Copyright
©The Author(s) 2022.
World J Orthop. Mar 18, 2022; 13(3): 238-249
Published online Mar 18, 2022. doi: 10.5312/wjo.v13.i3.238
Published online Mar 18, 2022. doi: 10.5312/wjo.v13.i3.238
Figure 1 Fat pad sign.
Lateral radiograph of a 13-year-old boy, showing an anterior and posterior fat pad sign without visible fracture. A proximal radius fracture was identified using computed tomography.
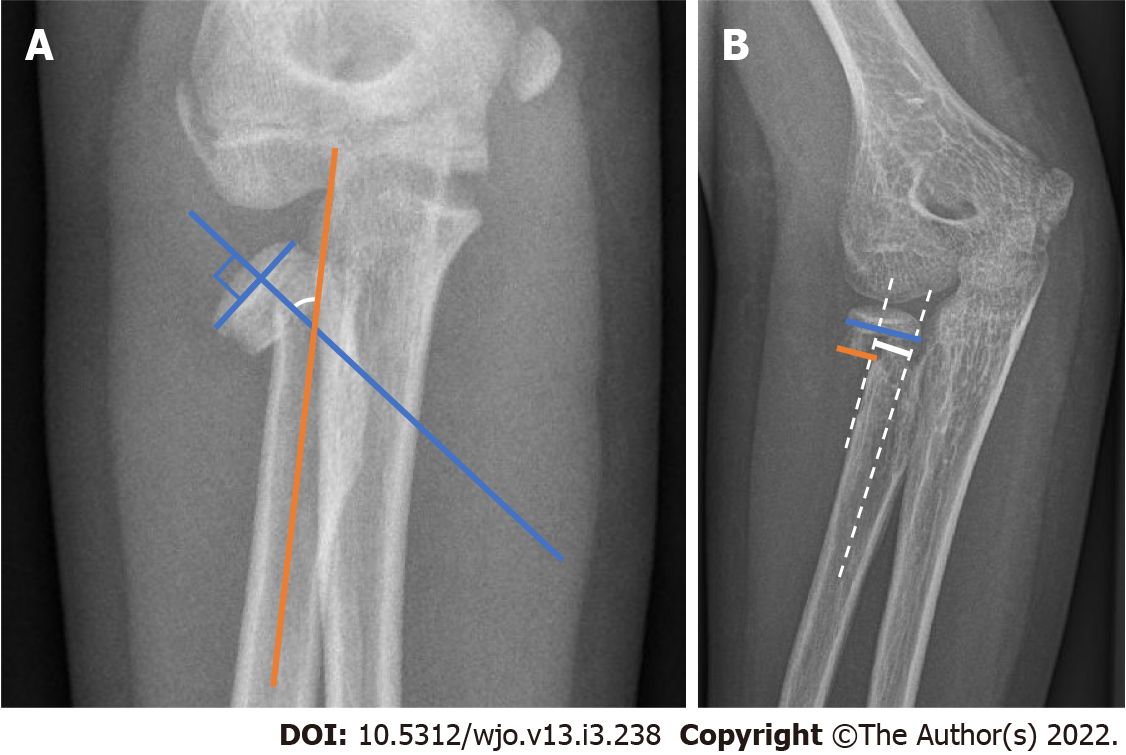
Figure 2 Measurement of angulation and translation of the proximal radius fracture.
A: Angulation measurement. Angulation of a proximal radius fracture is measured by drawing a line perpendicular to the surface of the radial head (blue line) and a line through the middle of the radial shaft (orange line). The angle is measured at the intersection of the two lines (white arc); B: Translation measurement. Translation of a proximal radius fracture is calculated by dividing the length the uncovered part of the metaphysis (orange line) by the total width of the proximal radius (blue line), multiplying by one hundred provides the percentage of translation. Alternatively, the distance from the middle of the proximal part to the middle of the distal part can be measured in millimeters (continuous white line).
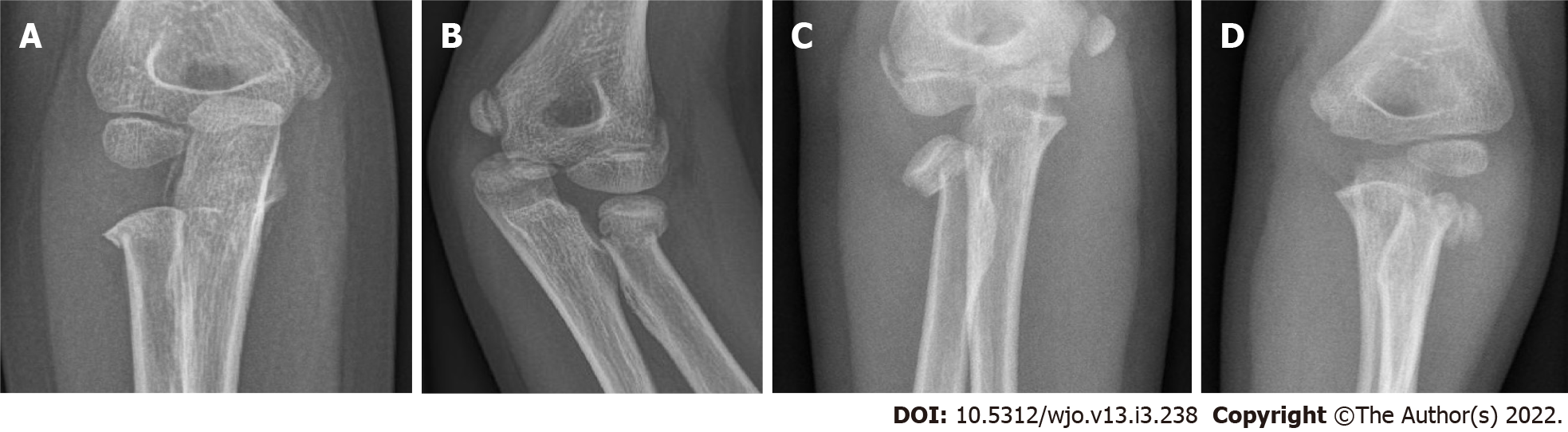
Figure 3 Anteroposterior radiograph of proximal radius fracture.
A: Grade I fracture. Anteroposterior radiograph of a 5-year-old boy with a proximal radius fracture that is (nearly) nondisplaced. Judet grade I; Metaizeau grade I; O’Brien type I; B: Grade II fracture. Radiograph of a 9-year-old girl with a proximal radius fracture in 27 degrees of angulation and 17% translation. Judet grade II; Metaizeau grade II; O’Brien type I; C: Grade III fracture. Anteroposterior radiograph of a 10-year-old girl with a proximal radius fracture in 58 degrees of angulation and 55% translation. Judet grade III; Metaizeau grade III; O’Brien type II; D: Grade IV fracture. Anteroposterior radiograph of a 7-year-old girl with a proximal radius fracture in 87 degrees of angulation and 80% translation. Judet grade IVb; Metaizeau grade IVb; O’Brien type III.
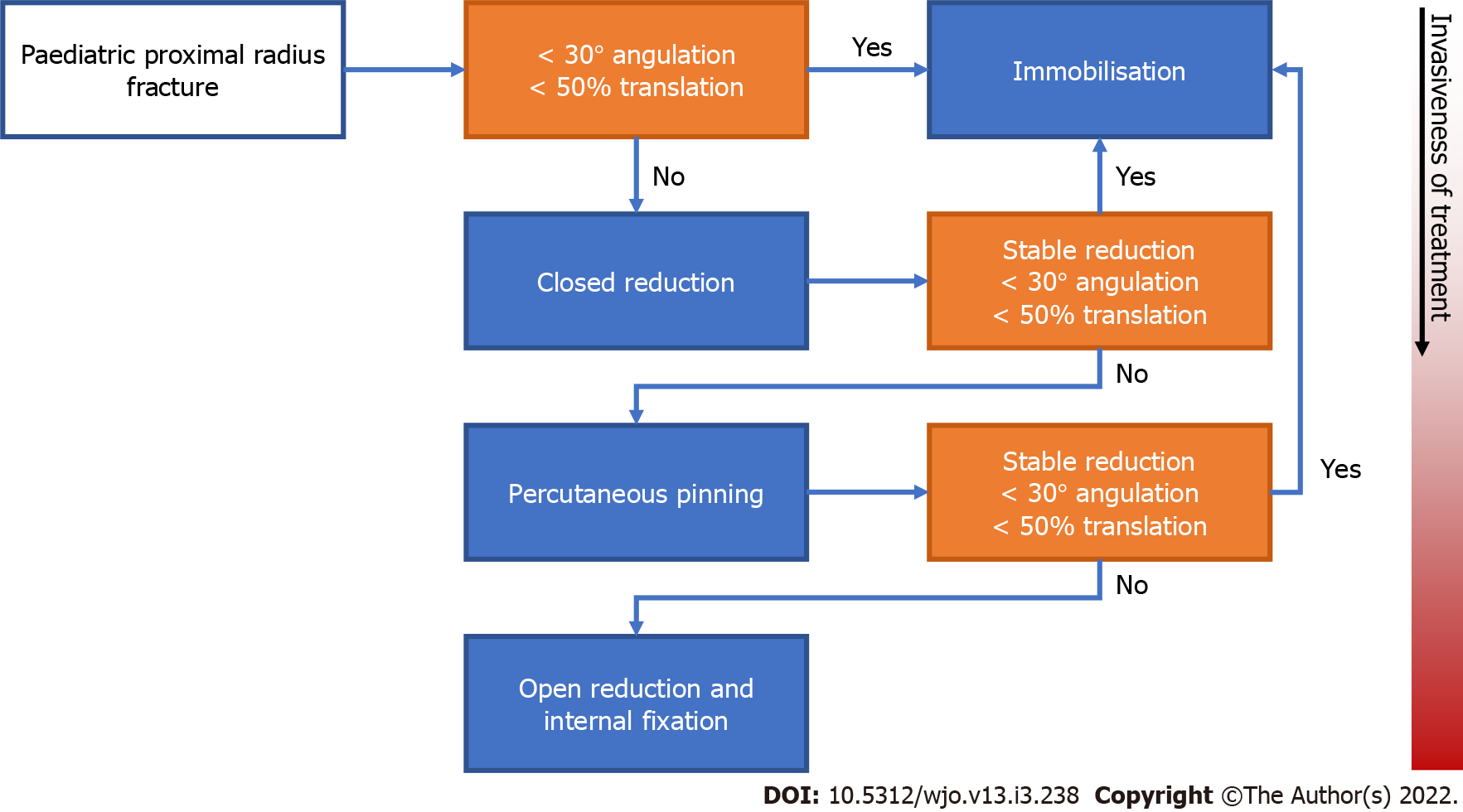
Figure 4 Treatment flowchart.
Treatment flowchart that plots the stepwise progression from conservative to increasingly invasive treatment of pediatric proximal radius fractures. Starting from the left, orange boxes represent points of decision-making and blue boxes represent treatment options. Boxes placed lower in the chart represent more invasive procedures than those placed above.
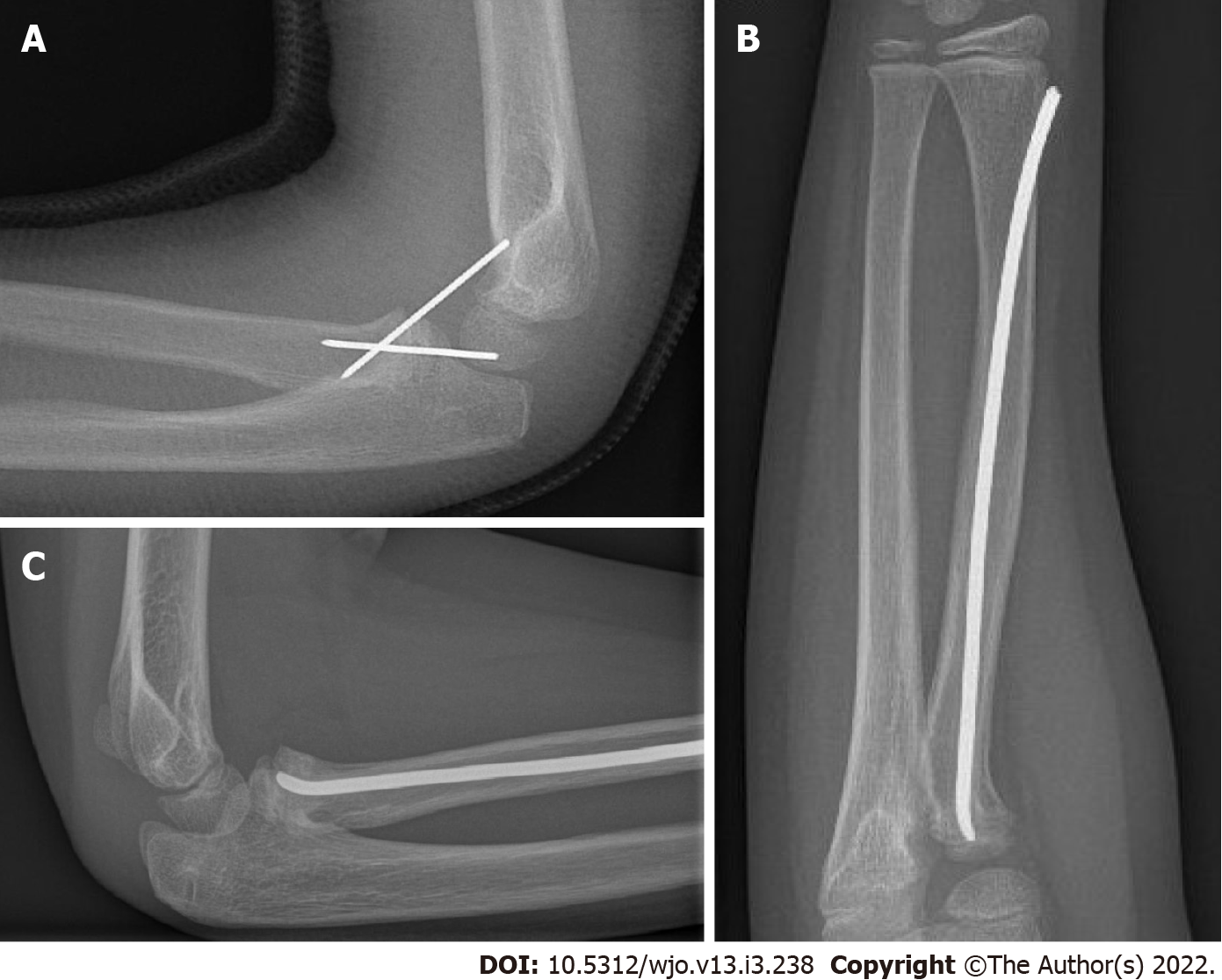
Figure 5 A fracture can be reduced percutaneously in several ways.
A: Percutaneous Kirschner wire fixation. Lateral radiograph of a 7-year-old boy with a proximal radius fracture after percutaneous reduction and fixation using two Kirschner wires; B and C: Intramedullary nail: Anteroposterior radiograph of a 10-year-old girl with a proximal radius fracture that was reduced and fixated using a flexible intramedullary nail (Metaizeau technique) (B), Lateral radiograph of a 10-year-old girl with a proximal radius fracture that was reduced and fixated using a flexible intramedullary nail (Metaizeau technique) (C).
- Citation: Macken AA, Eygendaal D, van Bergen CJ. Diagnosis, treatment and complications of radial head and neck fractures in the pediatric patient. World J Orthop 2022; 13(3): 238-249
- URL: https://www.wjgnet.com/2218-5836/full/v13/i3/238.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i3.238