Published online Jul 18, 2019. doi: 10.5312/wjo.v10.i7.278
Peer-review started: February 15, 2019
First decision: April 16, 2019
Revised: May 10, 2019
Accepted: June 25, 2019
Article in press: June 25, 2019
Published online: July 18, 2019
Processing time: 155 Days and 10.4 Hours
Platelet-rich plasma (PRP) is an increasingly used biologic adjunct for muscle injuries, as it is thought to expedite healing. Despite its widespread use, little is known regarding the mechanisms by which PRP produces its efficacious effects in some patients.
To clarify the effects of PRP on muscular pathologies at the cellular and tissue levels by evaluating the basic science literature.
A systematic review of PubMed/MEDLINE and EMBASE databases was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and checklist. Level III in vivo and in vitro studies examining PRP effects on muscles, myocytes and/or myoblasts were eligible for inclusion. Extracted data included PRP preparation methods and study results.
Twenty-three studies were included (15 in vivo, 6 in vitro, 2 in vitro/in vivo). Only one reported a complete PRP cytology (platelets, and red and white blood cell counts). Five in vitro studies reported increased cellular proliferation, four reported increased gene expression, and three reported increased cellular differentiation. Five in vivo studies reported increased gene expression, three reported superior muscle regeneration, and seven reported improved histological quality of muscular tissue.
The basic science literature on the use of PRP in muscle pathology demonstrates that PRP treatment confers several potentially beneficial effects on healing in comparison to controls. Future research is needed to determine optimal cytology, dosing, timing, and delivery methods of PRP for muscle pathologies.
Core tip: Platelet-rich plasma (PRP) has gained much attention in the treatment of muscle injuries for its potential beneficial effects in both operative and non-operative settings without knowledge of its mechanism of action. The current systematic review synthesizes the effects of PRP at the basic science level. PRP was found to induce cellular proliferation and differentiation, the production of various growth factors, muscle regeneration, and changes in gene expression. Only one study reported a complete PRP cytology. This study highlights the underlying mechanisms of PRP in muscle pathology at the basic science level, and emphasizes the need for standardization in PRP preparation and reporting.
- Citation: Kunze KN, Hannon CP, Fialkoff JD, Frank RM, Cole BJ. Platelet-rich plasma for muscle injuries: A systematic review of the basic science literature. World J Orthop 2019; 10(7): 278-291
- URL: https://www.wjgnet.com/2218-5836/full/v10/i7/278.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i7.278
Over the past several years, there has been increasing interest in biologic agents as both nonoperative treatment modalities and augments to surgical procedures, to potentially accelerate the healing process and expedite return to sport after muscle injury. Platelet-rich plasma (PRP) is a blood product that is rich in platelets and many different cytokines and growth factors, such as transforming growth factor beta (TGF-β1), insulin-like growth factor-1 (IGF-1), and vascular endothelial growth factor (VEGF), whose influence on the healing of ligaments, muscles, tendons, joints, and soft tissue has been extensively studied[1-5]. In muscle pathology in particular, PRP’s abundance of growth factors and cytokines is purported to expedite healing through the induction of cellular proliferation and migration, increased angiogenesis, and muscle tissue regeneration[6-8]. These notions have led to the clinical use of PRP for both acute and chronic muscle injuries, despite the lack of both basic science and clinical evidence that justifies its use and efficacy[7,9,10]. At best, several clinical studies and trials on the use of PRP for muscle injuries have been published with varying results[3,7-9]. Therefore, it is imperative to clarify which mediators in particular facilitate these potential effects, both to better understand PRP as a biological augment, and to aid in the optimization of PRP preparations for clinical use.
The use of PRP in clinical settings requires controlled clinical trials, with consistent methodology in terms of dosing and preparation. However, what must precede is a rigorous examination of the effects of PRP in vitro and in vivo to fully understand its mechanisms of action and appropriate clinical targets. The purpose of this systematic review is to clarify the effects of PRP on muscular pathologies at the cellular and tissue levels by evaluating the basic science literature. Furthermore, the authors hypothesized that the use of PRP would confer multiple beneficial effects in the healing of muscle injuries in comparison to controls.
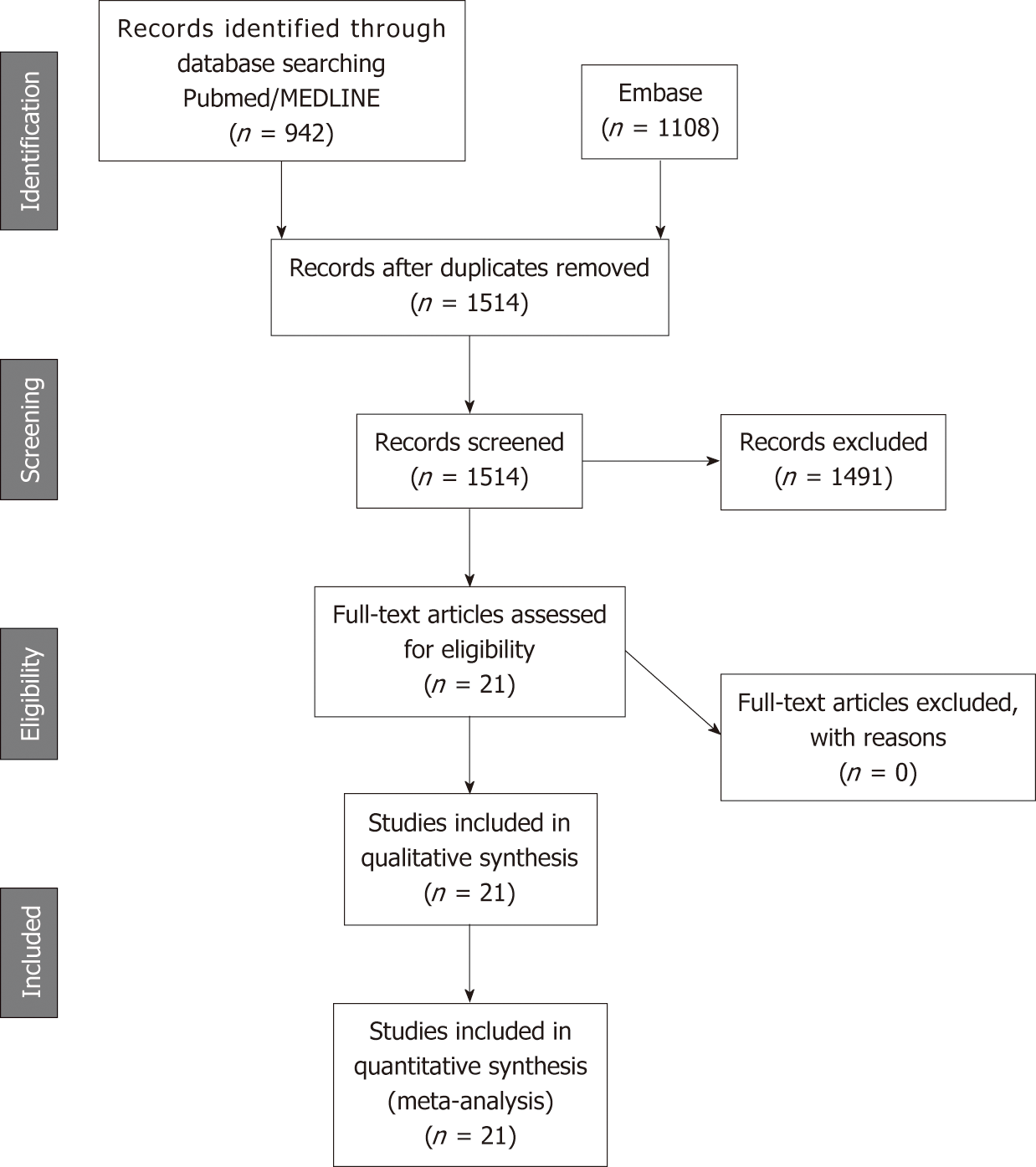
A systematic review of the PubMed/MEDLINE and EMBASE databases was performed in December 2017 using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines with a PRISMA checklist. The search was performed using the following keywords: (platelet rich plasma OR PRP OR autologous conditioned plasma OR ACP) AND (muscle OR myocyte OR skeletal muscle OR muscle injury).
The inclusion criteria for full-text reviews were level III in vivo and in vitro studies examining the effects of PRP on muscles, myocytes and/or myoblasts, that also included a well-defined control group (saline solution, no treatment, or control cell medium). Animal studies that observed the effects of PRP on traumatic and surgically-induced muscle injuries were included. In studies that reported results with additional treatments, only results that compared PRP directly with the control were analyzed. Exclusion criteria included non-English language articles, clinical studies, randomized controlled trials, review articles, articles not published in peer-reviewed journals, and studies without a control group. All references within included studies were cross-referenced for potential inclusion. One author independently performed the search and identified studies for inclusion.
Two authors extracted data using a predefined data collection sheet. Collected data included the characteristics and cytology of PRP, growth factor concentration, adhesive protein concentration, clotting factor concentration, fibrinolytic factors, proteases and antiproteases, basic proteins, membrane glycoproteins, dense granule bioactive molecules, pro-inflammatory cytokine concentration, anti-inflammatory cytokine concentration, and other proteins. In addition, study design and methods, study subjects, outcomes measured, and results were recorded. These variables included cell viability, cell proliferation, cell migration, gene expression, mechanical properties, gross appearance, and mechanical or histological examinations. If results were significantly different between the experimental and control cohorts, it was considered to be a positive or negative result based on the relative change observed. If no difference was observed between the experimental and control cohort groups, it was recorded as no change observed. Once data analysis was complete, data were analyzed for trends in outcomes by comparing the PRP treatment with controls.
The search for studies on the use of PRP in muscle pathology yielded 1013 results on PubMed/Medline and 1117 results from EMBASE. Duplicates were excluded, and 1570 studies fit the inclusion criteria for systematic review according to the search parameters described above (Figure 1). The full-text review yielded 23 articles that met the inclusion criteria for muscle pathology. Of the included studies, 15 were in vivo, 6 were in vitro, and 2 had both in vitro and in vivo study arms.
Of the 6 in vitro muscle studies (Table 1), 4 (66.6%) studied myoblasts[1,11-13], one studied a range of human-derived cells (myocytes, tenocytes, osteocytes and osteoblasts)[7], and one solely studied myocytes[14]. Of the first group, two studied human-derived myoblasts[11,12], while the other two studied murine-derived myoblasts[1,13].
| Ref. | PRP preparation | Cytology findings | Study design | Outcomes measured | Results |
| Kelc et al[11], 2015 | Whole blood in citrate dextrose anticoagulant spun 10 min at 1500 rpm. Three PRP solutions prepared at differing “growth factor concentrations” by diluting with DMEM (5%, 10% and 20%) | Not reported | Human CD56+ Myoblast cells cultured and treated with PRP (5,10,20%) and/or decorin for 4 d of treatment | Cell viability, proliferation. Myogenic differentiation, TGF-β and other fibrotic cytokine expression, MRF | PRP increased myoblast proliferation, viability, and differentiation. PRP supported myogenic shift in differentiation. Decreased TGF-β and other fibrotic cytokine expression and increased expression of MRFs |
| Mazzocca et al[7], 2012 | PRP-LP (low platelet) – single 1500 rpm spin for 5 min. Plasma layer isolated. PRP-DS (High Platelet, high WBC) – double spin first at 1500 rpm for 5 min then again at 6300 rpm for 20 min. PRP-HP (High platelet, low WBC) – single 3200 rpm spin for 15 min | PRP-LP – Platelet (Plt) count equal to 382.0 ± 111.6 103/µL; RBC 0; WBC 0.6 ± 0.3 103/µL. PRP-HP – Plt count equal to 940.1 ± 425.8 × 103/µL; RBC 1.5± 2.5 × 103/µL; WBC 17.0 ± 5.2 × 103/µL. PRP-DS - Plt count equal to 472.6 ± 224.2 × 103/µL; RBC 0.0 ± 0.1 × 103/µL, WBC 1.5 ± 0.6 × 103/µL | Human muscles isolated from lattisimus dorsi transfer procedures cultured for 2 wk to allow for myocyte outgrowth. Myocytes treated with three PRP treatments for 96 h | Cell proliferation, growth factor concentrations (EGF, FGF2, HGF, IGF-1, PDGF, TGF-β, VEGF) | PRP-DS and PRP-LP increased cell proliferation. PRP-LP increased concentration of all growth factors except HGF, FGF, & EGF. PRP-DS increased concentration of all growth factors except FGF & HGF. PRP-HP increased concentration of all growth factors except FGF |
| McClure et al[1], 2016 | Prepared with commercial SmartPReP® 2 system. Frozen thaw protocol to lyse platelets. Product then frozen and lyophilized to create dry PRGF | Not reported | C2C12 murine myoblasts cultured and expanded and treated with PRGF at various concentrations for 7 d | Proliferation (MTS proliferation assay), myogenic regulatory factor (MRFs) concentration, cell differentiation, skeletal muscle cell signaling, scaffold fiber alignment | PRP dose dependently increased myoblast cell proliferation, differentiation, skeletal muscle cell signaling, and concentration of MRFs (MyoD, MyoG) |
| Miroshnychenko et al[12], 2017 | 50 mL whole blood from seven volunteers processed with Pure PRP kit (EmCyte Corp) into: (1) Single spin leukocyte poor PRP; (2) Single spin mod-PRP with TGF-β1 and MSTN depletion; (3) Dual spin PRP; (4) Dual spin Mod-PRP; and (5) PPP. Second spin was 550 × g for 5 min and removed all platelets | PRP - Plt count equal to 879 ± 350.6 103/µL; WBC 1.8 ± 2.3 103/µL. PPP -Plt count equal to 9.9 ± 4.9 103/µL | Human skeletal muscle myoblast (HSMM) cell culture (CC-2580, Lanza) used to produce positive control (treated with 2% horse serum in myogenic DMEM/F-12 medium) and negative control (treated with 10% FBS in SkBM-2 basal medium). HSMM treated at varying concentrations with plasma formulations | Cell proliferation, protein production, myoblast differentiation, gene expression (MYH, MYH2, MSTN, MEF2C) | Single spin PRP & single spin Mod-PRP greatest influence on myoblast proliferation, but did not promote myogenic differentiation or formulation of myotubules. PPP and double spin PRP had little effect on proliferation, but greatest effects on promotion of myogenic differentiation and myotubule formation. PPP had a dose-dependent effect (peaking at 4%) on increasing MYH expression |
| Tsai et al[13], 2017 | Whole blood from Sprague-Dawley rats in acid citrate-dextrose, spun at 800 × g for 30mins. Plasma isolated and spun at 3000 × g for 20 min. 10% thrombin solution added and again centrifuged at 5500 × g for 15 min. Final release filtered by 0.22 μm ultra-filtration and frozen at -20 °C | Not reported | Skeletal muscle cells isolated from Sprague-Dawley rats cultured and treated with PRP releasate. MTT assay and Immunohistochemistry with ki-67 stain also used to determine cell proliferation. Western blot used to determine changes in protein expression. Flow cytometry used to evaluate cell-cycle progression | Cell proliferation, cell viability, protein expression (cyclin A2, cyclin B1, cdk1, cdk2, PCNA) | PRP increased skeletal muscle cell viability & cell proliferation by shifting cells from the G1 phase to the S1 phase and G2/M phases. PRP increased protein expression of cyclin A2, cyclin B1, cdk1, cdk2, PCNA |
| Tsai et al[14], 2017 | Whole blood from Sprague-Dawley rats in acid citrate-dextrose, spun at 800 × g for 30 min. Plasma isolated and spun at 3000 × g for 20 min. 10% thrombin solution added and again centrifuged at 5500 × g for 15 min. Final release filtered by 0.22 μm ultra-filtration and frozen at -20 °C | Not reported | Myocyte migration evaluated by trans-well filter migration assay and electric cell-substrate impedance sensing. Myocyte spreading evaluated microscopically. Formation of filamentous actin (F-actin) cytoskeleton assessed by immunofluorescence staining. Protein expressions of paxillin and focal adhesion kinase (FAK) assessed by Western blot analysis | Myocyte migration, spreading, FAK and Paxillin expression, F-actin formation | PRP dose-dependently promoted (1) Myocyte migration, (2) Spreading, (3) Paxillin and FAK expression, (4) F-actin formation, and (5) Wound healing |
Two studies (33.3%) reported that the platelet concentration of the final PRP preparation was increased compared to control (Table 2)[7,12]. Only one in vitro muscle study reported white blood cell concentration[7]. In this study, 3 different PRP preparations at varying platelet and leukocyte concentrations were created, and cytology was reported. Only one study reported a complete cytology of PRP, which included platelet count, red blood cell count, and white blood cell count.
| Component | Reported studies, n (%) | Studies not reporting, n (%) |
| Platelet count | 15 (65.2) | 8 (34.8) |
| White blood cell count | 6 (26.1) | 17 (73.9) |
| Red blood cell count | 1 (4.3) | 22 (95.7) |
All six studies analyzed cell proliferation in response to PRP treatment, and all reported significant increases[1,7,11-14] (Table 3). In 4 studies (66.6%), the effect of PRP on cell differentiation was examined, and 3 (50%) observed increases[1,7,11,12] (Table 3). One study (16.7%) analyzed cell signaling in response to PRP treatment, reporting no effect[1] (Table 3). All 6 studies examined the effect of PRP on the regulation of gene expression, and reported significant increases in stem cell markers[7], particularly those indicative of early differentiation[1], cell-cycle mediators[13], myosin heavy chain expression[12], and mediators of cellular migration[14] (Table 3). One study reported a dose-dependent increase in cell migration and spreading with PRP treatment[14]. None of the in vitro studies assessed inflammatory mediation, proteoglycan or collagen content (Table 3).
| Outcome | Studies reporting, n (%) | Significant increase, n | No significant change, n | Significant decrease, n |
| Cell viability | 2 (33.3) | 2 | 0 | 0 |
| Cell proliferation | 5 (83.3) | 5 | 0 | 0 |
| Proteoglycan and collagen content | 0 (0) | 0 | 0 | 0 |
| Gene expression | 5 (83.3) | 4 | 0 | 1 |
| Cell migration | 1 (16.7) | 1 | 0 | 0 |
| Cell differentiation | 3 (50) | 3 | 0 | 0 |
| Inflammatory mediation | 0 (0) | 0 | 0 | 0 |
Of the 15 in vivo studies, 11 (73.3%) reported platelet concentrations in their final PRP preparations[2,3,8,15-22] (Table 2). All 11 studies reported platelet concentrations greater than that of whole blood. Five studies (33.3%) reported PRP WBC concentration. Two of these studies reported an increase in WBC concentration relative to whole blood[15,17]. One study reported an increased RBC count relative to whole blood in their PRP preparation[15]. None of the studies reported a complete cytology of PRP.
A variety of animal models and muscles were used (Table 4). Studies also performed histologic[3,6,8,9,15,17,18,20-25] and gross anatomical[6,15,17,20,21,23] assessments of the muscles (Table 5). Eight studies reported improved functional and structural variables, reduced fibrosis, and increased muscular regeneration in PRP-treated muscle compared to control muscle[6,15,17,20-23,25]. Several studies reported increased angiogenesis after PRP treatment[17,20,21,23]. Four studies reported increased leukocyte infiltration at the injection site[8,9,18,25]. With regards to changes in collagen deposition, one study reported increased type III collagen, one reported increased type I collagen[25], and two reported no change in collagen content[2,8]. One study reported significant increases in growth factor concentrations (EGF, PDGF-BB, PDGF-AA, HGF, IGF, TGF-β1) compared to control groups, as well as a greater number of VEGF receptors[15] (Table 5). In this study, it was found that the growth factors with the most robust increase relative to baseline were PDGF and HGF, and that leukocytes were the main source of VEGF[15].
| Ref. | PRP preparation | Cytology findings | Study design | Outcomes measured | Results |
| Borrione et al[9], 2014 | Whole blood collected in sodium citrate spun twice first at 220 × g for 15 min and again at 1270 × g for 5 min. Pellet re-suspended and activated with 10% CaCl2 (20 mL) | Not reported | 102 Wistar male adult rats had flexor sublimis muscle surgically cut and PRP immediately applied | Macroscopic evaluation, H&E changes, Leukocyte infiltration & WBC numbers, MyoD protein expression, gene expression of CD3, CD8, CD19, and CD 68, Myo D. Outcomes measured up to 7 d | PRP led to greater & earlier leukocyte infiltration (lymphocytes & monocytes) than control. PRP increased gene & MyoD protein expression |
| Cunha et al[2], 2014 | Whole blood spun at 220 × g for 20 min at 20 °C. PRP combined with thrombin and activated with 10% CaCl2 to yield PRP gel | Not reported | 20 Wistar adult male rats had vastus lateralis surgically injured. Rats randomized to treatment with and without PRP +/- exercise training | Serum lactate levels, histological analysis measuring type 1 and type 3 collagen at 3 wk after treatment | Exercise training + PRP led to greatest increase in type 3 collagen and decrease in type 1 collagen |
| Delos et al[3], 2014 | Whole blood collected in citrate phosphate dextrose. Spun at 1000 × g for 15 min at 4 °C. Second spin under same conditions. 100 µL of PRP used for treatment | PRP – Plt count equal to 2.19 × 106 ± 2.69 × 105 µL, WBC 22.54 × 103/µL | 46 male Lewis rats underwent single blunt injury to gastrocnemius muscle. Four treatment groups: Immediate PRP, Immediate saline, PRP day 1, PRP day 3 | Histology, biomechanical testing (maximal isometric torque), amount of fibrosis (Masson’s trichome staining), IHC. Outcomes measured at day 15 | PRP did not demonstrate any effects on outcomes including isometric torque strength, amount of fibrosis, or inflammation |
| Denapoli et al[15], 2016 | Pure leukocyte poor PRP: Blood in 70% EDTA HEPES buffer spun at 300 × g/15 min and again 1000 × g/10 min. Platelets separated and 70% EDTA HEPES buffer added | Pure PRP- Plt count equal to 1090.0 ± 70.7 × 103/µL | 30 male 10– to 12-week-old C57BL/6 wild-type mice had surgically induced blunt contusion to tibialis anterior muscle. 10 µL, pure PRP was injected at day 1, 4 and 7 d after injury. Outcomes measured at day 30 | Histologic assessment of repair. Treadmill exercise for functional performance. Other PRP preparations were created and cytology & growth factor concentrations were compared between PRP groups. However, only pure leukocyte poor PRP was used in muscle contusion model | The day 7 PRP treated group had best functional performance and the most peripheral nucleated fibers on histology suggesting fastest recovery and decreased fibrosis |
| Dimauro et al[16], 2014 | Whole blood collected in citrate phosphate dextrose. Spun at 220 × g/15 min, and again at 1270 × g/5 min. Pellet re-suspended and activated with 10% CaCl2 | Averages not reported. However, PRP reported to have platelet concentration > 1250000 and WBC, neutrophils < baseline | 40 Wistar male adult rats had surgical lesion made in flexor sublimus muscle. 20 rats immediately treated with PRP, other 20 untreated. Additional 10 rats anesthetized with lesion made. Outcomes measured at days 2 and 5 | Gene expression of many intrinsic factors in regenerating skeletal muscle (e.g. cytokines, MRFs, growth factors), protein expression of MyoD1, Pax7, myogenin, stress response proteins, and apoptotic markers | PRP increased early expression of pro-inflammatory cytokines (e.g., TGF-β1, IL-1β. Increased expression of MRFs. No effect on VEGF. Increased ERK activation & IGF-1Eb expression |
| Gigante et al[23], 2012 | Whole blood collected in citrate phosphate dextrose (1:5). Spun at 1000 × g/6 min. Supernatant activated with CaCl2 and then spun at 1450 × g/15 min | Not reported | Surgically induced bilateral lesions of longissimus dorsi muscle and subsequently treated with PRP matrix evaluated over 60 d | Histologic evaluation of neovascularization, muscle regeneration, fibrosis and inflammation. IMHC of myoD and Myogenin | Improved fibrosis, muscular regeneration and neovascularization. Increased expression of Myogenin |
| Hammond et al[6], 2009 | Femoral/renal veins or intracardiac punctures on five adult male Sprague-Dawley rats (20 mL blood/each). PRP separated from whole blood (Symphony II Platelet Concentration System, DePuy). PPP used for control. Remaining PRP subjected to high frequency ultrasound (10 s). 100 µL used for injections | Not reported | 72 adult male Sprague-Dawley rats had strain of tibialis anterior induced with superimposed lengthening contraction onto maximal isometric contraction using either a single repetition or multiple repetitions. Outcomes measured at days 3, 5, 7, 14, 21 | Maximal isometric contraction and torque, Isometric torque, histology, and gene and protein expression of MyoD and myogenin, PDGF and IGF-1 concentrations in PRP and PPP | PRP had higher concentrations of PDGF and IGF-1. In single repetition group, PRP resulted in increased force only at day 3. No difference in return to function. For multiple repetitions, PRP improved force at multiple time points and faster return to function |
| Li et al[17], 2016 | PRP isolated from three rats and mixed in citrate-phosphate-dextrose isolated as above. Centrifuged at 160 × g/20 min. Supernatant transferred, centrifuged 400 × g/15 min. Pellet re-suspended with remaining plasma to yield PRP | PRP - Plt count equal to 6.44 ± 0.64 × 106/µL, WBC 22.37 ± 2.25 × 103/µL | 16 male Fisher rats injured with cardiotoxin injection into tibialis anterior. Four treatments: (1) Control, (2) 50 µL PRP, (3) 50 µL PRP neutralized with 280 ng/µL TGF-β1 antibody, (4) 50 µL PRP neutralized with 1400 ng/µL TGF-β1 antibody. Outcomes at 7, 14 d | Assessed muscle regeneration and collagen deposition with histology. IMHC for CD31, Alpha-SMA, Pax-7, CD68, transglutaminase-2, dystrophin to determine differentiation and mechanism for repair | PRP accelerated muscle regeneration (increased regenerating myofibers), increased angiogenesis (increased MVD-CD31, MVD-α-SMA) TGF-β1 neutralization of PRP reduced collagen deposition, PRP reduced macrophages and inflammatory response |
| Martins et al[19], 2016 | Whole blood centrifuged 180 × g/10 min. Supernatant transferred and centrifuged at 1000 × g/10 min. Pellet re-suspended and activated with 10% calcium gluconate | PRP - Plt count equal to 4904/µL | Gastrocnemius Muscle contusion model studying the effect of PRP and reactive oxygen species over a 7-d treatment course | Reactive species byproducts (TBARS, DCFHRS), mitochondria function (MTT assay), antioxidant enzyme activities (GSH, CAT, SOD) and myeloperoxidase | PRP reduces oxidative damage and MPO enzyme, increases antioxidants |
| Ozaki et al[21], 2016 | 4mL blood from cardiac puncture combined with 0.2 mL 10% sodium citrate. Centrifuged 200 × g/15 min. Top two fractions isolated and centrifuged, at 500 × g/10 min | PRP- Plt count equal to 4999 × 103/µL | Thirty-five male Wistar rats in 5 groups (n = 7): control (C), control lesion (CL), lesion treated with low-level laser therapy (LLt), lesion treated with PRP (LP), and lesion treated with both techniques (LLtP). Muscle injury by stretching gastrocnemius muscle. PRP (100 μL) injected into distal third of tibia to be applied to gastrocnemius muscle belly | Histology for morphology, inflammatory infiltrate, oxidative stress using Raman scattering spectroscopy, collagen content | CL group had increased macrophages and oxidative stress. LP group had decreased inflammation, increased tissue organization, and increased presence of regeneration cells |
| Pinheiro et al[24], 2016 | Intracardiac puncture -3 mL blood/each rat centrifuged 1200 × g/15 min to yield three layers. Isolated PRP/RBC layer, centrifuged 1min. PRP (0.2 mL) separated and activated with calcium gluconate (0.01 mL) to yield PRP gel | Cytology not provided | Ultrasound study following PRP therapy in a gastrocnemius muscle injury model | Pennation angle, Muscle thickness, Mean pixel intensity, claudication scores | No significant difference found |
| Quarteiro et al[8], 2015 | Four blood samples (8 mL/rat) from five rats mixed with anticoagulant Samples centrifuged and plasma separated. Plasma centrifuged and supernatant removed leaving PRP (1mL) | PRP - Plt count equal to 1019 ± 182.25 × 103/µL | Gastrocnemius muscle injury model | Histologic assessment | No difference in collagen content at 21 days. Inflammatory process observed in groups treated with PRP |
| Terada et al[20], 2013 | Blood obtained from intracardiac puncture. Centrifuged 800 rpm/ 15 min at 25 °C. Three PRP preparations created (rPRP, gPRP and hPRP). All three activated with 10% CaCl2 and bovine thrombin (300 IU, Fibriquik Thrombin, BioMerieux Inc., Durham, NC, United States) | PRP - Plt count equal to 208.0 ± 25.8 × 103/mL | PRP +/- Losartan in a tibialis anterior contusion model | IMHC (VEGF, CD31, Follistatin), Isometric Torque, Histological assessment (fibrosis and number of regenerating myofibers) | PRP in conjunction with losartan improved muscle recovery, reduced fibrosis. increased angiogenesis. PRP alone had similar but lesser effects |
| Contreras-Muñoz et al[22], 2017 | 3.5-4 mL whole blood obtained from intracardiac puncture, added to citrate phosphate dextrose, spun at 400 × g for 10 min. Plasma fraction extracted and spun at 800 g for 10 min | PRP - Plt count equal to 3.73 ± 0.25 × 106 platelets/ µL; WBC - 0.004 ± 0.0054 × 103 /µL | 40 rats assigned to five groups: Injured rats (medial gastrocnemius injury) + single PRP injection (PRP group), daily exercise training (Exer group), or combination of single PRP injection and daily exercise training (PRP-Exer group). Untreated and intramuscular saline–injected animals were used as controls | Histologic and immunofluorescence analysis, force assessment, cross-sectional area of newly formed muscle fibers, dMHC and presence of collagen 1 in scar formation | 18%, 20%, and 30% strength increase in PRP, PRP-Exer, and Exer groups. 1.5-, 2-, 2.5-fold increase in myofiber cross sectional area in PRP, PRP-Exer, and Exer groups. 20%, 34%, 41% of reduction scar formation in PRP, PRP-Exer, and Exer groups. 35% and 47% decrease in percentage of dMHC-positive regenerating fibers in PRP-Exer and Exer groups |
| Garcia et al[25], 2017 | Cardiac puncture (4 mL) combined with 10% sodium citrate, spun at 200 × g for 15 min. Top layer + buffy coat extracted, spun at 500 × g for 10 minf | PRP – Plt count equal to 4998.676 × 103 platelets/µL | 35 rats assigned to five groups: Control (C), Injury (soleus) Control (IC), injury PRP (IP), injury LLLT (ILT) and injury LLLT and PRP (ILTP) | Histologic assessment of muscle fiber morphology, collagen, inflammatory infiltrate | Intense polymorphic fibers (> 75%) in ILTP and IP groups. Lowest inflammatory infiltrate (< 20%) in ILTP compared to other injured groups. Significantly more focused collagen in ILT compared to IP and C groups |
| Outcome | Studies reporting, n (%) | Significant increase, n | No significant change, n | Significant decrease, n |
| Cell viability | 0 (0) | 0 | 0 | 0 |
| Gene expression | 5 (33.3) | 5 | 0 | 0 |
| Gross appearance of muscle repair | 1 (6.67) | 0 | 1 | 0 |
| Histologic assessment of muscle repair | 8 (53.3) | 7 | 1 | 0 |
| Proteoglycan content | 0 (0) | 0 | 0 | 0 |
| Collagen deposition | 7 (46.7) | 2 | 3 | 2 |
| Muscle strength | 4 (26.7) | 3 | 1 | 0 |
| Inflammatory mediation | 8 (53.3) | 4 | 1 | 3 |
| Growth factors | 1 (6.67) | 1 | 0 | 0 |
Of the 2 studies that examined both the in vivo and in vitro uses of PRP, one used human muscle-derived progenitor cells (hMDPCs) from unspecified skeletal muscle from living and post-mortem biopsies for the in vitro component[26], while the other used an established murine myogenic cell line (C2C12)[27] (Table 6). Only one study reported platelet count and WBC concentration[24], while neither reported RBC count. For the in vivo component, the gastrocnemius muscle of a mouse[26] and the rotator cuff muscles (supraspinatus and infraspinatus) of a rat[27] were used. The in vitro studies reported the following with regards to PRP treatment relative to controls: Increased cell proliferation[27], increased expression of stem cell markers[26], increased myotube formation and area[27], increased myogenic proliferation and decreased lipid droplets[27], and increased Pax7 and myogenin gene expression[27] (Table 7). Further-more, the in vivo component of one study assessed hMDPC expansion[26] (Table 6).
| Ref. | PRP preparation | Cytology findings | Study design | Outcomes measured | Results |
| Takase et al[27], 2017 (In vitro arm) | Whole blood extracted from male volunteers, combined with 12 mL 3.13% sodium citrate. Centrifuged 2400 rpm/10 min, again at 3600 rpm/15 min for 10 mL PRP and PPP. PRP activated by freezing at -80 °C; centrifuged again at 10000 rpm/10 min | PRP – Plt count equal to 7.2 × 105 - 9.4 × 105 platelets/mL | Murine myogenic cell line (C2C12 cells) subjected to PRP treatment. Cell morphology assessed by phase microscopy. Myotube quantification assessed by immunocytostaining. Cell proliferation assessed using water-soluble tetrazolium salt (WST) assay using a cell counting Kit-8. Oil Red-O staining used to identify lipid droplets and accumulation determined by phase contrast microscopy. rt-PCR used to quantify myogenic and adipogenic markers | Cell proliferation, myogenic differentiation (Pax7, myogenin), adipogenic differentiation [PPARγ, CCAAT/enhancer binding protein (C/EBPα)] | PRP inhibited myotube formation, decreased average area of myotubes, induced myogenic proliferation compared to myogenic group. Number of lipid droplets in PRP-adipogenic group was lower than adipogenic group. PRP suppressed expression of Pax7, myogenin, PPARγ and C/ERPα |
| (In vivo arm) | 8 mL blood retrieved from one, 3-mo old, Sprague-Dawley rat, combined with 2 mL 3.13% sodium citrate Centrifuged at 1500 rpm for 10 min. Second spin at 3000 rpm for 10 min yielded PRP (1mL) and PPP. PRP frozen at -80 °C until needed | PRP - Plt count equal to 1.6 × 109 platelets/mL | PRP injection into subacromial space of five rat rotator cuff tear models Infraspinatus used for histology. Muscles cryosectioned, fixed with 4% PFA, stained with Oil Red-O and hematoxylin. Supraspinatus used for biochemical assays. rt-PCR to quantify genes | Oil Red-O positive lipid droplet formation, adipogenic differentiation [PPARγ, CCAAT/enhancer binding protein (C/EBPα)], and muscular atrophy [(Muscle RING Finger Protein-1 (MuRF-1) and atrogin-1] | Rotator tear groups had increased MuRF-1, atrogin-1, PPARγ and C/EBPα PRP decreased lipid droplet presence. PRP decreased expression of PPARγ and C/EBPα |
| Li et al[26], 2013 (In vivo arm) | Human whole blood from Central Blood Bank, Pittsburgh, PA, United States centrifuged 3000 g/ 10 min. Fraction of PRP poor supernatant transferred, PRP pellet re-suspended. PRP concentration measured by hemocytometer, activated with human thrombin (1U/mL). PRP releasate separated from cellular debris by centrifugation 3000 × g/30 min. PRP releasate stored at -80 °C | Cytology not provided | Gastrocnemius of mdx-SCID mice damaged with cardiotoxin and treated with hMDPCs treated with PRP | Histological assessment of as the number of hMHC-I-positive myofibers/1 × 105 injected cells | PRP maintained hMDPCs growth and regeneration of myofibers |
| (In vitro arm) | Centrifuged at 3000 × g for 10 min at RT. PRP activated with one unit per mL human thrombin. After activation, the PRP releasate obtained by centrifugation at 3000 × g for 30 min | PRP – Plt count equal to 2000/µL | hMDPCs isolated from donors cultured in PRP versus 20% FBS as a control. Assessed Proliferation, role of exogenous growth factors, gene expression, and cell differentiation | Proliferation, growth factor PDGF, VEGF, TGF-B1 RT-PCR for expression profile of stem cell markers and differentiation | PRP increased cell proliferation. PRP with anti TGF-B1 and anti VEGF did not. PRP increased the expression of BMPR1-A, BMPR1-B, BMPR2, ALDH, SOX2, Aggrecan, and Desmin. No difference in differentiation capacity |
| Outcome | Studies reporting, n (%) | Significant increase, n | No significant change, n | Significant decrease, n |
| Cell viability | 0 (0) | 0 | 0 | 0 |
| Cell proliferation | 1(25) | 1 | 1 | |
| Cell differentiation | 1 (25) | 1 | 0 | 0 |
| Gene expression | 3 (75) | 3 | 0 | 2 |
| Gross appearance of muscle repair | 0 (0) | 0 | 0 | 0 |
| Histologic assessment of muscle repair | 2 (50) | 2 | 1 | 1 |
| Proteoglycan content | 0 (0) | 0 | 0 | 0 |
| Collagen deposition | 0 (0) | 0 | 0 | 0 |
| Muscle strength | 0 (0) | 0 | 0 | 0 |
| Inflammatory mediation | 0 (0) | 0 | 0 | 0 |
The principle findings of this systematic review are as follows: (1) In the majority of studies, PRP treatment increased myocyte proliferation, growth factor expression (e.g., PDGF-A/B and VEGF), leukocyte recruitment, and angiogenesis in muscle models when compared to control groups; (2) PRP preparation techniques remain inconsistent across studies in the basic science literature; and (3) Evidence from in vitro and in vivo basic science studies suggest that PRP has the potential to serve as an efficacious treatment modality that may expedite the healing process for muscular pathologies, based off of the observed effects at the cellular and tissue levels in treatment groups relative to control groups.
The results from the current study suggest that PRP may have differential effects on myoblast proliferation and differentiation, depending on the formulation of PRP at the basic science level. The traditional formulation of leukocyte-poor PRP that is not modulated to remove specific growth factors or platelets was shown to promote myoblast proliferation. Significant increases in myocyte proliferation were observed in all of the in vitro studies included in this review[1,7,11-13,26]. Li et al[26] reported that PRP upregulated the expression of stem cell markers in hMDPCs. Miroshnychenko et al[12] also found that traditional unmodified leukocyte-poor PRP increased proliferation of human skeletal muscle myoblasts. However, the unmodified leukocyte-poor PRP had very little effect on myoblast differentiation. On the other hand, platelet-poor plasma and double spin PRP (aimed to remove platelets) significantly promoted the induction of human myoblasts into the differentiation state. Early cell differentiation was also observed in an additional three in vitro studies[1,11,12]. It is plausible that the increases in both differentiation and proliferation underlie some of the histological findings in the in vivo muscle publications, which demonstrated that PRP treatment accelerated muscular regeneration and reduced fibrosis when compared to controls[6,15,17,20,21,23].
The differential effects of different PRP formulations on myoblast proliferation and differentiation suggest that the growth factors that promote the proliferation of myoblasts may be very different than those that promote myoblast differentiation. Several studies demonstrated PRP-induced quantifiable increases in growth factor expression[15,16], as well as observable histological increases in leukocyte recruitment to the area of injury[8,9,18]. Denapoli et al[15] reported significant increases in VEGF receptors, as well as growth factors including but not limited to PDGF, Flt-1, and EGF in PRP-treated groups when compared to the control group. PRP treatment was also found to increase angiogenesis when compared to the control[17,20,23].
