Published online Feb 18, 2019. doi: 10.5312/wjo.v10.i2.90
Peer-review started: November 10, 2018
First decision: December 7, 2018
Revised: January 22, 2019
Accepted: January 26, 2019
Article in press: January 26, 2019
Published online: February 18, 2019
Processing time: 104 Days and 15.7 Hours
Total hip and knee replacements are being performed in increasing numbers in progressively younger patients with higher activity demands. Many such patients have expectations of returning to athletic activity post-operatively yet are not always able to do so and the reasons behind this have not been extensively examined. We hypothesise that any reasons for a failure to return to athletic activity post-operatively are multi-factorial.
To quantify the return to athletic activity following lower limb joint arthroplasty and understand qualitative reasons for altered activity participation.
A single centre, single surgeon retrospective questionnaire for hip and knee arthroplasty patients under age 60 years, minimum two years post-surgery with exclusion criteria of multiple degenerative joint involvement and multiple medical co-morbidities. Outcomes were validated joint-specific (Oxford hip and knee) and lifestyle questionnaires [short form 12 (SF-12) and University of California, Los Angeles (UCLA)] and an activity questionnaire assessing ability participation in athletic activity post-operatively. Statistical analysis was performed on the validated outcome data, including comparison between hip and knee replacements. Frequency tables were produced to quantify the different athletic activities participated in by patients.
Responses were received from 64 patients (80% response rate). There was a statistically significant improvement in Oxford hip and knee scores following surgery. SF-12 scores also improved for all patients, but no statistically significant difference was seen between joints (P = 0.88). Mean UCLA scores pre-operatively were 7.67 and at two years post-operatively were 7.69, with no statistically significant change (P = 0.91). All patients reported high satisfaction and improved ability to perform athletic activity at a higher frequency compared to pre-operatively. The most common reasons for changing activity participation were not wanting to stress their joint replacement or instructions by other doctors or the lead surgeon. There was no difference in the responses to the questionnaire based on type of joint replacement (P = 0.995).
Patients receiving a joint replacement are able to participate in athletic activity to high levels and are satisfied with their outcomes. Reasons for non-participation are multi-factorial.
Core tip: Returning to athletic activity is an important goal for many younger patients undergoing hip or knee arthroplasty. Up until now, it is known that, whilst some are able to return to athletic activity, not all patients return to their chosen activity. This qualitative study demonstrates that patients are highly satisfied with their arthroplasty with respect to returning to athletic activity but the reasons for changing their activity of choice varies equally from decisions made by the patient themselves to instructions provided by their surgeon or other medical practitioner.
- Citation: Jassim SS, Tahmassebi J, Haddad FS, Robertson A. Return to sport after lower limb arthroplasty - why not for all? World J Orthop 2019; 10(2): 90-100
- URL: https://www.wjgnet.com/2218-5836/full/v10/i2/90.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i2.90
Total joint replacement (TJR) is an increasingly-performed orthopaedic operation in the United Kingdom[1] and the patient groups having these operations are progressively younger with high activity levels and thus high demands. Sophisticated measures have been developed to more closely reflect health gains associated with TJR beyond mortality and morbidity rates, operative complications and implant survival[2,3]. General function has been shown to improve following TJR but an important and often-neglected consideration are the levels of athletic participation following these operations in younger populations; this has particular relevance given that athletes are at greater risk of developing osteoarthritis of the hip and knee[4-6]. Such patients will have high expectations of continuing to participate in athletic activity following surgery[7].
Relatively few studies have investigated return to sporting activity following TJR. Conflicting opinions have emerged about the suitability of athletic activity following total hip replacement (THR)[8-12] and total knee replacement (TKR)[13,14]. Recent studies analysing the return to sport for both TKR and THR patients were unable to find a difference in rates between the two joints[15,16]. It has, however, been demonstrated that rather than the type of implant received, characteristics such as male sex, lower age, lower BMI and a high pre-operative level of sport participation predicted increased chances of return to athletic activity post-TJR[17].
In addition, TJR patients participating in athletic activities may be at increased risk of acute complications, such as periprosthetic fracture or dislocation; repetitive loading of the implant may pre-dispose to osteolysis and subsequent aseptic loosening[18]. Implant retrieval studies in TKR patients have demonstrated a statistically significant correlation between rates of linear and volumetric wear and University of California, Los Angeles (UCLA) activity scores[19]; similar associations are seen in THR populations[20].
Therefore, although participation in sporting activity is possible post-TJR, it has also been demonstrated that there is a decline in high-impact activities and no studies have explicitly considered specific reasons for the failure of patients to continue with such high-impact activity following TJR. Understanding this is key so that patients considering TJR can be well informed regarding their post-operative prognosis for sporting participation. The aim of this study is to investigate the activity levels and rate of return to athletic activity post arthroplasty and identify qualitative reasons for changes in activity participation.
A single centre, single surgeon, retrospective questionnaire study was designed. Ethical board approval was received. From the personal database of the lead surgeon (FSH), a list of patients who have received either THR or TKR was obtained with at least 2 years’ follow-up. Patients were excluded if they were over the age of 65 years, had an American Society of Anaesthesiologists (ASA) grade of greater than 2 or another joint replacement in situ in order to control for factors that are known to reduce participation in sports post arthroplasty and confound results[17].
Participation in sports after arthroplasty was determined with the use of self-administered validated activity and lifestyle questionnaires and a subjective activity-related questionnaire. The Oxford Knee and Hip Scores (OKS, OHS)[21] were used to assess the joint-specific functional abilities of the patients. The short form 12 (SF-12) was used to assess the general lifestyle of the patient and has also been validated following TJR[22]. The UCLA activity scale was used to determine participation in functional activity related to sports and correlates most closely with other functional activity scores in comparison to the Tegner score[23]. Patients were asked to complete one UCLA score for the time just prior to their operation and one for their current activity levels. A questionnaire was designed to specifically assess patients’ participation levels in sporting activity and reasons behind a lack of participation of sports (if any) (Appendix 1). All patients under the care of the lead surgeon have their OKS/OHS and SF-12 scores collected at the time of surgery as routine practice; these scores were used as their baseline measurements.
