Copyright
©The Author(s) 2024.
World J Orthop. Aug 18, 2024; 15(8): 683-695
Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.683
Published online Aug 18, 2024. doi: 10.5312/wjo.v15.i8.683
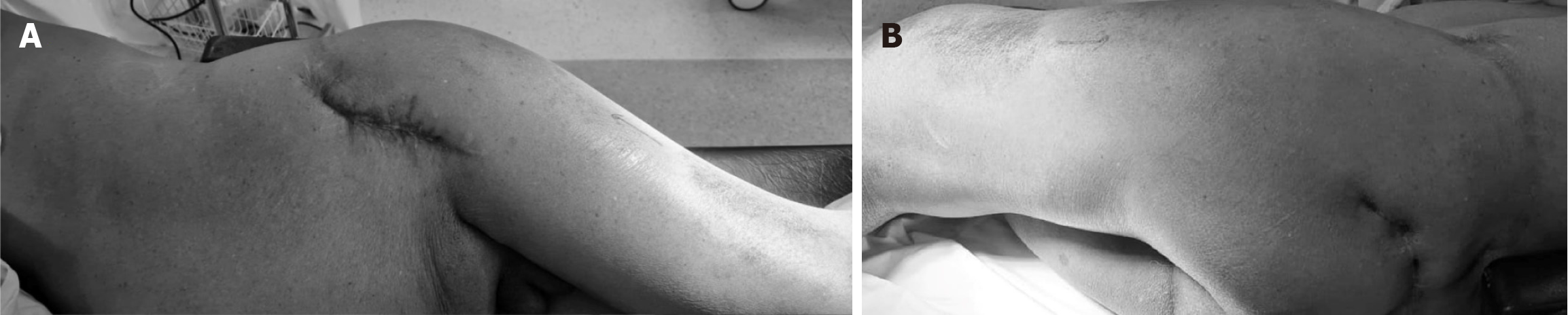
Figure 1 Skin scarring is not uncommon at total hip arthroplasty for childhood disorder sequelae.
Patient in lateral position. A: Anterior aspect surgical puckered scar extending from the anterior superior iliac spine suggestive of scarring of the anterior soft tissues; B: Posterior scar with puckering posterior to the greater trochanter.
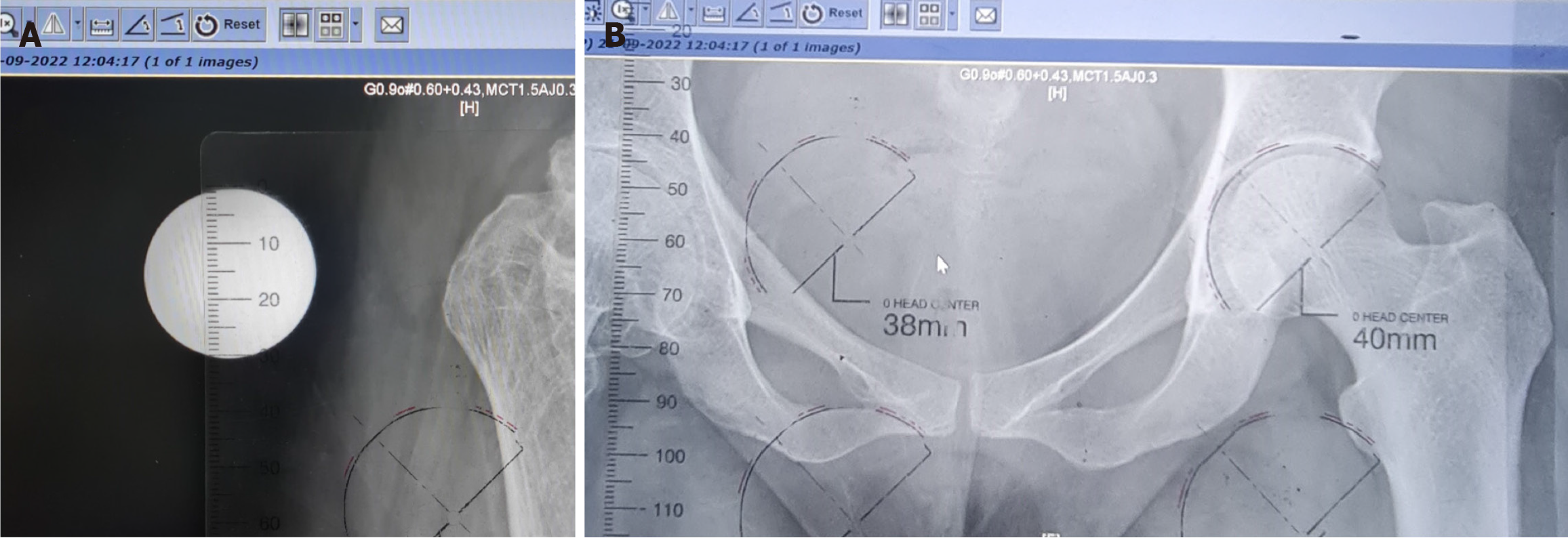
Figure 2 Templating with digital X-rays using a computer.
A: 3-cm diameter metal ball is strapped to the thigh for X-ray. The scale on the template is matched to 3 cm by using the zooming feature (zoom in or zoom out); B: Match the size of the acetabulum to the correct size. Care is taken to assess the optimal size with respect to the teardrop, lateral edge, and acetabular floor. Arrows indicating the ball size matched and the template matching acetabular component size.