Several studies also demonstrated that PRP formulations that limit the presence of growth factors that are detrimental to muscle regeneration, such as TGF-ß1 and myostatin, had greater influence on myoblast differentiation and healing. Both Denapoli et al[15] and Miroshnychenko et al[12] found that leukocyte-poor formulations of PRP that significantly limited the presence of TGF-B1 had more beneficial effects on muscle healing. These results support the hypothesis that leukocyte-poor PRP may be most effective at mediating skeletal muscle repair through limiting detrimental growth factors and increasing the concentrations of beneficial growth factors that promote angiogenesis, proliferation and differentiation at the site of injury. A significant amount of further research is warranted to determine the optimal growth factor milieu that promotes muscular regeneration and healing. The differential responses of myocytes and myoblasts to different PRP formulations demonstrates the need for a better basic science understanding of muscular regeneration and healing, and how PRP influences each phase from inflammation to regeneration and fibrosis.
This study has limitations for its interpretation. First, several studies reported the cytology of PRP. For comparative purposes, standardization in protocol and PRP composition is required to document the efficacy of PRP across research studies[28]. The clinical literature on PRP for orthopedic pathologies has been greatly limited by the lack of impressive reporting of the PRP preparation protocol. Only 10% of clinical studies reported a clear description of the preparation of the PRP utilized, allowing it to be reproduced, which is consistent with the most recent systematic review of PRP protocol standardization that reports a 16% rate of reporting quantitative metrics[28]. The results from this study demonstrate that the same shortcomings exist in the basic science literature on the use of PRP for muscle pathology. Given that both Mazzocca et al[7] and Miroshnychenko et al[12] reported differences in findings depending on what PRP preparations they use, it is essential that this important information is documented and standardized. In both clinical and basic science studies on PRP, the authors agree with Chahla et al[28] that the protocol of PRP preparation must be clearly articulated and reproducible in both basic science and clinical studies, so that the results across studies can be compared to ultimately allow us to determine the optimal preparation to treat both chronic and acute muscle injuries. The minimum reporting guidelines established by consensus and published by Murray IR et al[28]. should be utilized by all journals as the minimum requirements a study on PRP must meet before publication.
Another limitation of the basic science literature is that the majority of the injuries to animal models are surgically-induced instead of occurring from trauma or wear. It is not uncommon for muscle injuries to present chronically in the clinic, and even acute lesions to muscles may present after a delay. Chronic degeneration and acute injury lead to distinctively different cellular and molecular responses that may respond differently to PRP. In addition, the biologic milieu created by the cellular and molecular responses in both chronic and acute muscle pathology changes over time. Thus, a better understanding of these time-dependent changes in the biologic milieu (e.g., host pH, cytokine and growth factor concentration), and the influence of timing, delivery, and dosing of PRP, needs to be better understood and further studied.
In conclusion, the basic science literature on the use of PRP in muscle pathology demonstrates that PRP confers several potentially beneficial effects on healing in comparison to controls at the basic science level. Future research is needed to determine the optimal cytology, dosing, timing, and delivery method of PRP for both chronic and acute muscle pathology.
Platelet-rich plasma (PRP) is a biological adjunct derived from autologous blood, which is thought to aid the healing of various bone, ligament, cartilage, and muscle injuries. PRP is composed of various cytokines, growth factors, and concentrations of leukocytes and platelets. PRP is often used clinically to expedite healing as a non-operative treatment or operative adjunct. However, studies have reported mixed effects of PRP, and clinicians continue to employ this adjunct despite little understanding of its mechanism of action.
The main topics of the current study are (1) The various mechanisms of PRP action at the molecular and tissue levels for muscle injuries; and (2) Reporting patterns of PRP preparations in these studies. The current study seeks to clarify the underlying mechanisms of action of PRP, in terms of its ability to induce cellular changes and changes at the histologic and tissue levels, which are not well-described.
The main objective of the current study is to clarify the effects of PRP at the cellular and tissue levels through synthesizing its mechanisms of action from available basic science studies on muscle injuries. A secondary objective that was realized was that it is important to understand PRP preparations across multiple studies to allow for the standardization of study protocols and better comparisons.
A systematic review of basic science studies from the PubMed/MEDLINE and EMBASE databases was conducted, as these studies would allow for the best understanding of the mechanism of action of PRP at the cellular and tissue levels. Using a custom pre-determined spreadsheet of a wide variety of growth factors, cytokines, and other molecular markers, each study was analyzed, and these variables were subsequently extracted. The PRP preparation methods were also extracted.
A total of 23 articles were identified. PRP conferred multiple beneficial effects on muscles both in vitro and in vivo through the upregulation of genes beneficial to healing and muscle regeneration, increasing cellular proliferation and differentiation, and producing superior tissue quality and biomechanical properties in comparison to placebo. However, this study also identified the lack of PRP cytology reporting among these studies, of which only one study reported a full cytology.
PRP confers multiple beneficial effects at the basic science level in models of muscle injury compared to placebo through changes at the cellular level, which include gene expression, growth factor and cytokine concentrations, increased angiogenesis, and cellular differentiation and proliferation. PRP also mediates increased muscle regeneration at the gross level, and superior histologic quality when compared to placebo in a few studies. There was significant variability in both PRP preparation and reporting among the included studies.
This study highlights the importance of understanding processes at the basic science level in order to provide better insight into clinical practice. Future research is needed to determine the optimal cytology, dosing, timing, and delivery method of PRP for muscle injuries. Higher level randomized studies will need to be performed in order to determine these factors. Furthermore, it will be essential for future studies to use standardized protocols, such that outcomes and practices with PRP become reproducible.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A, Emara KM, Peng BG S-Editor: Gong ZM L-Editor: Filipodia E-Editor: Liu JH
| 1. | McClure MJ, Garg K, Simpson DG, Ryan JJ, Sell SA, Bowlin GL, Ericksen JJ. The influence of platelet-rich plasma on myogenic differentiation. J Tissue Eng Regen Med. 2016;10:E239-E249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Cunha RC, Francisco JC, Cardoso MA, Matos LF, Lino D, Simeoni RB, Pereira G, Irioda AC, Simeoni PR, Guarita-Souza LC, Carvalho KA. Effect of platelet-rich plasma therapy associated with exercise training in musculoskeletal healing in rats. Transplant Proc. 2014;46:1879-1881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Delos D, Leineweber MJ, Chaudhury S, Alzoobaee S, Gao Y, Rodeo SA. The effect of platelet-rich plasma on muscle contusion healing in a rat model. Am J Sports Med. 2014;42:2067-2074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Cheng M, Wang H, Yoshida R, Murray MM. Platelets and plasma proteins are both required to stimulate collagen gene expression by anterior cruciate ligament cells in three-dimensional culture. Tissue Eng Part A. 2010;16:1479-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Dhillon MS, Karna SK, Dhatt SS, Behera P, Bhatia A. Can Platelet rich plasma stimulate human ACL growth in culture? A preliminary experience. Muscles Ligaments Tendons J. 2015;5:156-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Hammond JW, Hinton RY, Curl LA, Muriel JM, Lovering RM. Use of autologous platelet-rich plasma to treat muscle strain injuries. Am J Sports Med. 2009;37:1135-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 173] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 7. | Mazzocca AD, McCarthy MB, Chowaniec DM, Dugdale EM, Hansen D, Cote MP, Bradley JP, Romeo AA, Arciero RA, Beitzel K. The positive effects of different platelet-rich plasma methods on human muscle, bone, and tendon cells. Am J Sports Med. 2012;40:1742-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 8. | Quarteiro ML, Tognini JR, de Oliveira EL, Silveira I. The effect of platelet-rich plasma on the repair of muscle injuries in rats. Rev Bras Ortop. 2015;50:586-595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Borrione P, Grasso L, Chierto E, Geuna S, Racca S, Abbadessa G, Ronchi G, Faiola F, Di Gianfrancesco A, Pigozzi F. Experimental model for the study of the effects of platelet-rich plasma on the early phases of muscle healing. Blood Transfus. 2014;12 Suppl 1:s221-s228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Yoshioka T, Kanamori A, Washio T, Aoto K, Uemura K, Sakane M, Ochiai N. The effects of plasma rich in growth factors (PRGF-Endoret) on healing of medial collateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc. 2013;21:1763-1769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Kelc R, Trapecar M, Gradisnik L, Rupnik MS, Vogrin M. Platelet-rich plasma, especially when combined with a TGF-β inhibitor promotes proliferation, viability and myogenic differentiation of myoblasts in vitro. PLoS One. 2015;10:e0117302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Miroshnychenko O, Chang WT, Dragoo JL. The Use of Platelet-Rich and Platelet-Poor Plasma to Enhance Differentiation of Skeletal Myoblasts: Implications for the Use of Autologous Blood Products for Muscle Regeneration. Am J Sports Med. 2017;45:945-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Tsai WC, Yu TY, Lin LP, Lin MS, Wu YC, Liao CH, Pang JS. Platelet rich plasma releasate promotes proliferation of skeletal muscle cells in association with upregulation of PCNA, cyclins and cyclin dependent kinases. Platelets. 2017;28:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Tsai WC, Yu TY, Lin LP, Lin MS, Tsai TT, Pang JS. Platelet rich plasma promotes skeletal muscle cell migration in association with up-regulation of FAK, paxillin, and F-Actin formation. J Orthop Res. 2017;35:2506-2512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Denapoli PM, Stilhano RS, Ingham SJ, Han SW, Abdalla RJ. Platelet-Rich Plasma in a Murine Model: Leukocytes, Growth Factors, Flt-1, and Muscle Healing. Am J Sports Med. 2016;44:1962-1971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Dimauro I, Grasso L, Fittipaldi S, Fantini C, Mercatelli N, Racca S, Geuna S, Di Gianfrancesco A, Caporossi D, Pigozzi F, Borrione P. Platelet-rich plasma and skeletal muscle healing: a molecular analysis of the early phases of the regeneration process in an experimental animal model. PLoS One. 2014;9:e102993. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Li H, Hicks JJ, Wang L, Oyster N, Philippon MJ, Hurwitz S, Hogan MV, Huard J. Customized platelet-rich plasma with transforming growth factor β1 neutralization antibody to reduce fibrosis in skeletal muscle. Biomaterials. 2016;87:147-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 18. | Harris NL, Huffer WE, von Stade E, Larson AI, Phinney S, Purnell ML. The effect of platelet-rich plasma on normal soft tissues in the rabbit. J Bone Joint Surg Am. 2012;94:786-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Martins RP, Hartmann DD, de Moraes JP, Soares FA, Puntel GO. Platelet-rich plasma reduces the oxidative damage determined by a skeletal muscle contusion in rats. Platelets. 2016;27:784-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Terada S, Ota S, Kobayashi M, Kobayashi T, Mifune Y, Takayama K, Witt M, Vadalà G, Oyster N, Otsuka T, Fu FH, Huard J. Use of an antifibrotic agent improves the effect of platelet-rich plasma on muscle healing after injury. J Bone Joint Surg Am. 2013;95:980-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 21. | Ozaki GA, Camargo RC, Koike TE, Garcia TA, Castoldi RC, Pereira JD, Constantino CJ, Camargo Filho JC. Analysis of photobiomodulation associated or not with platelet-rich plasma on repair of muscle tissue by Raman spectroscopy. Lasers Med Sci. 2016;31:1891-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Contreras-Muñoz P, Torrella JR, Serres X, Rizo-Roca D, De la Varga M, Viscor G, Martínez-Ibáñez V, Peiró JL, Järvinen TAH, Rodas G, Marotta M. Postinjury Exercise and Platelet-Rich Plasma Therapies Improve Skeletal Muscle Healing in Rats But Are Not Synergistic When Combined. Am J Sports Med. 2017;45:2131-2141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Gigante A, Del Torto M, Manzotti S, Cianforlini M, Busilacchi A, Davidson PA, Greco F, Mattioli-Belmonte M. Platelet rich fibrin matrix effects on skeletal muscle lesions: an experimental study. J Biol Regul Homeost Agents. 2012;26:475-484. [PubMed] |
| 24. | Pinheiro CL, Peixinho CC, Esposito CC, Manso JE, Machado JC. Ultrasound biomicroscopy and claudication test for in vivo follow-up of muscle repair enhancement based on platelet-rich plasma therapy in a rat model of gastrocnemius laceration. Acta Cir Bras. 2016;31:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Garcia TA, Camargo RCT, Koike TE, Ozaki GAT, Castoldi RC, Camargo Filho JCS. Histological analysis of the association of low level laser therapy and platelet-rich plasma in regeneration of muscle injury in rats. Braz J Phys Ther. 2017;21:425-433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Li H, Usas A, Poddar M, Chen CW, Thompson S, Ahani B, Cummins J, Lavasani M, Huard J. Platelet-rich plasma promotes the proliferation of human muscle derived progenitor cells and maintains their stemness. PLoS One. 2013;8:e64923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 27. | Takase F, Inui A, Mifune Y, Sakata R, Muto T, Harada Y, Ueda Y, Kokubu T, Kurosaka M. Effect of platelet-rich plasma on degeneration change of rotator cuff muscles: In vitro and in vivo evaluations. J Orthop Res. 2017;35:1806-1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 28. | Chahla J, Cinque ME, Piuzzi NS, Mannava S, Geeslin AG, Murray IR, Dornan GJ, Muschler GF, LaPrade RF. A Call for Standardization in Platelet-Rich Plasma Preparation Protocols and Composition Reporting: A Systematic Review of the Clinical Orthopaedic Literature. J Bone Joint Surg Am. 2017;99:1769-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 378] [Article Influence: 47.3] [Reference Citation Analysis (0)] |