A total of 80 suitable patients were selected from the database. All patients were contacted by telephone to gain consent for participation. Instructions for completing questionnaires were given with a further option for contact after receipt of the questionnaire to discuss any points for clarification. All patients agreeing to participate received the above questionnaires either via email or via post with a stamped-return envelope. After two weeks, 52 questionnaires were received. The remainder received a telephone call as a reminder and 8 further responses were received. Two weeks following this, the remaining non-responding patients received a telephone call as a reminder. The final number of questionnaires received was 64, giving a total 80% response rate. Upon collection of all data, the scores were entered into a secure database. The sample mean and standard deviation was calculated for the OHS, OKS, SF-12 and UCLA scores. Frequency tables were made for the responses to the sports activity questionnaire.
Descriptive statistical testing was done using XLSTAT software version 7 (Addinsoft, New York, United States) and separate analysis was performed for THR and TKR patients. A Shapiro-Wilk calculation demonstrated the scores were normally distributed and a paired t-test was used to compare outcomes within the different joint replacements at baseline and at two years, whilst an independent t-test was used to compare the outcomes of SF-12 and UCLA scores between THR and TKR patients. Chi-squared testing was used to compare the outcomes of the activity questionnaire. A significance level of P = 0.05 was set.
A total of 80 questionnaires were sent out to eligible participants and a total of 64 completed forms were received, giving a response rate of 80%. All patients were a minimum of two years since their operation. Their demographics are presented in Table 1.
| THR | TKR | Total | |
| Number of patients | 40 | 24 | 64 |
| Mean age (SD; range) in years | 53.1 (8.4; 33-64) | 60 (2.5; 54-64) | 55.7 (7.5; 33-64) |
| Sex M:F | 19:21 | 10:14 | 29:35 |
| Mean time since operation (SD; range) in years | 3.3 (1.1; 2.5-5) | 3 (0.9; 2-4.5) | 3.1 (0.9; 2-5) |
There was an increase between mean baseline and two-year OHS and OKS scores (Table 2), which was statistically significant (P < 0.0001). There was an increase between the mean baseline and two-year SF-12 scores for both the physical and mental portions which was statistically significant (P < 0.0001). The difference between the two joint cohorts demonstrated a higher mean physical score for the TKR cohort but no statistically significant difference between the two joints using an independent t-test at two years post-TJR (P = 0.88) and a higher mean mental score for the TKR cohort at two years post-TJR which was statistically significant (P = 0.005).
| THR | TKR | Total | |
| OHS/OKS | |||
| Mean Baseline score (SD; range) | 21.25 (4.8; 13-35) | 25.08 (5.8; 14-36) | - |
| Mean 2-yr post-TJR score (SD; range) | 40.68 (3.1; 35-47) | 41.67 (4; 33-47) | - |
| SF-12 | |||
| Mean Baseline Physical score (SD; range) | 35.9 (6.3; 22.2-49.8) | 37 (9.7; 15.4-51.9) | 36.29 (7.7; 15.4-51.9) |
| Mean 2-yr Physical post-TJR score (SD; range) | 46.1 (6.4; 29.2-60.3) | 46.4 (9.5; 29.3-61.8) | 46.19 (7.6; 29.2-61.8) |
| Mean Baseline Mental score (SD; range) | 48.4 (7.9; 24.1-68.9) | 54.3 (8.3; 34.1-68.7) | 50.52 (8.5; 24.1-68.9) |
| Mean 2-yr Mental post-TJR score (SD; range) | 55.2 (6.7; 33.4-69) | 57.7 (7.9; 37.3-69.3) | 54.16 (7.5; 33.4-69.3) |
| UCLA scores | |||
| Mean Baseline score (SD; range) | 7.78 (1.2; 6-10) | 7.5 (1.1; 6-10) | 7.67 (1.2; 6-10) |
| Mean 2-yr post-TJR score (SD; range) | 7.93 (1.2; 6-10) | 7.29 (0.9; 6-9) | 7.69 (1; 6-10) |
The mean baseline UCLA score for the entire cohort was 7.67 (range 6-10). At two years, the mean score was 7.69 (range 6-10) with no statistically significant difference (P = 0.91) between baseline and two year scores. Nine patients had an improvement in their score at 2 years whilst seven patients had a decrease in their score; 48 patients had the same score. Within the joints, there was an increase in the mean UCLA score in THR patients (7.78 to 7.93) and a decrease in TKR patients (7.5 to 7.29). Neither of these results was statistically significant (P = 0.47 for THR cohort and P = 0.17 for TKR cohort). The difference between the two joint cohorts is shown in Table 2, demonstrating that THR patients had a higher mean 2 year UCLA score than the TKR cohort; this was found to be statistically significant (P = 0.03). There were no dislocations and no revisions for fracture, infection or instability amongst the patients.
