Published online Feb 18, 2019. doi: 10.5312/wjo.v10.i2.115
Peer-review started: November 27, 2018
First decision: December 30, 2018
Revised: January 14, 2019
Accepted: January 26, 2019
Article in press: January 26, 2019
Published online: February 18, 2019
Processing time: 83 Days and 17.8 Hours
Lisfranc injuries are rare and can be easily missed. This injury is extremely rare in children, with limited published data. Different treatment options have been described; one of the options in adults is the “mini” TightRope™ Syndesmosis Device that provides non-rigid fixation with impressive results. However, there is no reference regarding the use of this device in children.
We describe the case of an 11-year-old girl who sustained a Lisfranc injury of her right foot that was initially missed in the Accident and Emergency department of her local hospital. This case was a ligamentous/periosteal sleeve avulsion type of Lisfranc injury and a percutaneous technique using the “mini” TightRope™ syndesmosis device was used. Clinical and radiological results were excellent at final follow up.
The “mini” TightRope™ syndesmosis device is a promising method of fixation for children with certain Lisfranc injuries. This method has many advantages, including the non-rigid type of the fixation and no need for subsequent metalwork removal.
Core tip: We describe the case of an 11-year-old girl who sustained a ligamentous/periosteal sleeve avulsion type of Lisfranc injury of her right foot that was initially missed in a local Accident and Emergency department. The “mini” TightRope™ syndesmosis device, can be used safely and effectively in children with certain Lisfranc injuries, based on experience in the adult literature.
- Citation: Tzatzairis T, Firth G, Parker L. Adolescent Lisfranc injury treated with TightRopeTM: A case report and review of literature. World J Orthop 2019; 10(2): 115-122
- URL: https://www.wjgnet.com/2218-5836/full/v10/i2/115.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i2.115
Jacques Lisfranc de St. Martin (1787-1847) was a French surgeon who lived during the Napoleonic Wars. Lisfranc (surgeon and gynaecologist) was founder of a great number of surgical procedures including surgical resection in rectal carcinoma, lithotomy in women and a variety of amputations[1]. In 1815, during the Napoleonic Wars, he encountered a soldier who suffered from gangrene on his foot after having a fall from his horse. This is when his name got, for the first time, affiliated with the terms “Lisfranc joint” and “Lisfranc injury” after performing a tarsometatarsal-level amputation on this soldier. Although, in reality, Lisfranc did not describe the anatomy or the mechanism of injury, nowadays his name has come to mean a dislocation/fracture injury at the tarso-metatarsal joints[2].
Anatomically, the Lisfranc joint complex consists of ligaments and bones that connect the midfoot and forefoot (tarsometatarsal, intermetatarsal and anterior intertarsal joints). Each cuneiform bone articulates with one of the medial metatarsal whereas the lateral two metatarsals articulate with the cuboid. Apart from the trapezoid geometry of the cuneiforms and their “Roman arch” alignment, extra stability is provided by a number of ligaments. The most important is the Lisfranc ligament that connects the lateral aspect of the medial cuneiform with the base of the second metatarsal. The ligament is of vital importance to stability in this part of the foot, as there is no ligamentous connection between the first and the second metatarsal[3].
Many different classification systems have been proposed, with the first one originally been described in 1909 by Quenu and Kuss[4]. That was the first classification system describing the injuries as homolateral, isolated or divergent based on the direction of the displaced metatarsals. Many years later, Hardcastle et al[5] categorized these injuries in three different types based on displacement and incongruity. Myerson followed with modification to Hardcastle’s system (Table 1)[6]. Despite these multiple classification systems, the treatment method and the clinical outcome do not reliably correlate with any injury type[5,7,8].
| Incogruity | Subtype | Description |
| Type A: Complete | - | Dislocation of M1-M5 in the same direction (either lateral or dorsoplantar) |
| Type B: Incomplete | B1 | Medial dislocation involving only the M1 joint |
| B2 | Lateral dislocation involving any of the M2-M4 | |
| Type C: Incomplete/Complete | C1 | Divergent, incomplete dislocation involving M1 and some of the lateral metatarsals |
| C2 | Divergent, complete dislocation involving M1 and all of the lateral metatarsals |
Lisfranc injuries are rare (around 0.2% of all fractures) with reported incidence of 1:55000 per year (male:female = 4:1). It occurs more often in athletes and there is a peak at the third decade of life[9]. The rate of delayed diagnosis is up to 24%, most of these being pure ligamentous injuries[10]. In children this injury is extremely rare. There is nothing published regarding the epidemiology of this injury and the largest series in the literature includes only 52 children over a 12-year period. There are no specific guidelines regarding the treatment in children and many options have been described[11].
