Copyright
©The Author(s) 2021.
World J Orthop. Sep 18, 2021; 12(9): 685-699
Published online Sep 18, 2021. doi: 10.5312/wjo.v12.i9.685
Published online Sep 18, 2021. doi: 10.5312/wjo.v12.i9.685
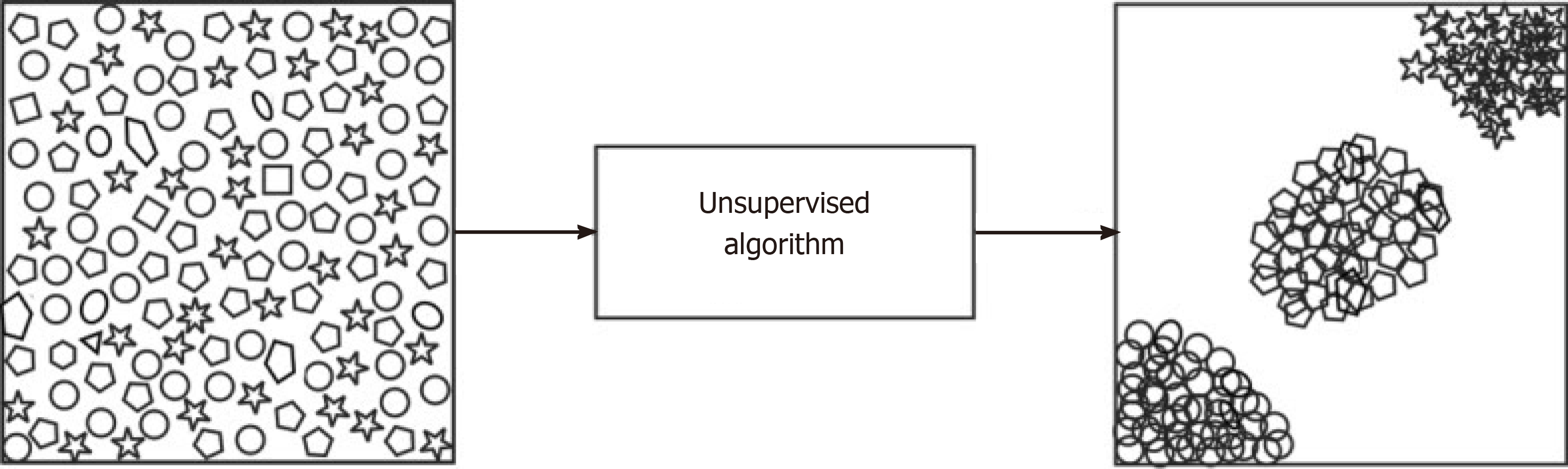
Figure 1 A visual illustration of an unsupervised algorithm[11].
Reused with permission. Citation: Sidey-Gibbons JAM, Sidey-Gibbons CJ. Machine learning in medicine: a practical introduction. BMC Med Res Methodol 2019; 19: 64.
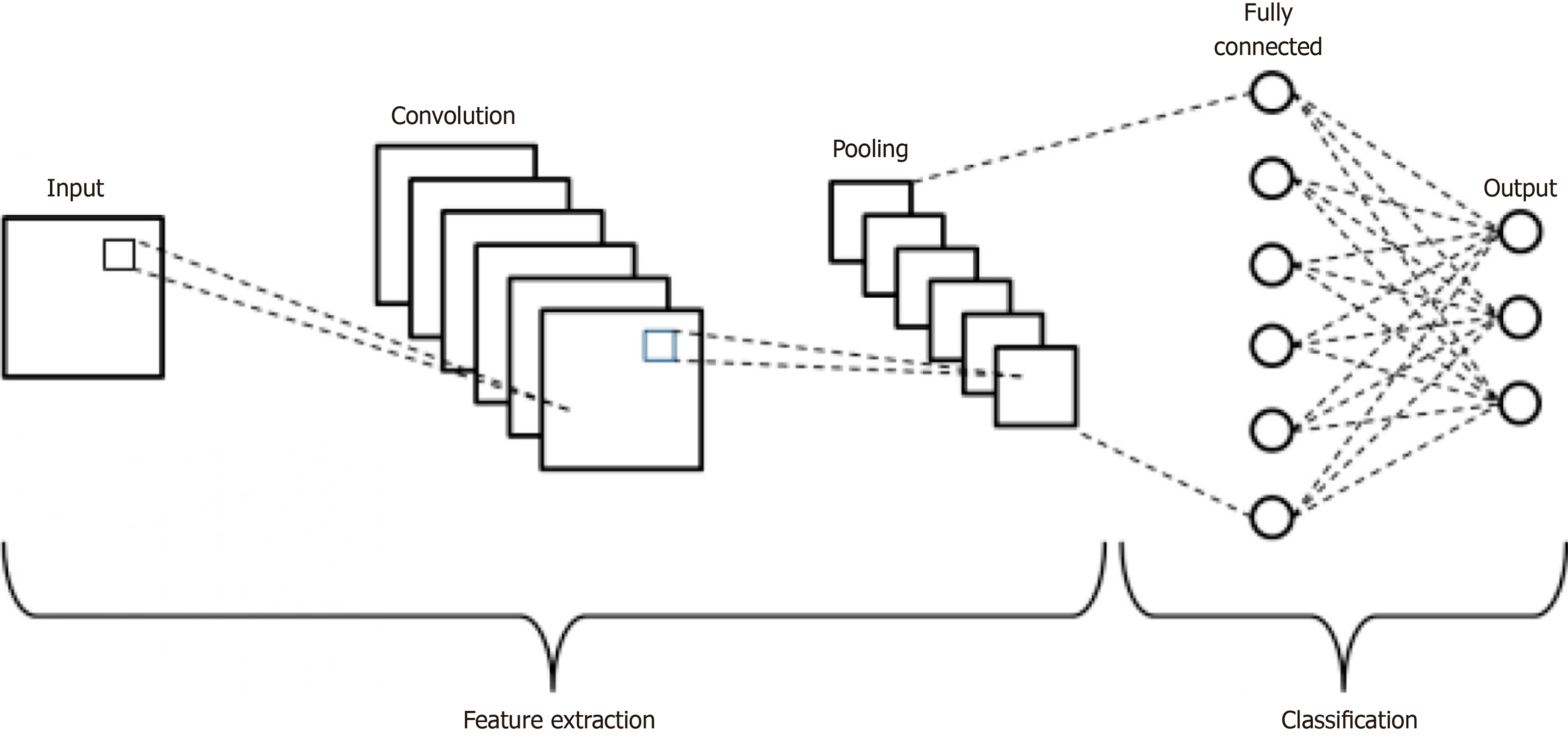
Figure 2 Schematic diagram of a basic convolutional neural network architecture[18].
Reused with permission. Citation: Phung VH, Rhee EJ. A High-Accuracy Model Average Ensemble of Convolutional Neural Networks for Classification of Cloud Image Patches on Small Datasets. App Sci 2019; 9: 4500.
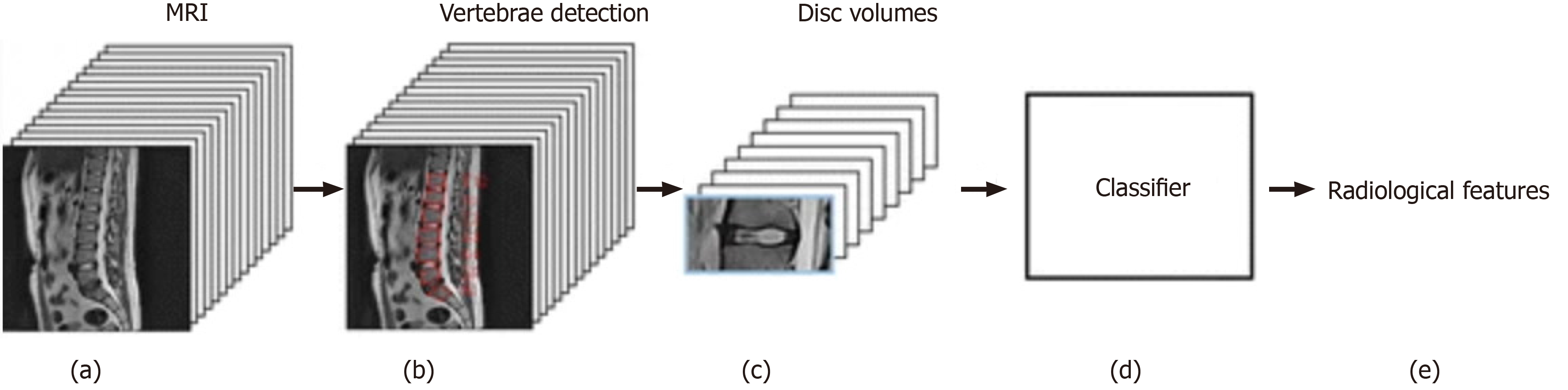
Figure 3 Input processing pipeline of T2 sagittal magnetic resonance imaging and output predictions of radiological features[65].
Reused with permission. Citation: Jamaludin A, Lootus M, Kadir T, Zisserman A, Urban J, Battié MC, Fairbank J, McCall I; Genodisc Consortium. ISSLS PRIZE IN BIOENGINEERING SCIENCE 2017: Automation of reading of radiological features from magnetic resonance images (MRIs) of the lumbar spine without human intervention is comparable with an expert radiologist. Eur Spine J 2017; 26: 1374-1383.
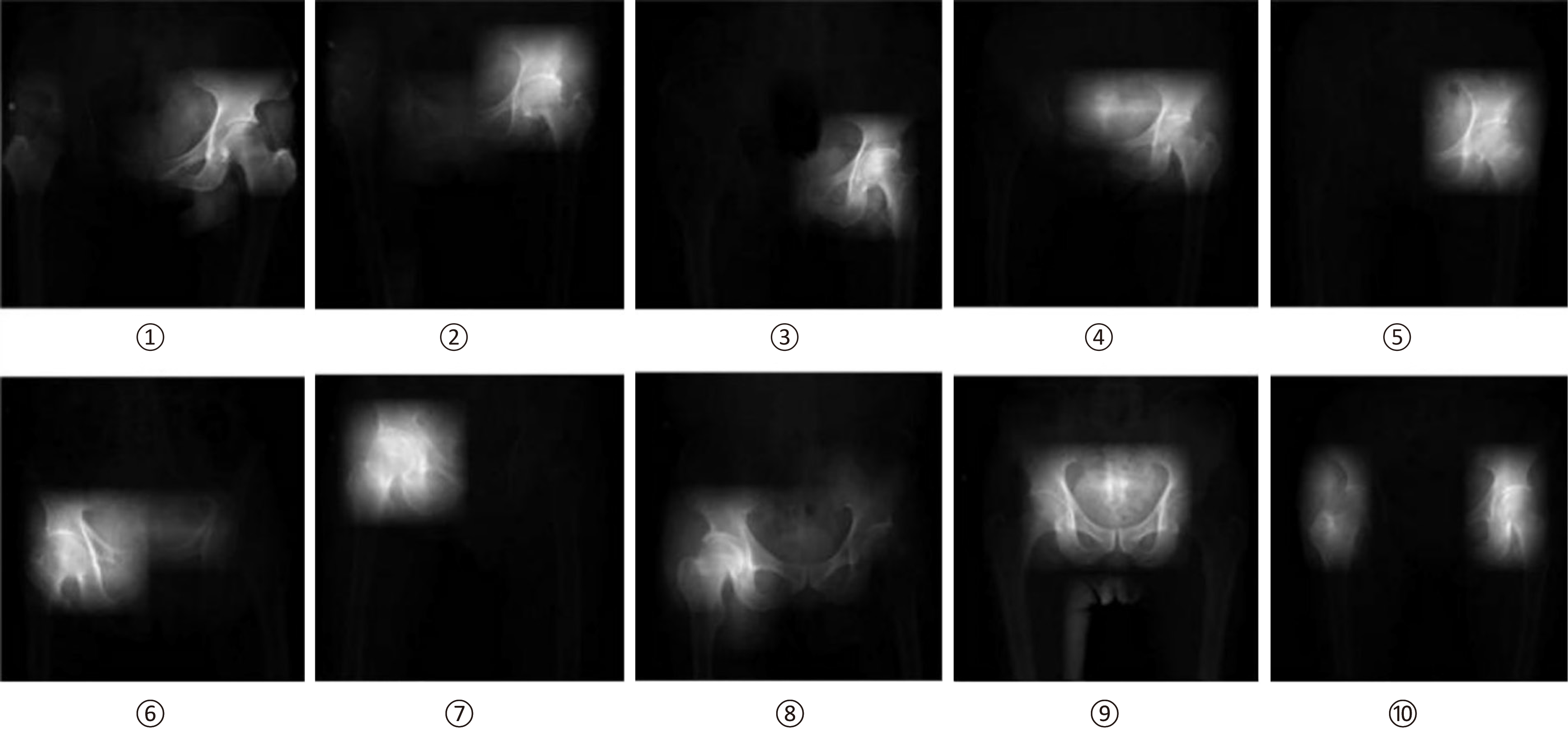
Figure 4 Saliency images from left hip joint (1-5), right hip joint (6-8), and both hip joints (9,10)[70].
Reused with permission. Citation: Xue Y, Zhang R, Deng Y, Chen K, Jiang T. A preliminary examination of the diagnostic value of deep learning in hip osteoarthritis. PLoS One 2017; 12: e0178992.
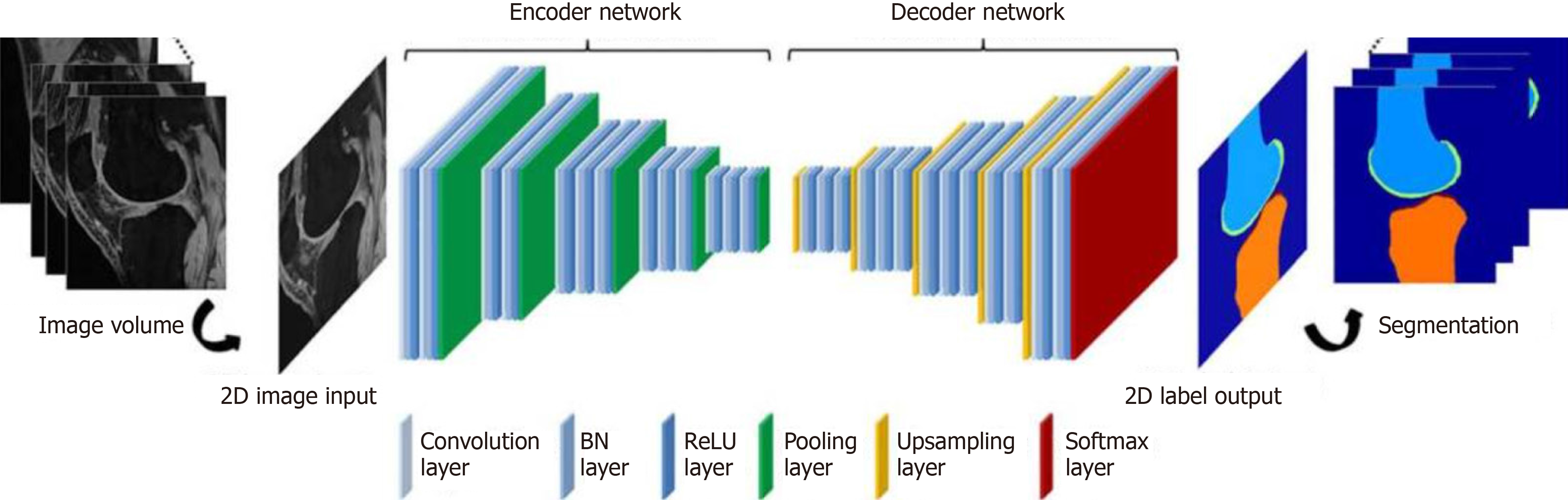
Figure 5 Convolutional neural network depiction of a knee image data set for bone and cartilage segmentation and labeling[72].
Reused with permission. Citation: Liu F, Zhou Z, Jang H, Samsonov A, Zhao G, Kijowski R. Deep convolutional neural network and 3D deformable approach for tissue segmentation in musculoskeletal magnetic resonance imaging. Magn Reson Med 2018; 79: 2379-2391.
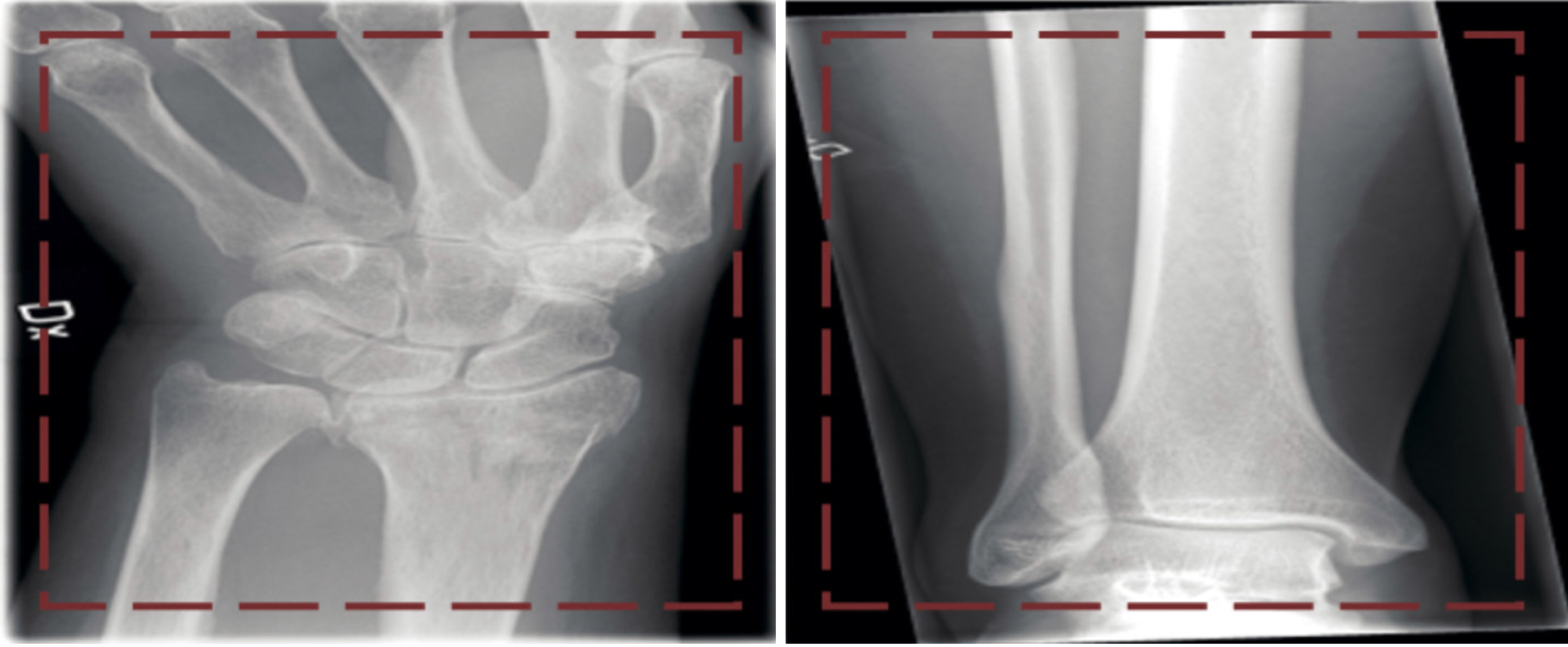
Figure 6 Two images (left, wrist fracture; right, no fracture) from the dataset presented to the network[74].
Reused with permission. Citation: Olczak J, Fahlberg N, Maki A, Razavian AS, Jilert A, Stark A, Sköldenberg O, Gordon M. Artificial intelligence for analyzing orthopedic trauma radiographs. Acta Orthop 2017; 88: 581-586.
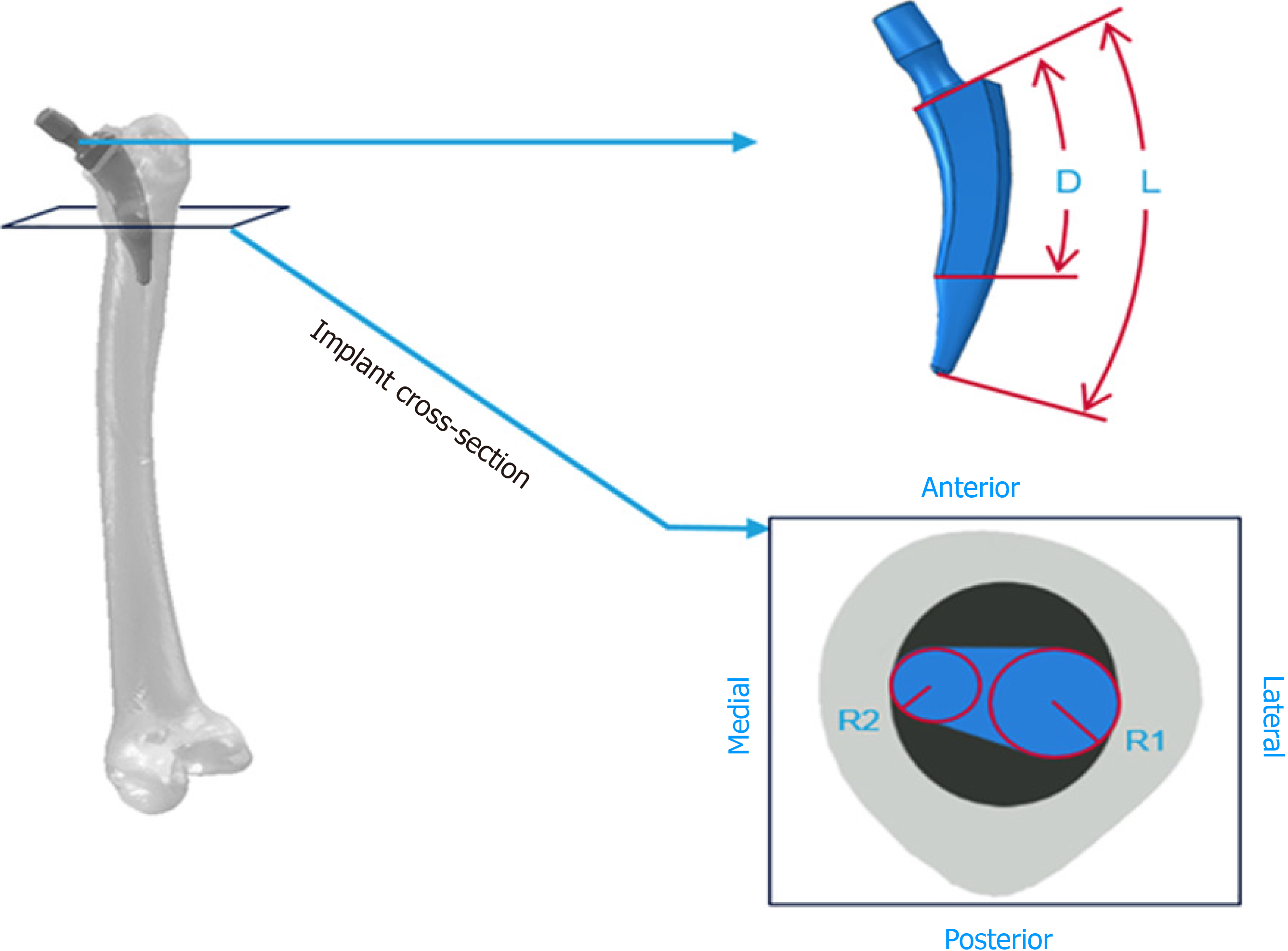
Figure 7 Graphic representation of the four parameters (L, total stem length; R1, radial circumference in the lateral side; R2, radial circumference in the medial; D, distance between the implant neck and the central stem surface)[86].
Reused with permission. Citation: Cilla M, Borgiani E, Martínez J, Duda GN, Checa S. Machine learning techniques for the optimization of joint replacements: Application to a short-stem hip implant. PLoS One 2017; 12: e0183755.
- Citation: Lalehzarian SP, Gowd AK, Liu JN. Machine learning in orthopaedic surgery. World J Orthop 2021; 12(9): 685-699
- URL: https://www.wjgnet.com/2218-5836/full/v12/i9/685.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i9.685