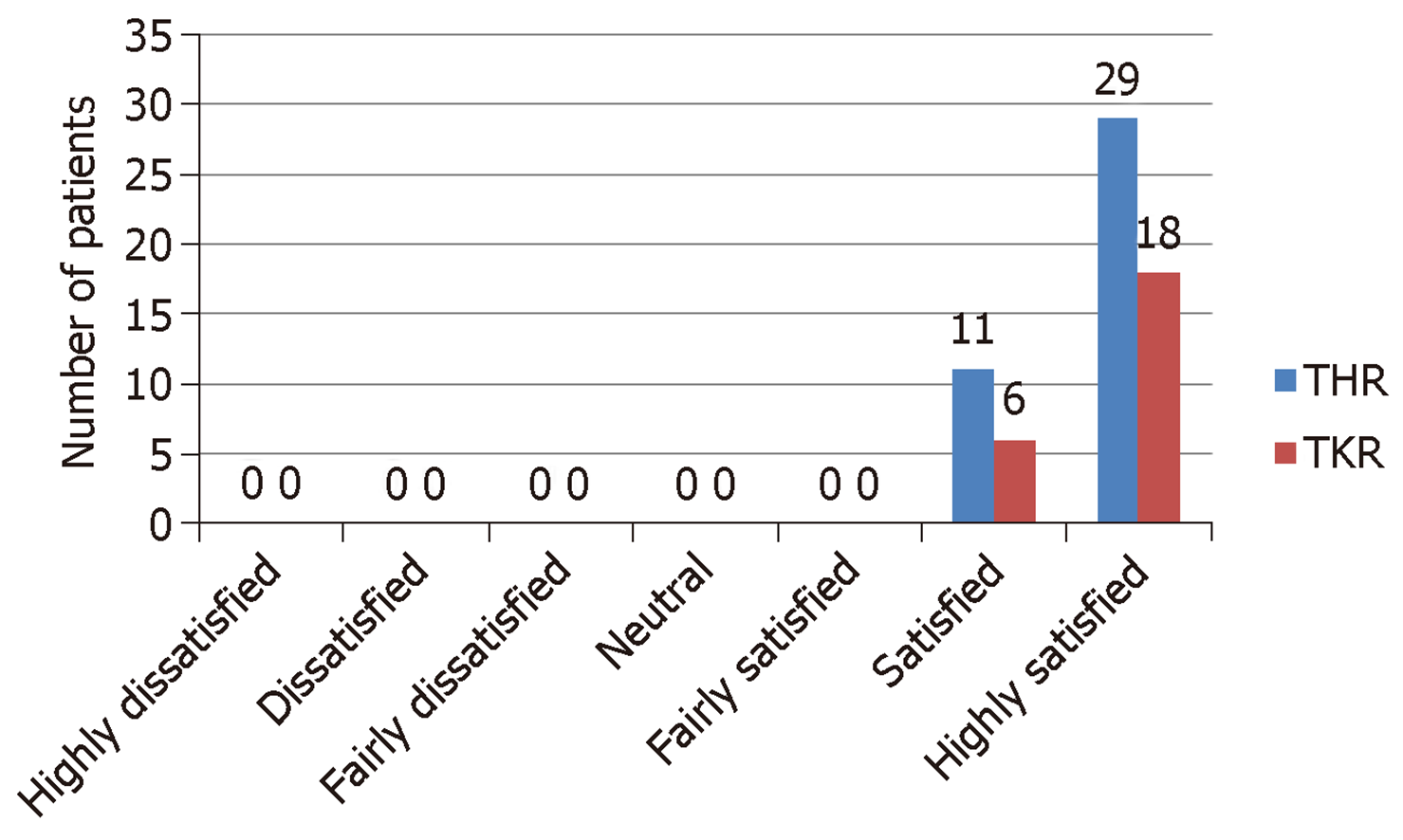
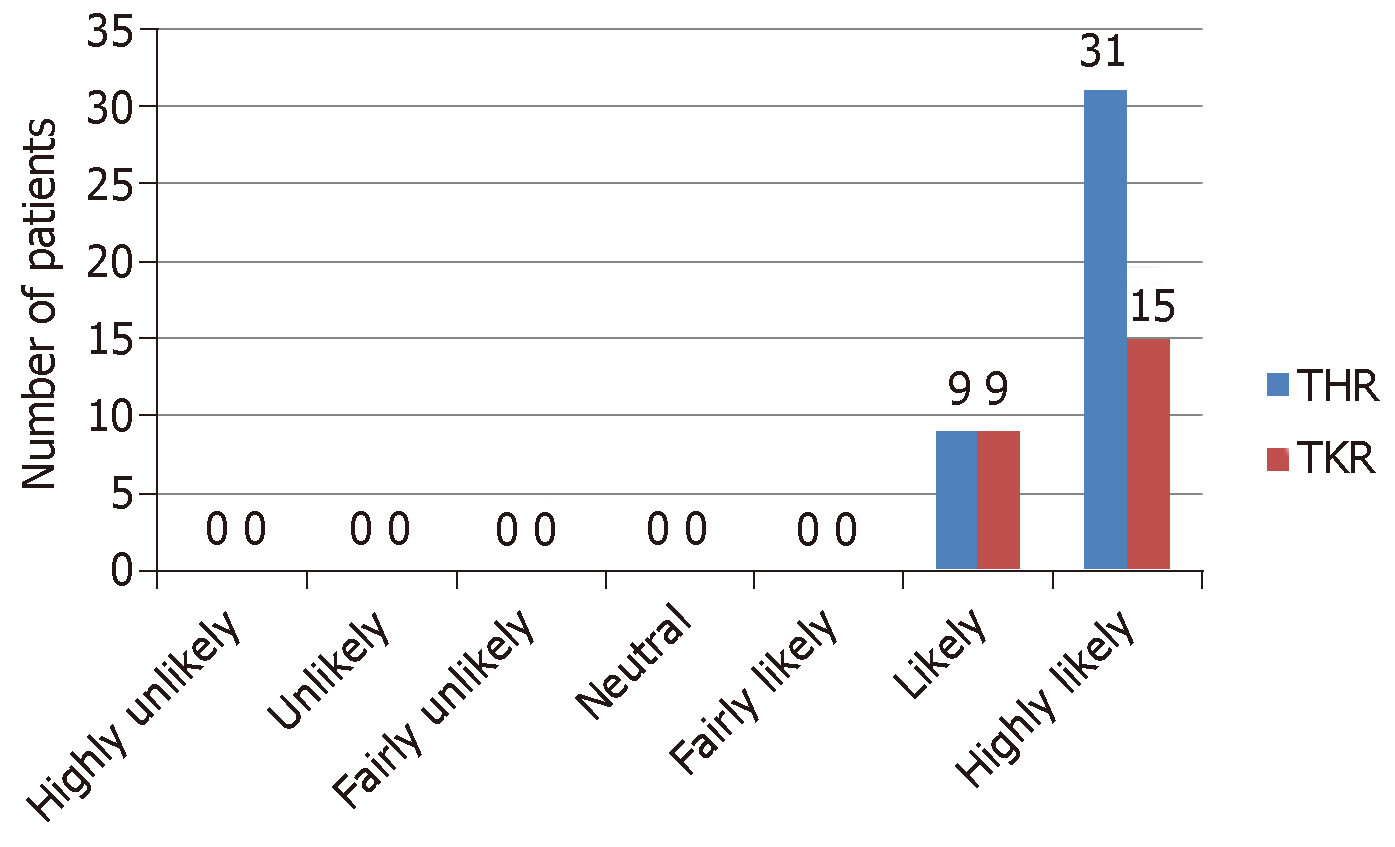
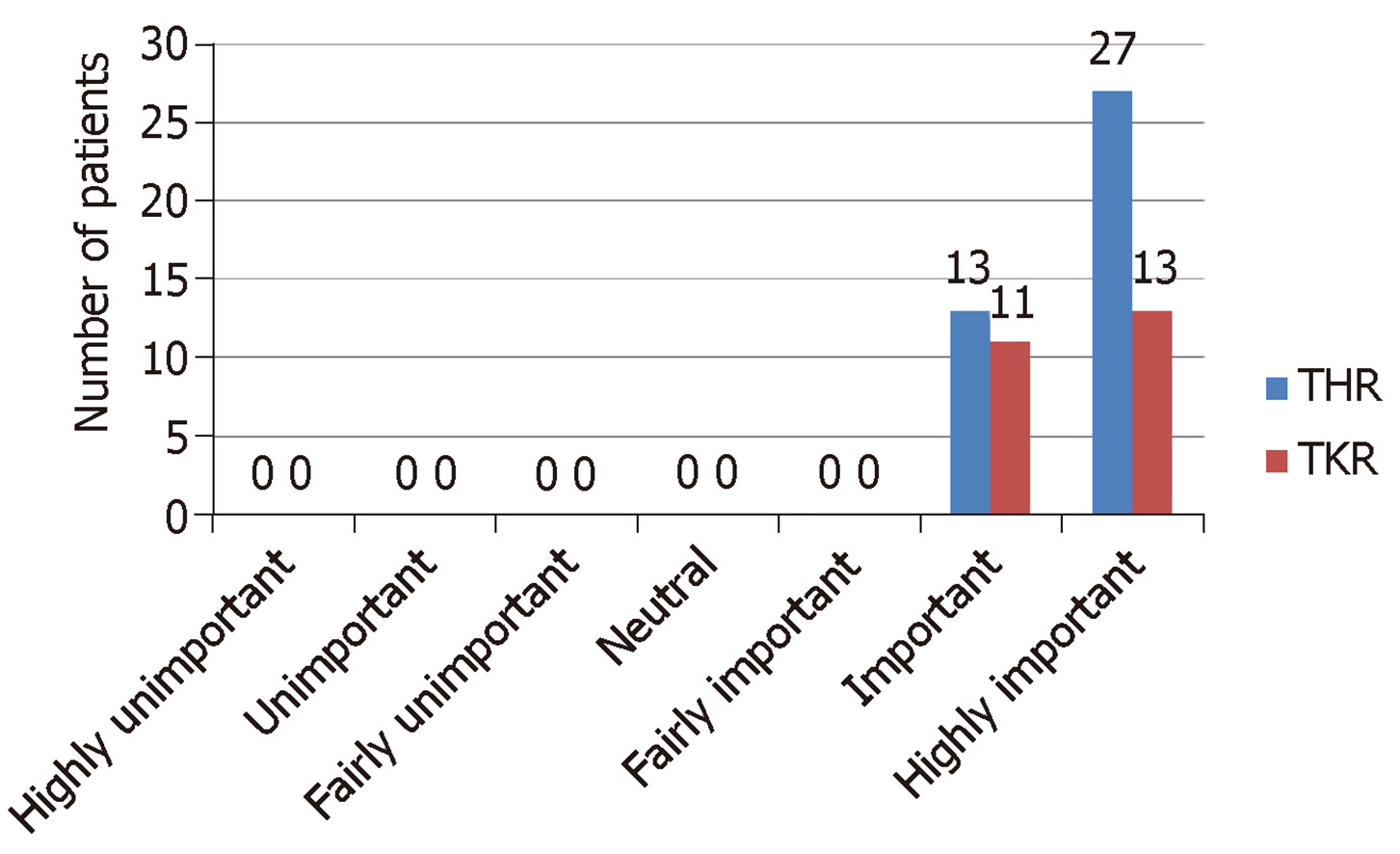
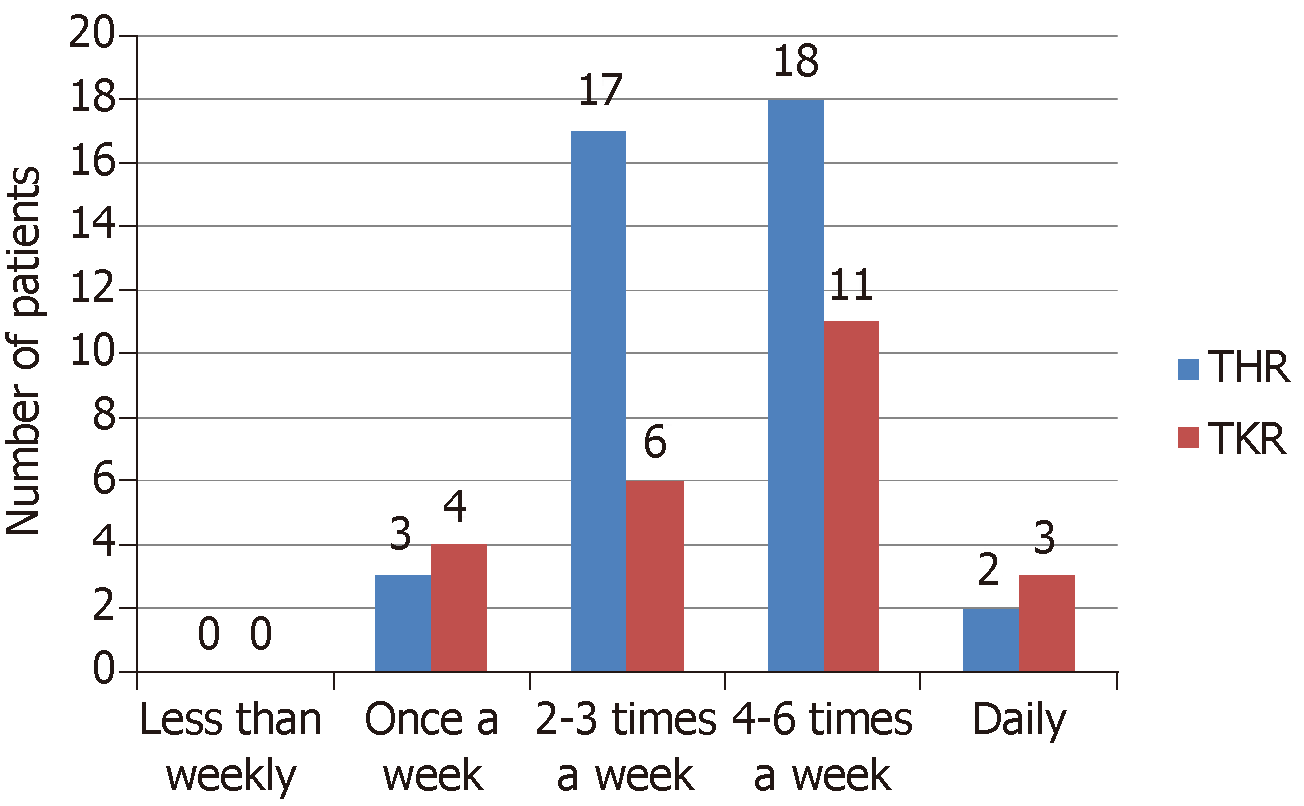
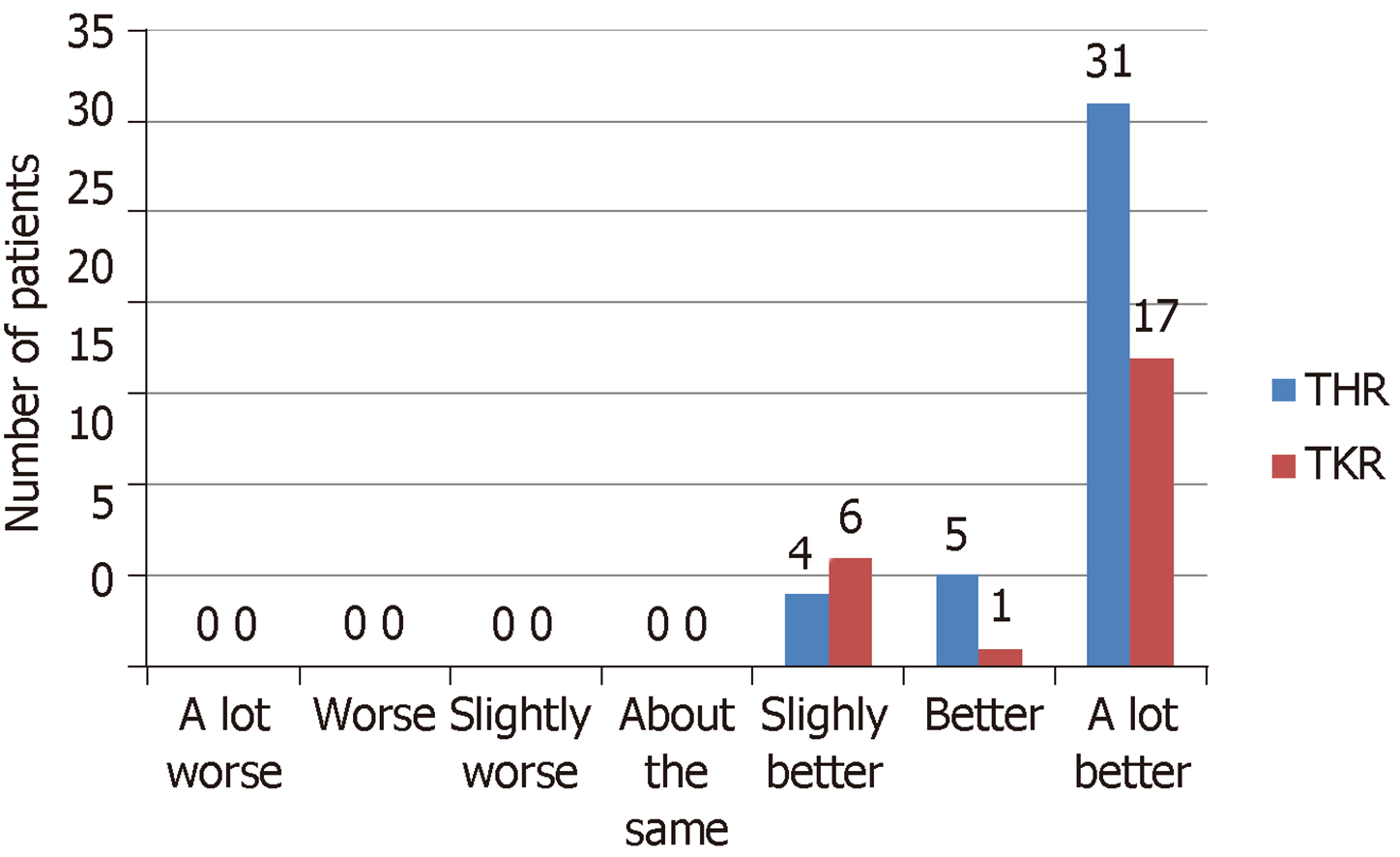
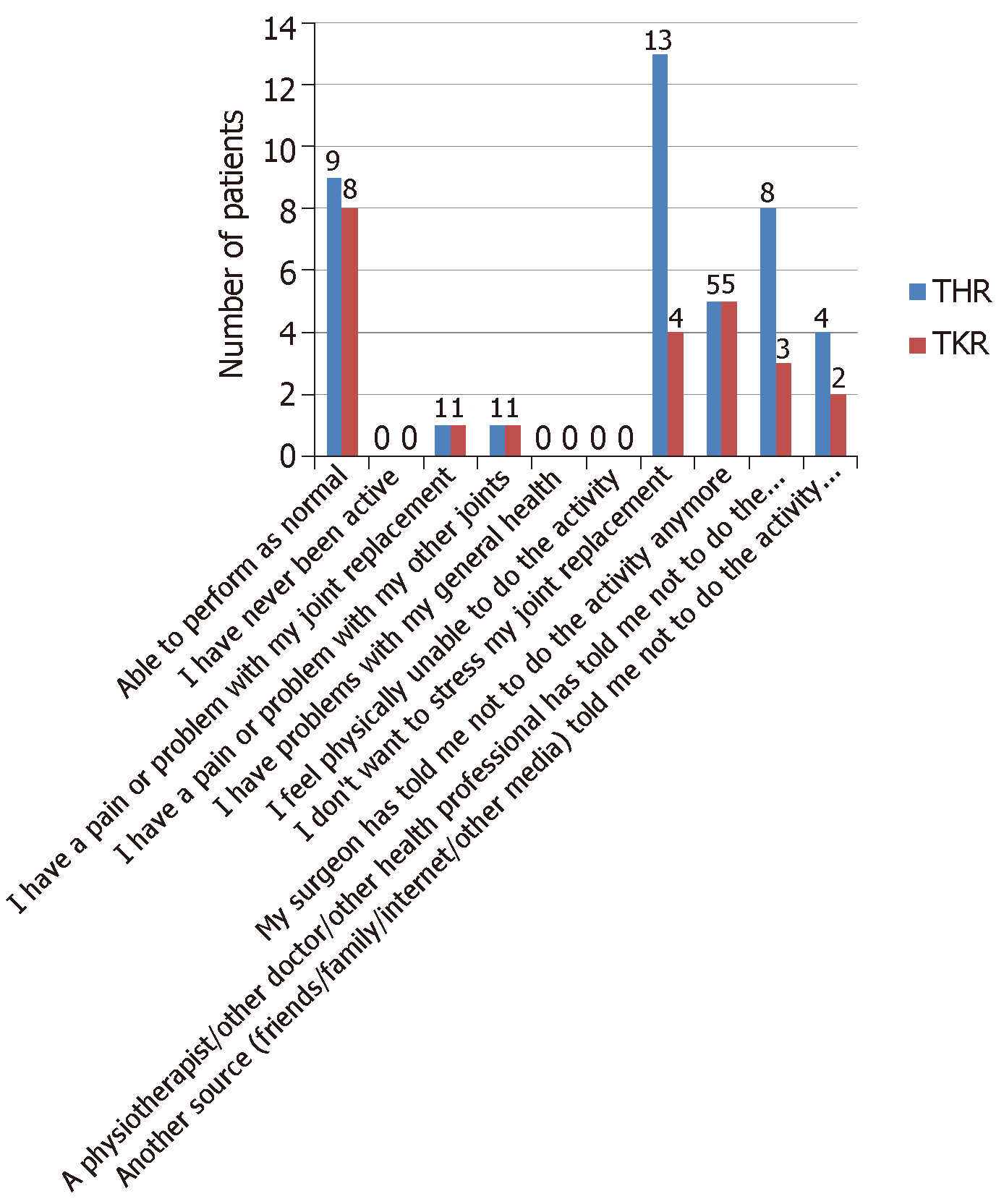
The responses to the questionnaire are displayed in Figures 1-6 and Table 3. There were no statistically significant differences in the responses based on the type of TJR for satisfaction with their TJR (P = 0.997), likelihood of recommending a TJR (P = 0.644), importance of athletic activity post-TJR (P = 0.768), frequency of performing athletic activity post-TJR (P = 0.834) and ability to perform athletic activity post-TJR (P = 0.645)
| Activity | Pre-TJR frequency (patients) | Post-TJR frequency (patients) |
| Cycling | 12 | 4 |
| Golf | 10 | 11 |
| Running | 9 | 9 |
| Walking | 8 | 6 |
| Dance | 6 | 3 |
| Tennis | 5 | 8 |
| Football | 2 | 2 |
| Gym | 2 | 9 |
| Sky diving | 2 | 0 |
| Yoga | 2 | 2 |
| Judo | 1 | 0 |
| Pilates | 1 | 3 |
| Table tennis | 1 | 0 |
| Rugby | 1 | 0 |
| Scuba diving | 1 | 1 |
| Swimming | 1 | 1 |
| Badminton | 0 | 1 |
| Triathlon | 0 | 2 |
When asked the reasons for non-participation in their chosen athletic activity, 17 patients felt they had no limitations to performing their chosen activity. The most common reasons listed for non-participation were “I don’t want to stress my joint replacement” (17 patients), “A physiotherapist/other doctor/other health professional has told me not to do the activity any more” (11 patients) and “My surgeon has told me not to do the activity anymore” (10 patients). There was no statistically significant difference in the responses based on type of TJR (P = 0.995).
The aim of this study was investigate the two-year activity levels and rate of return to athletic activity post arthroplasty and identify qualitative reasons for changes in activity participation. It has been demonstrated that all patients in our cohort returned to athletic activity. Patients are satisfied with their TJR and the ability to perform athletic activity is important. The most common sports to participate in pre-operatively are cycling, golf and running; post-operatively, these tend to be maintained, with tennis and gym also becoming popular. Patients are often able to return to their chosen activity and perform at a similar, if not better, ability in comparison to pre-operative levels. Patients are able to participate in athletic activity at least weekly, if not more frequently. The main reasons for non-participation in athletic activity were because of themselves not wanting to stress their joint replacement or under instruction from the surgeon or other doctor/health professional.
In our cohort 100% of patients returned to athletic activity. This compares favourably with studies reporting a range of rates of return to sport between 54%[24] and 98%[25]. A higher rate of return to athletic activity has been observed with later studies and may reflect a more relaxed attitude of surgeons to what their patients may be permitted to do after surgery based on a greater body of evidence.
The range of sports described by our patients is fairly typical of other studies and comparatively, our cohort maintains a higher level of performance. Only seven of the cohort had a lower UCLA score at two years in comparison to their baseline score. In these cases, there was no consistent reasoning given for a change in their activity participation. The relatively younger age of our study, combined with the absence of other joint problems can explain our cohort’s overall maintenance of high impact activities. In addition, the questionnaire may not have accurately reflected a flux in the types of activity performed: some patients may have tried to persist with their higher-impact activity for a period after their operation before trying and settling for a lower-impact activity. Similarly, there may be some patients who have started lower-impact activities after their operation but may eventually start and sustain higher-impact activities. Therefore, the post-operative UCLA scores may alter with further follow-up.
Our study had a mean post-operative UCLA score of 7.69, comparing favourably with other studies[26,27]. Some have reported higher UCLA scores: Jackson et al[28] demonstrated a mean UCLA score of 8.3 at 8.7 years post-TKR in 93 patients. Here, the main target population involved golf, which automatically gives a UCLA score of 8. Girard et al[25] demonstrated a mean UCLA score of 9.1 at 3.7 years post-HRA in 50 patients. Here, there was a lower mean patient age of 51.5 years in comparison to 55.7 in our study; it can be argued that the lower age in addition to our mixed cohort of types of arthroplasty may have influenced the mean score.
In our study, the mean two-year SF-12 physical and mental scores were higher for our TKR cohort than our THR cohort; these differences were not statistically significant for the physical portion but were significant for the mental portion of the questionnaire. Given the lack of differences between the joints in other aspects of the questionnaires, we cannot find a meaningful reason for this. The mean two-year UCLA scores were higher for THR patients compared to TKR patients (7.93 vs 7.29). This was not found to be statistically significant. All but seven patients either increased or maintained their baseline UCLA score. Amongst the cohort with a lower 2-year UCLA score, there were five THR patients and two TKR patients. When comparing the two joint cohorts, we did not see any statistically significant differences for any of the parameters in the sports activity questionnaire. These findings have replicated one of the larger recent studies in this area that did not find any differences in UCLA scores or other functional outcomes between TKR and THR patients[17].