The TightRope™ syndesmosis device (Arthrex Inc., Naples, FL) was originally made for the injured ankle syndesmosis to provide non-rigid fixation[12]. Its “mini” version has been used to treat syndesmotic injuries, including Lisfranc injuries[13]. The TightRope™ consists of two buttons connected to each other by fiber wire. Tensioning and compression of the Lisfranc joint can be achieved without using any screws at all.
No articles regarding the use of the TightRope™ in children’s Lisfranc injury were found. This case report presents the first described case of a Lisfranc injury in a 11-year-old girl treated with the TightRope™ technique.
An 11-year-old girl was referred to our clinic by her general practitioner for bilateral patellar instability with symptoms starting 4 mo prior.
However, two weeks before, she had a fall after tripping, and sustained an injury at her right foot. On the day of injury she was admitted to the Accident and Emergency (A and E) department of a different hospital for pain limiting her ability to weight bear on that foot. Although a clinical assessment and an X-ray were performed, the injury was initially missed and due to discomfort and pain she was treated with a walking boot.
During the appointment in our clinic, her patella instability was assessed clinically and radiographically. Increased ligamentous laxity with no previous injury or patella dislocation was noted. Her family and past medical history were free. However, her parents mentioned the recent injury on her right foot and described the ongoing symptoms. On examination there was swelling throughout the midfoot with tenderness over the tarsometatarsal joint and she was still unable to bear weight. As a result, apart from the knee X-rays we requested additional X-rays of the right foot (anteroposterior, lateral and oblique view) (Figure 1). The X-ray showed “malalignment of the intermediate cuneiform with the second metatarsal, with a small bone fragment of the adjacent bone, in keeping with a Lisfranc fracture/dislocation”.
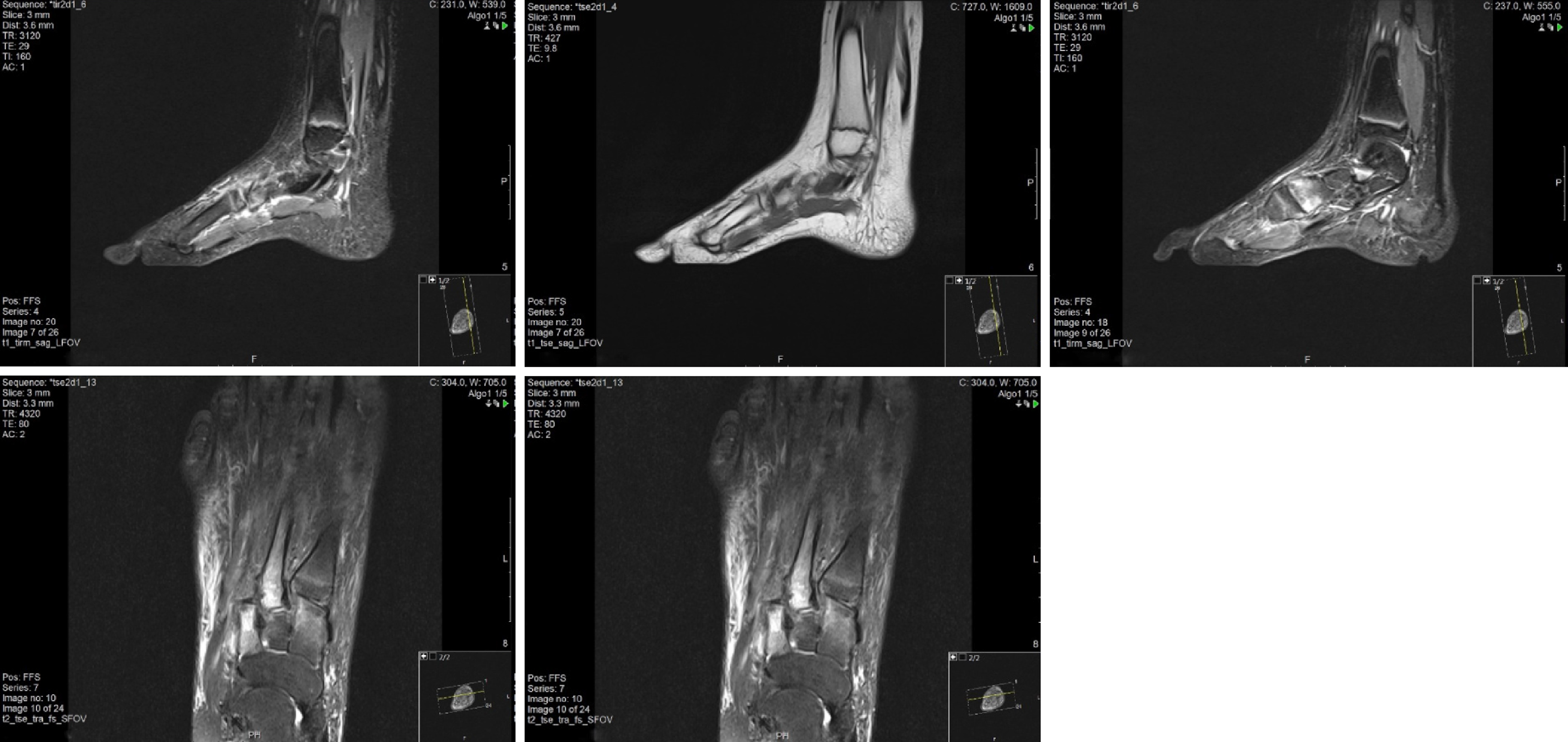
No further laboratory tests were needed but an urgent magnetic resonance imaging scan (MRI) was scheduled that same day to further assess the injury. The MRI revealed: (1) Disruption of the Lisfranc ligament with mild associated displacement of the first and second metatarsals in relation to the medial and intermediate cuneiforms; (2) High T2 marrow signal at the bases of the 1st-4th metatarsals; (3) Free fluid around the tarsal bones; and (4) Sprain of calcaneonavicular ligament (Figure 2). A final diagnosis was made, based on this MRI report of a ligamentous/periosteal avulsion type Lisfranc injury.
Based on the clinical and radiographical findings and after having a thorough discussion with the parents, the advantages (improve bone/ligament healing, improve symptoms/pain and increase movement/ROM) and the disadvantages (scar, infection, nerve/vessel injury, need for additional procedure, stiffness, anaesthetic risks) of a potential operation were discussed. She was then taken to theatre and under general anaesthetic an examination under anaesthesia revealed instability between the first and second metatarsals with concomitant dorsal subluxation and surgical treatment was decided.
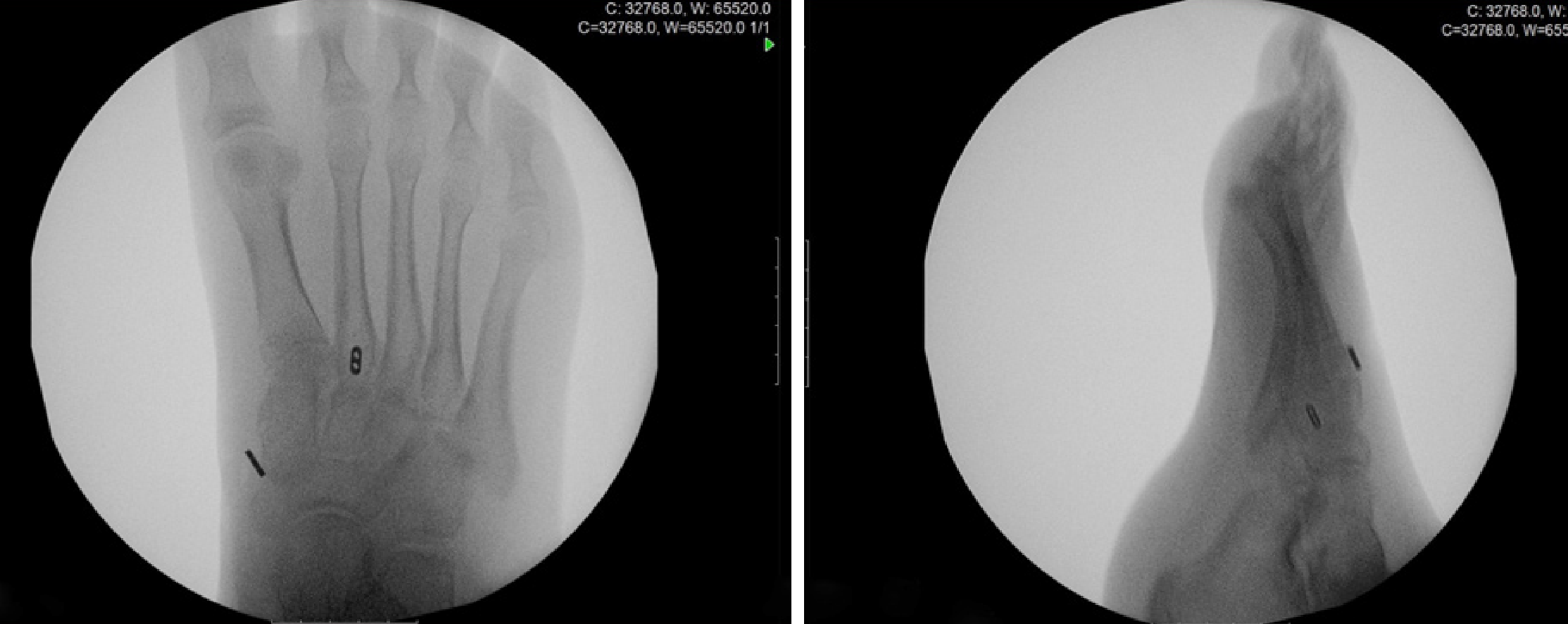
Considering the age of our patient and trying to prevent any articular damage we used the TightRope™ technique under the same anaesthetic. Under c-arm guidance the medial cuneiform and base of second metatarsal were identified. Two small incisions were made, dorsally over the lateral aspect of the 2nd metatarsal base and over the medial aspect of the medial cuneiform. Reduction of the joint was achieved with a bone reduction clamp. A drill hole (2 mm) was made from the medial cuneiform into the second metatarsal (base). The device