Published online Nov 10, 2013. doi: 10.5306/wjco.v4.i4.102
Revised: September 17, 2013
Accepted: October 19, 2013
Published online: November 10, 2013
Processing time: 140 Days and 21.3 Hours
Pulmonary artery sarcoma (PAS) is a rare and lethal neoplasm that is usually diagnosed during surgery or autopsy. Early diagnosis and radical surgical resection offer the only chance for survival. However, making a preoperative histopathological diagnosis is quite difficult. We encountered a 57-year-old woman presenting a PAS that mimicked a pulmonary thromboembolism. After confirming a definitive diagnosis using a catheter suction biopsy, we successfully performed a right pneumonectomy via a median sternotomy without cardiopulmonary bypass. Eighteen months after surgery, no recurrence was observed.
Core tip: Pulmonary artery sarcoma (PAS) is a rare and lethal neoplasm that is and usually diagnosed during surgery or autopsy. Early diagnosis and radical surgical resection offer the only chance for survival. However, preoperative histopathological diagnosis is quite difficult owing to the location of the tumor and its rarity. We report a 57-year-old woman patient for whom a preoperative definitive diagnosis of PAS was obtained using catheter-suction biopsy and describe how we successfully performed a curative right pneumonectomy via a median sternotomy without cardiopulmonary bypass. Eighteen months after surgery, no recurrence was observed.
- Citation: Fukai R, Rokkaku K, Irie Y, Imazeki T, Katada Y, Watanabe H, Ueda Y, Miyamoto H, Chida M. Pulmonary artery sarcoma successfully treated by right pneumonectomy after definitive diagnosis. World J Clin Oncol 2013; 4(4): 102-105
- URL: https://www.wjgnet.com/2218-4333/full/v4/i4/102.htm
- DOI: https://dx.doi.org/10.5306/wjco.v4.i4.102
Pulmonary artery sarcoma (PAS) is a rare tumor that is generally considered fatal and is often misdiagnosed as a pulmonary embolism (PE)[1]. This misdiagnosis contributes to its poor prognosis, as it delays making the correct diagnosis and administering the appropriate treatment. Only a few hundred cases have been reported[2], following the first description by Mandelstamm in 1923[3]. Early diagnosis and radical surgical resection offer the only chance for survival, but owing to the location of the tumor and its rarity, preoperative histopathological PAS diagnosis has seldom been reported[4,5]. We report a patient for whom a preoperative definitive diagnosis of PAS was obtained using catheter-suction biopsy and describe how we successfully performed a curative right pneumonectomy.
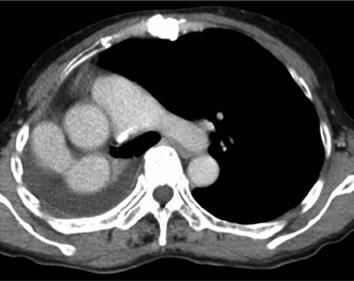
A 57-year-old female was referred to our hospital with an abnormal shadow on chest radiography and a history of chest pain, dyspnea, malaise, and fever. Her medical history included osteoporosis and scoliosis. Laboratory test results revealed a mild impairment of liver function, elevation of biliary enzymes and moderate increase of the erythrocyte sedimentation rate. A remarkable prolongation of the activated partial thromboplastin time (180/30.5 s) and a slight acceleration of the fibrinogen (618 mg/dL) and fibrin degradation products (6.4 μg/mL), as well as D-dimer (2.50 μg/mL), were also detected. She was initially diagnosed with a pulmonary embolism according to the enhanced computed tomography (CT) findings and underwent thrombolytic therapy with the placement of an inferior vena cava (IVC) filter. However, her symptoms and CT findings did not improve with treatment (Figure 1), and the IVC filter was retrieved. Moreover, positron emission tomography-computed tomography (PET/CT) revealed moderate 18F-fluorodeoxyglucose uptake in the pulmonary embolism. We then considered the possibility of PAS and performed a pulmonary angiography, which revealed a filling defect occupying the entire luminal diameter of the right main pulmonary artery at the base of the truncus anterior (Figure 2). We performed intravenous catheter-suction biopsy using a 9 F multipurpose-guiding catheter (Vista Brite Tip®, Cordis Corporation, East Bridgewater, NJ) and a 50 mL syringe at the right peripheral pulmonary artery. The proximal portion of the lesion, which mostly consisted of a blood clot, was too soft to perform a traditional biopsy. Pathology revealed a few atypical spindle cells in a large volume of clotted blood; according to these results, the lesion was definitively diagnosed as PAS. While awaiting surgery, the patient had a recurrence of chest pain and fever; we suspected that these symptoms were due to a repeat pulmonary infarction and that her initial symptoms indicated a prior infarction. We therefore performed lung perfusion scintigraphy. Compared with a previous examination performed 1.5 mo prior, the findings were obviously worsened: the right lung was not visualized on the scan (Figure 3).