Prior to this study, the literature did not hold many answers regarding the reasons for non-participation in activity post-surgery. Huch et al[9] reported that of the patients that reduced their athletic activity after TJR, almost half mentioned “precaution” and just over a quarter referenced pains in other joints. However, it was not clear as to the source of the basis of this precaution – whether it was from the patients themselves or as directed by their operating surgeon.
Similarly, there has been no clear consensus on the rationality of this “precaution” from patients, i.e., why do patients not want to test their new joint. It is suggested that reducing the intensity of such activities may prolong the lifespan of the replaced joint; however, no studies to date have explicitly linked high activity rates with an increased rate of implant revision and there have been no prospective studies to delineate guidelines for safe and appropriate activities for patients with a joint replacement.
Klein et al[29] took consensus from a leading body of surgeons on safe activities for patients with a joint replacement. Given some of the differences between the activities they deemed acceptable and those that are regularly performed post-TJR, this may represent a greater tolerance from surgeons towards granting their patients the ability to a greater number of activities. This may be secondary to improved confidence in surgical technique and biomaterial advances that conferred a longer implant lifespan. With an increasing number of studies on athletic activity after joint replacement available, it can be suggested that this evidence may be used to draft a more up-to-date consensus on the types of activity that patients should be able to perform.
This study has several strengths. It uses validated outcome scores allowing direct comparison with other studies. The mean outcome scores are comparable with other studies, demonstrating that our patient cohort can be considered as fairly typical of other cohorts and the conclusions on reasons for non-participation may be applied to the larger arthroplasty population with similar demographics. As patient selection has been restricted to those under the age of 60 years who have a low ASA grade and do not have multiple painful joints, this study has minimised factors known to significantly reduce participation in athletic activity post-TJR and given more insight into other factors that may reduce participation. Finally, to our knowledge, there are no other studies that have presented such detailed reasons for non-participation in athletic activity post-TJR, thus we present new information that can be used in advising surgeons, other allied healthcare professionals and their patients on capabilities in performing suitable athletic activities.
The limitations of this study are that it has a relatively small number of patients and short follow-up time. However, this study has a larger patient number and longer follow-up than other published studies. Our response rate was 80%, although this is not dissimilar to the rates of other postal questionnaire studies and we do not feel that the conclusions of the study would have been significantly altered with more responses. The study is retrospective in nature, thus the responses may be prone to re-call bias on the part of the patients. Many similar studies are also retrospective in nature; therefore we do not believe the validity of our findings is reduced. Finally, in finding the qualitative reasons for non-participation in athletic activity post-TJR, non-validated activity questionnaires were used. However, in order to gain specific reasons for changes in participation levels, a questionnaire designed to directly assess this was felt to be more suitable as the available validated questionnaires did not cover the desired information requested. In addition, several of the papers mentioned in this study have also used non-validated questionnaires in drawing their conclusions and therefore this paper is therefore comparable in drawing its own conclusions alongside these other studies.
Future research should build on our knowledge that, at present, is largely based on mid-term retrospective studies. Given the emergence of more sophisticated outcome scoring tools, it should be suggested that prospectively-designed studies with follow-up beyond 10-15 years are necessary, utilising validated outcome questionnaires alongside radiographic analysis tools, such as wear analysis software, to definitively answer questions on implant survival in cases of higher athletic activity. It is important that in addition to these outcomes, all complications associated with performing athletic activity are meticulously reported, along with suspected early revisions. Finally, an up-to-date consensus piece, led by the experts in the field of arthroplasty, could provide information to surgeons, patients and allied health professionals on suitable athletic activities post-TJR. This should be based on the most recent study evidence but should not neglect the experience of the surgeons.
In conclusion, it has been demonstrated that patients are able to return to a high level athletic activity at two years post-TJR with good functional outcome scores. Patients are highly satisfied with their joint replacement and are able to participate in a variety of activities, the most common being golf, running and gym work. Patients feel that their post-operative ability to perform their activities is better than pre-operatively. The main reason for changing their types of activity is because of wanting to protect their joint replacement, although some also cite instructions from their surgeon or other healthcare professional. We would recommend more prospective studies into this area of sports medicine and arthroplasty in addition to an up-to-date consensus piece by the key opinion leaders in this field to provide health professionals on suitable athletic activities post-TJR based on the most recent literature.
Lower limb arthroplasty is being performed in increasing numbers worldwide on progressively younger patients with few medical co-morbidities. Currently, patients who have stopped participating in athletic activity secondary to their degenerative joint disease may wish to consider returning to their chosen athletic activities. It is not presently clear as to why patients who undergo successful joint arthroplasty do not always return to athletic activity, either under any circumstance or in a different capacity to pre-operatively.
The issues surrounding returning to athletic activity following either hip or knee replacement are explored in this study, specifically the factors behind patients’ failure to return to participation in athletic activity post-operatively. Patient expectations being met are key in satisfaction following joint arthroplasty and having information on their ability to perform athletic activity post-operatively is significant information to present the patient with pre-operatively to allow them to make informed choices.
The main objective for this study was to examine the rate of return to athletic activity post lower limb arthroplasty and determine the qualitative reasons for any failure to return to athletic activity. These objectives were met as part of the study, demonstrating that questionnaire studies of this type can deliver qualitative responses as well as quantitative scores, from which meaningful conclusions can be drawn.
This was a single centre, single surgeon retrospective questionnaire study with descriptive statistical analysis performed to interpret the results; these methods are frequently employed in questionnaire studies of this nature.
This study demonstrated that patients can return to athletic activity following joint replacement to a satisfactory level. Reasons for non-participation in athletic activity include (in equal proportions) the patient not wanting to stress their joint replacement or instruction from either the lead surgeon or other doctor/health professional. Hip and knee replacements had similar outcomes and return to athletic activity rates. Problems remaining to be solved are the lack of explicit links between athletic activity and accelerated implant loosening; should such a link be established, it will affect the advice provided by health care professionals regarding the suitability of performing athletic activity post joint replacement.
The study found there are multiple factors behind a failure to return to athletic activity, including a patient wish to preserve their joint, instructions from the operating surgeon and instructions from another health care professional, including physiotherapists and general practitioners. There is no one single reason why people, with no other co-morbidities or painful joints, do not return to full athletic activity. People who are athletically active before joint replacement have a desire to return to activity post-operatively and are able to do so to a satisfactory level, with no significant differences between hip and knee replacements. The study offers original insight in that there are now qualitative reasons behind a failure to return to normal athletic activity. Future hypotheses that could be tested are that, given the vast ability of patients to perform activity to a high level post-operatively, restrictions on activity may be unnecessary and potentially relaxed given the ability of patients in this study. In addition to a prospective study investigating the conclusions further, a consensus piece could be developed to provide information to patients, surgeons and allied health professionals about suitable athletic activities post joint arthroplasty, based both on recent evidence but not neglecting the experience of the surgeons. The variety of qualitative reasons for non-participation in athletic activities represents a new area in this field. This study confirmed that patients are satisfied with their athletic capabilities following joint arthroplasty. This study may influence the decision making for patients wishing to undergo arthroplasty but also wanting to return to sport
This study demonstrated that qualitative research has a role in outcome data alongside validated outcome questionnaires. Future research should involve prospective studies with 10-15 year outcomes. The methodology should include validated outcome questionnaires for athletic activity alongside radiographic analysis to assess for implant loosening and assess implant survival in athletically active populations post arthroplasty.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Tripathy SK, Wyatt MC S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | National Joint Registry. Available from: http://www.njrcentre.org.uk/. |
| 2. | Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A:963-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Rissanen P, Aro S, Slätis P, Sintonen H, Paavolainen P. Health and quality of life before and after hip or knee arthroplasty. J Arthroplasty. 1995;10:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 109] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Elleuch MH, Guermazi M, Mezghanni M, Ghroubi S, Fki H, Mefteh S, Baklouti S, Sellami S. Knee osteoarthritis in 50 former top-level soccer players: a comparative study. Ann Readapt Med Phys. 2008;51:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Kujala UM, Kaprio J, Sarna S. Osteoarthritis of weight bearing joints of lower limbs in former élite male athletes. BMJ. 1994;308:231-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 177] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Spector TD, Harris PA, Hart DJ, Cicuttini FM, Nandra D, Etherington J, Wolman RL, Doyle DV. Risk of osteoarthritis associated with long-term weight-bearing sports: a radiologic survey of the hips and knees in female ex-athletes and population controls. Arthritis Rheum. 1996;39:988-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 249] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 823] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 8. | Cornell CN, Ranawat CS. Survivorship analysis of total hip replacements. Results in a series of active patients who were less than fifty-five years old. J Bone Joint Surg Am. 1986;68:1430-1434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Huch K, Müller KA, Stürmer T, Brenner H, Puhl W, Günther KP. Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis. 2005;64:1715-1720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 153] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 10. | Kilgus DJ, Dorey FJ, Finerman GA, Amstutz HC. Patient activity, sports participation, and impact loading on the durability of cemented total hip replacements. Clin Orthop Relat Res. 1991;269:25-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 32] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Schmidutz F, Grote S, Pietschmann M, Weber P, Mazoochian F, Fottner A, Jansson V. Sports activity after short-stem hip arthroplasty. Am J Sports Med. 2012;40:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Visuri T, Honkanen R. Total hip replacement: its influence on spontaneous recreation exercise habits. Arch Phys Med Rehabil. 1980;61:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Bradbury N, Borton D, Spoo G, Cross MJ. Participation in sports after total knee replacement. Am J Sports Med. 1998;26:530-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 120] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Chatterji U, Ashworth MJ, Lewis PL, Dobson PJ. Effect of total knee arthroplasty on recreational and sporting activity. ANZ J Surg. 2005;75:405-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 73] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Bauman S, Williams D, Petruccelli D, Elliott W, de Beer J. Physical activity after total joint replacement: a cross-sectional survey. Clin J Sport Med. 2007;17:104-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 16. | Wylde V, Blom A, Dieppe P, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90:920-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 124] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 17. | Williams DH, Greidanus NV, Masri BA, Duncan CP, Garbuz DS. Predictors of participation in sports after hip and knee arthroplasty. Clin Orthop Relat Res. 2012;470:555-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Golant A, Christoforou DC, Slover JD, Zuckerman JD. Athletic participation after hip and knee arthroplasty. Bull NYU Hosp Jt Dis. 2010;68:76-83. [PubMed] |
| 19. | Lavernia CJ, Sierra RJ, Hungerford DS, Krackow K. Activity level and wear in total knee arthroplasty: a study of autopsy retrieved specimens. J Arthroplasty. 2001;16:446-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 76] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Ollivier M, Frey S, Parratte S, Flecher X, Argenson JN. Does impact sport activity influence total hip arthroplasty durability? Clin Orthop Relat Res. 2012;470:3060-3066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 21. | Pynsent PB, Adams DJ, Disney SP. The Oxford hip and knee outcome questionnaires for arthroplasty. J Bone Joint Surg Br. 2005;87:241-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Paulsen A, Pedersen AB, Overgaard S, Roos EM. Feasibility of 4 patient-reported outcome measures in a registry setting. Acta Orthop. 2012;83:321-327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467:958-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 243] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 24. | Ritter MA, Meding JB. Total hip arthroplasty. Can the patient play sports again? Orthopedics. 1987;10:1447-1452. [PubMed] |
| 25. | Girard J, Miletic B, Deny A, Migaud H, Fouilleron N. Can patients return to high-impact physical activities after hip resurfacing? A prospective study. Int Orthop. 2013;37:1019-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 26. | Fisher N, Agarwal M, Reuben SF, Johnson DS, Turner PG. Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee. 2006;13:296-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | Sechriest VF 2nd, Kyle RF, Marek DJ, Spates JD, Saleh KJ, Kuskowski M. Activity level in young patients with primary total hip arthroplasty: a 5-year minimum follow-up. J Arthroplasty. 2007;22:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Jackson JD, Smith J, Shah JP, Wisniewski SJ, Dahm DL. Golf after total knee arthroplasty: do patients return to walking the course? Am J Sports Med. 2009;37:2201-2204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Klein GR, Levine BR, Hozack WJ, Strauss EJ, D'Antonio JA, Macaulay W, Di Cesare PE. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the Hip Society and American Association of Hip and Knee Surgeons. J Arthroplasty. 2007;22:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 111] [Article Influence: 6.2] [Reference Citation Analysis (0)] |