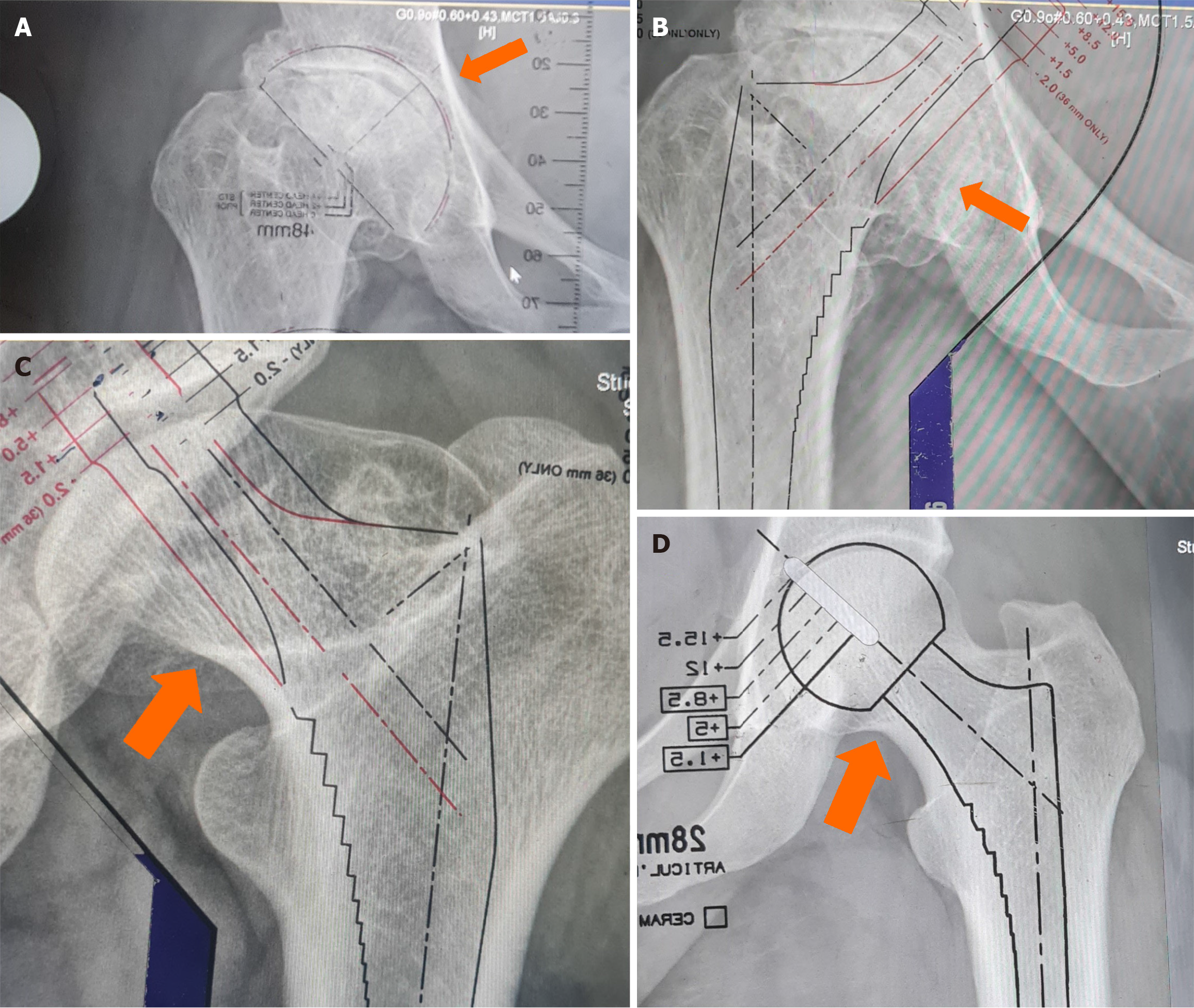
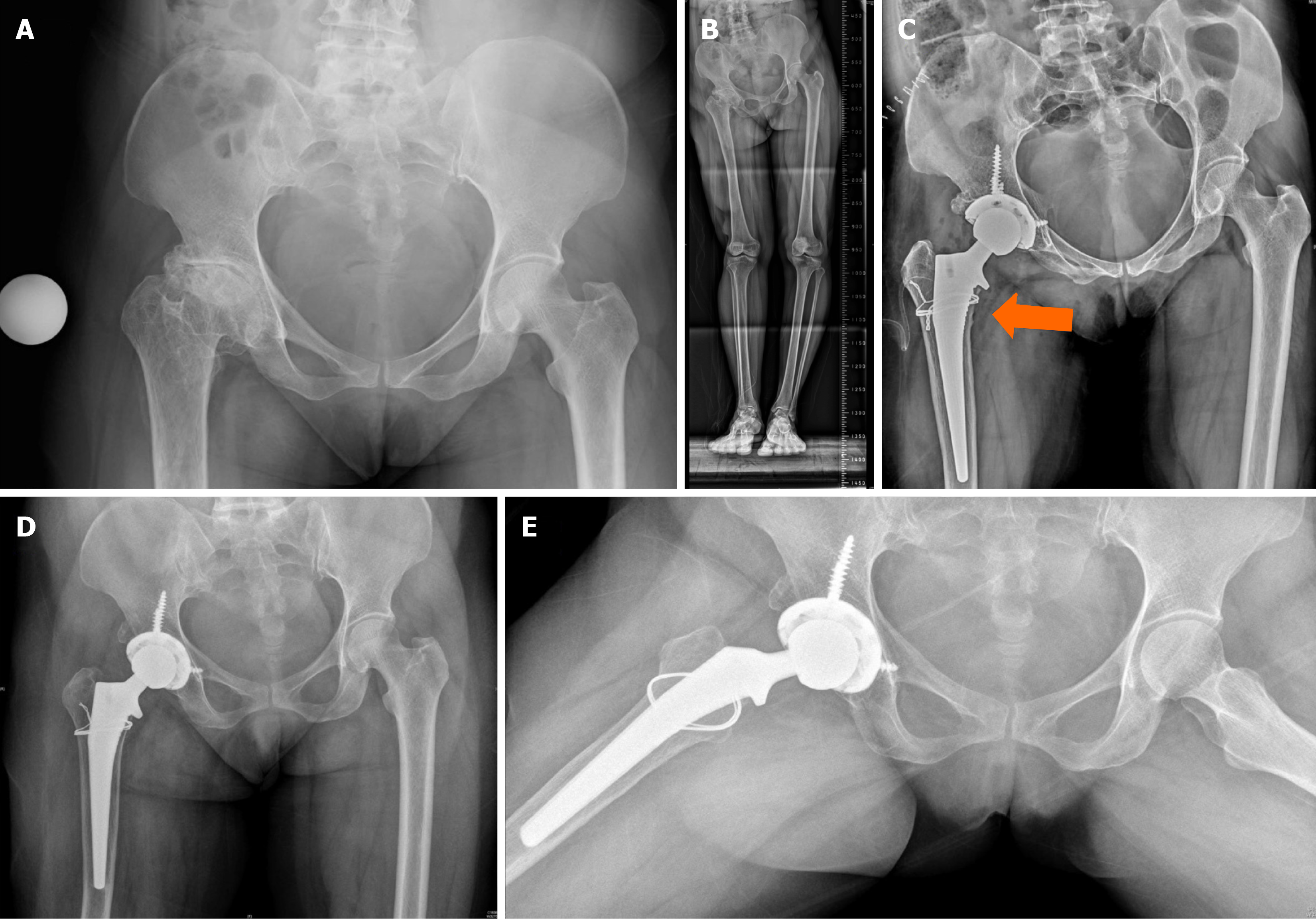
Figure 3 Routine preoperative templating is done for all cases for total hip arthroplasty in our unit using the described method.
