly patients. J Bone Joint Surg Br. 1989;71:619-623. [PubMed] |
| 3. | Kyle RF, Cabanela ME, Russell TA, Swiontkowski MF, Winquist RA, Zuckerman JD, Schmidt AH, Koval KJ. Fractures of the proximal part of the femur. Instr Course Lect. 1995;44:227-253. [PubMed] |
| 4. | Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87:1123-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 160] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 5. | Park SR, Kang JS, Kim HS, Lee WH, Kim YH. Treatment of intertrochanteric fracture with the Gamma AP locking nail or by a compression hip screw--a randomised prospective trial. Int Orthop. 1998;22:157-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Sadowski C, Lübbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002;84:372-381. [PubMed] |
| 7. | Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 865] [Cited by in RCA: 879] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 8. | Al-yassari G, Langstaff RJ, Jones JW, Al-Lami M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury. 2002;33:395-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 103] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Min WK, Kim SY, Kim TK, Lee KB, Cho MR, Ha YC, Koo KH. Proximal femoral nail for the treatment of reverse obliquity intertrochanteric fractures compared with gamma nail. J Trauma. 2007;63:1054-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Morihara T, Arai Y, Tokugawa S, Fujita S, Chatani K, Kubo T. Proximal femoral nail for treatment of trochanteric femoral fractures. J Orthop Surg (Hong Kong). 2007;15:273-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Yoo JH, Park JS, Noh KC, Chung KJ, Kim HK, Kang JK, Hwang JH. The Results of Proximal Femoral Nail Antirotation: A Comparative Study with Proximal Femoral Nail. J Korean Hip Soc. 2008;20: :286-292. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Adams CI, Robinson CM, Court-Brown CM, McQueen MM. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma. 2001;15:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 216] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006;37:984-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 135] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 14. | Newey ML, Ricketts D, Roberts L. The AO classification of long bone fractures: an early study of its use in clinical practice. Injury. 1993;24:309-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4325] [Cited by in RCA: 5119] [Article Influence: 165.1] [Reference Citation Analysis (0)] |
| 16. | Salvati EA, Wilson PD Jr. Long-term results of femoral-head replacement. J Bone Joint Surg Am. 1973;55:516-524. [PubMed] |
| 17. | Park YG, Jang S, Ha YC. Incidence, Morbidity and Mortality in Patients Older than 50 Years with Second Hip Fracture in a Jeju Cohort Study. Hip Pelvis. 2014;26:250-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998;87-94. [PubMed] |
| 19. | Cleveland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41-A:1399-1408. [PubMed] |
| 20. | Ito K, Hungerbühler R, Wahl D, Grass R. Improved intramedullary nail interlocking in osteoporotic bone. J Orthop Trauma. 2001;15:192-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 58] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Chinzei N, Hiranaka T, Niikura T, Tsuji M, Kuroda R, Doita M, Kurosaka M. Comparison of the Sliding and Femoral Head Rotation among Three Different Femoral Head Fixation Devices for Trochanteric Fractures. Clin Orthop Surg. 2015;7:291-297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Choo SK, Oh HK, Choi JY. PFNA and PFN in Intertrochanteric Fractures: Comparison Study of Sliding. J Korean Hip Soc. 2010;22:79-85. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Park JH, Lee YS, Park JW, Wang JH, Kim JG. A comparative study of screw and helical proximal femoral nails for the treatment of intertrochanteric fractures. Orthopedics. 2010;33:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Gardenbroek TJ, Segers MJ, Simmermacher RK, Hammacher ER. The proximal femur nail antirotation: an identifiable improvement in the treatment of unstable pertrochanteric fractures? J Trauma. 2011;71:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | Sharma A, Mahajan A, John B. A Comparison of the Clinico-Radiological Outcomes with Proximal Femoral Nail (PFN) and Proximal Femoral Nail Antirotation (PFNA) in Fixation of Unstable Intertrochanteric Fractures. J Clin Diagn Res. 2017;11:RC05-RC09. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 26. | Gavaskar AS, Subramanian M, Tummala NC. Results of proximal femur nail antirotation for low velocity trochanteric fractures in elderly. Indian J Orthop. 2012;46:556-560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Mallya S, Kamath SU, Madegowda A, Krishnamurthy SL, Jain MK, Holla R. Comparison of radiological and functional outcome of unstable intertrochanteric femur fractures treated using PFN and PFNA-2 in patients with osteoporosis. Eur J Orthop Surg Traumatol. 2019;29:1035-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Kashid MR, Gogia T, Prabhakara A, Jafri MA, Shaktawat DS, Shinde G. Comparative study between proximal femoral nail and proximal femoral nail antirotation in management of unstable trochanteric fractures. Int J Res Orthop. 2016;2:354-358. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Müller F, Doblinger M, Kottmann T, Füchtmeier B. PFNA and DHS for AO/OTA 31-A2 fractures: radiographic measurements, morbidity and mortality. Eur J Trauma Emerg Surg. 2019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |