Published online Mar 18, 2019. doi: 10.5312/wjo.v10.i3.128
Peer-review started: July 27, 2018
First decision: August 20, 2018
Revised: October 18, 2018
Accepted: November 26, 2018
Article in press: November 27, 2018
Published online: March 18, 2019
Processing time: 142 Days and 17.7 Hours
To compare rotating versus fixed-bearing Press-Fit Condylar (PFC) Sigma posterior stabilized (PS) total knee arthroplasty (TKA) with the new “J curve” femoral design in terms of clinical outcomes and anterior knee pain.
We retrospectively analyzed 39 patients who underwent primary total knee replacement surgery for knee osteoarthritis using the PFC Sigma PS TKA with either fixed (FP group, 20 cases) or rotating platform (RP group, 19 cases) treated between 2009 and 2013 by the same surgeon. The two groups were homogeneous for age, gender, weight, American Society of Anesthesiologists status, pre-operative clinical and functional scores, and prosthetic alignment at two years after surgery. We analyzed clinical outcomes score at two years follow-up using Knee Society Score (KSS), Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Performance Score, Short Form (SF) 36, and anterior knee pain assessed by the Hospital for Special Surgery (HSS) patellar score.
No differences were found in KSS, Knee Performance Score, and SF-36 outcome scores. A statistically significant difference was found in the HSS Patella score objective (FP: 22.36; RP: 28.75; P < 0.05), HSS Patella score total (FP: 73.68; RP: 86.50; P < 0.05), and KOOS symptoms (FP: 73.49; RP: 86.44; P < 0.05).
Rotating platform in PFC Sigma PS TKA appears to reduce the short-term incidence of anterior knee pain compared to the fixed platform.
Core tip: Rotating platform in Press-Fit Condylar Sigma posterior stabilized total knee arthroplasty reduces the short-term incidence of anterior knee pain compared to the fixed platform.
- Citation: Bigoni M, Zanchi N, Turati M, Pirovano G, Zatti G, Munegato D. Short-term differences in anterior knee pain and clinical outcomes between rotating and fixed platform posterior stabilized total knee arthroplasty with a new femoral component design. World J Orthop 2019; 10(3): 128-136
- URL: https://www.wjgnet.com/2218-5836/full/v10/i3/128.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i3.128
Total knee arthroplasty (TKA) has been shown to be a durable and successful treatment for end-stage arthritis of the knee[1]. Anterior knee pain is one of the major challenges after TKA and is one of the major causes of revision at five years follow-up[2-5]. The incidence of anterior knee pain after TKA is reported to be between 4 and 49%[6-10].
The causes of anterior knee pain are multifactorial, and can be functional (muscle imbalances, dynamic valgus[5]) or due to surgical and biomechanical aspects (patellofemoral compartment overstuffing[11], rotational alignment mistakes[12]). Additionally, the prosthetic design plays a role in the development of patellofemoral problems, primarily the design of the femoral component. Changes in the design of the femoral trochlear groove or in the femoral posterior condyle radius curvature have shown improvement in clinical outcomes. Femoral components with a posterior center of rotation have been shown to have a better outcome in terms of anterior knee pain[10]. This aspect has also been addressed in the design evolution of one of the most commonly used knee prosthesis.
The PFC-Sigma (DePuy Orthopaedics Inc., Warsaw, United States) TKA was introduced in 1996 as an improvement of the Press-Fit Condylar (PFC) implant (Johnson and Johnson, Raynham, Massachusetts, United States) and showed good mid-terms functional outcomes. Recently, some authors reported minor extensor mechanism complications following the use of this implant, such as patellar crepitation and patellar clunk syndrome, compared to other posterior stabilized (PS) models[13]. Because of these patellofemoral problems, the PFC-Sigma femoral component was re-designed, becoming available in 2009 under the name PFC Sigma PS available with a rotating platform and a fixed-bearing system. The principal modifications regarding the PS housing design included a “J curve” femoral design, a new femoral box, and smoother trochlear groove edges: these design changes provided better patellar tracking during range of motion (ROM)[14].
Is well known that geometry and kinematic patterns of different guided-motion prosthetic designs can affect the clinical-functional outcome in primary TKA[15]. Rotating platform TKA has numerous theoretical benefits, including the ability to self-align and accommodate small errors in component placement. If this is true, the improved patellar tracking might decrease the incidence of anterior knee pain[16].
Only a few studies[17,18] have investigated the clinical outcomes of the PFC-Sigma PS mobile-bearing versus fixed-bearing systems as a primary outcome measure. The short term clinical outcomes reported in the literature show different results depending on study design and prosthesis model[16,19-21]. This investigation aimed to compare the short term clinical and functional outcomes and the degree of anterior knee pain of these two bearing types in PS TKA with a new femoral component design at two years follow-up. The hypothesis is that mobile-bearing TKA reduces anterior knee pain by improving patellar tracking.
We considered only patients who underwent primary total knee replacement surgery for advanced degenerative knee OA, stage 3 or 4 of the Kellgren classification with limitation of daily activity, using the PFC Sigma PS TKA with either a fixed or rotating platform, treated between 2009 and 2013.
The inclusion criteria were: (1) correct prosthetic components alignment, as described by Cherian[22] (Table 1); (2) complete two years’ follow-up scores and X-rays; and (3) surgery performed by the same surgeon. Exclusion criteria were: (1) inflammatory systemic disease (e.g., rheumatoid arthritis); (2) impaired cognitive status; (3) body mass index > 40; and (4) conditions that could influence the clinical outcome (e.g., contralateral lower limb amputation, important limitation and/or pain in other joints of the lower limbs, systemic inflammatory joint disease, patients with Charnley classification B or C[23]).
| Radiographic alignment at two years, mean (SD) | FP | RP | P value |
| Anatomical axis | 174.7° (1.69°) | 175.30° (2.32°) | 0.428 |
| Mechanical axis | 179.49° (2.47°) | 181.10° (2.41°) | 0.838 |
| Anatomic lateral distal femoral angle (aLDFA) | 86.60° (3.5°) | 85.70° (2.74°) | 0.960 |
| Medial proximal tibial-angle (MPTA) | 89.84° (2.81°) | 90.31° (1.37°) | 0.084 |
| Posterior femoral-prosthetic angle | 90.3° (2.97°) | 88.51° (2.89°) | 0.753 |
| Posterior tibial-prosthetic angle | 88.9° (1.9°) | 89.07° (2.12°) | 0.790 |
| Anterior femoral-prosthetic angle | 8.2° (3.02°) | 6.42° (2.11°) | 0.262 |
| Patellar tilt angle alpha | 25.64° (7.87°) | 26.81° (4.84°) | 0.407 |
| Patellar tilt angle gamma | 1.32° (3.3°) | 1.87° (3.5°) | 0.805 |
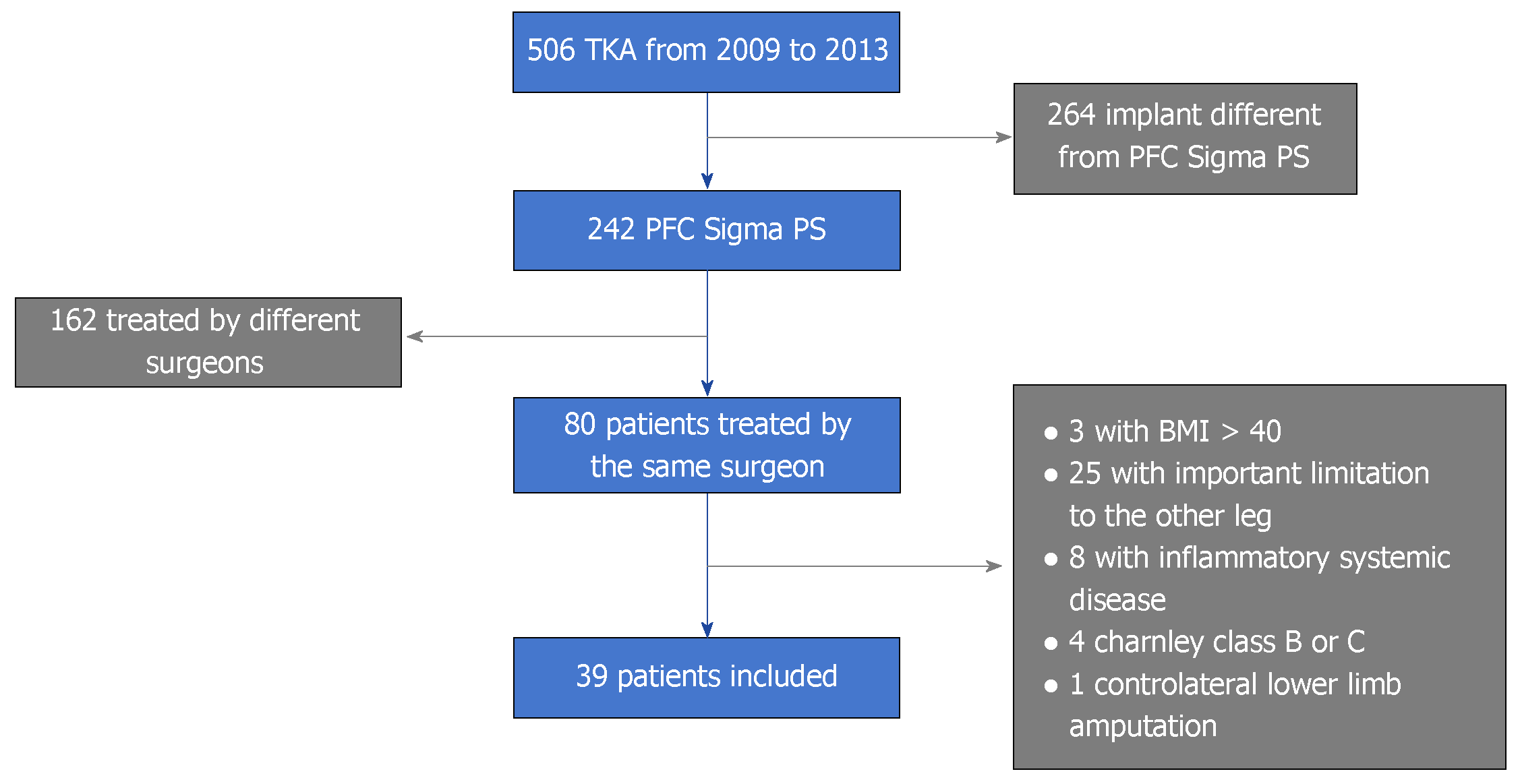
We performed in our hospital 506 TKA from 2009 to 2013 according to the previous criteria we excluded 264 patients that were implanted with different prothesis, 162 patients treated by a different surgeon and 41 patients for other reason listed in Figure 1.
Thirty-nine patients were eligible for the study criteria and we divided them in two groups: (1) DePuy Sigma Fixed Platform (FP): 20 patients; and (2) DePuy Sigma Rotating Platform (RP): 19 patients. For each patient, we retrospectively collected preoperative and postoperative data at 2 year follow-up.
The preoperative data were: demographic data, American Society of Anesthesiologists (ASA) score, functional status using the Knee Society score, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Performance Score, Short Form (36) Health Survey (SF-36), and Hospital for Special Surgery (HSS) Patellar Score.
The preoperative data were obtained during the outpatient assessment that is planned 2 wk before surgery.
At 2 years follow-up, we collected: X-ray exams (anteroposterior and lateral weight-bearing knee views, weight-bearing full length radiographs of the lower limbs, and a “Skyline” view), clinical and functional scores (subjective scores: KOOS[24] and SF-36[25]; objective scores: HSS Patella Score[26], Knee Performance Score[27], and Knee score[28]).
On the X-ray exams, we measured the anatomical axis and mechanical axis of the lower limb, the anatomic coronal and sagittal alignment of the femoral and tibial component, the angle of flexion of the femoral component with respect to the anterior cortex, and the alpha and gamma patellar angles with respect to the femoral component (Table 1)[22].
In our Hospital post-operative scores and X-rays are always requested in all the follow up outpatient visits after a TKA.
Pre-operative and follow up data were collected in 2016 retrospectively analyzing the outpatient visits.
The two groups were homogeneous for age, gender, weight, ASA status, pre-operative clinical and functional scores, and prosthetic alignment two years after surgery (Tables 1-3).
| Variable | FP | RP | P value |
| Age; yr, mean (SD) | 71.89 (9.8) | 71.70 (7.84) | 0.94 |
| Gender (% males); (M-F) | 45%; (9-11) | 36.8%; (7-12) | 0.43 |
| Weight; kg, mean (SD) | 78.36 (10.71) | 76.05 (14.32) | 0.57 |
| Pre-operative; ASA score | ASA 1: 0 (0%); ASA 2: 15 (75%); ASA 3: 5 (15%) | ASA 1: 2 (10.5%); ASA 2: 12 (63.1%); ASA 3: 5 (26.3%) | 0.85 |
| Scores before surgery, mean (SD) | FP | RP | P value |
| SF-36 | 66.63 (15.10) | 58.41 (20.30) | > 0.05 |
| KOOS | 51.2 (3.78) | 50.95 (4.07) | > 0.05 |
| HSS Patella Score | 53.15 (12.71) | 58.75 (7.04) | > 0.05 |
| Knee Performance Score | 48.68 (10.52) | 50.75 (22.43) | > 0.05 |
| Knee Score | 65.92 (9.44) | 69.77 (8.73) | > 0.05 |
The study protocol was approved by the local research ethic committee and all procedure was in accordance with the Helsinki Declaration of 1975, as revised in 2000.
Statistical analysis was performed using SPSS Version 16.0 software (SPSS Inc., Chicago, IL, United States). The chi-square test and the Fisher’s exact test were used to evaluate categorical data, in particular, the evaluation of gender and ASA score. We verified the normality of the data of each group with the Shapiro-Wilk test. The Student T-test was used to compare results with a normal distribution, and the Mann-Whitney test was used to evaluate groups without a normal distribution. For all statistical analysis, the significance threshold was set at a P-value of less than 0.05. A statistical review of the study was performed by a Biomedical Statistician.
The surgery was performed by the same surgeon (GZ), fellowship-trained in Joint Replacement Surgery. Every procedure was performed with spinal anesthesia. A first-generation cephalosporin (Cefamezin®, Pfizer, New York City, United States) was used as short-term antibiotic prophylaxis, administered 30 min preoperatively and 8 h and 16 h postoperatively, according to our institutional protocol. A tourniquet was applied before skin incision and deflated after the cemented component placement. A standard medial parapatellar approach was used, and the cruciate ligaments were removed. Distal femoral resection was done first using an intramedullary alignment guide, and then the proximal tibial resection was done with an extramedullary guide. The extension gap was then evaluated with spacer block and balanced if needed. The femoral component was externally rotated by 3°, using the posterior condyle line as a reference. Then, with the four in one cutting block in place, the flexion gap at 90° was checked using a spacer block 2 mm thinner than the extension spacer block to compensate for the thickness of the cutting block. If the extension and flexion gap were balanced, the remaining femoral cuts were performed. If the two gap were unbalanced, the flowchart described by Bottros[29] was used to balance them. The trial components were then positioned and limb alignment, range of movement, and the flexion-extension gaps were checked. The rotational alignment of the tibial component was determined using either the third part of the anterior tibial tuberosity or the dynamic flexion-extension alignment.
All patients were implanted with cemented PFC Sigma PS (DePuy Orthopaedics Inc., Warsaw, United States). The new design features included a “J curve” femoral design, three different tangential radius curves in the sagittal profile, and an increased radius in transition from anterior flange to the box to enhance patella tracking during flexion while reducing the risk of soft tissue impingement and associated patella crepitus. The blending radii around the medial and lateral edges of the femur have been increased to provide a smoother transition to reduce the risk of soft tissue impingement.
