Published online Aug 10, 2017. doi: 10.5306/wjco.v8.i4.366
Peer-review started: December 1, 2016
First decision: February 17, 2017
Revised: June 12, 2017
Accepted: July 21, 2017
Article in press: July 24, 2017
Published online: August 10, 2017
Processing time: 250 Days and 22.4 Hours
Pulmonary artery intimal sarcoma (PAIS) is a rare tumor with a very poor prognosis. Clinical and radiological findings usually mimic thromboembolic disease, leading to diagnostic delays. The treatment of choice is surgery, and adjuvant chemotherapy and radiotherapy have limited results. We report the case of a 48-year-old male patient, initially suspected with pulmonary thromboembolism. The angio-CT revealed a filling defect in the pulmonary artery trunk. The patient underwent surgery, resulting in with complete resection of the mass with a diagnosis of PAIS. The tumor progressed rapidly in the lung, requiring surgery of multiple lung metastases. The patient was treated with stereotactic body radiation therapy (SBRT) on two occasions for new pulmonary lesions. In the last followup (4 years after initial diagnosis), the patient was disease-free. In conclusion, SBRT proved to be an alternative treatment to metastasectomy, allowing palliative chemotherapy to be delayed or omitted, which may result in improved quality of life.
Core tip: Intimal sarcoma of the pulmonary artery is a rare tumor with a very poor prognosis. It has been described in a limited number of reports. This case is a uncommon patient with long-term survival despite having rapid metastatic progression, who maintains a complete remission after initial surgical treatment, completed after occurrence of progression with stereotactic body radiotherapy.
- Citation: García-Cabezas S, Centeno-Haro M, Espejo-Pérez S, Carmona-Asenjo E, Moreno-Vega AL, Ortega-Salas R, Palacios-Eito A. Intimal sarcoma of the pulmonary artery with multiple lung metastases: Long-term survival case. World J Clin Oncol 2017; 8(4): 366-370
- URL: https://www.wjgnet.com/2218-4333/full/v8/i4/366.htm
- DOI: https://dx.doi.org/10.5306/wjco.v8.i4.366
Pulmonary artery intimal sarcoma (PAIS) is a rare tumor first described by Mandelstamm[1] in 1923. Since then, about 300 cases have been reported in the literature[2,3]. The prognosis is generally poor, with a median overall survival of approximately 17 mo[2-4]. Clinical and radiological findings usually mimic thromboembolic disease, leading to diagnostic delays[5]. Surgical resection of the primary tumor is the best therapeutic option to prolong survival and adjuvant chemotherapy and radiotherapy have limited results[2,3]. The treatment of choice is surgery, as adjuvant chemotherapy and radiotherapy have limited results. When metastases occur, they may be resected in specific patients[6,7]. Otherwise, treatment is generally systemic and palliative in nature. In recent years, stereotactic body radiation therapy (SBRT) for lung metastases, a high-precision external radiotherapy technique, alternative to metastasectomy, has undergone significant development. Prospective phase I/II studies have shown that SBRT is safe and effective as treatment of lung metastases in oligometastatic patients who are not candidates for surgery[8,9]. SBRT of inoperable lung metastases is today considered routine in many centers. We report the case of a rapidly metastatic PAIS, with sustained complete remission following surgical resection and SBRT.
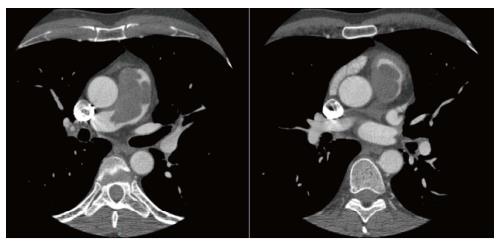
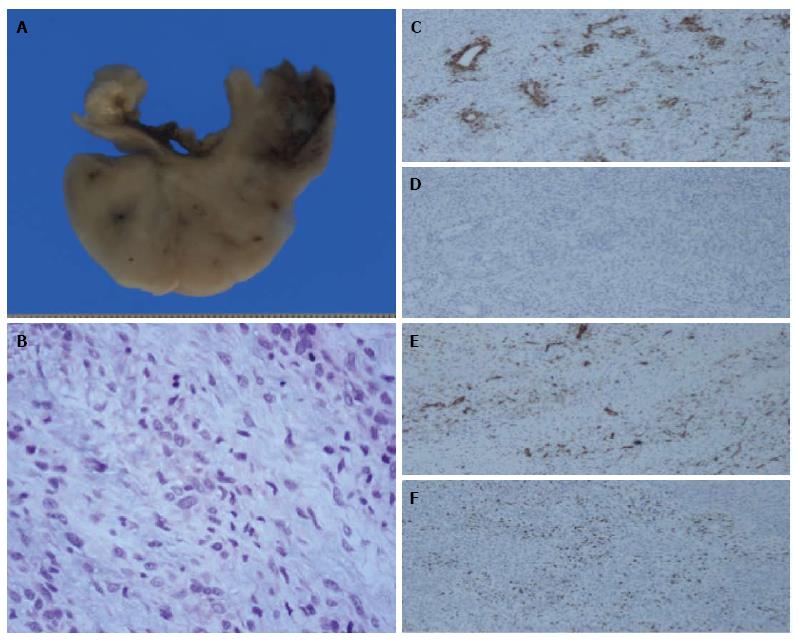
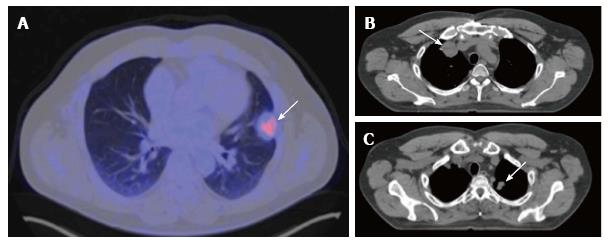
A 48-year-old male patient presenting with sudden-onset symptoms of sweating, dizziness and falling to the ground, with loss of consciousness, and spontaneous recovery. After observing electrocardiographic changes, he was hospitalized with suspected acute coronary syndrome. An angio-computed tomography (CT) was performed, resulting in a diagnosis of pulmonary thromboembolism, with no improvement after anticoagulant therapy. The patient was transferred to our hospital, where a repeat angio-CT was performed, revealing a filling defect in the pulmonary artery trunk, extending from the subvalvular area to the origin of the right pulmonary artery, with no change in size with respect to the previous angio-CT (Figure 1). The patient was operated on for a suspected primary tumor of the pulmonary artery, resulting in with complete resection of the mass, whose pathological result was an intermediate-grade malignant tumor suggestive of PAIS (Figure 2). Following an extension study, CT showed only a nonspecific pulmonary nodule of 4 mm in diameter in the right upper lobe. No adjuvant treatment was given. Three months later, a positron emission tomography-computed tomography (PET-CT) found that the previously mentioned nodule measured 6 mm, suggestive of metastasis. Another 4 mm de novo nodule was found and two more of 2-3 mm in size, possibly granulomas, all without an increase in metabolic activity. The patient underwent surgery where 4 bilateral pulmonary lesions, compatible with metastasis, were resected. Fifteen months later, a new PET-CT reveals a subpleural nodule in the left upper lobe, again suspicious of metastasis (Figure 3A), as well as several millimeter-size nodules reported in the previous CT, not metabolically characterizable. After discussion in a multidisciplinary committee, the patient was given treatment with SBRT (12 Gy × 5 fractions), with excellent control. Six months later, growth of the two new pulmonary lesions noted in the previous CT was observed (Figure 3B and C). Chemotherapy was prescribed, which was rejected by the patient, and a second course of SBRT was given on both pulmonary lesions. Nine months after SBRT, the patient is disease-free by PET-CT.
PAIS is characterized by insidious growth, causing extensive local invasion and hematogeneous metastases. Because it is a rare tumor, only case reports and small case series have been published, most of them focused on the histopathological findings and surgical aspects of its management[3,4,10-12]. Few patients achieve long-term survival and they are those without disease dissemination. The largest analysis of outcomes of this tumor reported better median survival of patients who received multimodality treatment with respect those who had single treatment (median survival of 24.7 and 8.0 mo, respectively). However, single treatment was defined as either surgery, chemotherapy or radiotherapy alone, instead of surgery without postoperative treatment[2]. Mussot et al[3] described a surgical series of 31 patients. They concluded that there appeared to be no statistical survival benefit in those who received adjuvant treatment compared to those who did not. A recent study[4] analyzed 20 patients diagnosed with PAIS obtaining a median overall survival of 17 mo: Patients who received postoperative chemo and radiotherapy showed a trend towards better survival compared to those who had surgery alone (24 mo vs 8 mo, P = 0.3417). Successful cases reported in metastatic patients are anecdotal. Thus, Said et al[13] reported a case of pulmonary artery angiosarcoma, with a follow-up of 5 years and multiple repeat lung metastasectomies, which has a disease-free interval of 1 year. Choi et al[14] published a case of PAIS with metastases in the thyroid and adrenal glands, 4.7 and 6.3 years, respectively, after initial surgery. Both metastases were surgically resected, with an unusual survival of 12.5 years up to the last follow-up. In our case, dissemination occurred much earlier, as the patient was operated on for lung metastases 5 mo after the initial surgery, though it is likely that patient was already metastatic at diagnosis. He is currently disease-free, 4 years after diagnosis. To our knowledge, this is the first published case of metastatic PAIS with long-term survival treated with surgery and SBRT.
In conclusion, SBRT proved to be an alternative treatment to metastasectomy, allowing palliative chemotherapy to be delayed or omitted, which may result in improved quality of life.
A 48-year-old male presenting sudden-onset symptoms of sweating, dizziness and fall, with momentary loss of consciousness.
Acute coronary syndrome.
Thromboembolic disease.
Angio-computed tomography: Filling defect in the pulmonary artery trunk, extending from the subvalvular area to the origin of the right pulmonary artery.
Intermediate-grade malignant tumor suggestive of pulmonary artery intimal sarcoma.
The patient underwent surgery. The tumor progressed rapidly in the lung, requiring surgery of multiple lung metastases. Finally, he was treated with stereotactic body radiation therapy on two occasions for new pulmonary lesions.
This case report describes a uncommon patient with exceptional long-term survival despite having rapid metastatic progression. This case teaches us that SBRT is an alternative treatment to metastasectomy, allowing palliative chemotherapy to be delayed or omitted.
The article presents an unusual case of intimal sarcoma of the pulmonary artery. There are a small number of cases reported. This is a rare sarcoma with very good response to treatment with radiotherapy.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Bramhall S, Cerwenka HR, Peters GJ S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Mandelstamm M. Über primäre Neubildungen des Herzens. Virchows Arch Pathol Anat. 1923;245:43-54. |
| 2. | Blackmon SH, Rice DC, Correa AM, Mehran R, Putnam JB, Smythe WR, Walkes JC, Walsh GL, Moran C, Singh H. Management of primary pulmonary artery sarcomas. Ann Thorac Surg. 2009;87:977-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 175] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 3. | Mussot S, Ghigna MR, Mercier O, Fabre D, Fadel E, Le Cesne A, Simonneau G, Dartevelle P. Retrospective institutional study of 31 patients treated for pulmonary artery sarcoma. Eur J Cardiothorac Surg. 2013;43:787-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 105] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 4. | Wong HH, Gounaris I, McCormack A, Berman M, Davidson D, Horan G, Pepke-Zaba J, Jenkins D, Earl HM, Hatcher HM. Presentation and management of pulmonary artery sarcoma. Clin Sarcoma Res. 2015;5:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 5. | Jiang S, Li J, Zeng Q, Liang J. Pulmonary artery intimal sarcoma misdiagnosed as pulmonary embolism: A case report. Oncol Lett. 2017;13:2713-2716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Digesu CS, Wiesel O, Vaporciyan AA, Colson YL. Management of Sarcoma Metastases to the Lung. Surg Oncol Clin N Am. 2016;25:721-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Chudgar NP, Brennan MF, Munhoz RR, Bucciarelli PR, Tan KS, D’Angelo SP, Bains MS, Bott M, Huang J, Park BJ. Pulmonary metastasectomy with therapeutic intent for soft-tissue sarcoma. J Thorac Cardiovasc Surg. 2017;154:319-330.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 8. | Okunieff P, Petersen AL, Philip A, Milano MT, Katz AW, Boros L, Schell MC. Stereotactic Body Radiation Therapy (SBRT) for lung metastases. Acta Oncol. 2006;45:808-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 165] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 9. | Rusthoven KE, Kavanagh BD, Burri SH, Chen C, Cardenes H, Chidel MA, Pugh TJ, Kane M, Gaspar LE, Schefter TE. Multi-institutional phase I/II trial of stereotactic body radiation therapy for lung metastases. J Clin Oncol. 2009;27:1579-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 435] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 10. | Grazioli V, Vistarini N, Morsolini M, Klersy C, Orlandoni G, Dore R, D’Armini AM. Surgical treatment of primary pulmonary artery sarcoma. J Thorac Cardiovasc Surg. 2014;148:113-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 11. | Huo L, Moran CA, Fuller GN, Gladish G, Suster S. Pulmonary artery sarcoma: a clinicopathologic and immunohistochemical study of 12 cases. Am J Clin Pathol. 2006;125:419-424. [PubMed] |
| 12. | Tavora F, Miettinen M, Fanburg-Smith J, Franks TJ, Burke A. Pulmonary artery sarcoma: a histologic and follow-up study with emphasis on a subset of low-grade myofibroblastic sarcomas with a good long-term follow-up. Am J Surg Pathol. 2008;32:1751-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Said SM, Sundt TM 3rd, Garces YI, Wigle DA. 5-year survival after multiple repeat metastasectomy for pulmonary artery angiosarcoma. Ann Thorac Surg. 2011;91:e49-e51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Choi YM, Jang EK, Ahn SH, Jeon MJ, Han JM, Kim SC, Han DJ, Gong G, Kim TY, Shong YK. Long-term survival of a patient with pulmonary artery intimal sarcoma after sequential metastasectomies of the thyroid and adrenal glands. Endocrinol Metab (Seoul). 2013;28:46-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |