Published online Dec 10, 2014. doi: 10.5306/wjco.v5.i5.1113
Revised: June 24, 2014
Accepted: August 27, 2014
Published online: December 10, 2014
Processing time: 281 Days and 17.4 Hours
Pulmonary blastoma is an uncommon lung malignancy, usually presenting itself as a large chest mass causing pain, hemoptysis, cough and dyspnea; however, it is asymptomatic in up to 40% of patients. We present the case and suggestive images of a 37-year-old non-smoking lady with a monophasic pulmonary blastoma located in the lower lobe of the left lung who underwent a left posterolateral thoracotomy with lower lobectomy, hilar and mediastinal node dissection, followed by chemo and radiation therapy. After 36 mo, there is no disease progression and the patient is in good health, clinically stable and without significant chest pain.
Core tip: Pulmonary blastoma is a rare condition and diagnosis may be difficult to obtain. It is important to underline that the appropriate management of this unusual type of lesion can be achieved only by a multidisciplinary specialized team, able to plan the correct integrated strategy based on aggressive surgery and chemo-radiation therapy.
- Citation: Magistrelli P, D’Ambra L, Berti S, Bonfante P, Francone E, Vigani A, Falco E. Adult pulmonary blastoma: Report of an unusual malignant lung tumor. World J Clin Oncol 2014; 5(5): 1113-1116
- URL: https://www.wjgnet.com/2218-4333/full/v5/i5/1113.htm
- DOI: https://dx.doi.org/10.5306/wjco.v5.i5.1113
Pulmonary blastoma is an unusual lung malignancy, constituting about 0.5% of all lung tumors[1-4]. Its histology resembles lung fetal tissue and can express both epithelial and mesenchymal features. Despite its assumed embryonal origin, the tumor predominantly affects adults[3]. The literature reports a limited number of cases classified as adult type pulmonary blastoma or child pleuropulmonary blastoma[5-8].
In adults, the neoplasm generally presents itself as a large and symptomatic mass causing cough, hemoptysis, fever and chest pain.
A 37-year-old non-smoking lady was admitted to the hospital with persistent chest pain, fever and hemoptysis. The chest X-ray showed a gross opacity in the left basal pulmonary field which was first suspected to be empyema complicating a pulmonary infection.
The computed tomography scan (CT scan) revealed the presence of a ten centimeter neoplasm located in the left basal hemithorax. Bronchoscopy showed neoplastic well vascularized vegetation occluding the left lower bronchus and histology through the biopsy permitted diagnosis of a monophasic pulmonary blastoma or the so called fetal adenocarcinoma. The immunohistochemistry obtained by fine needle aspiration biopsy of the lesion under CT scan guidance confirmed the rare lung tumor.
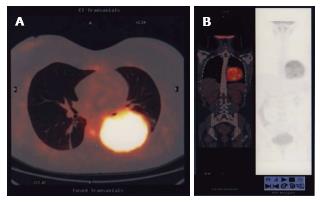
The stage was completed by a CT/positron emission tomography scan (CT/PET), showing an abnormal 18F-FDG uptake limited to the round mass with an elevated SUV of 13, a specific feature of this type of blastoma[1,9]. There was no evidence of other pathological localizations, confirming that the disease was enclosed in the left lung (Figure 1).
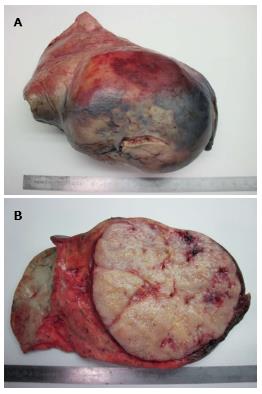
Pre-operative work-up showed no contraindications so the patient underwent surgery. We performed a left posterolateral thoracotomy with lower lobectomy and hilar and mediastinal node dissection (Figure 2).
The postoperative course was uneventful, the drains were removed three days after surgery and the patient was discharged three days later.
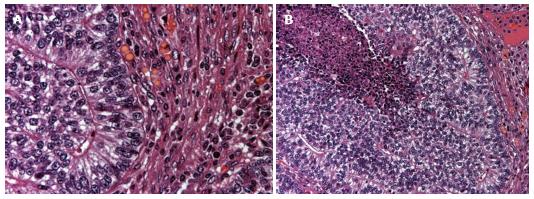
Definitive histology confirmed a pT3, pN2, M0 malignant monophasic pulmonary blastoma with only one metastatic mediastinal lymph node (Figure 3). The bronchial stump and the multiple specimens taken on the parietal and mediastinal pleura were negative.
A month later the patient was evaluated by our interdisciplinary team and was considered eligible for adjuvant chemo and radiation therapy.
Follow-up at 6, 12, 24 and 36 mo revealed no disease progression on PET/CT scan, with a serum decrease of oncological markers. The patient is now in good health, clinically stable and without significant chest pain.
Pulmonary blastoma is a rare neoplasm with distinctive biological behavior[4]. It was described for the first time in 1952 by Barnard as an “embryoma” and in 1961 was regularly classified by Spencer who established that the tumor arises from pulmonary blastema as tumors developed from fetal tissues[5,10].
The neoplasm was divided by Koss et al[11] into three groups: biphasic pulmonary blastoma, monophasic pulmonary blastoma with prevalent epithelial expression, and pleuropulmonary blastoma with mesenchymal expression[2,5,10,11].
In adults, the tumor presents itself as a large chest mass causing pain, hemoptysis, cough and dyspnea; however, up to 40% of patients may be asymptomatic[4]. Diagnosis may be difficult to obtain because of the unusual pleomorphic histology but it has to be suspected when there is cytological evidence of heterogeneity with epithelial and mesenchymal malignant cells[12-14]. The radiological appearance consists of a well-delimited circle mass ranging in size from 1.5 to 13 cm in diameter.
Surgical excision is the treatment of choice[4,15]. The prognosis reported in the literature is generally poor, with limited survival within 2-3 years from diagnosis. The difference in survival rate depends on mediastinal node involvement and over the last ten years a better prognosis has been shown with preoperative neoadjuvant chemotherapy[14,16].
In a case of N2 disease, postoperative adjuvant radiation therapy and chemotherapy based on cisplatin and etoposide are considered the treatments of choice[14,17,18].
In conclusion, adult pulmonary blastoma is an unusual lung tumor presenting itself as a large invasive mass. Diagnosis, treatment and follow-up have to be planned by a multidisciplinary team. Integrated strategy based on aggressive surgery and chemo-radiation therapy may be the best choice for a successful treatment.
A 37-year-old non-smoking lady with persistent chest pain, fever and hemoptysis.
A ten centimeter neoplasm located in the left basal hemithorax.
Empyema complicating a pulmonary infection.
A well-delimited circle mass ranging in size from 1.5 to 13 cm in diameter.
pT3, pN2, M0 monophasic pulmonary blastoma with one metastatic mediastinal lymph node.
Left posterolateral thoracotomy with lower lobectomy and hilar and mediastinal node dissection followed by chemo and radiation therapy.
The rare presentation of pulmonary blastoma can make obtaining a diagnosis difficult, so a meticulous evaluation by a multidisciplinary team is mandatory in suspected cases.
Pulmonary blastoma is a rare condition that has to be managed by a multidisciplinary team to plan the correct integrated strategy based on aggressive surgery and chemo-radiation therapy.
This is a report of a rare case of a malignant lung tumor. The presentation is simple but adequate.
P- Reviewer: Andersen PE, Pereira-Vega A, Wang HY S- Editor: Song XX L- Editor: Roemmele A E- Editor: Lu YJ
| 1. | Keu KV, Berry GJ, Quon A. Classic biphasic pulmonary blastoma demonstrated by 18F-FDG PET/CT. Clin Nucl Med. 2014;39:346-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Daghfous H, Belloumi N, Braham E, Ben Saad S, El Bay R, El Mezni F, Tritar F. [Case report of pulmonary biphasic tumor with unusual follow-up.]. Rev Pneumol Clin. 2014;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Wang YX, Zhang J, Chu XY, Liu Y, Li F, Wang ZB, Wei LX. Diagnosis and multi-modality treatment of adult pulmonary plastoma: Analysis of 18 cases and review of literature. Asian Pac J Trop Med. 2014;7:164-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Dixit R, Joshi N, Dave L. Biphasic pulmonary blastoma: An unusual presentation with chest wall, rib, and pleural involvement. Lung India. 2014;31:87-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Chen S, Wang S, Gao J, Zhang S. [Pleuropulmonary blastoma: a clinicopathological analysis]. Zhongguo Feiai Zazhi. 2010;13:550-553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Hill DA, Jarzembowski JA, Priest JR, Williams G, Schoettler P, Dehner LP. Type I pleuropulmonary blastoma: pathology and biology study of 51 cases from the international pleuropulmonary blastoma registry. Am J Surg Pathol. 2008;32:282-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 139] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 7. | Dishop MK, Kuruvilla S. Primary and metastatic lung tumors in the pediatric population: a review and 25-year experience at a large children’s hospital. Arch Pathol Lab Med. 2008;132:1079-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Sonoda LI, Wagner T, Sanghera B, Wong WL. 18F-FDG PET/CT appearances of adult pulmonary blastoma. Clin Nucl Med. 2013;38:737-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Zagar TM, Blackwell S, Crawford J, D’Amico T, Christensen JD, Sporn TA, Kelsey CR. Preoperative radiation therapy and chemotherapy for pulmonary blastoma: a case report. J Thorac Oncol. 2010;5:282-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Koss MN, Hochholzer L, O’Leary T. Pulmonary blastomas. Cancer. 1991;67:2368-2381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Wang J, Sun H, Bai R, Liu H, Yu T. Pulmonary blastoma with endobronchial growth. J Thorac Oncol. 2009;4:543-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | He W, Jiang G, Xie B, Liu M. Radical resection of a pulmonary blastoma involving the pulmonary artery. Eur J Cardiothorac Surg. 2008;34:695-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Iwata T, Nishiyama N, Inoue K, Kawata Y, Izumi N, Tsukioka T, Shinkawa K, Suehiro S. Biphasic pulmonary blastoma: report of a case. Ann Thorac Cardiovasc Surg. 2007;13:40-43. [PubMed] |
| 15. | Mistry JH, Pawar SB, Mehta H, Popov AF, Mohite PN. Primary pulmonary blastoma of monophasic variety--diagnosis and management. J Cardiothorac Surg. 2013;8:144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Liman ST, Altinok T, Topcu S, Tastepe AI, Uzar A, Demircan S, Demirag F. Survival of biphasic pulmonary blastoma. Respir Med. 2006;100:1174-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Schulze SM, Sbayi S, Costic JT, Moser RL. A rare case of classic biphasic pulmonary blastoma. Am Surg. 2005;71:1078-1081. [PubMed] |
| 18. | Walker RI, Suvarna K, Matthews S. Case report: pulmonary blastoma: presentation of two atypical cases and review of the literature. Br J Radiol. 2005;78:437-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |