Published online Feb 10, 2018. doi: 10.5306/wjco.v9.i1.20
Peer-review started: September 7, 2017
First decision: October 30, 2017
Revised: November 5, 2017
Accepted: December 4, 2017
Article in press: December 4, 2017
Published online: February 10, 2018
Processing time: 157 Days and 3.5 Hours
Adrenocortical carcinoma (ACC) is a rare malignancy with generally poor outcomes and limited treatment options. While surgical resection can be curative for early local disease, most patients present with advanced ACC owing to nonspecific symptoms. For those patients, treatment options include systemic chemotherapy and locoregional therapies including radiofrequency ablation and transarterial chemoembolization. We present the first reported case of utilizing yttrium-90 microsphere selective internal radiation therapy (SIRT) in combination with first line EDP-M (Etoposide, Doxorubicin, Cisplatin, Mitotane) chemotherapy and debulking surgical primary tumor resection for treatment of metastatic ACC. Stable complete radiologic response has been maintained after twelve months with resolution of clinical symptoms. These findings prompt the need for further consideration and studies to elucidate the role of SIRT in combination with systemic and surgical treatment for metastatic ACC.
Core tip: Adrenocortical carcinoma (ACC) is a rare malignancy with generally poor outcomes and limited treatment options. Approximately 70% of ACC patients have unresectable stage III or IV disease on initial presentation. Yttrium-90 microsphere selective internal radiation therapy was applied toward hepatic metastases for a patient with metastatic ACC in combination with first line chemotherapy and debulking surgical primary tumor resection. A stable complete radiologic response has been maintained for twelve months with resolution of clinical symptoms.
- Citation: Makary MS, Krishner LS, Wuthrick EJ, Bloomston MP, Dowell JD. Yttrium-90 microsphere selective internal radiation therapy for liver metastases following systemic chemotherapy and surgical resection for metastatic adrenocortical carcinoma. World J Clin Oncol 2018; 9(1): 20-25
- URL: https://www.wjgnet.com/2218-4333/full/v9/i1/20.htm
- DOI: https://dx.doi.org/10.5306/wjco.v9.i1.20
Adrenocortical carcinoma (ACC) is a rare malignancy that constitutes less than 5% of all adrenal incidentalomas and has an estimated annual incidence of 1-2 cases per million people[1-3]. ACC carries a poor prognosis with an overall 5-year survival of 16%-44%[4-6]. Surgical resection is the treatment of choice with those presenting with only local disease. However, most patients present with advanced disease and are not surgical candidates, and 80% of even those patients with local disease treated surgically develop local or distant recurrence following complete resection[7]. Indeed, given the nonspecific ACC symptoms, approximately 70% of ACC patients have unresectable stage III or IV disease on initial presentation[8]. In those cases, treatment options include mitotane, systemic chemotherapy, external beam radiotherapy, radiofrequency ablation (RFA), transarterial chemoembolization (TACE), or a combination of these therapies. In this case study, we present a complete radiologic and clinical response to yttrium-90 (Y-90) microsphere selective internal radiation therapy (SIRT) treatment of hepatic metastases in conjunction with surgery and chemotherapy for treatment of a patient with advanced disease. A critical review of the current therapies and treatment strategies is also presented.
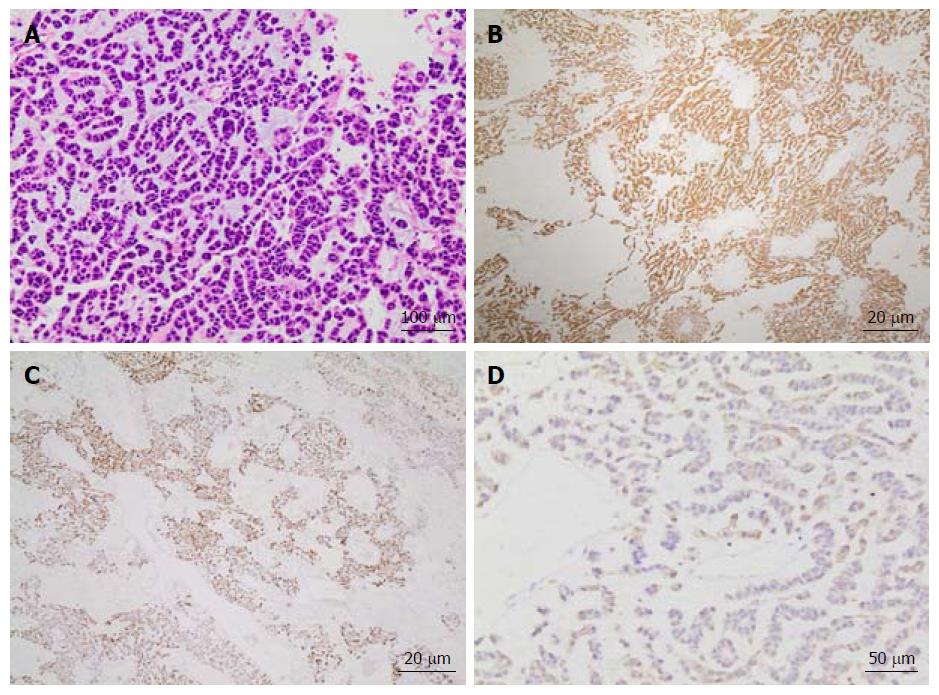
A 60-year-old female patient with a past medical history significant only for poorly controlled hypertension despite medical therapy presented with a large left adrenal mass incidentally discovered on MRA during workup for renal artery stenosis. Abdominal MR imaging revealed a heterogeneous, partially necrotic left adrenal mass measuring 5.6 cm × 8.9 cm as well as multiple bilobar enhancing liver metastases. Histologic (Figure 1A) and immunologic evaluation of a biopsied hepatic lesion showed metastatic carcinoma positive for inhibin (Figure 1B), melan-A (Figure 1C), and CKAE1/3 (Figure 1D) with an immunohistochemical staining profile consistent with metastatic ACC. Serology values revealed normal urine cortisol [14.1 mcg/24 h (normal range: 3-22)], low adrenocorticotropic hormone (ACTH) [5.1 pg/mL (normal range: 9-50)], normal plasma metanephrines [0.20 nmol/L (normal range < 0.50)] and high aldosterone [38.8 ng/dL (normal range: 1-16)].
The Berruti chemotherapy regimen of Etoposide, Doxorubicin and Cisplatin plus Mitotane (EDP-M) was immediately initiated[9] for a total of five 28-d cycles. Subsequent abdominal MRI and PET/CT evaluation demonstrated overall improvement in metastatic disease burden with interval decrease in size of the left adrenal mass. Given the response to chemotherapy and following a multidisciplinary tumor board discussion, decision was made to pursue an open adrenalectomy debulking surgery two months following chemotherapy completion to reduce the hormonal load for clinical symptomatic control. Intraoperatively, the entire adrenal mass was resected en bloc without difficulty. Adjacent paraaortic, omental, peripancreatic thickened pearly lymph nodes were resected with a clear periadrenal margin obtained. The adrenal vein and artery were identified with no tumoral involvement visualized. The patient had an uneventful post-operative hospital course and was discharged in 5 d in stable condition.
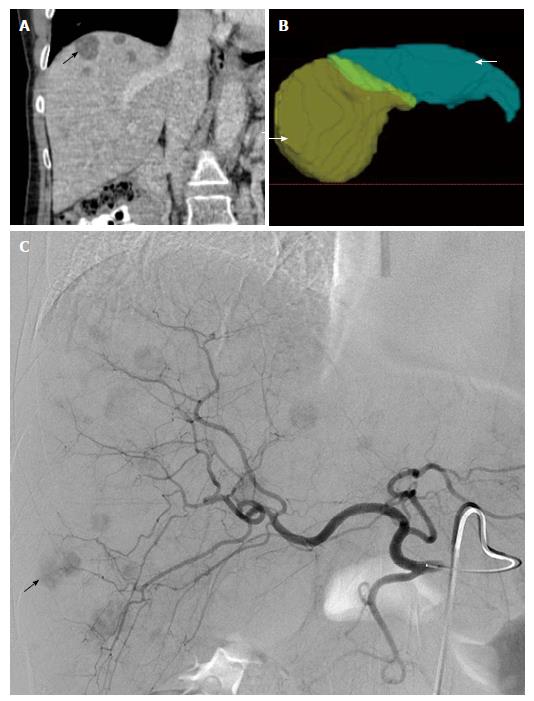
Additionally, to further control the bilobar liver metastases, decision was made to undergo two lobar Y-90 treatments using Y-90 TheraSphere microspheres (BTG, London, United Kingdom). The patient was evaluated for radioembolization with selective hepatic arteriography (Figure 2). Arterial administration of 4.1 mCi of 99mTc-MAA (Drax Image MAA kit; 99.7% purity) in the proper hepatic artery demonstrated a hepatopulmonary shunt of 0.8% on planar scintigraphy and SPECT, which is within acceptable range (< 10%). Additional pretreatment planning included evaluation with an abdominal CTA which revealed no variant vascular anatomy (Figure 2A). Based on imaging, estimated right hepatic lobe volume of 1339 ml and left hepatic lobe volume of 409 ml were used to calculate the radioactivity required to deliver a desired dose of 120 Gy to each lobe (Figure 2B). Patient underwent treatment of the right hepatic lobe (Figure 2C) followed by the left lobe within a month. Post-treatments, she tolerated the procedures well with low-grade fevers lasting for 24 h and intermittent right upper quadrant pain, both of which are common and expected following this treatment, which resolved within 2-3 wk.
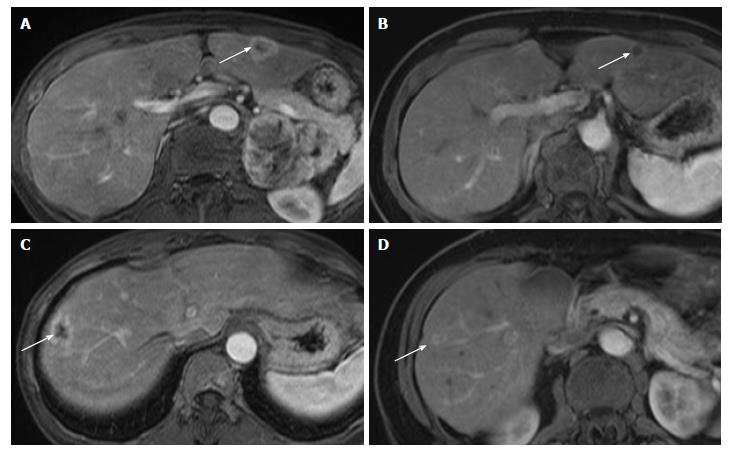
The patient tolerated the treatment well, experienced a drop in aldosterone levels (2.8 ng/dL), and has been normotensive and off of antihypertensive medication following intervention. Post Y-90 therapy imaging at 1 year revealed significantly smaller and less numerous hepatic lesions (Figure 3). Additionally, no mass was identified in the adrenal resection. Patient is currently in observation with periodic surveillance imaging and serology.
ACC is a rare malignancy but is highly lethal with limited treatment options. Given its rarity, ACC is difficult to study with most studies being retrospective case series with several key randomized trials[9-11]. In a large landmark Phase II trial by Berruti et al[9] in 2005, the combination of etoposide, doxorubicin and cisplatin plus mitotane (EDP-M) in the treatment of advanced adrenocortical carcinoma demonstrated an overall response rate of 49%, a median time to progression of 9.1 mo, and an overall survival of 28.5 mo in a cohort of 72 patients[9]. A previous study by Khan et al[10] in 2000 reported an overall response rate of 36% and a 2- and 5-year survival of 70% and 33%, respectively, with mitotane plus streptozotocin (M-S). In the First International Randomized trial in locally advanced and Metastatic Adrenocortical Carcinoma Treatment (FIRM-ACT) in 2012 of 304 patients, there was no significance difference in the overall survival between EDP-M vs M-S (14.8 mo and 12.0 mo, respectively, P = 0.07), but the response rates (23.2% vs 9.2%, P < 0.001) and progression-free survival (5.0 mo vs 2.1 mo, P < 0.001) were significantly better with EDP-M[11].
In addition to systemic chemotherapy, surgical resection and local treatment modalities such as RFA and TACE are key palliative treatment options. While adrenalectomy for local ACC disease can be curable and is first line therapy, surgical debulking is also often performed, as done here, in the setting of advanced metastatic disease for control of hormone excess[12]. RFA has been also used in addition to surgery or as an alternative to surgery to reduce tumor burden. TACE has been utilized previously to treat liver metastases, although its efficacy has not been assessed specifically for ACC in clinical trials. ACC patients have been rendered disease free following hepatic RFA treatment in retrospective studies, but RFA has limited efficacy in patients with bilobar and multiple lesions as in our patient, highly vascularized metastases, or metastases in proximity to large vessels due to the heat-sink effect[13,14]. In these patients, TACE, or the local intra-arterial delivery of chemotherapy to liver lesions with embolic agents, has been performed. Limited evaluation of TACE in the ACC literature demonstrates a partial response in 21% of patients and stabilization in 62%[15].
In our case, we chose to pursue Y-90 SIRT for bilobar liver disease in a patient with metastatic ACC with the hopes of improving upon the outcomes previously seen with TACE. The benefit of Y-90 over TACE is that it can be delivered in an outpatient setting rather than the inpatient setting as reported previously for ACC, which offers convenience for the patients and is potentially more cost-effective[16]. While Y-90 radioembolization has been primarily studied as a locoregional therapy for hepatic metastases from colorectal carcinoma or for multifocal hepatocellular carcinoma, we present its first successful utility when coupled with surgery and systemic chemotherapy to treat a patient with advanced ACC. Indeed, following a single session to each hepatic lobe, this patient has continued to demonstrate a positive radiologic and clinical response twelve months following treatment. Similar positive outcomes were observed by Hendlisz et al[17] in a Phase III trial comparing fluorouracil infusion alone or combined with Y-90 radioembolization for metastatic colorectal cancer to the liver, which revealed a longer time to progression in the Y-90 arm (5.5 mo vs 2.1 mo, P = 0.003). Cosimelli et al[18] reported the results of Phase II trial showing that radioembolization alone produced meaningful response and disease stabilization in patients with advanced, unresectable and chemorefractory metastatic CRC[18]. Our findings prompt further investigation through similar trials for patients with advanced ACC.
In conclusion, this case study presents the successful treatment of metastatic ACC by combining Y-90 locoregional therapy for bilobar liver disease with first line EDP-M chemotherapy and debulking surgery. This strategy allowed for disease management for at least 12 mo following a single outpatient Y-90 treatment for each hepatic lobe rather than the repeated inpatient treatments required previously through TACE with possibly superior results. Future prospective trials are needed to further elucidate the role of Y-90 radioembolization for treatment of advanced ACC.
A 60-year-old female patient with a past medical history significant only for poorly controlled hypertension despite medical therapy presented with a large left adrenal mass incidentally discovered on MRA during workup for renal artery stenosis.
The clinical examination of the patient revealed elevated blood pressure and abdominal pain.
The differential diagnosis includes renal artery stenosis, adrenal phenochromcytoma, adrenocortical carcinoma, hyperaldosteronism, and hyperthyroidism.
Serology values revealed normal urine cortisol [14.1 mcg/24 h (normal range: 3-22)], low adrenocorticotropic hormone (ACTH) [5.1 pg/mL (normal range: 9-50)], normal plasma metanephrines [0.20 nmol/L (normal range < 0.50)] and high aldoesterone [38.8 ng/dL (normal range: 1-16)].
Abdominal MR imaging revealed a heterogeneous, partially necrotic left adrenal mass measuring 5.6 cm × 8.9 cm as well as multiple bilobar enhancing liver metastases.
Histologic and immunologic evaluation of a biopsied hepatic lesion showed metastatic carcinoma positive for inhibin, melan-A, and CKAE1/3 with an immunohistochemical staining profile consistent with metastatic adrenocortical carcinoma.
We present the first reported case of utilizing yttrium-90 microsphere selective internal radiation therapy (SIRT) in combination with first line EDP-M (Etoposide, Doxorubicin, Cisplatin, Mitotane) chemotherapy and debulking surgical primary tumor resection for treatment of metastatic adrenocortical carincoma.
While surgical resection can be curative for early local disease, most patients present with advanced ACC owing to nonspecific symptoms. For those patients, previous reports studied treatment options including systemic chemotherapy and locoregional therapies including radiofrequency ablation and transarterial chemoembolization.
Adrenocortical carcinoma (ACC) is a rare malignancy that constitutes less than 5% of all adrenal incidentalomas and has an estimated annual incidence of 1-2 cases per million people. EDP-M (etoposide, doxorubicin and cisplatin plus mitotane) is first line chemotherapy for advanced adrenocortical carcinoma demonstrating an overall response rate of 49%, a median time to progression of 9.1 mo, and an overall survival of 28.5 mo in prior studies.
This case study presents the successful treatment of metastatic ACC by combining Y-90 locoregional therapy for bilobar liver disease with first line EDP-M chemotherapy and debulking surgery. This strategy allowed for disease management for at least 12 mo following a single outpatient Y-90 treatment for each hepatic lobe rather than the repeated inpatient treatments required previously through TACE with possibly superior results.
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Cerwenka H, Demirci E, Sandri GBL, Tarazov PG, Tsoulfas G S- Editor: Kong JX L- Editor: A E- Editor: Li RF
| 1. | Zini L, Porpiglia F, Fassnacht M. Contemporary management of adrenocortical carcinoma. Eur Urol. 2011;60:1055-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Wandoloski M, Bussey KJ, Demeure MJ. Adrenocortical cancer. Surg Clin North Am. 2009;89:1255-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Koschker AC, Fassnacht M, Hahner S, Weismann D, Allolio B. Adrenocortical carcinoma -- improving patient care by establishing new structures. Exp Clin Endocrinol Diabetes. 2006;114:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Lafemina J, Brennan MF. Adrenocortical carcinoma: past, present, and future. J Surg Oncol. 2012;106:586-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Bilimoria KY, Shen WT, Elaraj D, Bentrem DJ, Winchester DJ, Kebebew E, Sturgeon C. Adrenocortical carcinoma in the United States: treatment utilization and prognostic factors. Cancer. 2008;113:3130-3136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 360] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 6. | Berruti A, Baudin E, Gelderblom H, Haak HR, Porpiglia F, Fassnacht M, Pentheroudakis G; ESMO Guidelines Working Group. Adrenal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23 Suppl 7:vii131-vii138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 219] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 7. | Dackiw AP, Lee JE, Gagel RF, Evans DB. Adrenal cortical carcinoma. World J Surg. 2001;25:914-926. [PubMed] |
| 8. | Fay AP, Elfiky A, Teló GH, McKay RR, Kaymakcalan M, Nguyen PL, Vaidya A, Ruan DT, Bellmunt J, Choueiri TK. Adrenocortical carcinoma: the management of metastatic disease. Crit Rev Oncol Hematol. 2014;92:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Berruti A, Terzolo M, Sperone P, Pia A, Della Casa S, Gross DJ, Carnaghi C, Casali P, Porpiglia F, Mantero F. Etoposide, doxorubicin and cisplatin plus mitotane in the treatment of advanced adrenocortical carcinoma: a large prospective phase II trial. Endocr Relat Cancer. 2005;12:657-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 190] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 10. | Khan TS, Imam H, Juhlin C, Skogseid B, Gröndal S, Tibblin S, Wilander E, Oberg K, Eriksson B. Streptozocin and o,p’DDD in the treatment of adrenocortical cancer patients: long-term survival in its adjuvant use. Ann Oncol. 2000;11:1281-1287. [PubMed] |
| 11. | Fassnacht M, Terzolo M, Allolio B, Baudin E, Haak H, Berruti A, Welin S, Schade-Brittinger C, Lacroix A, Jarzab B. Combination chemotherapy in advanced adrenocortical carcinoma. N Engl J Med. 2012;366:2189-2197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 585] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 12. | Else T, Kim AC, Sabolch A, Raymond VM, Kandathil A, Caoili EM, Jolly S, Miller BS, Giordano TJ, Hammer GD. Adrenocortical carcinoma. Endocr Rev. 2014;35:282-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 607] [Article Influence: 55.2] [Reference Citation Analysis (0)] |
| 13. | Ripley RT, Kemp CD, Davis JL, Langan RC, Royal RE, Libutti SK, Steinberg SM, Wood BJ, Kammula US, Fojo T. Liver resection and ablation for metastatic adrenocortical carcinoma. Ann Surg Oncol. 2011;18:1972-1979. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 14. | Bauditz J, Quinkler M, Wermke W. Radiofrequency thermal ablation of hepatic metastases of adrenocortical cancer--a case report and review of the literature. Exp Clin Endocrinol Diabetes. 2009;117:316-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Gates VL, Marshall KG, Salzig K, Williams M, Lewandowski RJ, Salem R. Outpatient single-session yttrium-90 glass microsphere radioembolization. J Vasc Interv Radiol. 2014;25:266-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | de Baere T, Teriitehau C, Deschamps F, Catherine L, Rao P, Hakime A, Auperin A, Goere D, Elias D, Hechelhammer L. Predictive factors for hypertrophy of the future remnant liver after selective portal vein embolization. Ann Surg Oncol. 2010;17:2081-2089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Hendlisz A, Van den Eynde M, Peeters M, Maleux G, Lambert B, Vannoote J, De Keukeleire K, Verslype C, Defreyne L, Van Cutsem E. Phase III trial comparing protracted intravenous fluorouracil infusion alone or with yttrium-90 resin microspheres radioembolization for liver-limited metastatic colorectal cancer refractory to standard chemotherapy. J Clin Oncol. 2010;28:3687-3694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 272] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 18. | Cosimelli M, Golfieri R, Cagol PP, Carpanese L, Sciuto R, Maini CL, Mancini R, Sperduti I, Pizzi G, Diodoro MG, Perrone M, Giampalma E, Angelelli B, Fiore F, Lastoria S, Bacchetti S, Gasperini D, Geatti O, Izzo F; Italian Society of Locoregional Therapies in Oncology (SITILO). Multi-centre phase II clinical trial of yttrium-90 resin microspheres alone in unresectable, chemotherapy refractory colorectal liver metastases. Br J Cancer. 2010;103:324-331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 162] [Article Influence: 10.8] [Reference Citation Analysis (0)] |