We performed a right pneumonectomy through a median sternotomy, which is suitable for exposing the right main pulmonary artery between the ascending aorta and the superior vena cava without using an artificial cardiopulmonary machine. We transected the pulmonary artery after double-stapling at its origin, and the right main bronchus was also stapled at this location. The pulmonary veins in the right thoracic cavity were stapled. We did not carry out mediastinal lymph node dissection.
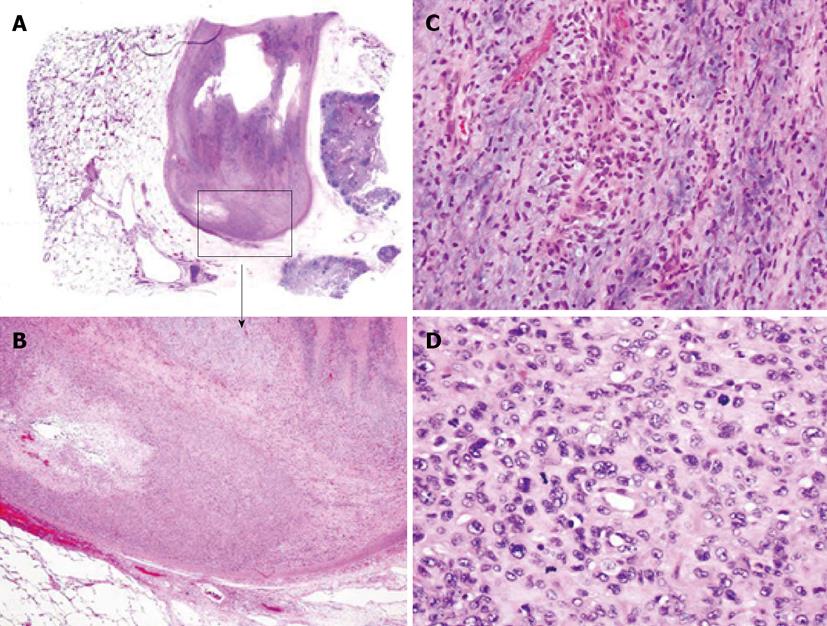
Macroscopically, a yellowish-white tumor was observed within the lumen of the right pulmonary artery, and diffuse lung congestion was noted. Microscopic examination revealed many atypical polymorphic spindle cells in the lumen of the pulmonary artery; the pathological diagnosis was intimal sarcoma of the pulmonary artery (Figure 4). The postoperative course of the patient was uneventful, and she was discharged 10 d after surgery. Eighteen months later, no evidence of recurrence was observed on CT angiography (Figure 5).
PAS is an extremely rare and usually lethal neoplasm that is most commonly diagnosed during surgery or autopsy. It is often misdiagnosed as PE[1], and its prognosis is very poor, partially due to this misdiagnosis precluding more rapid treatment. Because the tumor always arises from the central pulmonary arteries, preoperative histopathological diagnosis is quite difficult and has only rarely been reported[4,5]. We used transvenous catheter-suction biopsy that required repeated suction attempts using a syringe during pulmonary angiography because few tumor cells were present within an area of extensive coagulation. With a definitive diagnosis, we successfully performed a curative right pneumonectomy, and the patient has been in good health without recurrence for 1 year and 6 mo after surgery.
There are a few reasons why we chose right pneumonectomy as the curative operation for this patient. The first was the deterioration of her right lung, with a diffuse right lung infarction that had been ongoing for almost 1 year. The patient had gradually become accustomed to this cardiopulmonary status, with a narrowing of the right thorax already having occurred by the time she was referred to our hospital. We therefore decided that right pneumonectomy would be reasonable for this patient. We also thought that right pneumonectomy was necessary to achieve complete tumor resection, as tumor cells may have existed in the distal pulmonary artery-lumen coagulation. Gan et al[6] reported that patients with PAS who undergo distal embolectomy live longer than patients who do not, suggesting that PAS tumor cells exist in the distal pulmonary artery thrombi.
Differentiating between PAS and PE is extremely difficult. Our strongest reason for suspecting PAS was the enlargement of the pulmonary artery diameter on CT, which increased despite anticoagulant therapy. Yi et al[7] evaluated 7 patients with PAS and reported that CT can help differentiate PAS from PE by indicating a low-attenuation filling defect that occupies the entire luminal diameter of the proximal or main pulmonary artery in PAS. This finding was observed in all 7 patients (100%), and expansion of any segment of the pulmonary artery, with an extensive intraluminal filling defect, was observed in 6 of the 7 patients (86%). Moreover, Cox et al[2] described that the presence of a hilar mass causing unilateral enlargement of the pulmonary artery and proximal branches is specific to pulmonary artery sarcoma. Unilateral central embolus is uncommon. In patients diagnosed with PE, the possibility of PAS should be considered if a unilateral widened diameter of the pulmonary artery and/or a low-attenuation filling defect occupying the entire luminal diameter at the level of the main or proximal pulmonary artery is present.
In our patient, the 2 bouts of back pain and high fever were thought to be due to a major pulmonary infarction. The visible progression of her disease on lung perfusion scintigraphy over a 1.5-mo period was valuable in the decision of the appropriate pulmonary-artery transection site through a median sternotomy. If a patient presents suspicious symptoms that might indicate advancing PAS, clinicians should not hesitate to carry out additional examinations.
In a conclusion, PAS is a rare, life-threatening tumor that arises from the pulmonary artery and its proximal branches. The most effective treatment (and the best chance for survival) is radical surgery. We treated a patient with PAS using a right pneumonectomy after making a definitive diagnosis using catheter suction biopsy. The patient is alive and well, 18 mo after surgery.
We are grateful to Dr. Y Kawabata at the Saitama Cardiovascular and Respiratory Center for specialized pathological guidance.
P- Reviewer: Lee JS S- Editor: Wen LL L- Editor: A E- Editor: Liu XM
| 1. | Hoeper MM, Mayer E, Simonneau G, Rubin LJ. Chronic thromboembolic pulmonary hypertension. Circulation. 2006;113:2011-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Cox JE, Chiles C, Aquino SL, Savage P, Oaks T. Pulmonary artery sarcomas: a review of clinical and radiologic features. J Comput Assist Tomogr. 1997;21:750-755. [PubMed] |
| 3. | Mandelstamm M. uber primare Neubildungen des Herzens. Virchows Arch. 1923;245:43-54. |
| 4. | Yamada N, Kamei S, Yasuda F, Isaka N, Yada I, Nakano T. Primary leiomyosarcoma of the pulmonary artery confirmed by catheter suction biopsy. Chest. 1998;113:555-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Velebit V, Christenson JT, Simonet F, Maurice J, Schmuziger M, Hauser H, Didier D. Preoperative diagnosis of a pulmonary artery sarcoma. Thorax. 1995;50:1014-1015; discussion 1016-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Gan HL, Zhang JQ, Zhou QW, Xiao W, Gao YM, Liu S, Wang PS. Surgical treatment of pulmonary artery sarcoma. J Thorac Cardiovasc Surg. 2011;142:1469-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Yi CA, Lee KS, Choe YH, Han D, Kwon OJ, Kim S. Computed tomography in pulmonary artery sarcoma: distinguishing features from pulmonary embolic disease. J Comput Assist Tomogr. 2004;28:34-39. [PubMed] |