Published online Aug 18, 2019. doi: 10.5312/wjo.v10.i8.299
Peer-review started: March 15, 2019
First decision: June 12, 2019
Revised: June 27, 2019
Accepted: July 23, 2019
Article in press: July 23, 2019
Published online: August 18, 2019
Processing time: 157 Days and 12.2 Hours
Tibial shaft fractures are common injuries among the pediatric and adolescent population. Conservative treatment remains the preferred treatment. However, over the last two decades, there has been an increasing trend of operative fixation in pediatric tibia fractures, commonly with intramedullary nail fixation (IMN). Elastic stable intramedullary nails (ESIN) are heavily used especially in skeletally immature patients as they are physeal respecting and the technique for insertion is familiar. Alternatively, reamed locked intramedullary nails (RIMN) have gained traction in adolescents and skeletally immature pre-adolescents. When identifying publications germane to intramedullary fixation of pediatric tibia fractures, the majority investigated clinical and radiographic outcomes associated with ESIN. We were able to identify only one study specifically examining RIMN in this population, albeit other studies included patients treated with RIMN. In parallel, there has been considerable progress in the field of skeletal maturity estimation with criteria based on different anatomic regions. However, little data exists for trauma purposes as no gold standard system had been accepted and proven to be precise for determination of potential growth remaining around the knee or for quantifying the risk of damage to the proximal tibial physis. Systems devised have been either unvalidated or unnecessarily complex or both. In order to achieve more informed treatment choices and optimal patient outcomes when using IMN fixation in pediatrics, simple to use, validated plain film-based methodology is needed to define skeletal maturity for the proximal tibia. Additionally, further examination of outcomes and the role of RIMN in this population are warranted.
Core tip: Little data exists to support the use of reamed intramedullary nails (RIMN) in adolescents and skeletally immature pre-adolescents. However, RIMN is used as the cornerstone of fixation for skeletally mature patients and older skeletally immature patients. Although we are not aware of any papers or case reports of RIMN use which resulted in growth arrest or recurvatum deformity in the pediatric population, surgeons are reluctant to use this nail design in younger patients. Clinical data regarding RIMN and a reliable and easy to apply skeletal maturity measure for the proximal tibia are needed for better decision making in such cases.
- Citation: Weltsch D, Baldwin KD. Rigid locked nail fixation for pediatric tibia fractures - Where are the data? World J Orthop 2019; 10(8): 299-303
- URL: https://www.wjgnet.com/2218-5836/full/v10/i8/299.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i8.299
Tibial shaft fractures are the third most common pediatric fracture[1,2]. They represent the second most common reason for orthopedic inpatient admission to children’s hospitals[3-6].
Conservative treatment with closed reduction and cast immobilization remains the treatment modality of choice in children and adolescents with tibial shaft fractures[2,7-14]. In cases were the fracture pattern is assumed to be length unstable, open, or with soft tissue not amenable to casting, operative fixation may be chosen as the preferred treatment strategy[6,15].
Over the last two decades, there has been an increasing trend toward operative fixation in pediatric tibia fractures. Currently, tibia fractures account for 12% of all surgically managed pediatric fractures[1,2]. An intramedullary strategy is a commonly employed technique for tibial fracture fixation in children as it confers a bridge fixation with a long working length and encourages callus formation[4,5,9]. In the early 1980s, Ligier et al[16] reported that of placement of two curved rods in a straight bone would produce forces which opposed one another and obtain and maintain reduction of that bone. Their work in Nancy region of France and their publications[17,18] had popularized the usage of their elastic nails “Nancy nails” all around the world. Even today, elastic nails are an attractive option as they avoid physeal violation and offer a familiar technique to pediatric orthopedists that can be performed quickly and safely[2,4,6,11,19]. However, elastic stable intramedullary nails (ESIN) are theorized to provide a non-optimal solution for length unstable fracture patterns[19]. Additionally, as children become larger and more “adult-like” elastic nails may provide less reliable results. The transition in the age where this occurs is currently unclear. As such, many clinicians transition to more adult style fixation as the child ages, and tibia fractures are no different.
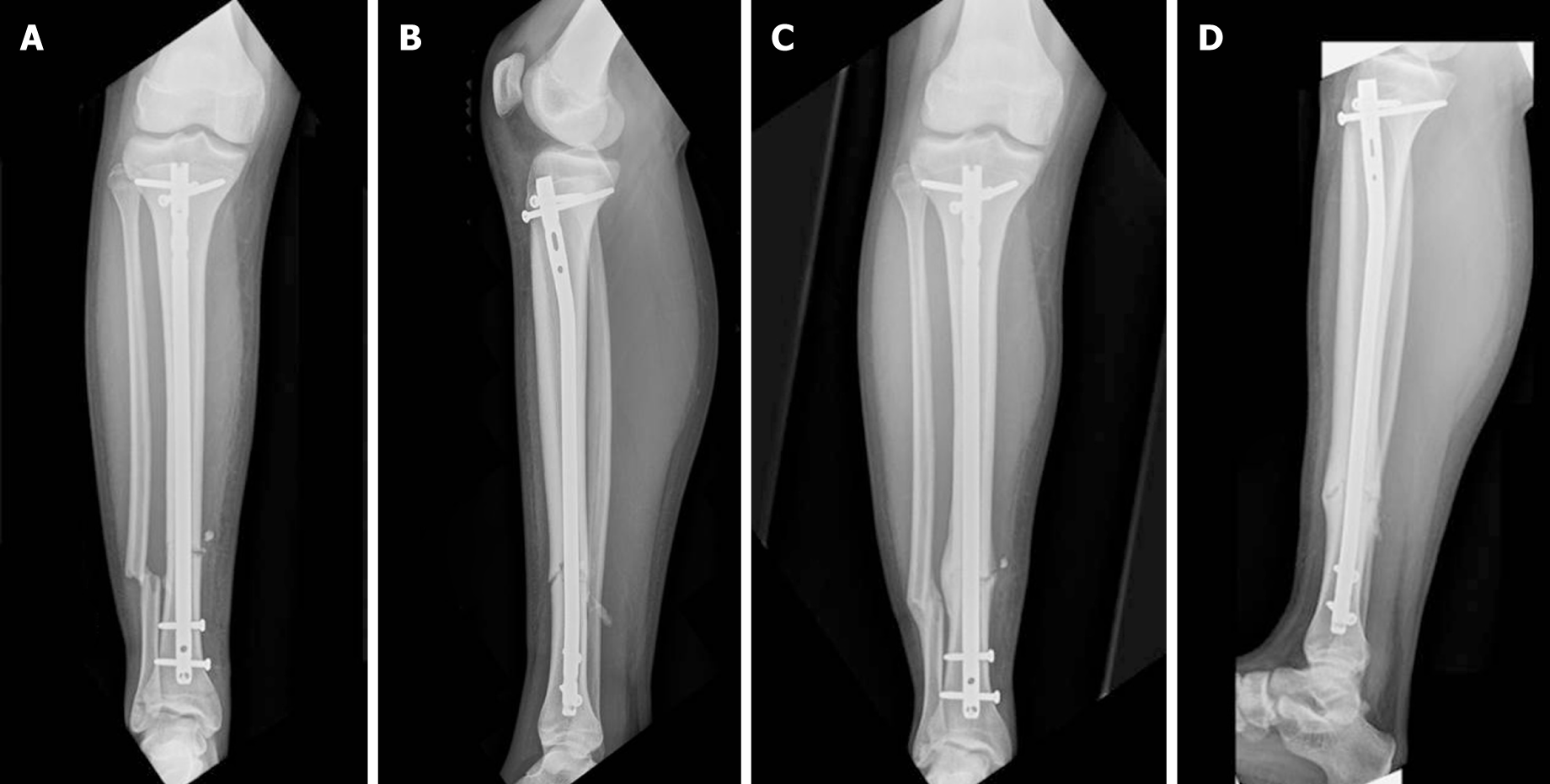
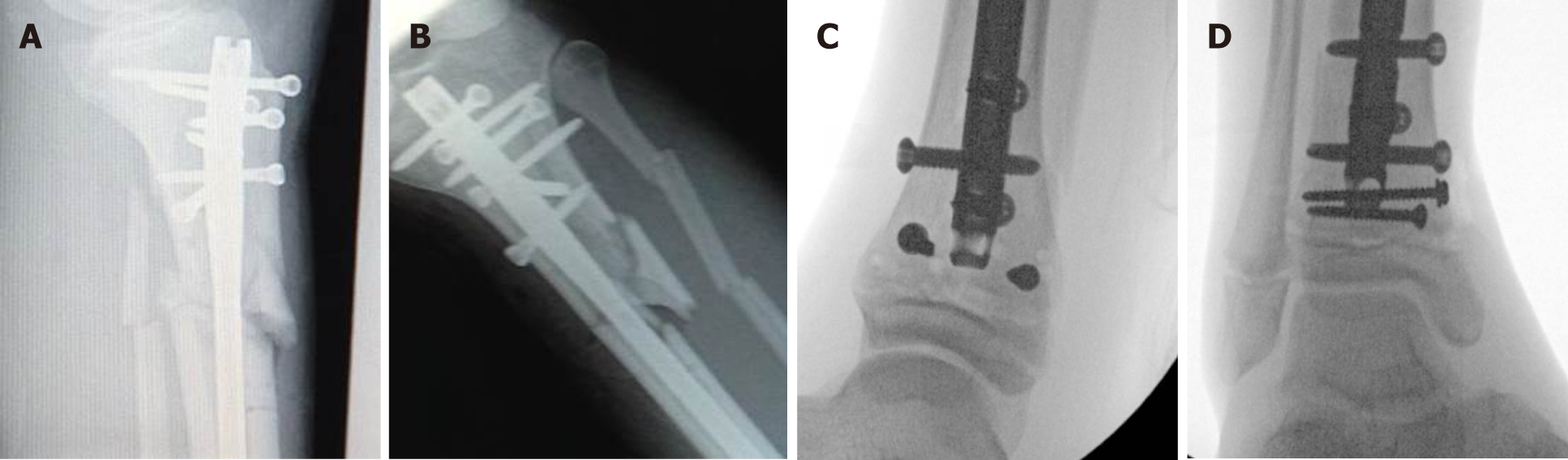
A rigid, locked nail (Figure 1) also termed reamed intramedullary nail (RIMN) confers rotational stability and adds the ability to treat more proximal and distal fractures via the usage of blocking screws and other advanced nailing strategies (Figure 2). Additionally, weight bearing may be allowed sooner than with ESIN, and hardware may need to be removed less often[5,6,9,11,19-22]. The insertion technique of RIMN however, adds risk for growth arrest at the proximal tibial physis and thus theoretically the risk of late recurvatum deformity in the sagittal plane[2,9,15,19,22].
Many studies have already evaluated the indications, techniques, and outcomes regarding the usage of elastic nails to treat these fractures. Perhaps surprisingly, a single study was identified examining the results of RIMN in pediatric patients. This study from the United Kingdom included 53 patients aged 13-16 years, treated with RIMN for tibial shaft fractures. Among these patients, thirty-six of these adolescent patients had open tibial physes at the time of intramedullary nailing. All 36 patients were re-imaged between 2 and 12 years after treatment to examine the effect of intramedullary nailing on tibial growth. The researchers reported excellent results with 100% union rates and no evidence of tibial shortening or partial growth arrest of the proximal tibial physis[23]. Although a low level of evidence, the study is at least suggestive that this approach is safe at short term follow up. The treatment of choice for the intramedullary strategy in many children, particularly in patients in the midst of the adolescent growth phase remains unclear. This lone article suggests that no appreciable growth arrest will occur, but we currently cannot say with confidence that there is no risk. Additionally, no reliable method exists to estimate skeletal maturity based on a tibia film, which renders retrospective study of this question difficult if not impossible.
There has been considerable progress in the field of skeletal maturity, and many methods exist to estimate growth remaining. Sanders published many studies on the subject, particularly as it relates to the estimation of scoliosis progression as it relates to growth centers in the shoulder and hand[24,25]. Similar data are not available in an accessible form for the knee to assess growth or growth arrest. Systems for estimating growth around the knee are either MRI based[26], non-validated, or too complex to be accessible to the average orthopedist[27,28]. As such, no gold standard system had been adopted to be precise for determination of potential growth remaining around the knee or for quantifying the risk of damaging the proximal physis. Currently orthopedists may use the fluoroscopy found in the OR to screen their patient’s hand for a gross assessment of general skeletal maturity. However even with this screening tool, no clinical data exists to guide the decision of “when is too young” to perform RIMN.
It is in our belief that the use of plain-film X-ray specifically around the knee joint, with new and improved skeletal maturity prediction methods (most probably based on the proximal tibia changes during maturation), would result in a more accurate estimation of skeletal maturity in this area. This in turn, could lead to a better understanding of the potential for harm in violation of the proximal tibial physis, at various stages of development. Creating such classification may also allow a common language when studying the question or consulting a colleague in a clinical scenario. Using this method, tibias treated with RIMN could be assessed retrospectively and assessed for growth arrest by the age estimated by the X-ray. In this fashion, a clearer picture could be obtained regarding which nail design to employ at a given development level of the child. The evidence-based clarifications and comparison between the type of nails would help us view the broader picture of using IMN fixation in pediatrics and will allow better treatment choices and more optimal patient outcomes.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nobile S S-Editor: Gong ZM L-Editor: A E-Editor: Liu JH
| 1. | Ward WT, Rihn JA. The impact of trauma in an urban pediatric orthopaedic practice. J Bone Joint Surg Am. 2006;88:2759-2764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 2. | Pennock AT, Bastrom TP, Upasani VV. Elastic Intramedullary Nailing Versus Open Reduction Internal Fixation of Pediatric Tibial Shaft Fractures. J Pediatr Orthop. 2017;37:e403-e408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Galano GJ, Vitale MA, Kessler MW, Hyman JE, Vitale MG. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop. 2005;25:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Srivastava AK, Mehlman CT, Wall EJ, Do TT. Elastic stable intramedullary nailing of tibial shaft fractures in children. J Pediatr Orthop. 2008;28:152-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Griffet J, Leroux J, Boudjouraf N, Abou-Daher A, El Hayek T. Elastic stable intramedullary nailing of tibial shaft fractures in children. J Child Orthop. 2011;5:297-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Goodbody CM, Lee RJ, Flynn JM, Sankar WN. Titanium Elastic Nailing for Pediatric Tibia Fractures: Do Older, Heavier Kids Do Worse? J Pediatr Orthop. 2016;36:472-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Shannak AO. Tibial fractures in children: follow-up study. J Pediatr Orthop. 1988;8:306-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 76] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Rickert KD, Hosseinzadeh P, Edmonds EW. What's New in Pediatric Orthopaedic Trauma: The Lower Extremity. J Pediatr Orthop. 2018;38:e434-e439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 9. | Sankar WN, Jones KJ, David Horn B, Wells L. Titanium elastic nails for pediatric tibial shaft fractures. J Child Orthop. 2007;1:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Mashru RP, Herman MJ, Pizzutillo PD. Tibial shaft fractures in children and adolescents. J Am Acad Orthop Surg. 2005;13:345-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 87] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Canavese F, Botnari A, Andreacchio A, Marengo L, Samba A, Dimeglio A, Pereira B, Mansour M, Rousset M. Displaced Tibial Shaft Fractures With Intact Fibula in Children: Nonoperative Management Versus Operative Treatment With Elastic Stable Intramedullary Nailing. J Pediatr Orthop. 2016;36:667-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Ho CA. Tibia Shaft Fractures in Adolescents: How and When Can They be Managed Successfully With Cast Treatment? J Pediatr Orthop. 2016;36 Suppl 1:S15-S18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Thompson GH, Wilber JH, Marcus RE. Internal fixation of fractures in children and adolescents. A comparative analysis. Clin Orthop Relat Res. 1984;10-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Kinney MC, Nagle D, Bastrom T, Linn MS, Schwartz AK, Pennock AT. Operative Versus Conservative Management of Displaced Tibial Shaft Fracture in Adolescents. J Pediatr Orthop. 2016;36:661-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Karaman I, Halici M, Kafadar IH, Guney A, Oner M, Gurbuz K, Karaman ZF. Mid-term results of the elastic intramedullary nailing in paediatric long bone shaft fractures: a prospective study of 102 cases. J Pediatr Orthop B. 2014;23:212-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 16. | Ligier JN, Metaizeau JP, Prévot J. [Closed flexible medullary nailing in pediatric traumatology]. Chir Pediatr. 1983;24:383-385. [PubMed] |
| 17. | Ligier JN, Metaizeau JP, Prévot J, Lascombes P. Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br. 1988;70:74-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 201] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Metaizeau JP. Stable elastic intramedullary nailing for fractures of the femur in children. J Bone Joint Surg Br. 2004;86:954-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 66] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Pandya NK, Edmonds EW. Immediate intramedullary flexible nailing of open pediatric tibial shaft fractures. J Pediatr Orthop. 2012;32:770-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Kubiak EN, Egol KA, Scher D, Wasserman B, Feldman D, Koval KJ. Operative treatment of tibial fractures in children: are elastic stable intramedullary nails an improvement over external fixation? J Bone Joint Surg Am. 2005;87:1761-1768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Bone LB, Sucato D, Stegemann PM, Rohrbacher BJ. Displaced isolated fractures of the tibial shaft treated with either a cast or intramedullary nailing. An outcome analysis of matched pairs of patients. J Bone Joint Surg Am. 1997;79:1336-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 75] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Metaizeau JD, Denis D. Update on leg fractures in paediatric patients. Orthop Traumatol Surg Res. 2019;105:S143-S151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Court-Brown CM, Byrnes T, McLaughlin G. Intramedullary nailing of tibial diaphyseal fractures in adolescents with open physes. Injury. 2003;34:781-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF, Arnold KD, McConnell SJ, Bauman JA, Finegold DN. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90:540-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 264] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 25. | Li DT, Cui JJ, DeVries S, Nicholson AD, Li E, Petit L, Kahan JB, Sanders JO, Liu RW, Cooperman DR, Smith BG. Humeral Head Ossification Predicts Peak Height Velocity Timing and Percentage of Growth Remaining in Children. J Pediatr Orthop. 2018;38:e546-e550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Pennock AT, Bomar JD, Manning JD. The Creation and Validation of a Knee Bone Age Atlas Utilizing MRI. J Bone Joint Surg Am. 2018;100:e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 27. | Knapik DM, Sanders JO, Gilmore A, Weber DR, Cooperman DR, Liu RW. A quantitative method for the radiological assessment of skeletal maturity using the distal femur. Bone Joint J. 2018;100-B:1106-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 28. | O'Connor JE, Coyle J, Spence LD, Last J. Epiphyseal maturity indicators at the knee and their relationship to chronological age: results of an Irish population study. Clin Anat. 2013;26:755-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |