Published online Apr 18, 2019. doi: 10.5312/wjo.v10.i4.212
Peer-review started: December 14, 2018
First decision: January 11, 2019
Revised: February 27, 2019
Accepted: March 12, 2019
Article in press: March 12, 2019
Published online: April 18, 2019
Processing time: 125 Days and 5.2 Hours
Leiomyosacromas in the Extremities are rare malignant smooth muscle tumors. Adjuvant radiation therapy, in combination with wide surgical excision allows the best chance of treatment. During the follow up pathological fractures are common complications that can be accompanied by Implant failure and defect situations that are most challenging in their management.
We present a case of a 52-year-old female suffering from a pathological fracture of the humeral shaft 10 yr after resection of a Leiomyosarcoma and postoperative radiotherapy. She developed implant failure after retrograde nailing and another failure after revision to double plate fixation. In a two-stage revision, the implants were removed and the huge segmental defect created after debridement was bridged by a compound osteosynthesis with nancy nails and bone cement for formation of the induced membrane. Due to the previous radiotherapy treatment, 20 cm of the humeral shaft were declared devascularized but were left in situ as a scaffold. In the second stage, a vascularized fibula graft was used in combination with a double plate fixation and autologous spongiosa grafts for final reconstruction.
This combinatory treatment approach led to a successful clinical outcome and can be considered in similar challenging cases.
Core tip: We present an innovative treatment alternative for segmental bone defects after pathological fracture, tumor resection and radiation of the humerus. A combination of Induced membrane, vascularized fibula graft and double plate fixation was used to bridge a segmental bone defect. Devascularized bone stock was left in situ as a scaffold and not resected as usual. The treatment approach led to a successful clinical outcome and can be considered in similar complex cases.
- Citation: Gathen M, Norris G, Kay S, Giannoudis PV. Recalcitrant distal humeral non-union following previous Leiomyosarcoma excision treated with retainment of a radiated non-angiogenic segment augmented with 20 cm free fibula composite graft: A case report. World J Orthop 2019; 10(4): 212-218
- URL: https://www.wjgnet.com/2218-5836/full/v10/i4/212.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i4.212
After resection of musculoskeletal tumors and following radiotherapy, bone necrosis, osteopenia or radiation-induced neoplasm can be seen[1]. Osteoradionecrosis after radiotherapy often shows a long latent period and the incidence rate is described between 1%-11%. Noteworthy, pathologic fractures become a feared complication and can occur even years after therapy[2].
When pathological fractures occur non-operative therapy rarely provides satisfactory return of function or pain relief. Stabilisation with different methods such as plate fixation, intramedullary nails, external fixators and segmental prosthetic implants can be used with reported osteosynthesis failure rates between 12.2%-22%[3,4]. In cases of segmental bone defects especially those associated with soft-tissue defects, reconstructive options remain limited. Additionally, the presence of previous radiated bone with no inherent angiogenic properties makes this problem even more challenging[3].
In the herein case study, we report the management of a recalcitrant distal humeral non union with implant failures after tumor resection and radiotherapy. Our strategy of optimum fixation accompanied by biological augmentation led to a successful outcome.
A 52-year-old female patient was referred to our institution with persistent pain of the right humerus due to recurrent implant failure and non-union of the right humerus
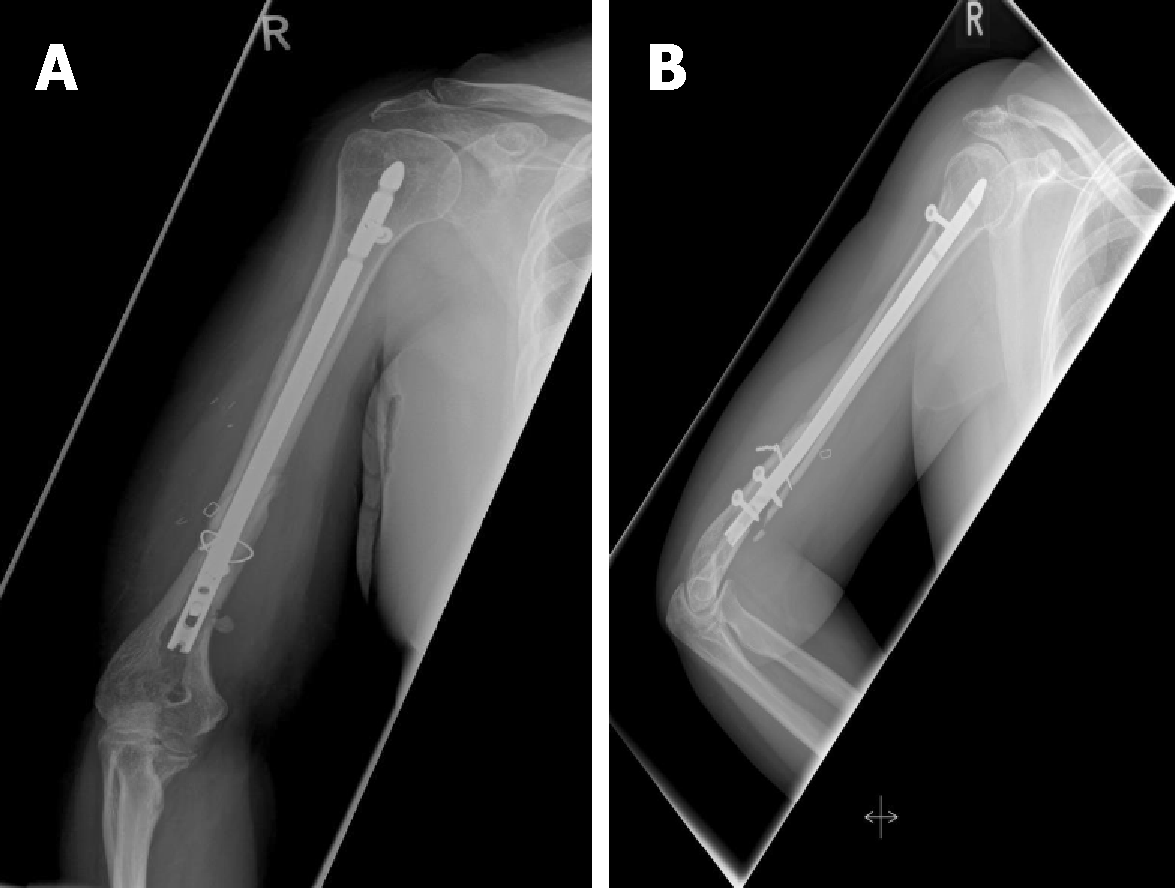
Ten years previously, the fracture area she was being treated for, had been diagnosed with a grade 2 Leiomyosarcoma. After surgical resection and free tissue transfer (groin flap for covering), a post-operative radiotherapy with 60Gy in 30 fractions was prescribed. The patient then sustained a closed fracture of the right humeral shaft whilst lifting a light object. The fracture was then stabilised with a retrograde nail but fixation failed after 18 mo (Figure 1).
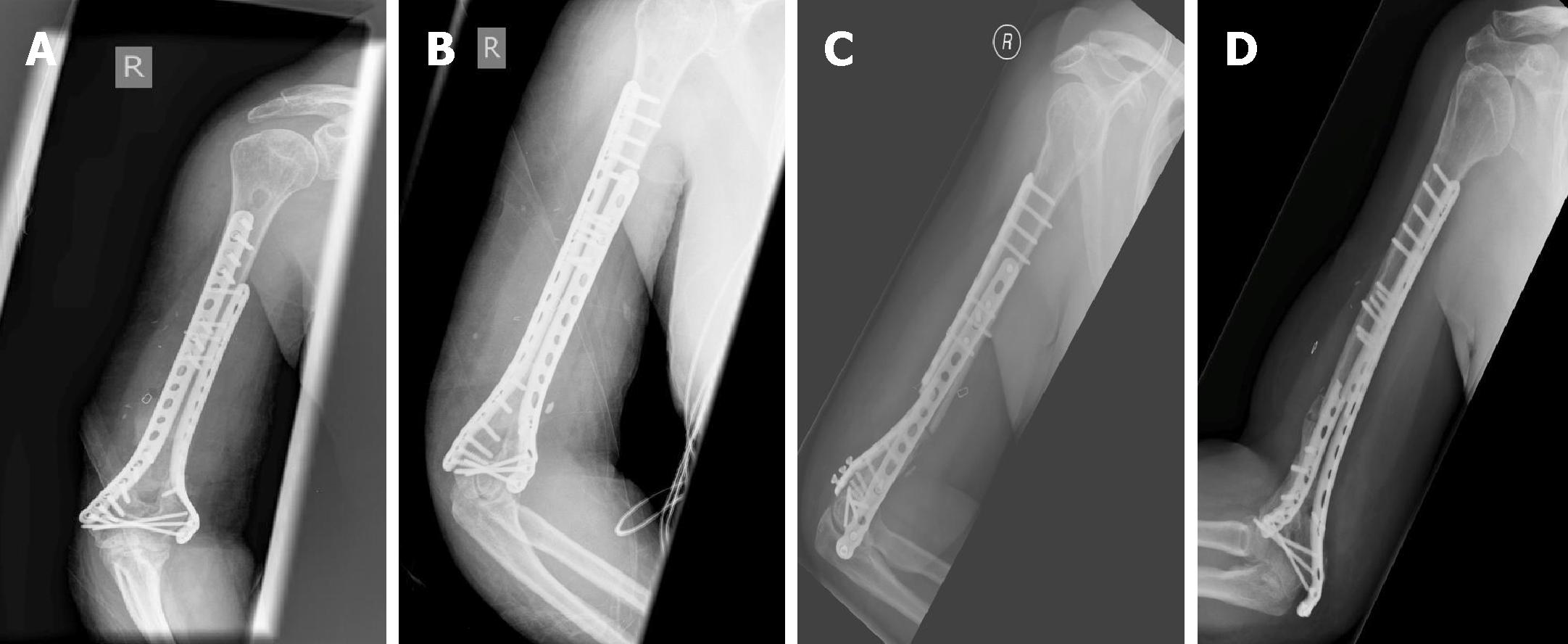
The fracture was next revised to a double plate fixation and biological en-hancement was achieved with the implantation of autologous bone grafting harvested from the pelvic iliac crest (Figure 2). However, 14 mo after the revision, the patient presented with non-union associated with implant failure and was referred to our institution (Figure 2).
The patient had a free previous medical history.
The patient showed movement dependent pain of the right upper arm. Due to the implanted double plate fixation there was no instability. After radiation and previous surgery the skin was compromised by massive scar tissue formations. The patient showed no clinical signs of infection and no neurological deficits.
Blood analysis as well as urine analysis were normal. Electrocardiogram, chest X-ray and arterial blood gas were also normal.
A staging computed tomography and magnetic resonance imaging scan of the upper arm showed no local recurrence or metastatic disease.
Distal humeral non-union associated with implant failure after resection of a Leiomyosacroma and following radiotherapy.
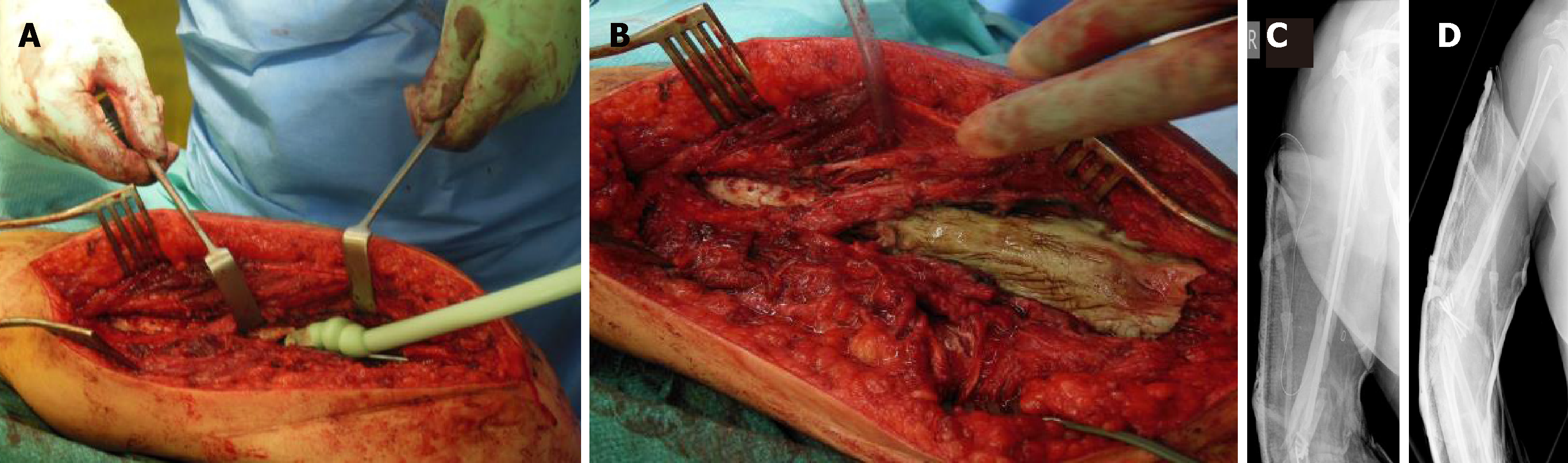
Due to the previous radiotherapy and concerns about the possibility of low-grade infection, a two-stage revision was planned. Initially, the implants were removed and the non union area was debrided with multiple tissue samples sent to microbiology. A defect of 2.5 cm was created. Temporary stabilisation was performed using a compound osteosynthesis with nancy nails and bone cement followed by wound closure (Figure 3). The notes from the referral hospital center were requested in order to identify the extent of the previous bone radiated area. Two out of the 5 culture specimens grew staphylococcus aureus and the patient was treated with appropriate antibiotics for a period of 6 wk.
During the second stage and despite the induction of the induced membrane (IM) (which can promote bone regeneration), it was felt that autologous bone grafting in isolation would not be successful since the bone edges around the non union site were lacking angiogenic capacity and healing potential[5]. The zone of the previous radiotherapy was assessed to have been from the olecranon fossa to 20 cm proximally just below the lesser tuberosity. In view of the extent area of radiated bone it was decided to leave this section of humerus in situ and considered it in our reconstruction strategy as a scaffold.
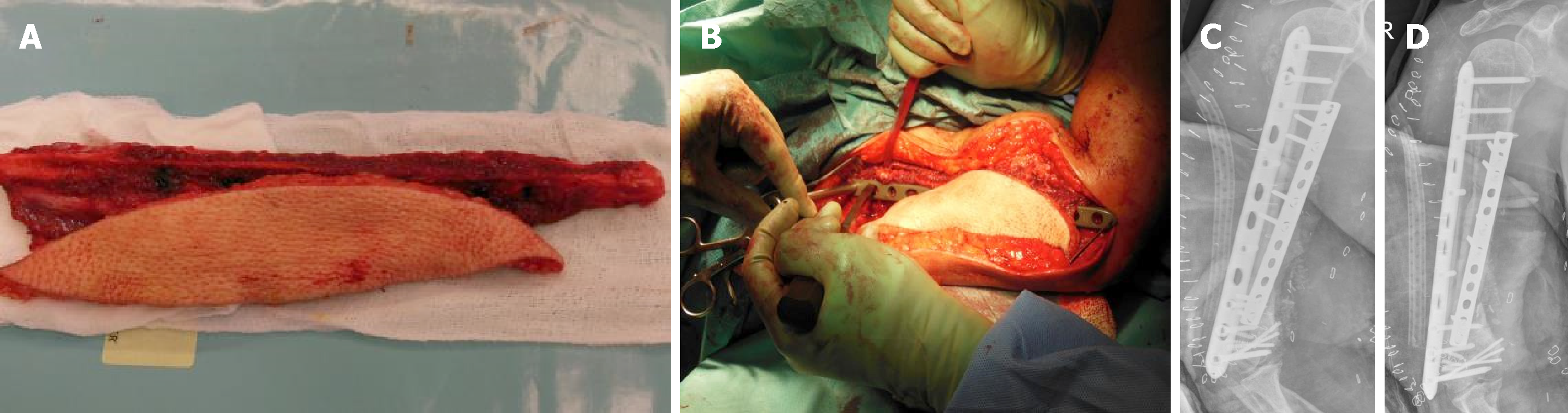
A composite fibula vascularised graft was harvested from the ipsilateral tibia 20 cm in length and the vascular graft was connected to the brachial artery. The fibula graft was placed anterior laterally and two plates were used for stabilisation. One to provide continuity to the distal and proximal radiated humeral segments and the other to stabilise the fibula on the humerus (Figure 4). The previous created bone defect was addressed by shortening of the humeral shaft by 2.5 cm. Autologous bone graft was implanted distally.
After a period of 6 months osseous healing was observed. Twelve months following reconstruction one plate was removed due to soft tissue irritation. At final follow up (2 years later), hypertrophy of the fibula graft was noted with restoration of right arm function (Figure 5). The range of motion was full flexion, minus 200 of full extension and full supination pronation of the forearm. Shoulder movements were full and pain free.
Pathological fractures of the humerus are common and associated with high re-operation rates[6]. Sarahrudi et al[4] analysed the treatment of 39 patients with pathological humerus fractures and reported a complication rate of 14.6%. They found intramedullary stabilization to be most reliable for fractures of the diaphysis and ORIF preferable for the treatment of metaphyseal fractures and for patients with a solitary metastasis[4]. In a different study, a cemented hemiprosthesis for proximal fractures was found most suitable and intramedullary nailing for lesions in the diaphysis[6].
Previous radiotherapy in the medical history of pathological fractures and particularly non union complicates treatment options and fracture healing potential due to radiation-induced osteopenia and loss of bone vitality. In our case there were 2 previous attempts of reconstruction without success. Although the masquelet technique was employed[5], it was felt that even with the presence of the IM in situ, which is highly vascular, containing growth factors and osteoprogenitor cells, the chance of healing was low. Consequently, it was deemed essential to bring vascularity to the region and structural support with the free fibula composite vascularised graft being the ideal option to bridge the avascular area of the humerus. Moreover, the retainment of the humeral avascular segment would simplify the reconstruction process by acting as a scaffold within the local environment. The double plate approach provided adequate mechanical stability until evolution of healing occurred.
Segmental defects in long bones are challenging tasks especially when further factors such as poor soft tissue, osteonecrosis or infections are present. A variety of techniques and their combinations have been described such as bone transportation, IM Technique, autograft bone grafting, and megaprosthesis[7-9].
Using a vascularized fibula graft is a highly sophisticated technical procedure with potential complications including non-union, graft fracture and donor site morbidity. Advantages include the straight configuration and dual vascularity (endosteal and periosteal). The method provides shorter duration than therapy with bone transportation and a tendency for hypertrophy in response to microscopic stress fractures[10,11]. The IM Technique is described for diaphyseal defects from 5 cm to 25 cm allowing formation of bone by means of endochondral ossification with high union rates of 90%[12].
In our case we employed a combination of techniques, including the IM, au-tologous bone grafting for the distal humerus segment, a composite vascular fibula graft and retainment of the radiated-devitalised humeral segment as a scaffold. One may argue that it is controversial that the avascular bone was left in situ because it is a widely accepted concept to resect avascular bone tissue completely[13,14]. However, this approach was found useful, eliminating the need of considering the use of a mega-prosthesis and facilitating the reconstruction process by acting as a bridge allowing implantation of the fibula graft.
We believe that the presented management of treatment of a recalcitrant humeral non-union with a background of previous pathological fracture following ra-diotherapy for leiomyosacroma is a promising alternative and should be considered as an option of treatment, when contemplating reconstruction of such complex cases.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gad EH, Salvadori M, Yu B S-Editor: Ji FF L-Editor: A E-Editor: Wu YXJ
| 1. | Ugurluer G, Akbas T, Arpaci T, Ozcan N, Serin M. Bone complications after pelvic radiation therapy: evaluation with MRI. J Med Imaging Radiat Oncol. 2014;58:334-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol. 2003;4:529-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 649] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 3. | Tatar Z, Soubrier M, Dillies AF, Verrelle P, Boisgard S, Lapeyre M. Assessment of the risk factors for impending fractures following radiotherapy for long bone metastases using CT scan-based virtual simulation: a retrospective study. Radiat Oncol. 2014;9:227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Sarahrudi K, Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma. 2009;66:789-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Giannoudis PV, Harwood PJ, Tosounidis T, Kanakaris NK. Restoration of long bone defects treated with the induced membrane technique: protocol and outcomes. Injury. 2016;47 Suppl 6:S53-S61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 150] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 6. | Wedin R, Hansen BH, Laitinen M, Trovik C, Zaikova O, Bergh P, Kalén A, Schwarz-Lausten G, Vult von Steyern F, Walloe A, Keller J, Weiss RJ. Complications and survival after surgical treatment of 214 metastatic lesions of the humerus. J Shoulder Elbow Surg. 2012;21:1049-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Noaman HH. Management of upper limb bone defects using free vascularized osteoseptocutaneous fibular bone graft. Ann Plast Surg. 2013;71:503-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Heitmann C, Erdmann D, Levin LS. Treatment of segmental defects of the humerus with an osteoseptocutaneous fibular transplant. J Bone Joint Surg Am. 2002;84-A:2216-2223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 9. | Calori GM, Colombo M, Malagoli E, Mazzola S, Bucci M, Mazza E. Megaprosthesis in post-traumatic and periprosthetic large bone defects: Issues to consider. Injury. 2014;45 Suppl 6:S105-S110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Molina CS, Stinner DJ, Obremskey WT. Treatment of Traumatic Segmental Long-Bone Defects: A Critical Analysis Review. JBJS Rev. 2014;2:pii: 01874474-201404000-00003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Bosemark P, Perdikouri C, Pelkonen M, Isaksson H, Tägil M. The masquelet induced membrane technique with BMP and a synthetic scaffold can heal a rat femoral critical size defect. J Orthop Res. 2015;33:488-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Masquelet AC. Induced Membrane Technique: Pearls and Pitfalls. J Orthop Trauma. 2017;31 Suppl 5:S36-S38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 123] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 13. | Wang T, Wang W, Yin ZS. Treatment of osteonecrosis of the femoral head with thorough debridement, bone grafting and bone-marrow mononuclear cells implantation. Eur J Orthop Surg Traumatol. 2014;24:197-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Abd-Ella MM, Galhoum A, Abdelrahman AF, Walther M. Management of Nonunited Talar Fractures With Avascular Necrosis by Resection of Necrotic Bone, Bone Grafting, and Fusion With an Intramedullary Nail. Foot Ankle Int. 2017;38:879-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |