Published online Jan 18, 2020. doi: 10.5312/wjo.v11.i1.57
Peer-review started: June 11, 2019
First decision: September 21, 2019
Revised: September 25, 2019
Accepted: November 25, 2019
Article in press: November 25, 2019
Published online: January 18, 2020
Processing time: 212 Days and 5.3 Hours
With the increasing complexity of surgical interventions performed in orthopaedic trauma surgery and the improving technologies used in three-dimensional (3D) printing, there has been an increased interest in the concept. It has been shown that 3D models allow surgeons to better visualise anatomy, aid in planning and performing complex surgery. It is however not clear how best to utilise the technique and whether this results in better outcomes.
To evaluate the effect of 3D printing used in pre-operative planning in orthopaedic trauma surgery on clinical outcomes.
We performed a comprehensive systematic review of the literature and a meta-analysis. Medline, Ovid and Embase were searched from inception to February 8, 2018. Randomised controlled trials, case-control studies, cohort studies and case series of five patients or more were included across any area of orthopaedic trauma. The primary outcomes were operation time, intra-operative blood loss and fluoroscopy used.
Seventeen studies (922 patients) met our inclusion criteria and were reviewed. The use of 3D printing across all specialties in orthopaedic trauma surgery demonstrated an overall reduction in operation time of 19.85% [95% confidence intervals (CI): (-22.99, -16.71)], intra-operative blood loss of 25.73% [95%CI: (-31.07, -20.40)], and number of times fluoroscopy was used by 23.80% [95%CI: (-38.49, -9.10)].
Our results suggest that the use of 3D printing in pre-operative planning in orthopaedic trauma reduces operative time, intraoperative blood loss and the number of times fluoroscopy is used.
Core tip: The use of three-dimensional (3D) printing in preoperative planning in orthopaedic trauma surgery is a relatively novel field. It has been shown that 3D models allow surgeons to better visualise anatomy, aid in planning and performing complex surgery. It is not clear how to utilise this technique and whether this results in better outcomes. This is the first systematic review and meta-analysis in this field to date. Our results suggest that the use of 3D printing in pre-operative planning in orthopaedic trauma reduces operative time, intraoperative blood loss and the number of times fluoroscopy is used.
- Citation: Morgan C, Khatri C, Hanna SA, Ashrafian H, Sarraf KM. Use of three-dimensional printing in preoperative planning in orthopaedic trauma surgery: A systematic review and meta-analysis. World J Orthop 2020; 11(1): 57-67
- URL: https://www.wjgnet.com/2218-5836/full/v11/i1/57.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i1.57
With the increasing complexity of operations and surgical decision-making, three-dimensional (3D) printing is a novel modality with the potential to make a huge impact in the surgical field. In 1984, the first patent for a 3D printer was filled in the United States by Charles Hall titled, “Apparatus for production of 3D objects by stereolithography”, which was, in effect, the world’s first 3D printer (Patent number: US4575330A). It has been used in a variety of different surgical specialties including plastic surgery, neurosurgery, cardiothoracic surgery, oral and maxillofacial surgery[1,2]. The first reported use in orthopaedics was in 1999 as an aid to pre-operative planning in complex spinal surgery[3].
3D printing also known as “rapid prototyping” or “additive manufacturing” creates a 3D model through different techniques. As opposed to traditional manufacturing techniques that are a “subtractive” process (removing excess material), 3D printing is an “additive” process. This involves creating 3D objects by adding material layer-by-layer. Firstly, a high-resolution computed tomography (CT) scan of the deformity, fracture or defect is required. Computer-aided design (CAD) software then creates a digitalised representation of an object, which is then converted most commonly into a stereolithograpy (STL) file[4]. STL files “cut up” the digitalised model created by the CAD software, allowing the 3D printer to print the object layer by layer[5].
In orthopaedics, the use of 3D printing can be broadly split into three categories. This includes: (1) The use of 3D printing in pre-operative planning; (2) 3D implants; and (3) 3D patient-specific instrumentation (PSI). In pre-operative planning, 3D printed models of the fracture configuration or pathology can allow surgeons to visualise relevant anatomy and help aid executing complex operations, for example in pelvic trauma surgery[6]. 3D printed implants can be used for direct replacement of a large defect after tumour resection and to aid reconstruction in limb-salvage surgery[7]. PSIs have a wide application across orthopaedics and are largely used for more accurate implant placement, especially in the presence of abnormal anatomy and deformities, as well as developing templates for deformity correction and tumour resection[8].
Despite 3D printing being described as the third industrial revolution, the necessary evidence to justify the expanding investment in 3D printing in surgery remains ambiguous. Whilst the concept of 3D printing is favoured, particularly in those countries with advanced economies, its widespread application to daily clinical practice is relatively unknown. As we approach the end of the second decade following the first use of 3D printing in orthopaedics, an overview of this innovation may allow us better understanding of its potential application in every day practice in orthopaedic trauma.
Studies comparing the use of 3D printing with conventional approaches have suggested an improvement in orthopaedic operative outcomes, as measured by blood loss, use of fluoroscopy and operative time[9-11]. However, the systematic assessment and meta-analysis of 3D printing in orthopaedic trauma as a single entity has not been performed. The aim of this comprehensive systematic review and meta-analysis was to draw evidence from all studies across all areas of orthopaedic trauma, irrespective of age and gender, to assess the overall role of 3D printing in orthopaedic preoperative planning and core surgical outcomes. The primary outcome measures in this review were (1) Operation time; (2) Intra-operative blood loss; and (3) Fluoroscopy used.
This study was performed in accordance to PRISMA guidelines for the reporting of systematic reviews[12]. The study protocol was pre-defined and registered on PROSPERO and can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018078429.
This paper included: (1) Full text papers in English language; (2) Humans of any age undergoing orthopaedic trauma procedures; (3) Randomised controlled trials (RCTs), case-control studies, cohort studies and case series of greater than 4 patients in orthopaedic trauma; and (4) Studies reporting the use of 3D printing in preoperative planning in orthopaedic trauma surgery.
Studies were excluded if they were (1) Case reports or case series with less than five patients; (2) Abstract only publication; (3) Involved 3D imaging but not 3D printing during the operative procedure; (4) Involved 3D printing but not preoperative planning; (5) Duplicate data set; (6) Studies assessing the use of 3D printing in manufacturing custom implants and PSI; and (7) Non-trauma (elective) orthopaedic surgery.
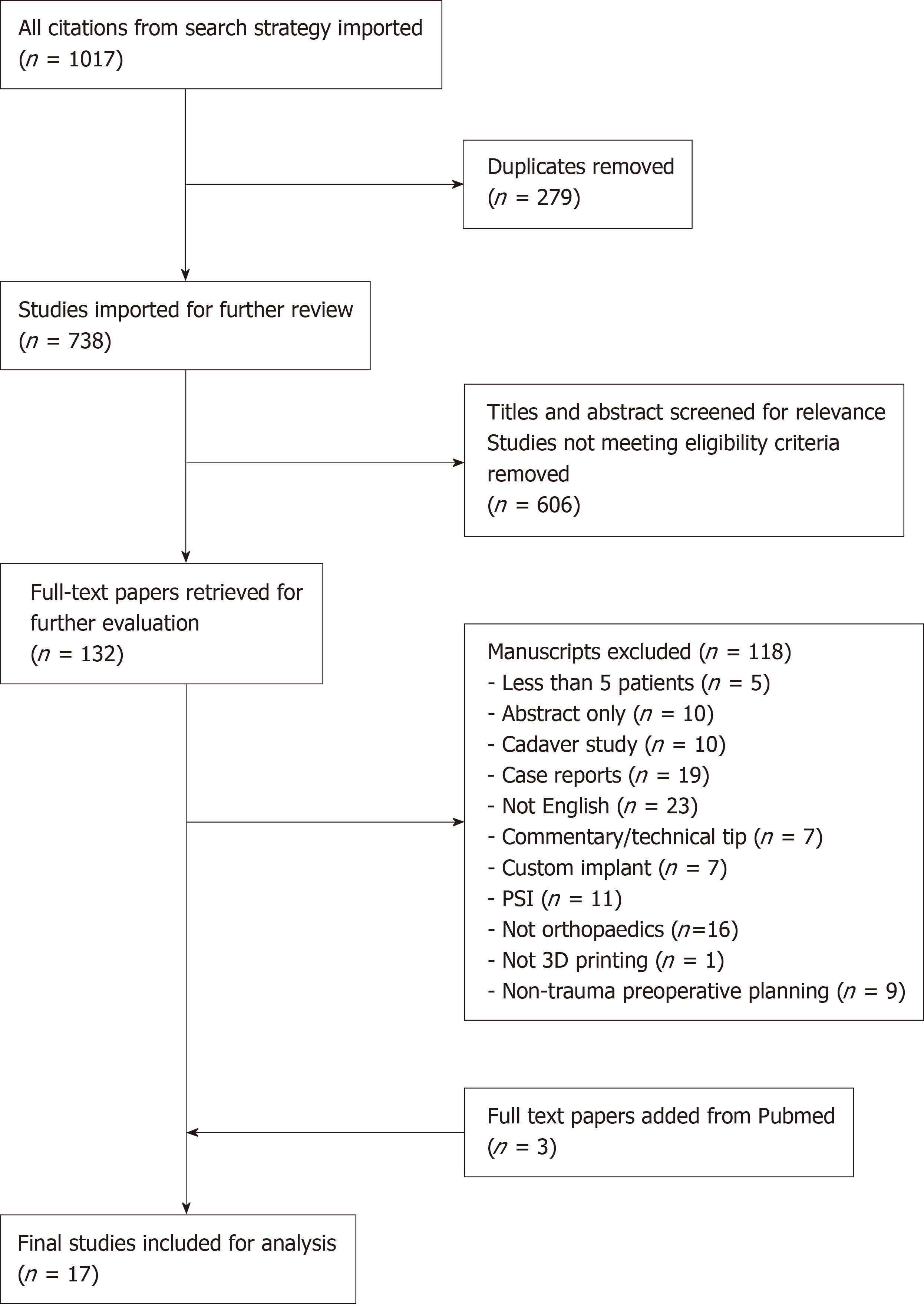
We performed a search of Medline, Ovid and Embase from inception to February, 8 2018 and imported citations into EndNote X7 (New York, United States) reference manager software. Duplicate citations were removed and the remaining citations were screened using title and abstract to match the eligibility criteria. Two authors (Morgan C and Khatri C) independently assessed each paper with discrepancies being resolved with discussion with senior authors (Ashrafian H, Hanna SA, Sarraf K). Additional papers that were appropriate via a manual search were added. The full search strategy can be found in the supplementary materials.
The primary outcome measures in this review were (1) Operation time; (2) Intra-operative blood loss; and (3) Fluoroscopy used.
Data was extracted and entered to Microsoft Excel (Microsoft Cop. Redmond, WA, United States) by two authors (Morgan C and Khatri C). Demographic data was extracted from each paper including year of publication, country of publication and type of 3D printing technology used. Specifically for the participants, the number of participants, age and gender ratio was determined.
Two authors (Morgan C and Khatri C) independently assessed the quality of included papers. For randomised controlled trials, the Jadad score was used[13]. This is a well-validated score that assesses the methodological quality of clinical trials by assessing the randomisation process and blinding the study has used. The Jadad score uses five questions, with a point scale of zero to five. We classified a score of ≥ 3 as “higher quality” and < 3 as “lower quality”. For all other study types, the Newcastle-Ottawa scale was used[14]. This score assesses studies based on three categories: (1) The selection of the study groups; (2) The comparability of the study groups; and (3) The ascertainment of the outcome measure in cohort studies. We classified studies with ≥ 7 stars as “higher quality” and < 7 stars as “lower quality”.
Meta-analysis was performed through the inverse-variance, random-effects model of DerSimonian and Laird for both continuous and categorical outcomes. Continuous outcomes were analysed by calculating the ratio of means for each study, with expression of uncertainty of each result represented by the 95% confidence intervals (CI). We substituted median for mean in studies where only the median was reported[15]. We performed meta-analysis if two or more separate studies were available. This was accomplished using Stata 15 (StataCorp., College Station, TX, United States). The I2 statistic was used to estimate the degree of heterogeneity between studies, where larger values indicate increasing heterogeneity.
Seventeen studies were found that fulfilled the inclusion criteria, producing a data set of 922 patients (Figure 1). Six of these studies were RCTs, two cohort studies (1 prospective, 1 retrospective) and nine case series (8 prospective, 1 retrospective). The area of orthopaedics and type of pathology varied and are shown in Table 1. The overall mean follow up was 18.16 mo. Data from studies with comparison groups that specifically looked at the primary outcomes were included in the meta-analysis.
| Ref. | Yr | Pathology | Area of orthopaedics | Country of study | Design | Newcastle ottawa Score | Jadad score (RCT) | 3DP technology | Total participants | Mean age | % Male |
| Bagaria et al[20] | 2017 | All | Mix | India | Retrospective case series | 1 | FDM | 50 | |||
| Belien et al[21] | 2017 | Os acromiale and acrominal fractures | Upper limb | Belgium | Prospective case series | 3 | STL | 5 | |||
| Chen et al[6] | 2017 | Die-Punch fractures | Upper limb | China | Randomi-sed control trial | 0 | STL | 107 | 28 | 60.7 | |
| Zheng et al[18] | 2017 | Intertrochanteric fracture | Hip | China | Retrospective cohort study | 7 | STL | 39 | 66 | 56.4 | |
| Zheng et al[10] | 2017 | Calcaneal fractures | Lower limb | China | Randomised control trial | 1 | STL | 75 | 45 | 58.7 | |
| Zheng et al[9] | 2018 | Humeral Intercondylar fractures | Upper limb | China | Randomised control trial | 1 | STL | 91 | 44.6 | 53.84 | |
| Yang et al[17] | 2017 | Elbow fractures | Upper limb | China | Randomi-sed control trial | 2 | STL | 40 | 38.6 | 70 | |
| Zhang et al[22] | 2017 | Lower limb fractures | Lower limb | China | Prospective case series | 1 | STL | 78 | 56 | 60.3 | |
| Bizzotto et al[23] | 2016 | Articular fractures | Upper and lower limb | Italy | Prospective case series | 1 | STL | 102 | 44.1 | ||
| Yang et al[16] | 2016 | Trimalleo-lar fractures | Lower limb | China | Randomi-sed control trial | 1 | STL | 30 | 36.5 | 53.3 | |
| Yang et al[24] | 2016 | Lateral tibial plateau fractures | Lower limb | China | Prospective case series | 2 | FDM | 7 | 44 | 42.9 | |
| You et al[11] | 2016 | Proximal humeral fractures | Upper limb | China | Randomised control trial | 2 | 66 | 66 | 40.9 | ||
| Zeng et al[25] | 2016 | Acetabular fracture | Pelvis | China | Prospective case series | 3 | STL | 10 | 50 | ||
| Li et al[19] | 2016 | Tile C pelvic fracture | Pelvis | China | Retrospective cohort study | 5 | 157 | 33 | 67.5 | ||
| Kim et al[26] | 2015 | Midshaft clavicle fractures | Upper limb | China | Prospective case series | 0 | STL | 7 | |||
| Zeng et al[27] | 2015 | Pelvic fracture | Pelvis | China | Prospective case series | 1 | 38 | 32 | 65.8 | ||
| Hurson et al[28] | 2007 | Acetabular fractures | Pelvis | Ireland | Prospective case series | 1 | SLS | 20 |
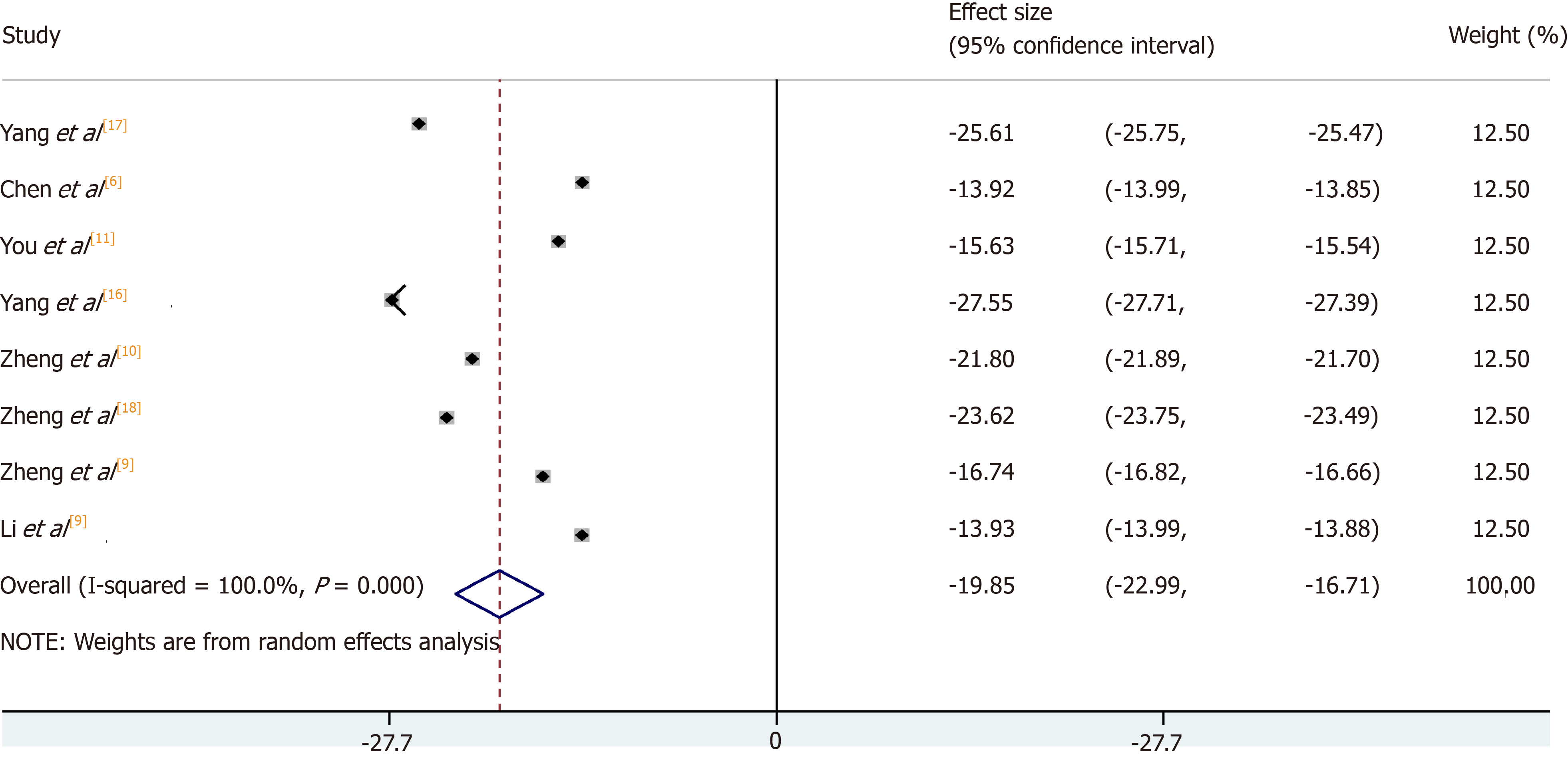
Operation time was measured in eight of these studies; six were RCTs[6,9-11,16-19]. Meta-analysis of these studies confirmed a significant reduction in operation time of 19.85% in the 3D printing group [95%CI: (-22.99, -16.71)] in comparison to the conventional group (see Figure 2). The heterogeneity was high (I2 = 100.0%).
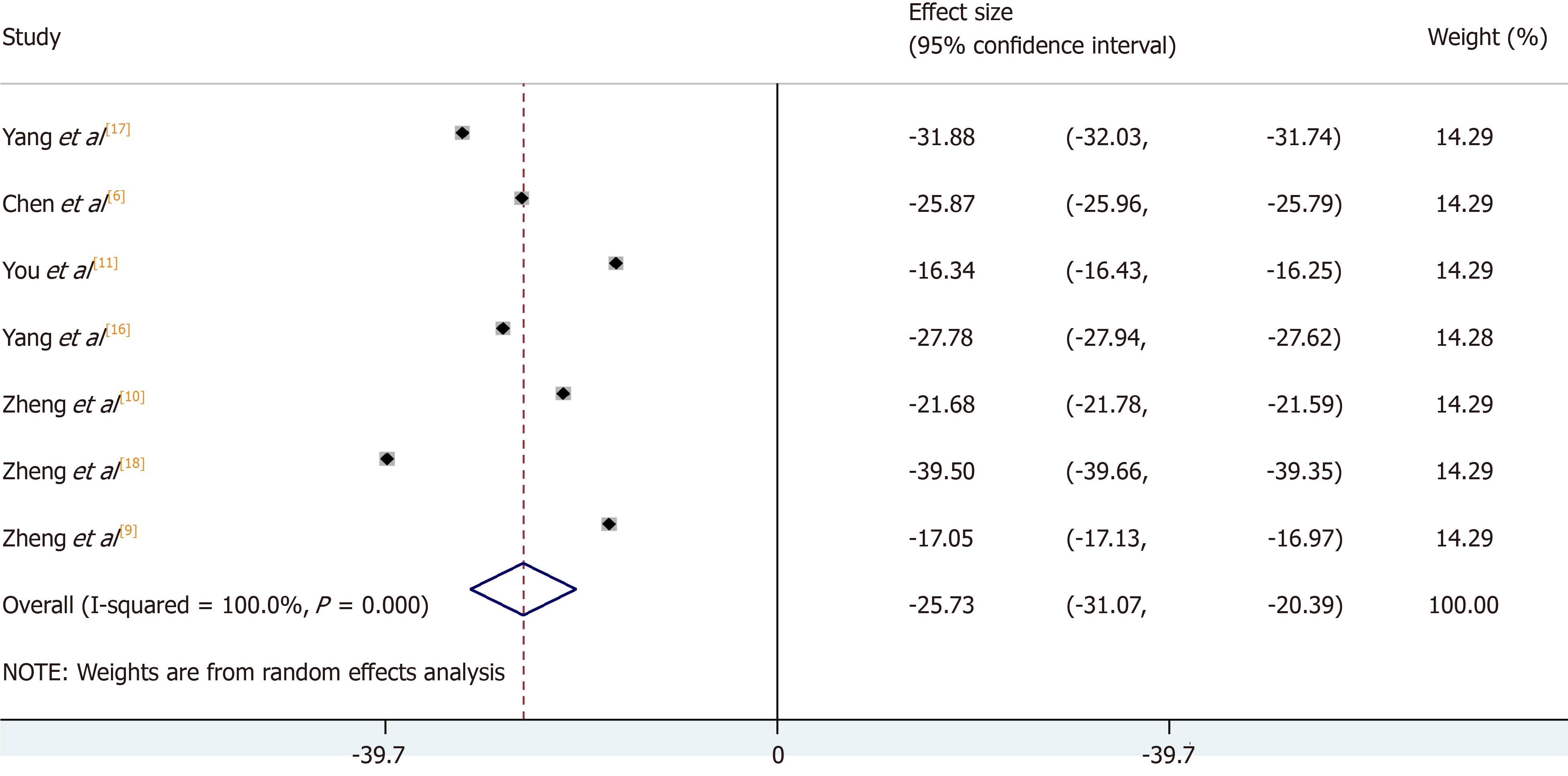
Intra-operative blood loss was investigated in seven studies; six were RCTs[6,9-11,16-18]. Meta-analysis revealed a significant reduction in blood loss of 25.73% (see Figure 3) with the use of 3D printing [95%CI: (-31.07, -20.40)]. The heterogeneity was high (I2 = 100.0%).
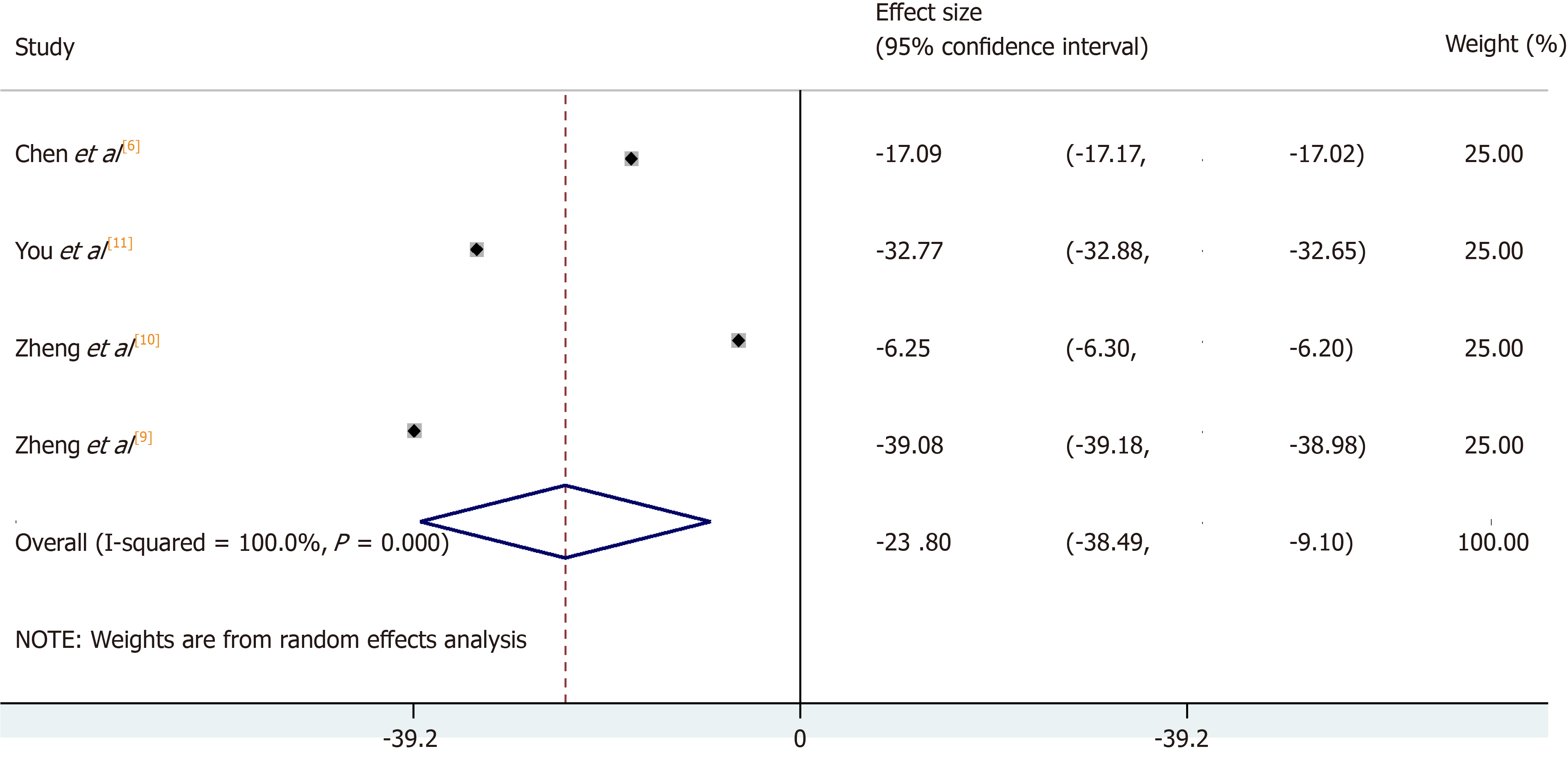
The number of times fluoroscopy was used was measured in four RCTs[6,9-11]. The use of 3D printing led to a significant reduction of 23.80% (see Figure 4) in the number of times fluoroscopy was used [95%CI: (-38.49, -9.10)]. The heterogeneity was high (I2 = 100.0%).
Our analysis demonstrates that the use of 3D printing in preoperative planning in orthopaedic trauma, can lead to a reduction in operation time, intra-operative blood loss and fluoroscopy used. Our systematic review represents the largest and most comprehensive in this area and is the first meta-analysis to date. Although research in the field consists of small-sized studies, findings confirm the current evidence in these studies of the positive effect of 3D printing in preoperative planning.
A shortened operation time of 19.85% with the use of 3D printing confers significant benefits to the patient and costs associated. Increased operative time has been found to be associated with an increased risk of developing post-operative complications, such as wound infections and deep vein thrombosis[29,30]. The reasons behind this are multifactorial and include: (1) the surgeon having a stronger appreciation of pathological anatomy through geometric characterisation by the 3D printed model; as such it allows the surgeon to physically review complex cases. For example, in pelvic surgery it allows the surgeon greater understanding of acetabular fractures and reduces the degree of inter-observer variability in the classification of these injuries[28]; (2) It facilitates pre-operative instrumentation decisions; and (3) Facilitates the planning of the surgical approach[10]; for example in trimalleolar fractures, the surgeon is able to determine the size of the internal fixation plate, clarify the placement position of the plate and screws and prebend the plate according to the morphology of the bone[16]; and (4) The 3D model also enables simulation of the surgery in vitro allowing the surgeon better understanding of fracture reduction, hence leading to a reduction in the operation time (in comparison to the control groups)[11]. Together, these elements of 3D printing that lead to a decreased operative time can translate into cost savings, specifically through decreased staff and operating room overheads. There is evidence to suggest that a decrease in operative time confers cost savings with a 45-min reduction in operation time leading to a saving of almost $2700 per case for a paediatric population[31].
Reducing blood loss and the need for blood transfusion in orthopaedic surgery remains a concern among surgeons and physicians in the perioperative period[32]. Many different methods have been developed including; controlled hypotensive anaesthesia, cell salvage techniques[33], and pharmacological interventions (tranexamic acid)[34]. Our results show a significant reduction in intra-operative blood loss (25.73%) with the use of 3D printing which carries powerful implications for pre- and peri-operative planning and practice especially in the context of trauma. A parallel can be drawn with a reduction in blood loss found with the use of robotic surgery[15]. Reasons studies attributed to the reduction of intra-operative blood loss are similar to those for reduction in operation time (better understanding of pathology and ability to plan the operation). The use of 3D printing in pelvic ring fractures demonstrated a reduced volume of fluid infused intra-operatively, with patients less likely to require a surgical drain or blood transfusion post-operatively[19]. Similar findings were reported with the use of 3D models in elbow fractures, it allowed the plate to be chosen and contoured accurately to ensure optimal compactness with the bone surface[17]. This minimised dissection of the surrounding tissue and protected the blood supply surrounding the fracture fragments, hence reducing intraoperative blood loss.
A small number of studies looked at the number of times intraoperative fluoroscopy was used and overall they reported a reduction in fluoroscopy of 23.80% with the use of 3D printing. This included calcaneal fractures, distal radius fractures and humeral fractures[6,9-11]. A reduction in fluoroscopy carries safety benefits through minimising patient radiation exposure. Radiation exposure remains a significant occupational hazard to the orthopaedic surgeon, radiographers and theatre staff throughout their careers[35] and also to patients subjected to this radiation. Although there is limited literature available on the appropriate amount of intraoperative fluoroscopy use in orthopaedics, a recent paper has reported reference values for common trauma operations[36]. Patient exposure to intraoperative radiation is an important factor to consider especially in the paediatric trauma setting as children are up to ten times more sensitive to radiation damage than adults[37].
An obstacle that exists for the transition of 3D printed models from small studies to large scale clinical practice is cost and production. Creating a 3D printed model, is a complex process requiring advanced computer software and a 3D printer. This process does not come without cost and the need for an experienced team that are familiar with the software. Clinically, not all fractures may require a CT scan, a plain radiograph may suffice, therefore the use of 3D printing may be most useful for complex fractures, for example in pelvic trauma. The cost of printing the model seemed to vary greatly from $2-3 per model to $330[17,38]. There is also the cost of the printer to consider with studies reporting the cost to be $1000-2200[9,31]. In the studies reviewed, the time taken to produce the model ranged from 5 h to 72 h, which is a potential limitation to the use of 3D printing in an acute trauma setting[6,18]. Nevertheless, an important factor to consider is that 3D printing in orthopaedics is a novel field. Therefore, as 3D printing technology progresses both the cost and production time is likely to reduce. Today, the most basic 3D printer for home use can be purchased for less than $200 compared to when 3D printers were first used in the 1980s costing around $300000 (at that time, corresponding to over $750000 in the current era)[39].
A number of studies in this review conducted patient and surgeon questionnaires on 3D printing[6,9,10,17]. It was found that the 3D models improved patient understanding of the fracture and communication with the doctor, leading to higher compliance with post-operative rehabilitation. Patients felt that conventional medical images such as plain radiograph or CT are too complicated to understand, however 3D models allow better visualisation of the fracture[17]. This technology therefore represents a powerful modality to enhance patient empowerment.
The reduction in the total hours worked by surgical trainees has led to an increase in the use of simulation-based training in orthopaedics[40,41], this has been used in fields such as arthroplasty, arthroscopy and trauma surgery[42,43]. With the increase in operative management for complex deformities, using 3D models enables these deformities to be recreated allowing the trainees to learn how to manage these challenging cases through simulation and apply this knowledge to the operating theatre. The advantages of 3D printing therefore have the potential to decrease surgical learning-curves and possibly improve surgical outcomes.
This is the first comprehensive systematic review and meta-analysis conducted on the use of 3D printing in preoperative planning across all types of orthopaedic trauma surgery on core surgical outcomes. It included 17 studies in which six were randomised control trials. However, the results presented here should be considered in the context of a number of limitations. Where meta-analysis was possible, the heterogeneity was high. However, this was not unexpected given the wide area of orthopaedics (where different specialties are highly distinct), type of pathology and patient demographics. It was not possible to carry out a subgroup analysis due to the limited number of studies in the different subspecialties of orthopaedic trauma. A high level of heterogeneity in the absence of any other clear evidence highlights that this scientific field is still in its infancy where its methodology and practices are highly variable, nevertheless the results of this integrated data does indicate the results of clinical effect in the absence of more robust evidence (which is clearly necessary in future studies).
Our focus on operation time, blood loss and number of times fluoroscopy was used was based primarily on the fact that these were the most commonly reported outcomes in the literature. However, these parameters may not fully demonstrate the true value of 3D printing in orthopaedics, parameters such as post-operative function or complications were not determined.
Case series were included to address the paucity of RCTs inevitably introducing other biases associated with this study design and contributing to the heterogeneity. Of note twenty-three of these studies were carried out in China comprising of 81% (745) of the total number of patients. Apart from the randomised control trials, overall the quality scoring of the studies were low, with all 11 studies scoring six or less in the Newcastle-Ottawa Scale. All six of the randomised control trials were of low quality as determined by the Jadad scale. Reasons for low scores include lack of surgeon blinding, which is unlikely to be possible in clinical trials of 3D printing. In many trials, however, the risk of bias relating to sequence generation, adequate follow up, study dropout rate and assessment of outcome was unclear as sufficient information was not available due to poor reporting. The risk of publication bias should also be considered. The number of participants in these studies were small, with the largest being 157, therefore the possibility of “small study effect” cannot be ignored.
In summary, our meta-analysis and systematic review on the use of 3D printing in preoperative planning in orthopaedic trauma suggests that 3D printing reduces operative time, intraoperative blood loss and the number of times fluoroscopy is used. 3D printing is a rapidly evolving field and it allows surgeons to gain better understanding of complex trauma cases and aid in surgical planning. The increased application of this technology has the potential to revolutionise orthopaedic practice and enhance clinical outcomes. There is however the need for an in-depth cost-analysis for the use of 3D printing in surgery, taking into account the production cost vs potential savings made by improved intra-operative outcomes. Further studies, in particular more randomised control trials in similar areas of orthopaedics are required to further enhance our knowledge of the role of 3D printing in orthopaedics and its application to daily clinical practice.
With the increasing complexity of operations and surgical decision-making, three-dimensional (3D) printing is a novel modality with the potential to make a huge impact in the surgical field. In orthopaedics, the use of 3D printing can be broadly split into three categories. This includes: (1) The use of 3D printing in pre-operative planning; (2) 3D implants; and (3) 3D patient-specific instrumentation. In pre-operative planning, 3D printed models of the fracture configuration or pathology can allow surgeons to visualise relevant anatomy and help aid executing complex operations. It is however not clear how best to utilise the technique and whether this results in better outcomes.
The focus of this study is the use of 3D printing in preoperative planning in orthopaedic trauma surgery. Studies comparing the use of 3D printing with conventional approaches have suggested an improvement in orthopaedic operative outcomes, as measured by blood loss, use of fluoroscopy and operative time. However, the systematic assessment and meta-analysis of 3D printing in orthopaedic trauma as a single entity has not been performed. The increased application of this technology has the potential to revolutionize orthopaedic practice and enhance clinical outcomes.
The aim of this research was to draw evidence from all studies across all areas of orthopaedic trauma, irrespective of age and gender, to assess the overall role of 3D printing in orthopaedic preoperative planning and core surgical outcomes. The primary outcome measures in this review were (1) Operation time; (2) Intra-operative blood loss; and (3) Fluoroscopy used.
This study was performed in accordance to PRISMA guidelines for the reporting of systematic reviews. The study protocol was pre-defined and registered on PROSPERO. A search of Medline, Ovid and Embase from inception to February 8, 2018 was carried out and citations were imported into EndNote X7 (New York, United States) reference manager software. Two authors independently assessed the quality of included papers. FFor randomised controlled trials, the Jadad score was used and for all other study types, the Newcastle-Ottawa scale was used. Meta-analysis was performed through the inverse-variance, random-effects model of DerSimonian and Laird for both continuous and categorical outcomes.
Seventeen studies (922 patients) met our inclusion criteria and were reviewed. The use of 3D printing across all specialties in orthopaedic trauma surgery demonstrated an overall reduction in operation time of 19.85% [95% confidence interval (CI): -22.99, -16.71], intra-operative blood loss of 25.73% (95%CI: -31.07, -20.40) and number of times fluoroscopy was used by 23.80% (95%CI: -38.49, -9.10). Overall, the quality of the studies was low and it was not possible to carry out a subgroup analysis due to the limited number of studies in the different subspecialties of orthopaedic trauma.
This meta-analysis and systematic review on the use of 3D printing in preoperative planning in orthopaedic trauma suggests that 3D printing reduces operative time, intraoperative blood loss and the number of times fluoroscopy is used. 3D printing is a rapidly evolving field and it allows surgeons to gain better understanding of complex trauma cases and aid in surgical planning. 3D printing should be considered as an adjunct to improve patient care by minimising operative insult in orthopaedic trauma surgery.
The study highlights the potential impact 3D printing can have in orthopaedic trauma surgery. Further studies, in particular more randomised control trials in similar areas of orthopaedics are required to further enhance our knowledge of the role of 3D printing in orthopaedics and its application to daily clinical practice. There is also the need for an in-depth cost-analysis for the use of 3D printing in surgery, taking into account the production cost vs potential savings made by improved intra-operative outcomes.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Huang AHC, Khajehei M, Lin JA, Xavier-Elsas P, Zhang ZH S-Editor: Tang JZ L-Editor: A E-Editor: Liu MY
| 1. | Giannopoulos AA, Steigner ML, George E, Barile M, Hunsaker AR, Rybicki FJ, Mitsouras D. Cardiothoracic Applications of 3-dimensional Printing. J Thorac Imaging. 2016;31:253-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 98] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 2. | Chae MP, Rozen WM, McMenamin PG, Findlay MW, Spychal RT, Hunter-Smith DJ. Emerging Applications of Bedside 3D Printing in Plastic Surgery. Front Surg. 2015;2:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 196] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 3. | D'Urso PS, Askin G, Earwaker JS, Merry GS, Thompson RG, Barker TM, Effeney DJ. Spinal biomodeling. Spine (Phila Pa 1976). 1999;24:1247-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 67] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Tack P, Victor J, Gemmel P, Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15:115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 811] [Cited by in RCA: 602] [Article Influence: 66.9] [Reference Citation Analysis (0)] |
| 5. | Heller M, Bauer HK, Goetze E, Gielisch M, Roth KE, Drees P, Maier GS, Dorweiler B, Ghazy A, Neufurth M, Müller WE, Schröder HC, Wang X, Vahl CF, Al-Nawas B. Applications of patient-specific 3D printing in medicine. Int J Comput Dent. 2016;19:323-339. [PubMed] |
| 6. | Chen C, Cai L, Zhang C, Wang J, Guo X, Zhou Y. Treatment of Die-Punch Fractures with 3D Printing Technology. J Invest Surg. 2018;31:385-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Ma L, Zhou Y, Zhu Y, Lin Z, Chen L, Zhang Y, Xia H, Mao C. 3D printed personalized titanium plates improve clinical outcome in microwave ablation of bone tumors around the knee. Sci Rep. 2017;7:7626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Ma L, Zhou Y, Zhu Y, Lin Z, Wang Y, Zhang Y, Xia H, Mao C. 3D-printed guiding templates for improved osteosarcoma resection. Sci Rep. 2016;6:23335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 9. | Zheng W, Su J, Cai L, Lou Y, Wang J, Guo X, Tang J, Chen H. Application of 3D-printing technology in the treatment of humeral intercondylar fractures. Orthop Traumatol Surg Res. 2018;104:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Zheng W, Tao Z, Lou Y, Feng Z, Li H, Cheng L, Zhang H, Wang J, Guo X, Chen H. Comparison of the Conventional Surgery and the Surgery Assisted by 3d Printing Technology in the Treatment of Calcaneal Fractures. J Invest Surg. 2018;31:557-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | You W, Liu LJ, Chen HX, Xiong JY, Wang DM, Huang JH, Ding JL, Wang DP. Application of 3D printing technology on the treatment of complex proximal humeral fractures (Neer3-part and 4-part) in old people. Orthop Traumatol Surg Res. 2016;102:897-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17544] [Article Influence: 1096.5] [Reference Citation Analysis (1)] |
| 13. | Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12275] [Cited by in RCA: 12889] [Article Influence: 444.4] [Reference Citation Analysis (1)] |
| 14. | Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8858] [Cited by in RCA: 12669] [Article Influence: 844.6] [Reference Citation Analysis (0)] |
| 15. | Tan A, Ashrafian H, Scott AJ, Mason SE, Harling L, Athanasiou T, Darzi A. Robotic surgery: disruptive innovation or unfulfilled promise? A systematic review and meta-analysis of the first 30 years. Surg Endosc. 2016;30:4330-4352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 16. | Yang L, Shang XW, Fan JN, He ZX, Wang JJ, Liu M, Zhuang Y, Ye C. Application of 3D Printing in the Surgical Planning of Trimalleolar Fracture and Doctor-Patient Communication. Biomed Res Int. 2016;2016:2482086. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Yang L, Grottkau B, He Z, Ye C. Three dimensional printing technology and materials for treatment of elbow fractures. Int Orthop. 2017;41:2381-2387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Zheng SN, Yao QQ, Mao FY, Zheng PF, Tian SC, Li JY, Yu YF, Liu S, Zhou J, Hu J, Xu Y, Tang K, Lou Y, Wang LM. Application of 3D printing rapid prototyping-assisted percutaneous fixation in the treatment of intertrochanteric fracture. Exp Ther Med. 2017;14:3644-3650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Li B, Chen B, Zhang Y, Wang X, Wang F, Xia H, Yin Q. Comparative use of the computer-aided angiography and rapid prototyping technology versus conventional imaging in the management of the Tile C pelvic fractures. Int Orthop. 2016;40:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Bagaria V, Chaudhary K. A paradigm shift in surgical planning and simulation using 3Dgraphy: Experience of first 50 surgeries done using 3D-printed biomodels. Injury. 2017;48:2501-2508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 21. | Beliën H, Biesmans H, Steenwerckx A, Bijnens E, Dierickx C. Prebending of osteosynthesis plate using 3D printed models to treat symptomatic os acromiale and acromial fracture. J Exp Orthop. 2017;4:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Zhang W, Ji Y, Wang X, Liu J, Li D. Can the recovery of lower limb fractures be achieved by use of 3D printing mirror model? Injury. 2017;48:2485-2495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Bizzotto N, Tami I, Santucci A, Adani R, Poggi P, Romani D, Carpeggiani G, Ferraro F, Festa S, Magnan B. 3D Printed replica of articular fractures for surgical planning and patient consent: a two years multi-centric experience. 3D Print Med. 2015;2:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 24. | Yang P, Du D, Zhou Z, Lu N, Fu Q, Ma J, Zhao L, Chen A. 3D printing-assisted osteotomy treatment for the malunion of lateral tibial plateau fracture. Injury. 2016;47:2816-2821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Zeng C, Xing W, Wu Z, Huang H, Huang W. A combination of three-dimensional printing and computer-assisted virtual surgical procedure for preoperative planning of acetabular fracture reduction. Injury. 2016;47:2223-2227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 111] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 26. | Kim HN, Liu XN, Noh KC. Use of a real-size 3D-printed model as a preoperative and intraoperative tool for minimally invasive plating of comminuted midshaft clavicle fractures. J Orthop Surg Res. 2015;10:91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 27. | Zeng C, Xiao J, Wu Z, Huang W. Evaluation of three-dimensional printing for internal fixation of unstable pelvic fracture from minimal invasive para-rectus abdominis approach: a preliminary report. Int J Clin Exp Med. 2015;8:13039-13044. [PubMed] |
| 28. | Hurson C, Tansey A, O'Donnchadha B, Nicholson P, Rice J, McElwain J. Rapid prototyping in the assessment, classification and preoperative planning of acetabular fractures. Injury. 2007;38:1158-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 129] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 29. | Daley BJ, Cecil W, Clarke PC, Cofer JB, Guillamondegui OD. How slow is too slow? Correlation of operative time to complications: an analysis from the Tennessee Surgical Quality Collaborative. J Am Coll Surg. 2015;220:550-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 236] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 30. | Kim JY, Khavanin N, Rambachan A, McCarthy RJ, Mlodinow AS, De Oliveria GS, Stock MC, Gust MJ, Mahvi DM. Surgical duration and risk of venous thromboembolism. JAMA Surg. 2015;150:110-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 243] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 31. | Cherkasskiy L, Caffrey JP, Szewczyk AF, Cory E, Bomar JD, Farnsworth CL, Jeffords M, Wenger DR, Sah RL, Upasani VV. Patient-specific 3D models aid planning for triplane proximal femoral osteotomy in slipped capital femoral epiphysis. J Child Orthop. 2017;11:147-153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 32. | Ponnusamy KE, Kim TJ, Khanuja HS. Perioperative blood transfusions in orthopaedic surgery. J Bone Joint Surg Am. 2014;96:1836-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 123] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 33. | Sharrock NE, Mineo R, Urquhart B, Salvati EA. The effect of two levels of hypotension on intraoperative blood loss during total hip arthroplasty performed under lumbar epidural anesthesia. Anesth Analg. 1993;76:580-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Poeran J, Rasul R, Suzuki S, Danninger T, Mazumdar M, Opperer M, Boettner F, Memtsoudis SG. Tranexamic acid use and postoperative outcomes in patients undergoing total hip or knee arthroplasty in the United States: retrospective analysis of effectiveness and safety. BMJ. 2014;349:g4829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 332] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 35. | Giordano BD, Grauer JN, Miller CP, Morgan TL, Rechtine GR 2nd. Radiation exposure issues in orthopaedics. J Bone Joint Surg Am. 2011;93:e69(1-e610). [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 36. | Rashid MS, Aziz S, Haydar S, Fleming SS, Datta A. Intra-operative fluoroscopic radiation exposure in orthopaedic trauma theatre. Eur J Orthop Surg Traumatol. 2018;28:9-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 37. | Furlow B. Radiation protection in pediatric imaging. Radiol Technol. 2011;82:421-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 38. | Yang JC, Ma XY, Xia H, Wu ZH, Ai FZ, Zhang K, Yin QS. Clinical application of computer-aided design-rapid prototyping in C1-C2 operation techniques for complex atlantoaxial instability. J Spinal Disord Tech. 2014;27:E143-E150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 39. | Hoang D, Perrault D, Stevanovic M, Ghiassi A. Surgical applications of three-dimensional printing: a review of the current literature & how to get started. Ann Transl Med. 2016;4:456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 180] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 40. | Palan J, Roberts V, Bloch B, Kulkarni A, Bhowal B, Dias J. The use of a virtual learning environment in promoting virtual journal clubs and case-based discussions in trauma and orthopaedic postgraduate medical education: the Leicester experience. J Bone Joint Surg Br. 2012;94:1170-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | Sonnadara RR, Van Vliet A, Safir O, Alman B, Ferguson P, Kraemer W, Reznick R. Orthopedic boot camp: examining the effectiveness of an intensive surgical skills course. Surgery. 2011;149:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 42. | Coughlin RP, Pauyo T, Sutton JC, Coughlin LP, Bergeron SG. A Validated Orthopaedic Surgical Simulation Model for Training and Evaluation of Basic Arthroscopic Skills. J Bone Joint Surg Am. 2015;97:1465-1471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 43. | Sugand K, Mawkin M, Gupte C. Validating Touch Surgery™: A cognitive task simulation and rehearsal app for intramedullary femoral nailing. Injury. 2015;46:2212-2216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (1)] |