A: Affected side size shows larger size to due to distortion – indicated by the arrow. Restoration of hip centre was done with the same size; B–D: Templating the femur shows low neck cut, normal offset available is oversized in 3 hips as indicated by the arrows. Soft tissue release combined with use of a shorter offset/neck would be required tore produce offset on the normal side which is checked intraoperatively. Primary hip implants are available with short, normal and high offset options.
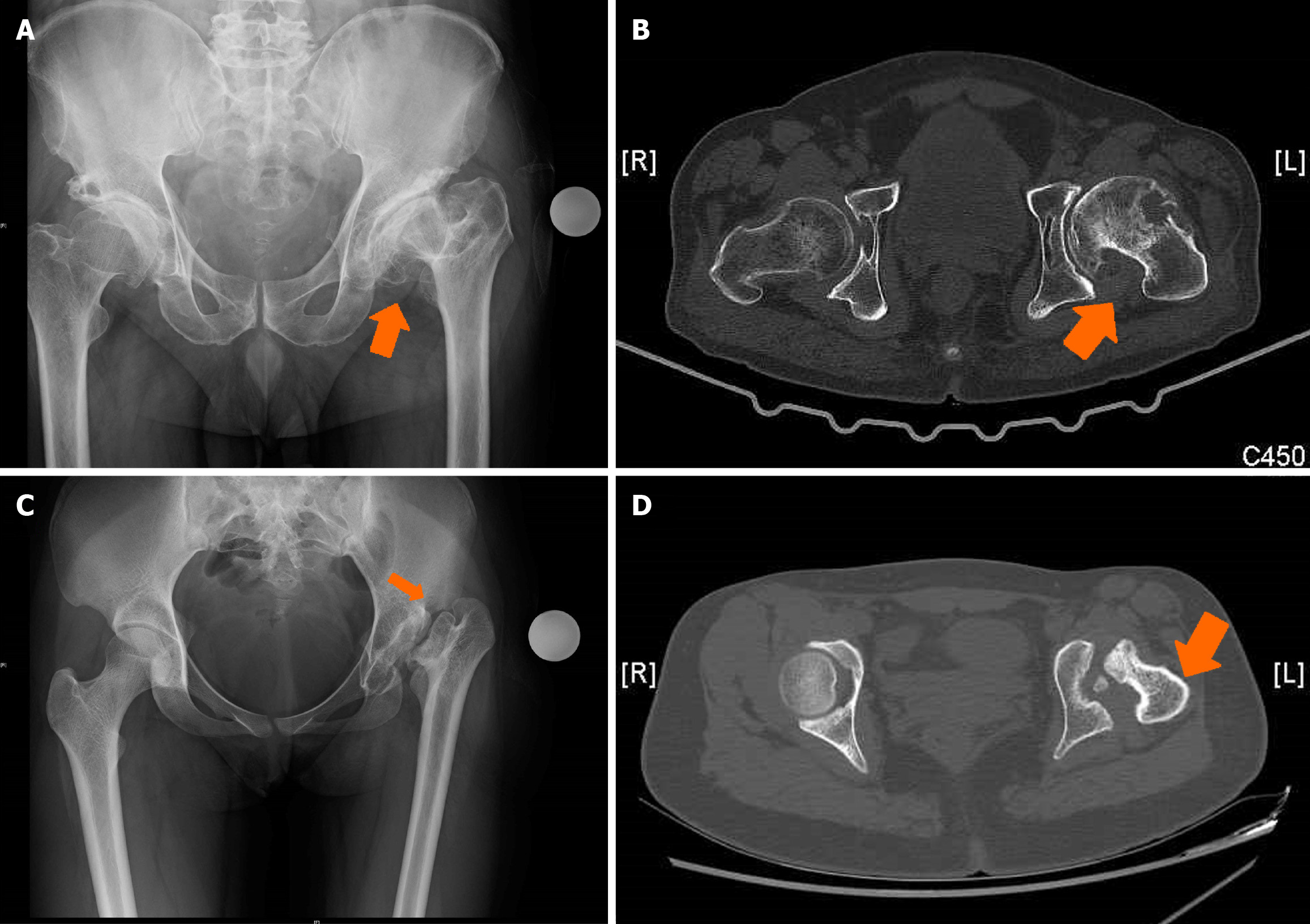
Figure 4 Anatomical abnormalities in the proximal femur include anteversion changes.
A and B: X-ray of both hips anteroposterior (AP) showing dysplastic hip left with computed tomography (CT) assessment showing increased anteversion and deformed head and acetabulum; C and D: X-ray of both hips AP showing postseptic sequelae in left hip at total hip arthroplasty with computed tomography (CT) images showing large medial osteophyte, head malformation and increased femoral anteversion. Arrows indicating the changes in the X-ray and CT images. Preoperative evaluation helps in identification and adjustment of intraoperative femoral version.
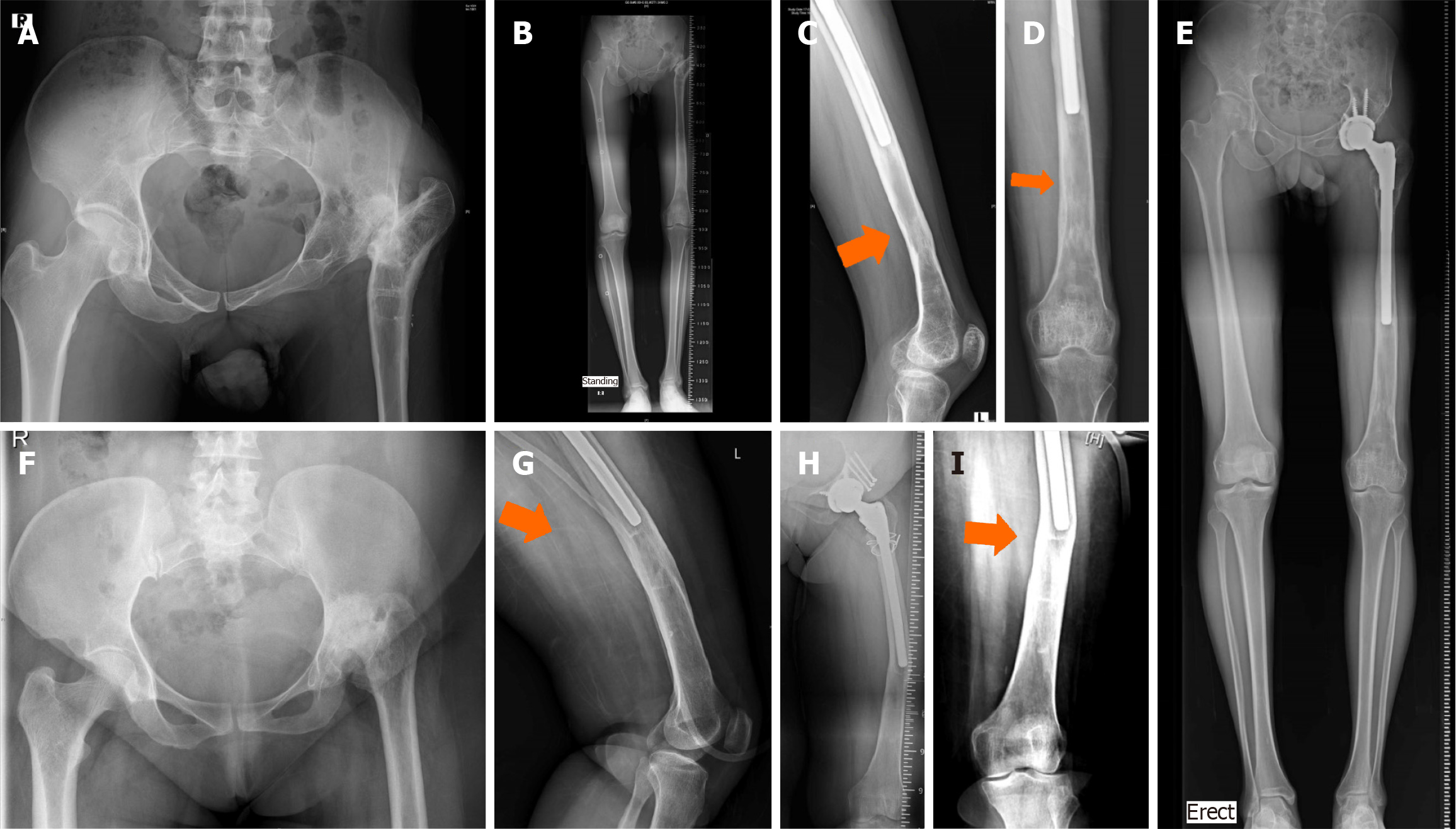
Figure 5 Prior femoral procedures produce distortion in the proximal and/or distal femur.
A–E: Prior proximal femur valgus osteotomy and distal femur lengthening needed correction of the proximal angulation, shortening and judicious reaming distally to obtain optimum fixation length. Arrows indicating area of femur canal distortion; F–I: Childhood hip arthritis with significant shortening required extensive release and shortening osteotomy. Distal femoral canal changes with 15 angulation due to prior lengthening had to be managed with careful femur canal preparation for a long modular implant. Orange arrows show the canal distortion. Reaming was done gradually as significant resistance was encountered at that segment. Intraoperative imaging is important in these situations.
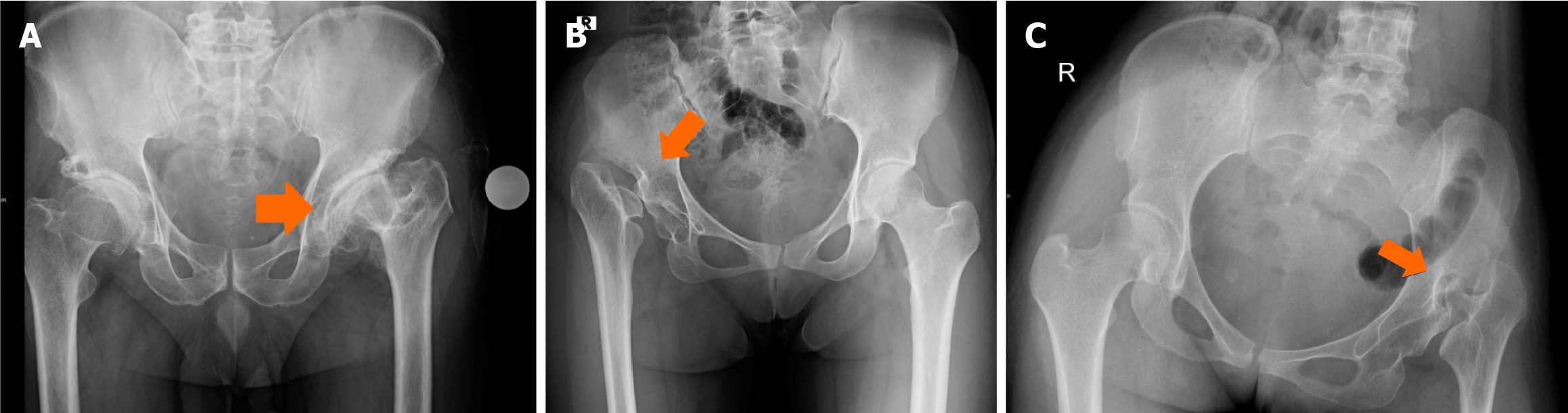
Figure 6 Supratrochanteric shortening: the femoral head is below the level of the greater trochanter, and the lesser trochanter is above the level of the teardrop.
A: The left hip; B: Right hip; C: Left hip. The femur head is significantly distorted. Restoration of hip centre would often require adequate soft tissue release and use of primary femoral implants.
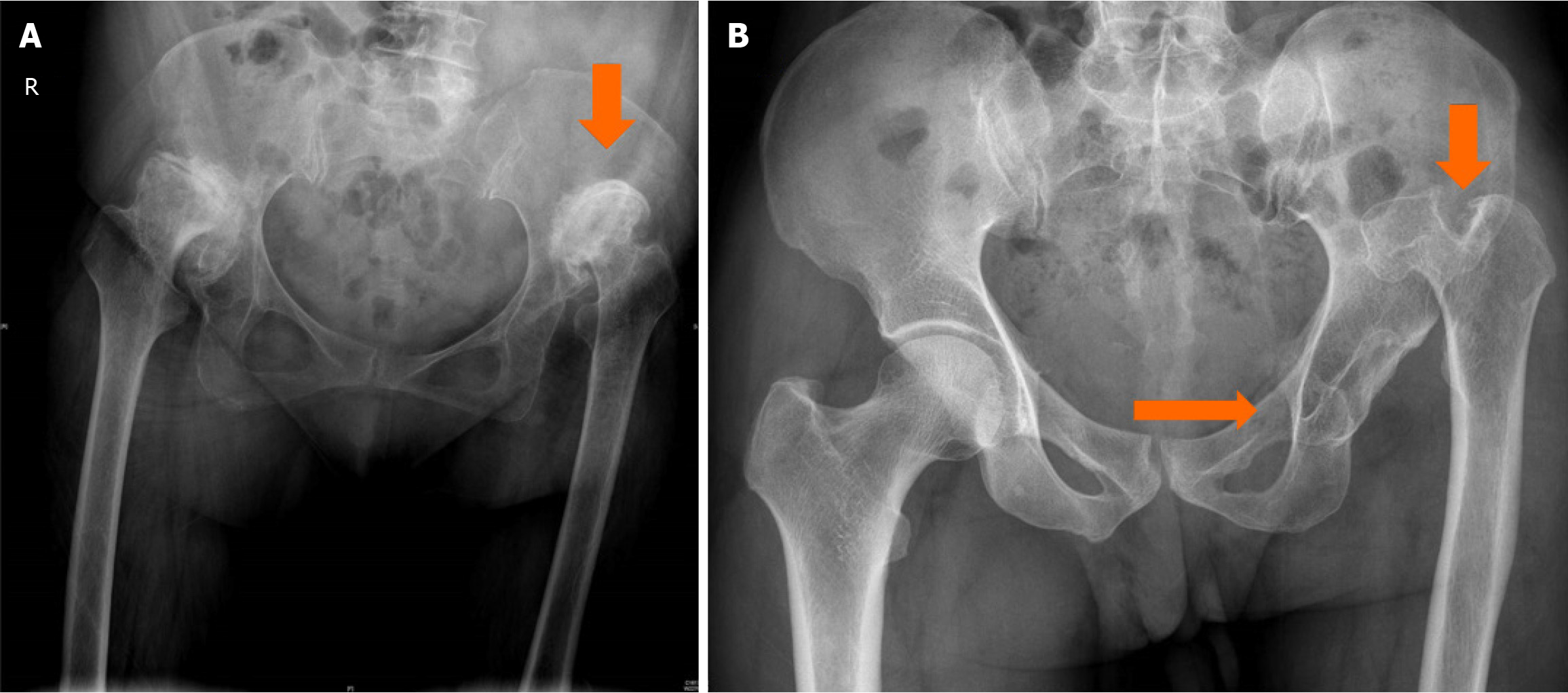
Figure 7 Infratrochanteric shortening: The relationship between the head of the femur and greater trochanter is maintained while the lesser trochanter is above the level of the teardrop (indicated by the arrows).
A: Both hips; B: Left hip. Restoration of the hip centre would require identification of the true acetabulum, acetabular centre restoration, and sub trochanteric shortening would almost certainly be required.
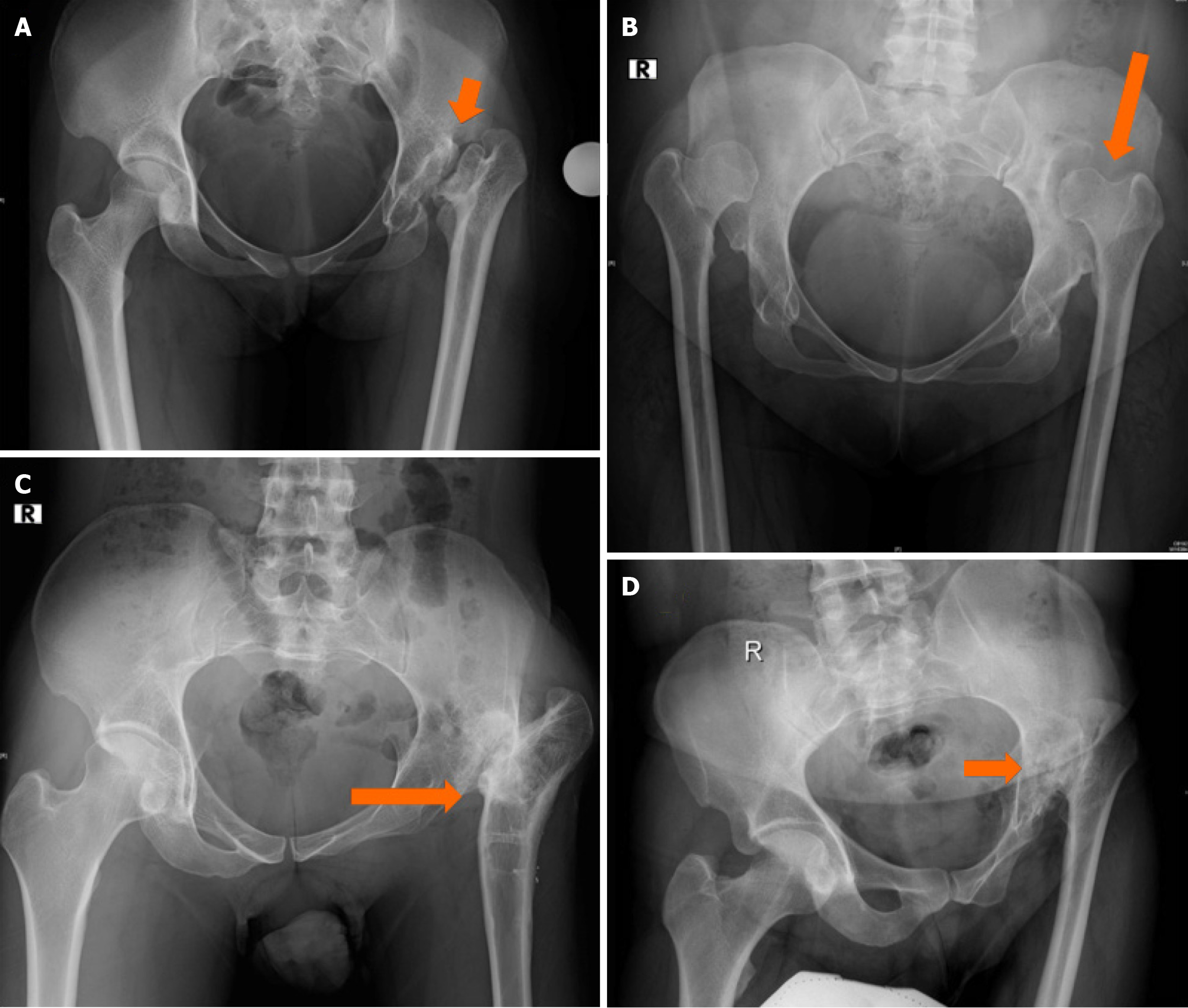
Figure 8 Combined supra- and infratrochanteric shortening.
A: Left hip shortening; B: Bilateral shortening due to neglected hip dysplasia; C: Postoperative proximal femur deformity and shortening; D: Postseptic sequelae in the left hip with shortening of both supra- and infratrochanteric shortening – indicated by the arrows in hips with childhood arthritis sequelae.
Figure 9 Perthes sequelae hip at total hip arthroplasty with thin femoral cortices.
A and B: Femur preparation done with care, however developed crack on trial reduction; C: Stability was achieved with wiring as indicated with the arrow; D and E: Follow-up with restoration of hip centre and well-fixed femur.
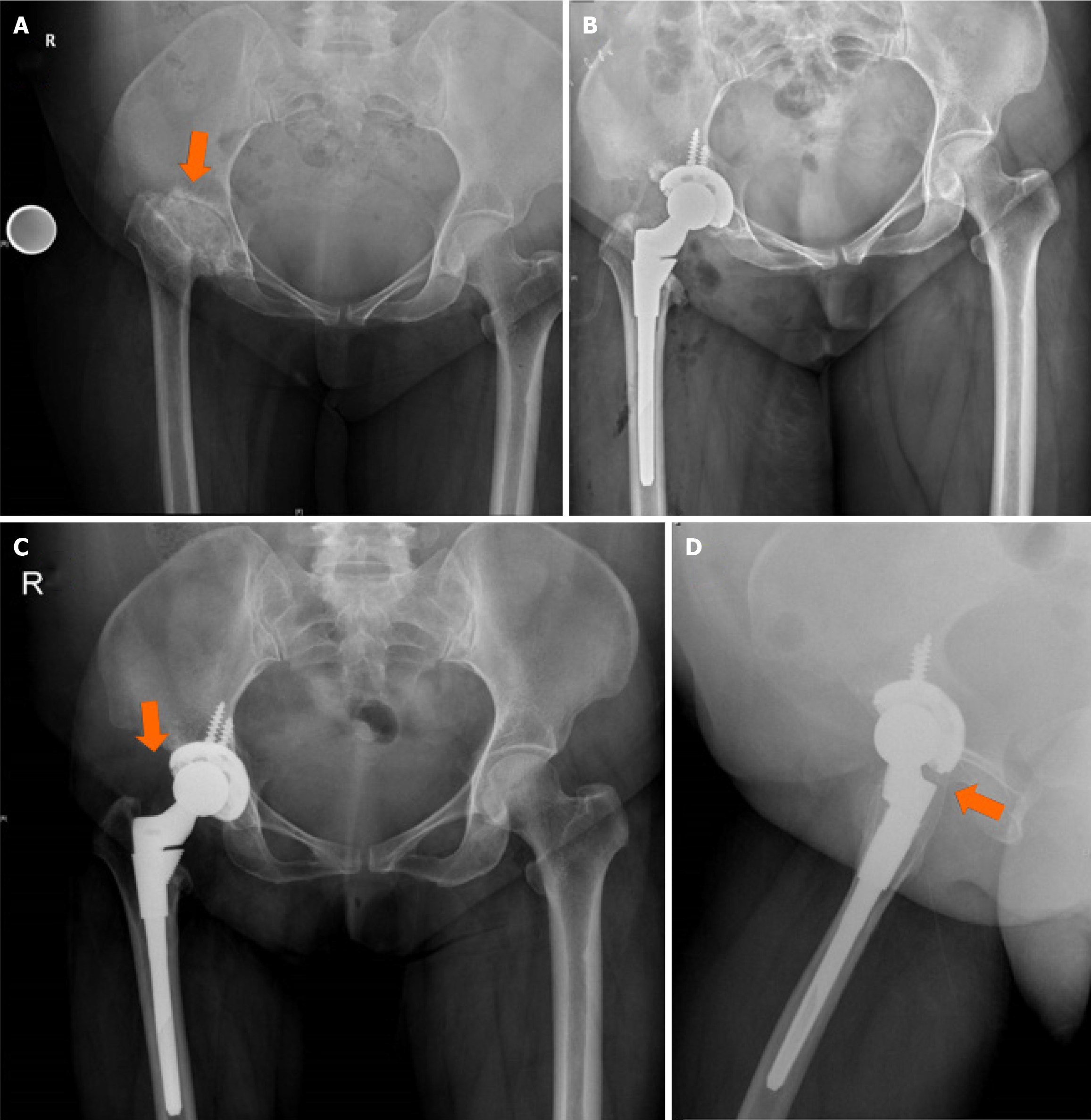
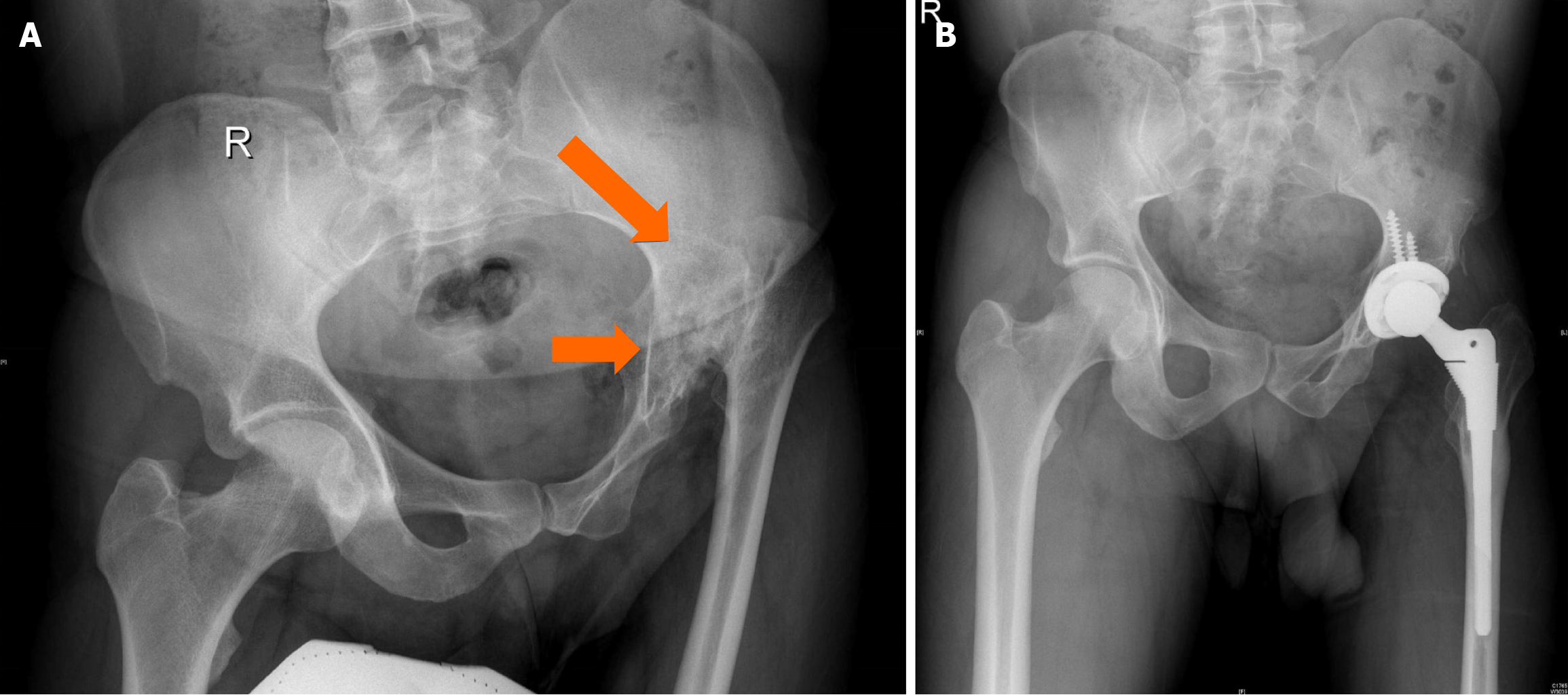
Figure 10 X-ray both hips in a young adult with history of right lower limb shortening and limp since childhood.
A: Dysplastic hip sequelae with supratrochanteric shortening and proximal migration; B: Modular stem for neck length and version adjustment; C and D: Follow-up shows restoration of hip centre, offset and length. Arrows show the distortion, offset and the femoral version.
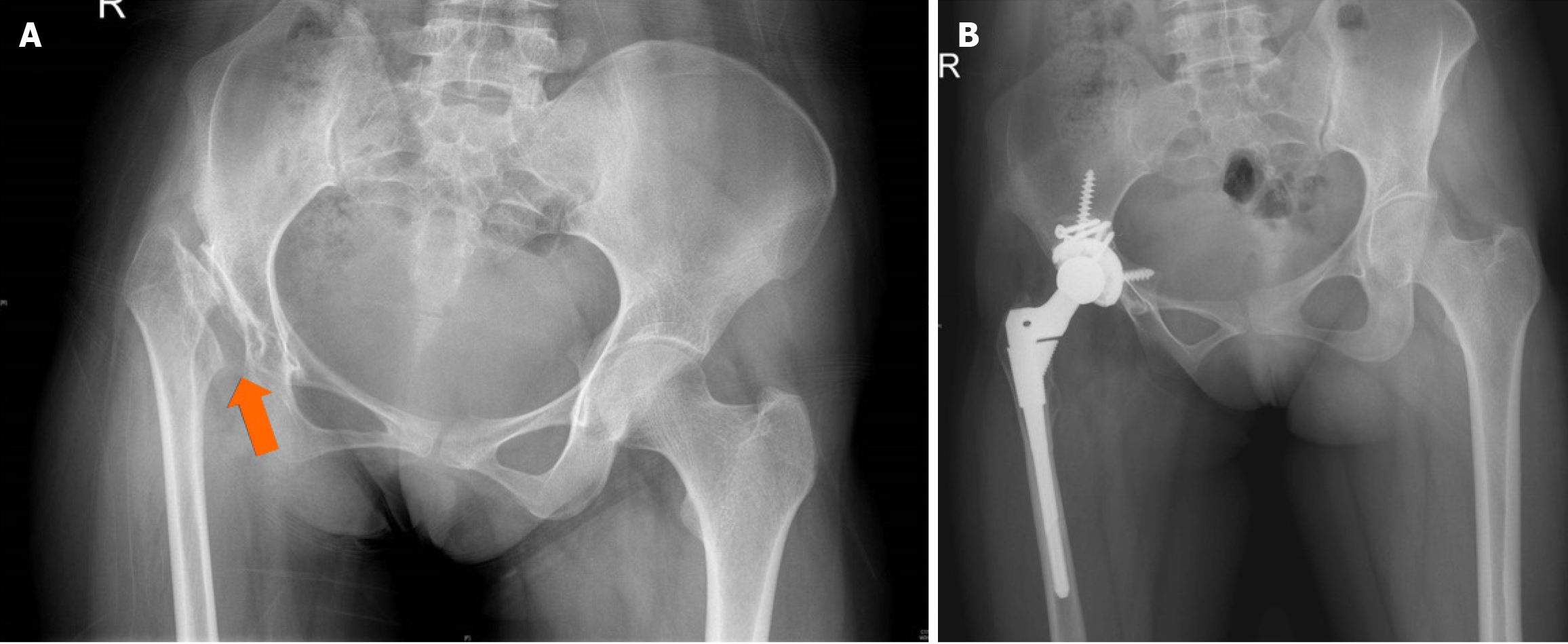
Figure 11 Woman aged 20 years with childhood arthritis of the right hip.
A: Infratrochanteric shortening with small size acetabulum (arrow), femur, and narrow canal. Shallow acetabulum with posterosuperior defect was seen on computed tomography assessment; B: Follow up – acetabular centre restoration with small cup, bone graft from head remnant, shortening osteotomy, modular femur with restoration of hip centre and offset.
Figure 12 Perthes disease sequelae with flattening of the acetabulum, head deformation (arrow) and shortening.
Acetabular preparation, soft tissue release and appropriate femur sizing are required to restore offset and limb length.
Figure 13 Slipped capital epiphysis sequelae in a 53-year-old man.
A: Proximal femur osteotomy done earlier with distortion of the proximal femur anatomy (arrows); B and C: Femur canal entry identification and preparation needs particular attention to achieve stable fixation and reconstruction.
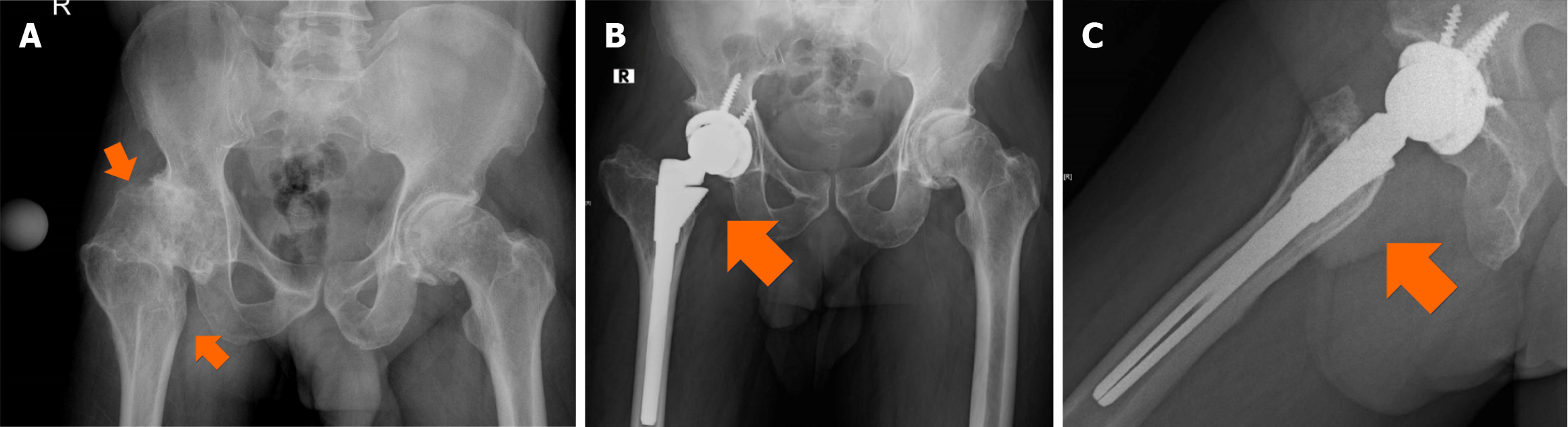
Figure 14 Man aged 39 years with left hip childhood arthritis sequelae.
A: Postseptic sequelae with small femur, pelvis and soft tissue changes. The acetabulum and proximal femur (arrows) need proper identification to restore the anatomical centre; B: Follow-up. Identifying the true acetabulum, small acetabular size, soft tissue release, femoral shortening, modular femur, hip centre restoration, neck length and offset requirements are challenging in these cases. This can be achieved with proper preoperative planning and intraoperative assessment.
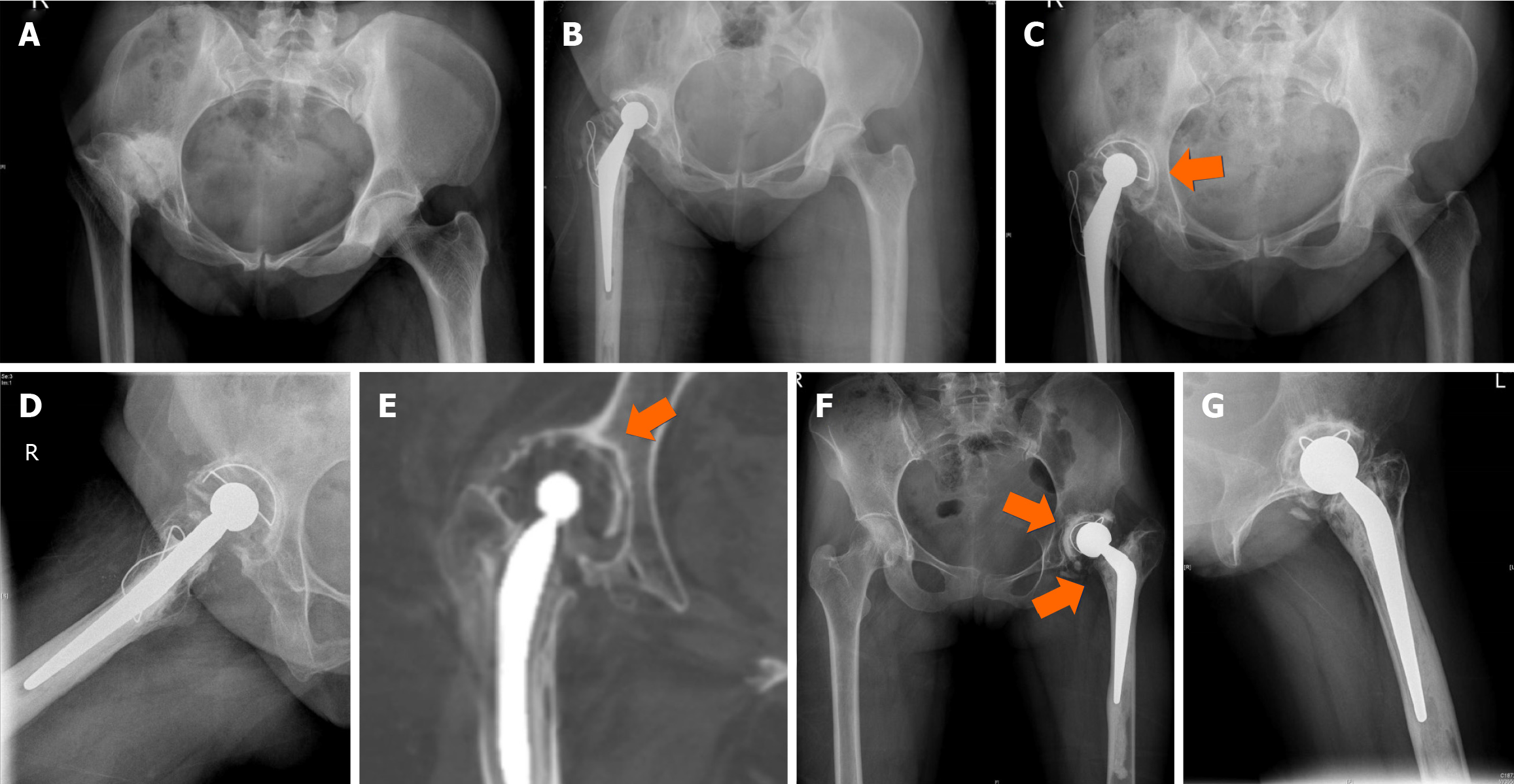
Figure 15 High hip centre/inadequate restoration of hip centre at total hip arthroplasty.
A and B: Proximal and lateral migrated dysplastic hip after total hip arthroplasty (THA) with high hip centre. Greater trochanter fracture at reduction stabilised with wiring; C–E: 15-year follow-up with symptomatic acetabular loosening confirmed with computed tomography assessment. This required acetabular revision with hip centre restoration with augments; F and G: Dysplastic hip with cemented THA at 6 years follow-up –proximal and lateralised acetabulum, with reduced neck length and offset femur. Shortening, limp and pain required revision in this hip with acetabular loosening(arrows). Restoration of hip centre, offset was done with true acetabular floor identification, small component, soft tissue release and femur revision.
- Citation: Oommen AT. Total hip arthroplasty for sequelae of childhood hip disorders: Current review of management to achieve hip centre restoration. World J Orthop 2024; 15(8): 683-695
- URL: https://www.wjgnet.com/2218-5836/full/v15/i8/683.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i8.683