Copyright
©The Author(s) 2024.
World J Orthop. Nov 18, 2024; 15(11): 1056-1074
Published online Nov 18, 2024. doi: 10.5312/wjo.v15.i11.1056
Published online Nov 18, 2024. doi: 10.5312/wjo.v15.i11.1056
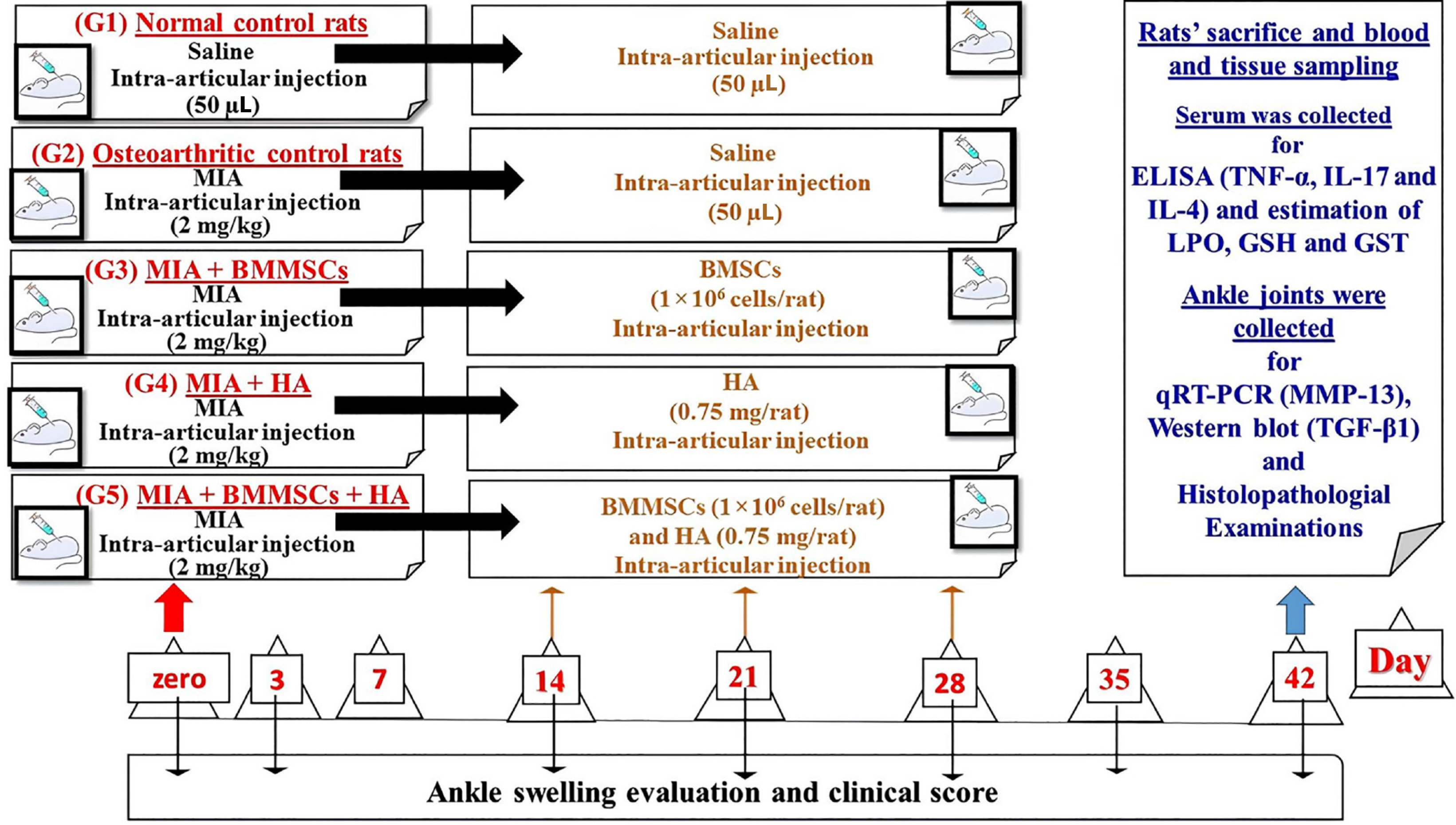
Figure 1 Design, setting of the study and animal grouping.
BMMSCs: Bone marrow mesenchymal stem cells; GSH: Glutathione; GST: Glutathione S-transferase; HA: Hyaluronic acid; IL-17: Interleukin-17; LPO: Lipid peroxidation; MIA: Monosodium iodate; MMP-13: Matrix metalloproteinase 13; ROS: Reactive oxygen species; TGF-β1: Transforming growth factor beta 1; TNF-α: Tumor necrosis factor alpha.
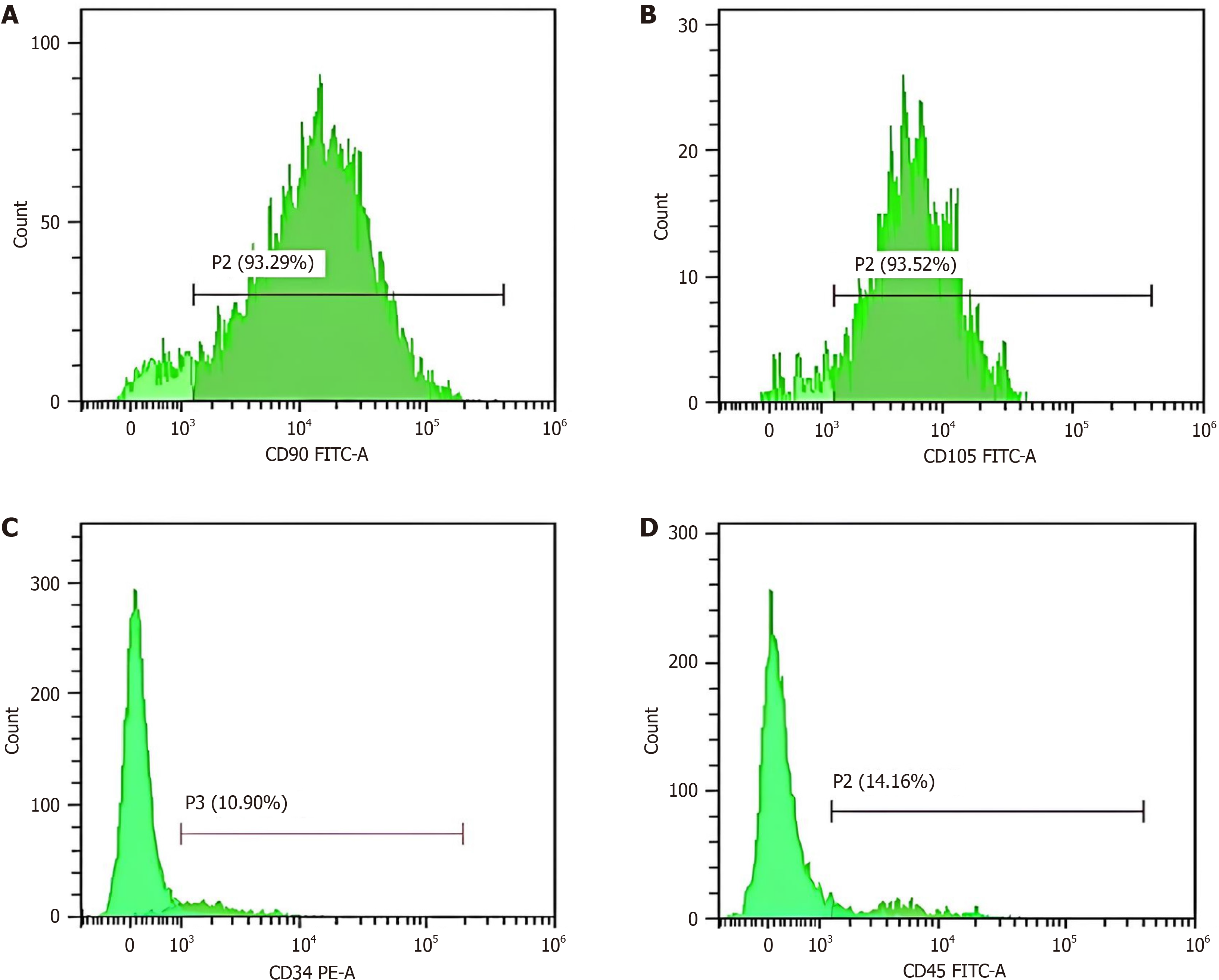
Figure 2 Immunophenotyping of bone marrow mesenchymal stem cells by detection of surface markers including cluster of differ
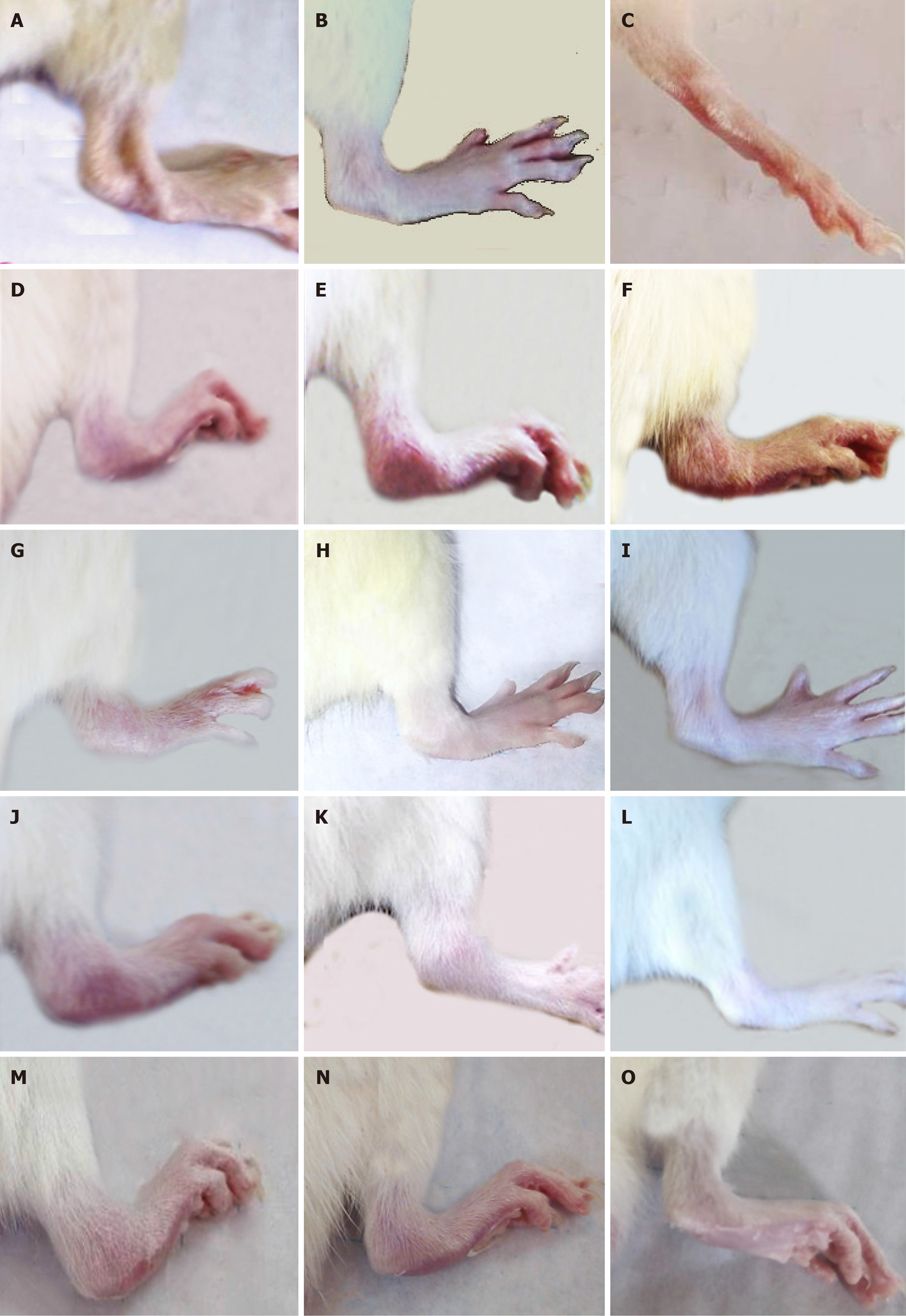
Figure 3 Right hind leg pictures of the tested groups.
A-C: Right hind legs normal rats at the 4th week (A), 5th week (B), and 6th week (C); D-F: Osteoar
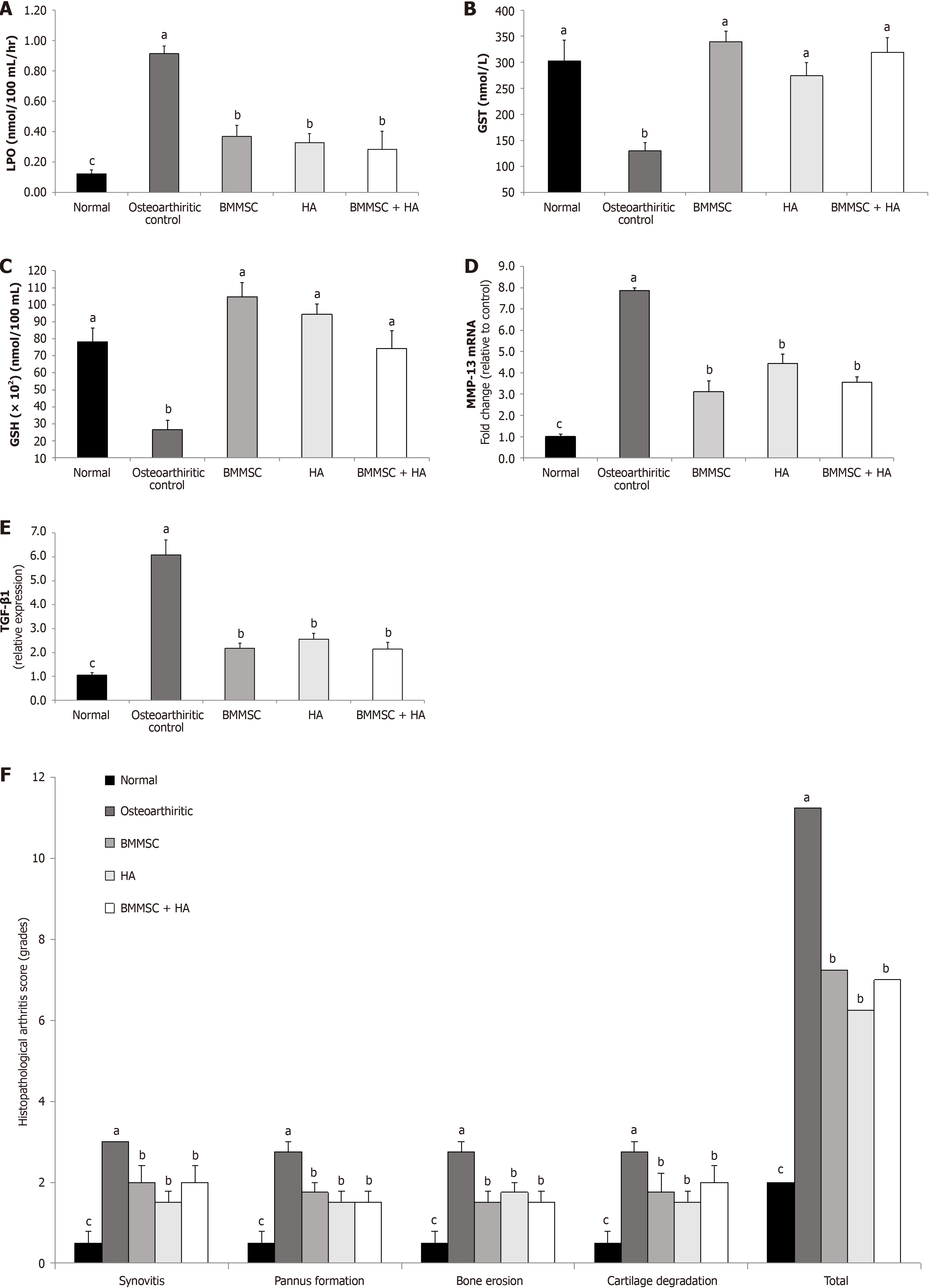
Figure 4 Effect of bone marrow mesenchymal stem cells and/ or hyaluronic acid treatments.
A: Effect of bone marrow mesenchymal stem cells (BMMSCs) and/or hyaluronic acid (HA) treatments on serum lipid peroxidation (LPO) level of monosodium iodate-administered rats; B: Effect of BMMSC and/or HA treatments on serum glutathione S-transferase (GST) activity in monosodium iodate-administered rats; C: Effect of BMMSC and/or HA treatments on serum glutathione (GSH) content in monosodium iodate-administered rats; D: Effect of BMMSC and/or HA treatments on matrix metalloproteinase 13 (MMP-13) mRNA expression level in joint tissue of monosodium iodate-administered rat; E: Effect of BMMSCs and/or HA treatments on transforming growth factor-β (TGF-b) protein expression level in the joint tissue of monosodium iodate-administered rat; F: Effect of BMMSCs and/or HA treatments on the histopathological arthritis score monosodium iodate-administered rat. The histological lesion scores of synovitis (synovial inflammation), pannus formation, bone resorption, and cartilage destruction were demonstrated. aP < 0.05, compared values with b, c and d are significantly different; bP < 0.05, compared values with a, c and d are significantly different; cP < 0.05, compared values with a, b and d are significantly different; dP < 0.05, compared values with a, b, and c are significantly different.
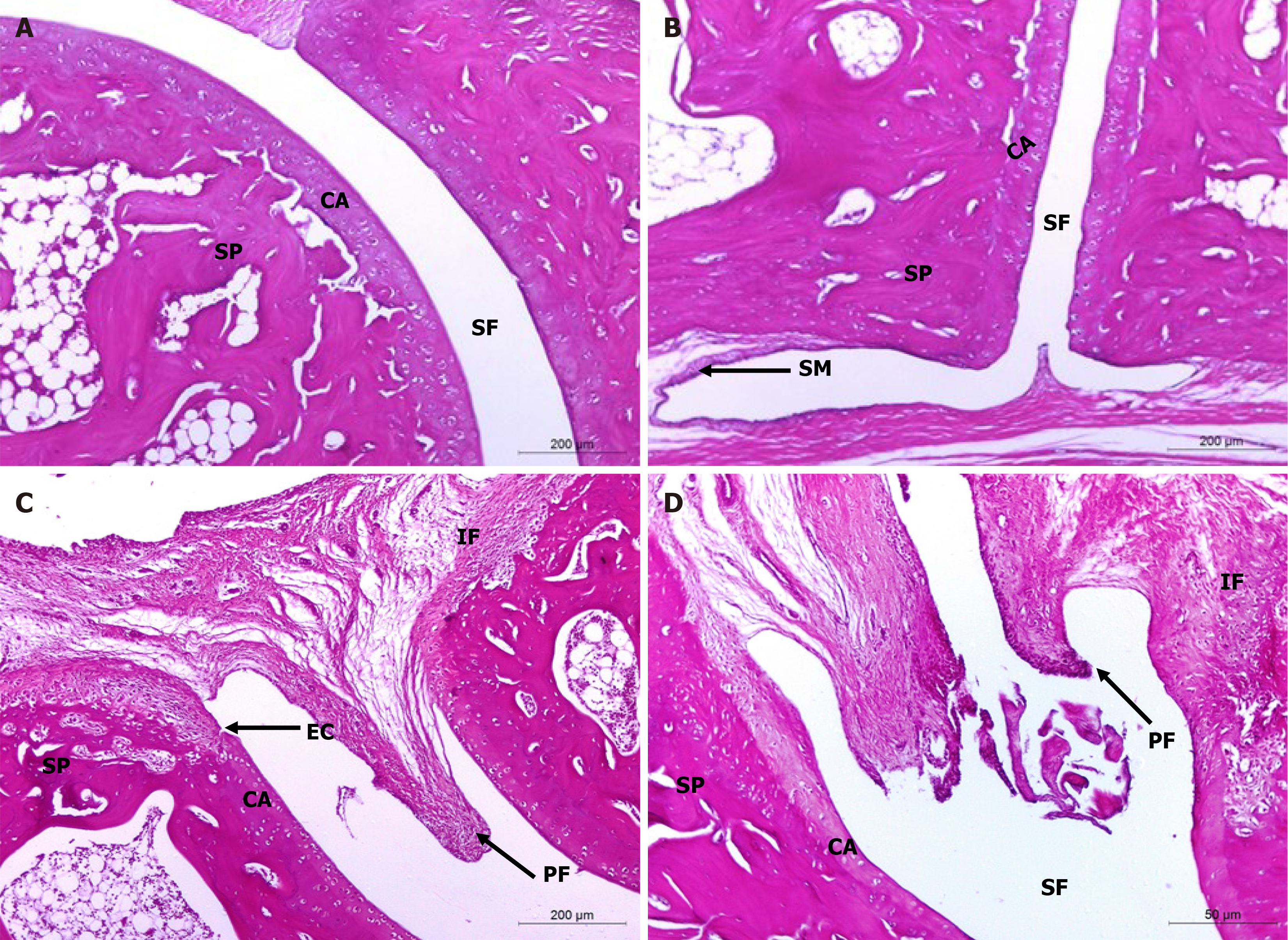
Figure 5 Histopathological evaluation of treatments on monosodium iodate-induced osteoarthritis in rat.
A and B: Microphotographs showing the histological changes in hind ankle of normal control (photomicrographs); C and D: Osteoarthritic control rats (photomicrographs) in Hematoxylin and eosin (100 ×) stained sections. The integral histological architecture of hind ankle joints was found in normal control rats. Osteoarthritic control rats showed synovial hyperplasia, mononuclear inflammatory cell infiltration, marked pannus formation, cartilage destruction and bone erosion. CA: Articular cartilage; EC: Erosion of cartilage; IF: Inflammatory cells infiltration; PF: Pannus formation; SF: Synovial fluid; SM: Synovial membrane; SP: Spongy bone.
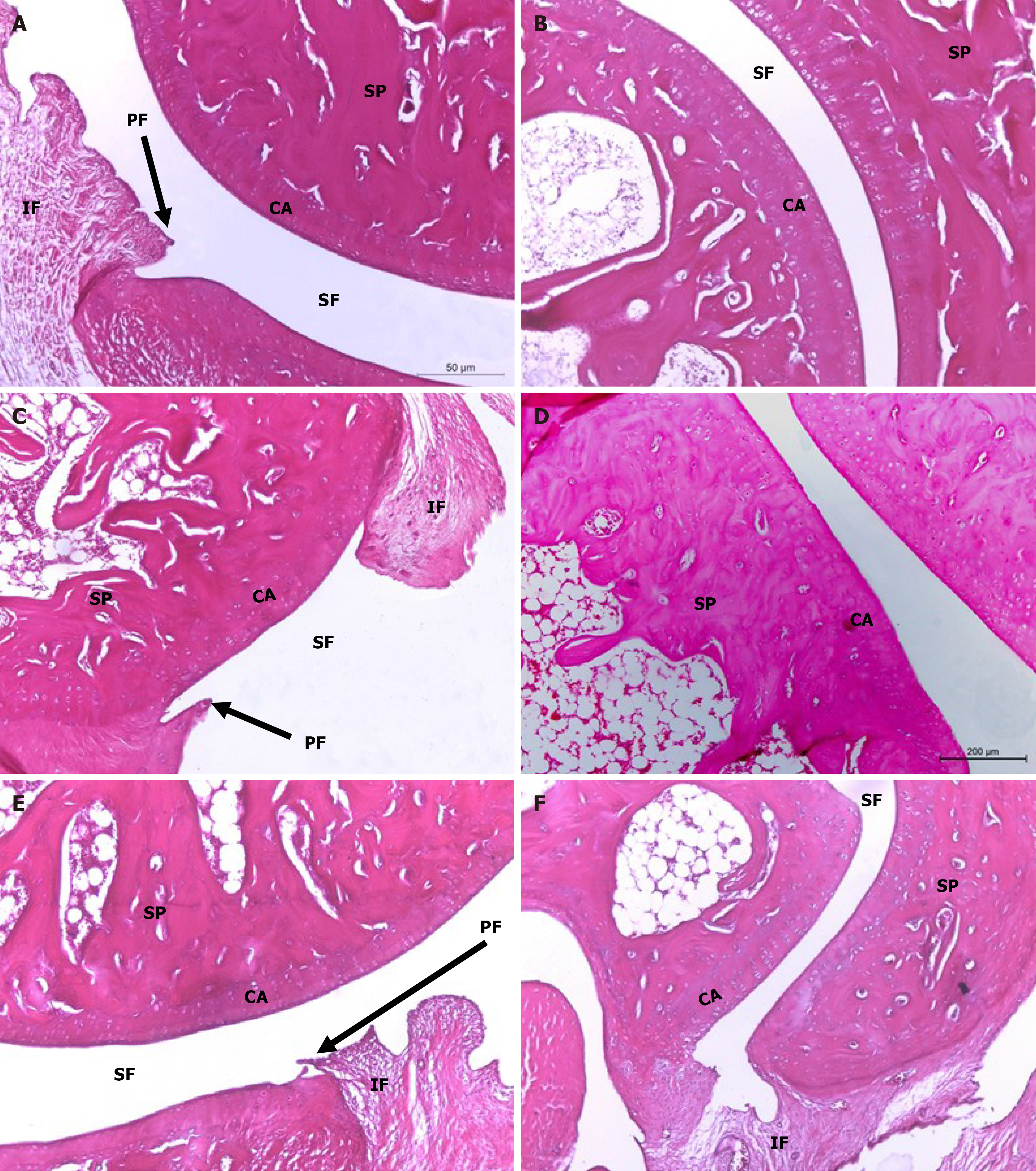
Figure 6 Histopathological evaluation of treatments on monosodium iodate-induced osteoarthritis in rat.
Microphotographs showing the histological changes of hind ankle in hematoxylin and eosin (100 ×) stained sections. A and B: The histological picture of hind ankle joints of osteoarthritic rats treated with hyaluronic acid (HA); C and D: The histological picture of hind ankle joints of osteoarthritic rats treated with bone marrow mesenchymal stem cells (BMMSCs); E and F: Treated with BMMSCs + HA revealed improvements in the ankle joint articular tissue integrity and architecture with suppressed inflammation and reduced synovial membrane thickening. CA: Articular cartilage; EC: Erosion of cartilage; IF: Inflammatory cell infiltration; PF: Pannus formation; SF: Synovial fluid; SM: Synovial membrane; SP: Spongy bone.
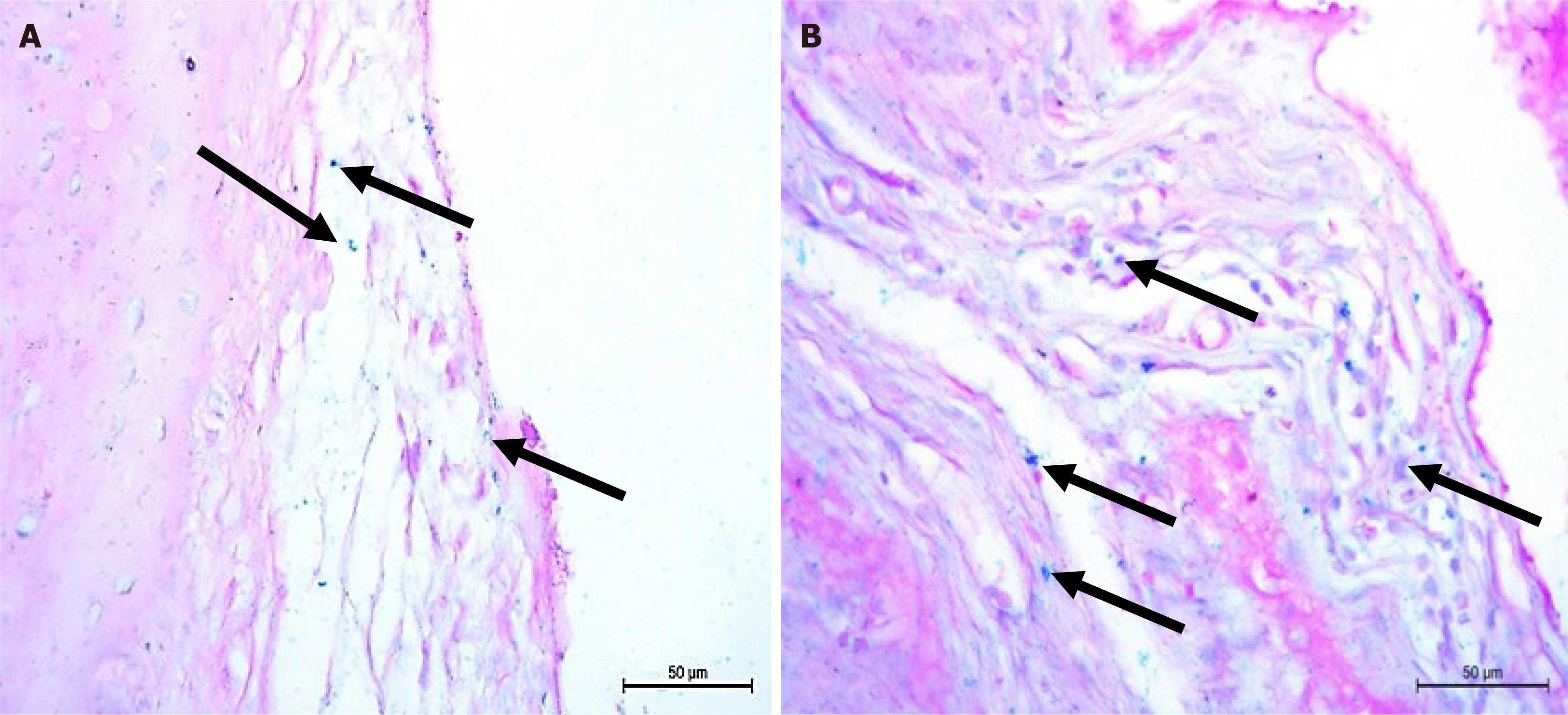
Figure 7
Osteoarthritic rats in bone marrow mesenchymal stem cells treated groups showing Prussian blue positive cells were distri
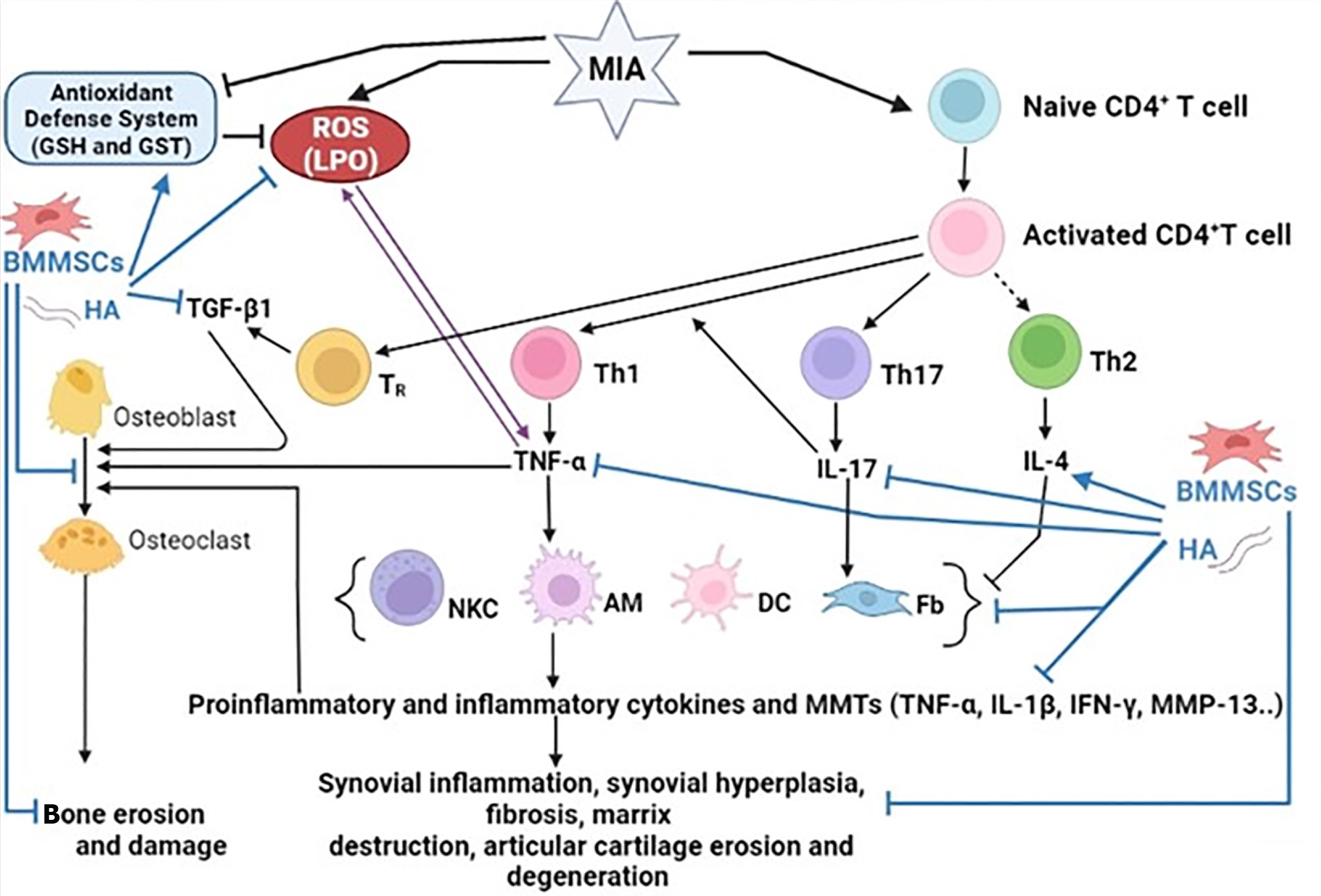
Figure 8 Schematic figure showing mechanisms of actions of bone marrow mesenchymal stem cells and hyaluronic acid in improving osteoarthritis in Wistar rats.
BMMSCs: Bone marrow mesenchymal stem cells; GSH: Glutathione; GST: Glutathione S-transferase; HA: Hyaluronic acid; IL-17: Interleukin-17; LPO: Lipid peroxidation; MIA: Monosodium iodate; MMP-13: Matrix metalloproteinase 13; ROS: Reactive oxygen species; TGF-β1: Transforming growth factor beta 1; TNF-α: Tumor necrosis factor alpha.
- Citation: Hagag UI, Halfaya FM, Al-Muzafar HM, Al-Jameel SS, Amin KA, Abou El-Kheir W, Mahdi EA, Hassan GANR, Ahmed OM. Impacts of mesenchymal stem cells and hyaluronic acid on inflammatory indicators and antioxidant defense in experimental ankle osteoarthritis. World J Orthop 2024; 15(11): 1056-1074
- URL: https://www.wjgnet.com/2218-5836/full/v15/i11/1056.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i11.1056