was guided and pulled through under fluoroscopic guidance. The medial cuneiform and the lateral wall of the 2nd metatarsal base were engaged and the required compression was applied. The reduction was maintained after taking the clamp off (Figure 3). Extra care was taken to be sure that there was no soft tissue between the medial and lateral buttons and bone surface. Post-operatively, the foot was held in a moonboot for 4 wk, with partial weight-bearing with crutches for the first two weeks.
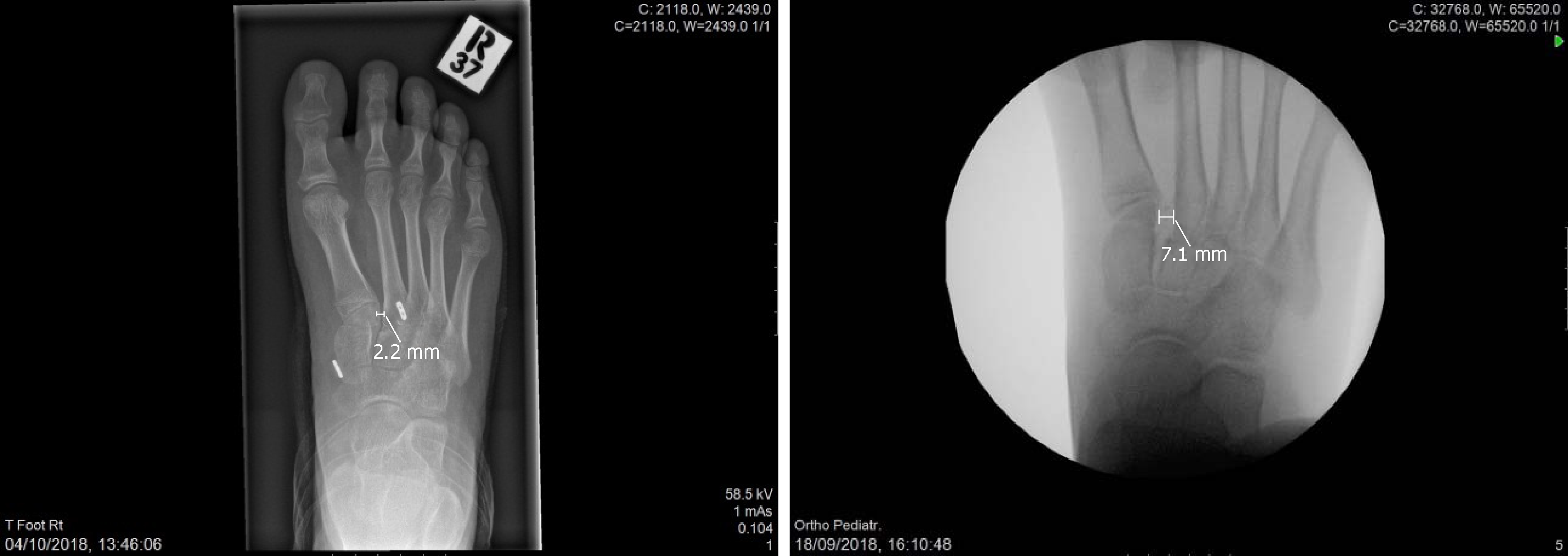
In the 3rd week the patient was reviewed in our clinic. The X-ray demonstrated excellent maintenance of reduction of the Lisfranc joint (2.2 mm distance between 1st and 2nd metatarsals post-operatively, compared to 7.1 mm pre-operatively) and patient’s symptoms had improved (Figure 4). At six weeks post-operatively, after 3 sessions of physiotherapy, the patient was able to fully weight bear without symptoms. At 12 wk post-operatively, the X-ray showed preserved reduction of the Lisfranc joint and she remained symptom-free.
Lisfranc injuries in adults are rare and known to be easily missed[10]. In the paediatric population the lack of data in the literature suggests that it is even less common or underdiagnosed or a combination of both. There are few studies of Lisfranc injuries in children and thus the treatment strategies are based on the reported results applying to adults. Depending on the mechanism of injury and its result (ligamentous and/or osseous injury), different treatment options have been described including conservative treatment, use of k-wires and/or screws and/or plates[11,14,15]. These methods seem to offer really stable fixation but disadvantages and complications have been reported including screw breakage, reduced range of motion and pain of the affected area, extensive cartilage damage, prolonged immobilization period and need for additional procedures to remove the screws[16-19]. Specifically, a cadaveric study showed that use of a 3.5 mm trans-articular screw can lead on to significant damage of the tarso-metatarsal joint[16]. Dorsal or plantar plating with locking, low-profile plates seem to provide adequate outcomes and stability[16,20]. Recently, the mini-TightRope™ technique was described as an option in the treatment of isolated Lisfranc ligament injuries with promising results. However, further studies are needed to confirm the long-term results[13,21,22].
The TightRope™ construct is made of 2 buttons (one flat 5.5 mm round stainless-steel button and a second oblong 2.6 mm × 8.0 mm stainless-steel button) connected to each other by 4 strands of #2 fibre wire. This structure creates a double pulley system between the two anchored ends which allows for better compression between the two bones. Usually, a two-incision technique is used with the first one being dorsally between the 1st and 2nd metatarsal and the second incision medially to the medial cuneiform. Extra care should be taken to protect the neurovascular bundle lying dorsally. After reducing the fracture/dislocation with a clamp and under fluoroscopic guidance, a drill is made from the medial cuneiform into the second metatarsal base over a guide wire (or retrogradely). The suture passes through this hole and is tightened making sure that the buttons remain flush over the cortex and the reduction is maintained. Further radiographs are obtained to confirm it and anatomic alignment is checked with direct inspection.
Brin et al[13] in their case series of adults highlighted the advantages of this method, in addition to the excellent clinical results that were reported. Non-rigid fixation seems to enhance healing, early weight bearing and early mobilization. Additionally, this method has a short learning curve and there is no need for a second operation to remove the metalwork[13].
In 2009, a cadaveric study concluded that the suture-button technique can provide similar results when compared to screw fixation with the advantage of avoiding an additional operation to remove the hardware prior to weight bearing[22]. To the best of our knowledge, this is the first description of a paediatric Lisfranc injury treated with TightRope™. Our case was a ligamentous/periosteal avulsion Lisfranc injury and therefore we opted to follow this method, based on the adult literature[13,22,23].
Although our hospital is a tertiary hospital this kind of injury is rarely seen. From our database search we managed to find only a few cases in the last ten years. Most of them were treated with open reduction and internal fixation (ORIF) with plate and screws. Two cases in which there was no displacement, and mild tenderness, were treated conservatively. No complications were seen, apart from post-operative stiffness in the ORIF “group” and the need for additional procedure to remove the metalwork.
Literature dealing with Lisfranc injuries in adolescents/children are extremely limited (Table 2). Veijola et al[14] in their retrospective study included six patients (range 13 to 16 years) treated with ORIF. In all but one case, they achieved anatomical reduction, but most patients claimed discomfort in the injured foot. Hill et al[11] reviewed 56 children treated for bony or ligamentous Lisfranc injuries with ORIF or non-operative management. These authors didn’t find any correlation between age and type of injury but concluded that a large percentage of patients, even if they had open physes, required surgery. An important limitation was the lack of data on outcomes and follow-up[11]. A case of a 10-year-old girl who sustained a Lisfranc fracture-dislocation in 2013 was presented by Lesko et al[24] last year. Injury was fixed with ORIF but now (5 years post-operatively) she has developed functional pain and radiographic evidence of degenerative arthritis. All the other articles found in the literature did not deal with treatment and outcome but discussed the mechanism of injury which was not the focus of this report[15,25,26].
| Article | Type of study | No. of patients | Type of fixation | Result |
| Lisfranc Injury in Adolescents (Veijola et al[14], 2013) | Retrospective | 6 | ORIF | Good anatomical reduction, post-operative discomfort |
| Lisfranc injuries in children and adolescents (Hill et al[11], 2017) | Retrospective | 56 | ORIF (19); Conservatively (37) | Good post-operative results with rare complications (physeal arrest, broken implant) |
| Midfoot Degenerative Arthritis and Partial Fusion After Pediatric Lisfranc Fracture-Dislocation (Lesko et al[24], 2018) | Case report | 1 | ORIF | Functional pain and radiographic evidence of degenerative arthritis: 5-yr post-operatively |
| Pediatric Lisfranc injury: “bunk bed” fracture (Johnson[15], 1981) | Retrospective | 16 | - | Pathogenesis of Lisfranc injury |
| Plantar-flexion tarsometatarsal joint injuries in children (Buoncristiani et al[25], 2001) | Retrospective | 8 | Conservative | Early degenerative changes can occur and may be responsible for chronic pain and activity limitation |
| Tarso-metatarsal joint injuries in children (Wiley[26], 1981) | - | - | - | Pathogenesis of Lisfranc injury |
This minimally invasive technique has many advantages: (1) reduced duration of the procedure; (2) non-rigid type of the fixation that allows early mobilization; (3) prevention of cartilage damage; and (4) no need for metalwork removal. The main limitation of this study is that it is just a case report, but we hope that it will open the way for further research using this technique for ligamentous Lisfranc injuries in children.
The TightRope™ syndesmosis device technique in children with ligamentous Lisfranc injuries is efficacious as it combines the advantages of a percutaneous technique with a less rigid type of fixation and good short-term results. Further research is needed to confirm its routine use in children.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Hooper GJ, Malik H, Serban ED, von Engelhardt LV S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | M. Lisfranc on Diseased Joints. Med Chir Rev. 1826;5:296-297. [PubMed] |
| 2. | Cassebaum WH. Lisfranc fracture-dislocations. Clin Orthop Relat Res. 1963;30:116-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 62] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | de Palma L, Santucci A, Sabetta SP, Rapali S. Anatomy of the Lisfranc joint complex. Foot Ankle Int. 1997;18:356-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 114] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 4. | Quenu E, Küss G. Etude sur les luxations du métatarse (luxations metatarsotarsiennes) du diastasis entre le 1er et le 2e métatarsien. Rev Chir. 1909;39:1093-1134. |
| 5. | Hardcastle PH, Reschauer R, Kutscha-Lissberg E, Schoffmann W. Injuries to the tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg Br. 1982;64:349-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 270] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Myerson MS. The diagnosis and treatment of injury to the tarsometatarsal joint complex. J Bone Joint Surg Br. 1999;81:756-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Myerson MS, Fisher RT, Burgess AR, Kenzora JE. Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot Ankle. 1986;6:225-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 476] [Cited by in RCA: 400] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 8. | Shariff S, Clark C, Dega R. Lisfranc injury classifications. The Internet Journal of Orthopedic Surgery. 2008;11(1). |
| 10. | Sherief TI, Mucci B, Greiss M. Lisfranc injury: how frequently does it get missed? And how can we improve? Injury. 2007;38:856-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Hill JF, Heyworth BE, Lierhaus A, Kocher MS, Mahan ST. Lisfranc injuries in children and adolescents. J Pediatr Orthop B. 2017;26:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Cottom JM, Hyer CF, Philbin TM, Berlet GC. Treatment of syndesmotic disruptions with the Arthrex Tightrope: a report of 25 cases. Foot Ankle Int. 2008;29:773-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 13. | Brin YS, Nyska M, Kish B. Lisfranc injury repair with the TightRope device: a short-term case series. Foot Ankle Int. 2010;31:624-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Veijola K, Laine HJ, Pajulo O. Lisfranc injury in adolescents. Eur J Pediatr Surg. 2013;23:297-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Johnson GF. Pediatric Lisfranc injury: "bunk bed" fracture. AJR Am J Roentgenol. 1981;137:1041-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Alberta FG, Aronow MS, Barrero M, Diaz-Doran V, Sullivan RJ, Adams DJ. Ligamentous Lisfranc joint injuries: a biomechanical comparison of dorsal plate and transarticular screw fixation. Foot Ankle Int. 2005;26:462-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 137] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Ando A, Hagiwara Y, Tsuchiya M, Onoda Y, Suda H, Chimoto E, Itoi E. Increased expression of metalloproteinase-8 and -13 on articular cartilage in a rat immobilized knee model. Tohoku J Exp Med. 2009;217:271-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Kuo RS, Tejwani NC, Digiovanni CW, Holt SK, Benirschke SK, Hansen ST, Sangeorzan BJ. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am. 2000;82-A:1609-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 278] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 19. | Rammelt S, Schneiders W, Schikore H, Holch M, Heineck J, Zwipp H. Primary open reduction and fixation compared with delayed corrective arthrodesis in the treatment of tarsometatarsal (Lisfranc) fracture dislocation. J Bone Joint Surg Br. 2008;90:1499-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 20. | Marks RM, Parks BG, Schon LC. Midfoot fusion technique for neuroarthropathic feet: biomechanical analysis and rationale. Foot Ankle Int. 1998;19:507-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 100] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 21. | Baravarian B, Geffen D. Lisfranc tightrope. Foot Ankle Spec. 2009;2:249-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Panchbhavi VK, Vallurupalli S, Yang J, Andersen CR. Screw fixation compared with suture-button fixation of isolated Lisfranc ligament injuries. J Bone Joint Surg Am. 2009;91:1143-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 23. | Regauer M, Baumbach S, Brumann M, Mutschler W, Polzer H. [Lisfranc dislocation fracture: Dynamic examination under anesthesia and minimally invasive stabilization with mini-TightRope®]. Unfallchirurg. 2015;118:727-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Lesko G, Altman K, Hogue G. Midfoot Degenerative Arthritis and Partial Fusion After Pediatric Lisfranc Fracture-Dislocation. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Buoncristiani AM, Manos RE, Mills WJ. Plantar-flexion tarsometatarsal joint injuries in children. J Pediatr Orthop. 2001;21:324-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Wiley JJ. Tarso-metatarsal joint injuries in children. J Pediatr Orthop. 1981;1:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 0.9] [Reference Citation Analysis (0)] |