Fixed bearings with oxidatively stable cross-linked polyethylene were implanted until May 2010 and mobile bearings with super polished GVF until 2013.
The patellae were treated by denervation and patelloplasty without replacement in all patients.
A standard TKA rehabilitation protocol was performed. On the second post-operative day, physical therapy and continuous passive motion were started in all patients. After approximately 5 d in the hospital, patients were followed in a rehabilitation service for 3 wk.
The clinical and functional evaluation with scores 24 months after surgery demonstrated the following results (Table 4).
| Scores two yr after surgery, mean (SD) | FP | RP | P value |
| SF-36 | 75.94 (17.27) | 65.10 (22.40) | > 0.05 |
| KOOS symptoms | 73.49 (17.63) | 86.44 (8.39) | < 0.05 |
| HSS Patella Score; HSS Patella Score objective | 73.68 (16.73); 22.36 (6.74) | 86.50 (12.98); 28.75 (6.66) | < 0.05; < 0.05 |
| Knee Performance Score | 80.26 (14.85) | 74.75 (10.52) | > 0.05 |
| Knee Score | 83.94 (12.35) | 87.52 (10.08) | > 0.05 |
The average SF-36 score was 75.94 (SD: ±17.27; range: 35.87-93.75) in the FP group and 65.1 (SD: ±22.4; range 19.50-95.5) in the RP group, in favour of the FP group. Knee Performance Score in the FP group was 80.26 (SD: ±14.85; range: 45-100) and 74.75 (SD: ±10.52; range 15-100) in the RP group, in favour of the FP group. Knee Score in the FP group was 83.94 (SD: ±12.35; range: 47-100) and 87.52 (SD: ±10.08; range: 67-100) in the RP group, in favour of the RP group. Considering these scores, we did not identify a statistically significant difference between groups.
Analyzing the KOOS total score, there was no statistically significant differences between groups, but evaluation of subsections of the score demonstrated differences. A statistically significant difference was found in the KOOS symptoms subsection, with a mean score of 73.49 (SD: ±17.63; range 32.14-96.93) in the FP group and 86.44 (SD: ±8.39; range 67.86-100) in the RP group (P < 0.05), in favour of the RP.
We found a statistically significant difference in the HSS Patella total score; values were 73.68 (SD: ±16.73; range 35-95) in the FP group and 86.50 (SD: ±12.98; range 50-100) and in the RP group (P < 0.05) in favour of the RP group. For the HSS Patella score objective subsection, values were 22.36 (SD: ±6.74; range 15-35) in the FP group and 28.75 (SD: ±6.66; range 10-35) in the RP group (P < 0.05), in favour of the RP group.
We didn’t found any major complication like infection, mobilization, patella dislocation or instability.
Minor complication were reported in two patients; they both developed a delayed wound healing, no surgical revision was necessary.
These two patients were heavy smoker, wound healing was achieved respectively in 4 and 6 week with weakly advanced dressing.
Mobile-bearing designs were introduced in TKA to decrease polyethylene wear by increasing the conformity of the implant in sagittal and coronal planes, without restricting the rotational freedom of the bearing. Several studied have confirmed that, in comparison to fixed-bearing designs, mobile-bearing designs result not only in decreased polyethylene wear, but also lower grade and more symmetrical wear[30-34]. Other advantage of mobile bearings were postulated, including more physiological knee kinematics and a facilitation of central patellar tracking by self-alignment[35,36].
In an intra-operative kinematic study, Sawaguchi et al[37] demonstrated that there was significantly improved patellar tracking with decreased patellofemoral contact stresses, because the rotating platform design, through bearing rotation, permits self-correction of component rotational mal-alignment, allowing better centralization of the extensor mechanism. This process of self-alignment might be expected to improve patellar tracking and reduce anterior knee pain, one of the major short term complaints after TKA[2-6]. The rotating platform also permits adaptation to inferior limb rotational defects, improving patello-femoral contact stresses[38].
Several studies have analyzed knee kinematics, functional outcome, and long-term survivorship of the rotating platform versus fixed platform as the primary outcome measure[39-41]. Symptoms were usually considered as secondary measures in rotating platform studies, because this component was primarily thought to increase survivorship of the implant thanks to increased implant conformity and contact area with reduced stress transmitted to the fixation interface and a lower and more symmetrical wear rate.
Recent meta-analyses[40,41] did not identify a clinical difference between mobile-bearing and fixed-bearing systems. Although a meta-analysis is advantageous compared to primary-source studies in terms of increased statistical power, it can be substantially affected by the weaknesses and heterogeneity of original studies (different implant models, different surgeons, different clinical scores). For example, not all mobile-bearings designs are the same and, often, different types of mobile-bearing system were grouped together for comparison against fixed-bearing implants.
Breugem et al[16], in a prospective double-blind study, found less anterior knee pain with PS mobile-bearing prosthesis compared to fixed-bearing systems of the same model with a 1 year follow-up and no difference in anterior knee pain after 7.9 years in the same group[7]. The patients included in the study were treated by three different fellowship-trained surgeons and clinical evaluation was made by four orthopedic surgeons. Kim et al[21] found better short terms clinical outcomes (2 years follow-up) in patients with the PFC Sigma DePuy rotating platform implant compared to the fixed platform of the same model.
The specific strengths of the current study are that all patients were treated by the same fellowship-trained surgeon with the same prosthesis model and the clinical valuation was made by the same orthopedic surgeon on a strongly selected population homogeneous for age, gender, pre-operative clinical status, comorbidities, and optimal prosthesis positioning.
We also recognize limitations of our study. First, this is a limited sample study, which could lead to a lack of power to detect clinically important differences. Second, this is a retrospective study with the relative disadvantage compared to a prospective one. We recommend more structured studies with a larger number of patients to support our results.
We found a significant difference in the HSS patella objective score in favor of the RP group, mainly due to the tenderness during palpation of the patella facet section. This result could reflect the reduction of stress forces on the patella and retinaculum ligament with the mobile-bearing prosthesis. A difference in KOOS symptoms in favor of the mobile-bearing system was also observed. This outcome investigates symptoms such as clicking, grinding, or stiffness during the ROM that are frequently report in patients with anterior knee pain. In this series, patients treated with the PFC Sigma PS TKA rotating platform showed better clinical outcomes compared with patients treated with the fixed system, with two years of follow-up. We choose this timing of follow-up to avoid any influence on the clinical outcome such as operative pain and psychological and functional limitation due to the rehabilitation period.
In conclusion, our data support the concept that the rotating platform prosthesis reduces the short-term incidence of anterior knee pain compared to the fixed platform system of the PFC Sigma PS TKA with “J curve” femoral design. Longer follow-up will determine whether this difference will persist or decrease.
Anterior knee pain is one of the most common complications after total knee arthroplasty (TKA). Several aspects can cause this problem included muscle imbalances, dynamic valgus, patellofemoral compartment overstuffing, rotational alignment mistakes and prosthetic design.
In 2009 Press-Fit Condylar (PFC) Sigma femoral component was re-designed in order to improve patellar tracking and reduce anterior knee pain.
This new knee prothesis was available with rotating or fixed platform under the name of PFC Sigma posterior stabilized (PS).
Only a few studies have analyzed clinical results of this new prothesis as primary outcome.
The aim to this study is to compare rotating versus fixed-bearing PFC Sigma PS with the new “J curve” femoral design in terms of clinical outcomes and anterior knee pain with two years of follow up.
Retrospective study with 39 patients underwent primary TKA with PFC Sigma PS TKA.
We analyzed clinical outcomes two years after surgery with Knee Society Score Knee Society score, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Performance Score, Short Form Health Survey (SF-36), and Hospital for Special Surgery (HSS) Patellar Score.
We found better clinical results (HSS Patellar score and KOOS) in PFC Sigma PS rotating platform compared to fixed platform.
PFC Sigma PS rotating platform reduce the short term incidence of anterior knee pain compared to the fixed platform model and improve clinical outcomes.
Long term follow up studies will be useful to understand if this difference will be unchanged over time.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Robertson JA, Papachristou G S- Editor: Dou Y L- Editor: A E- Editor: Wu YXJ
| 1. | NIH Consensus Statement on total knee replacement. NIH Consens State Sci Statements. 2003;20:1-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Watanabe T, Tomita T, Fujii M, Hashimoto J, Sugamoto K, Yoshikawa H. Comparison between mobile-bearing and fixed-bearing knees in bilateral total knee replacements. Int Orthop. 2005;29:179-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007;464:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 4. | Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88:734-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 100] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Petersen W, Rembitzki IV, Brüggemann GP, Ellermann A, Best R, Koppenburg AG, Liebau C. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop. 2014;38:319-328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 165] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 6. | Aglietti P, Baldini A, Buzzi R, Lup D, De Luca L. Comparison of mobile-bearing and fixed-bearing total knee arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 94] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Breugem SJ, van Ooij B, Haverkamp D, Sierevelt IN, van Dijk CN. No difference in anterior knee pain between a fixed and a mobile posterior stabilized total knee arthroplasty after 7.9 years. Knee Surg Sports Traumatol Arthrosc. 2014;22:509-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Ji HM, Ha YC, Baek JH, Ko YB. Advantage of minimal anterior knee pain and long-term survivorship of cemented single radius posterior-stabilized total knee arthroplasty without patella resurfacing. Clin Orthop Surg. 2015;7:54-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Smith H, Jan M, Mahomed NN, Davey JR, Gandhi R. Meta-analysis and systematic review of clinical outcomes comparing mobile bearing and fixed bearing total knee arthroplasty. J Arthroplasty. 2011;26:1205-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | van Jonbergen HP, Reuver JM, Mutsaerts EL, Poolman RW. Determinants of anterior knee pain following total knee replacement: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22:478-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 11. | Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Amis AA. The effect of overstuffing the patellofemoral joint on the extensor retinaculum of the knee. Knee Surg Sports Traumatol Arthrosc. 2009;17:1211-1216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Breugem SJ, Haverkamp D. Anterior knee pain after a total knee arthroplasty: What can cause this pain? World J Orthop. 2014;5:163-170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Ranawat AS, Ranawat CS, Slamin JE, Dennis DA. Patellar crepitation in the P.F.C. sigma total knee system. Orthopedics. 2006;29:S68-S70. [PubMed] |
| 14. | Indelli PF, Marcucci M, Pipino G, Charlton S, Carulli C, Innocenti M. The effects of femoral component design on the patello-femoral joint in a PS total knee arthroplasty. Arch Orthop Trauma Surg. 2014;134:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Mugnai R, Digennaro V, Ensini A, Leardini A, Catani F. Can TKA design affect the clinical outcome? Comparison between two guided-motion systems. Knee Surg Sports Traumatol Arthrosc. 2014;22:581-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Breugem SJ, Sierevelt IN, Schafroth MU, Blankevoort L, Schaap GR, van Dijk CN. Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Relat Res. 2008;466:1959–1965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Chen LB, Tan Y, Al-Aidaros M, Wang H, Wang X, Cai SH. Comparison of functional performance after total knee arthroplasty using rotating platform and fixed-bearing prostheses with or without patellar resurfacing. Orthop Surg. 2013;5:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Ferguson KB, Bailey O, Anthony I, James PJ, Stother IG, M J G B. A prospective randomised study comparing rotating platform and fixed bearing total knee arthroplasty in a cruciate substituting design--outcomes at two year follow-up. Knee. 2014;21:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Marques CJ, Daniel S, Sufi-Siavach A, Lampe F. No differences in clinical outcomes between fixed- and mobile-bearing computer-assisted total knee arthroplasties and no correlations between navigation data and clinical scores. Knee Surg Sports Traumatol Arthrosc. 2015;23:1660-1668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Lampe F, Sufi-Siavach A, Bohlen KE, Hille E, Dries SP. One year after navigated total knee replacement, no clinically relevant difference found between fixed bearing and mobile bearing knee replacement in a double-blind randomized controlled trial. Open Orthop J. 2011;5:201-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Kim YH, Yoon SH, Kim JS. Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res. 2009;467:493-503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Issa K, Mont MA. Mechanical, Anatomical, and Kinematic Axis in TKA: Concepts and Practical Applications. Curr Rev Musculoskelet Med. 2014;7:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 184] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 23. | Bjorgul K, Novicoff WM, Saleh KJ. Evaluating comorbidities in total hip and knee arthroplasty: available instruments. J Orthop Traumatol. 2010;11:203-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 129] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 24. | Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2362] [Cited by in RCA: 2817] [Article Influence: 104.3] [Reference Citation Analysis (0)] |
| 25. | Lohr KN, Aaronson NK, Alonso J, Burnam MA, Patrick DL, Perrin EB, Roberts JS. Evaluating quality-of-life and health status instruments: development of scientific review criteria. Clin Ther. 1996;18:979-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 405] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 26. | Badhe N, Dewnany G, Livesley PJ. Should the patella be replaced in total knee replacement? Int Orthop. 2001;25:97-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S208-S228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 672] [Cited by in RCA: 873] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 28. | Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;13-14. [PubMed] |
| 29. | Bottros J, Gad B, Krebs V, Barsoum WK. Gap Balancing in Total Knee Arthroplasty. J Arthroplasty. 2006;21:11-15. [RCA] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Bartel DL, Bicknell VL, Wright TM. The effect of conformity, thickness, and material on stresses in ultra-high molecular weight components for total joint replacement. J Bone Joint Surg Am. 1986;68:1041-1051. [PubMed] |
| 31. | D'Lima DD, Trice M, Urquhart AG, Colwell CW. Tibiofemoral conformity and kinematics of rotating-bearing knee prostheses. Clin Orthop Relat Res. 2001;235-242. [PubMed] |
| 32. | McEwen HM, Barnett PI, Bell CJ, Farrar R, Auger DD, Stone MH, Fisher J. The influence of design, materials and kinematics on the in vitro wear of total knee replacements. J Biomech. 2005;38:357-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 204] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 33. | Otto JK, Callaghan JJ, Brown TD. Gait cycle finite element comparison of rotating-platform total knee designs. Clin Orthop Relat Res. 2003;181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Ho FY, Ma HM, Liau JJ, Yeh CR, Huang CH. Mobile-bearing knees reduce rotational asymmetric wear. Clin Orthop Relat Res. 2007;462:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 35. | Delport HP, Banks SA, De Schepper J, Bellemans J. A kinematic comparison of fixed- and mobile-bearing knee replacements. J Bone Joint Surg Br. 2006;88:1016-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 36. | Rees JL, Beard DJ, Price AJ, Gill HS, McLardy-Smith P, Dodd CA, Murray DW. Real in vivo kinematic differences between mobile-bearing and fixed-bearing total knee arthroplasties. Clin Orthop Relat Res. 2005;204-209. [PubMed] |
| 37. | Sawaguchi N, Majima T, Ishigaki T, Mori N, Terashima T, Minami A. Mobile-bearing total knee arthroplasty improves patellar tracking and patellofemoral contact stress: in vivo measurements in the same patients. J Arthroplasty. 2010;25:920-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 38. | Peersman G, Taeymans K, Jans C, Vuylsteke P, Fennema P, Heyse T. Malrotation deformities of the lower extremity and implications on total knee arthroplasty: a narrative review. Arch Orthop Trauma Surg. 2016;136:1491-1498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Martin JR, Beahrs TR, Fehring KA, Trousdale RT. Rotating platform versus fixed bearing total knee arthroplasty at mid-term follow-up. Knee. 2016;23:1055-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Carothers JT, Kim RH, Dennis DA, Southworth C. Mobile-bearing total knee arthroplasty: a meta-analysis. J Arthroplasty. 2011;26:537-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 41. | Moskal JT, Capps SG. Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res. 2014;472:2185-2193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |