Published online Jun 10, 2012. doi: 10.5306/wjco.v3.i6.92
Revised: May 12, 2012
Accepted: June 5, 2012
Published online: June 10, 2012
Primary natural killer/T-cell (NK/T-cell) lymphoma of the gastrointestinal tract is a very rare disease with a poor prognosis, and the duodenum is quite extraordinary as a primary lesion site. Here, we describe a unique case of a primary duodenal NK/T-cell lymphoma in a 26-year-old man who presented with abdominal pain and weight loss. Abdominal computed tomography scan demonstrated a hypodense tumor in the duodenum. Because of massive upper gastrointestinal tract bleeding during hospitalization, the patient was examined by emergency upper gastrointestinal endoscopy. Under endoscopy, an irregular ulcer with mucosal edema, destruction, necrosis, a hyperplastic nodule and active bleeding was observed on the duodenal posterior wall. Following endoscopic hemostasis, a biopsy was obtained for pathological evaluation. The lesion was subsequently confirmed to be a duodenal NK/T-cell lymphoma. The presenting symptoms of primary duodenal NK-/T-cell lymphoma in this patient were abdominal pain and gastrointestinal bleeding, and endoscopy was important for diagnosis. Despite aggressive treatments, the prognosis was very poor.
- Citation: Li JZ, Tao J, Ruan DY, Yang YD, Zhan YS, Wang X, Chen Y, Kuang SC, Shao CK, Wu B. Primary duodenal NK/T-cell lymphoma with massive bleeding: A case report. World J Clin Oncol 2012; 3(6): 92-97
- URL: https://www.wjgnet.com/2218-4333/full/v3/i6/92.htm
- DOI: https://dx.doi.org/10.5306/wjco.v3.i6.92
Lymphoma is a heterogeneous disease as there is a great variety in the biology of normal lymphocytes and clinical behavior is different. The World Health Organization classification divides lymphoma biologically into B cell and T cell/natural killer (NK) cell lineages which are commonly called non-Hodgkin’s lymphoma (NHL). The incidence of the various subtypes varies widely as some lesions appear to be peculiar to particular sites and ethnic groups[1]. Primary NHL of the duodenum is an uncommon primary tumor of the gastrointestinal tract which accounts for less than 12% of all NHL[2,3]. The majority of these lymphomas arise in the stomach, with less than 30% arising in the small intestine[3]. The incidence of lymphoma decreases from the ileum to the jejunum to the duodenum[1]. The NK cell type can be classified into 3 subgroups: NK/T-cell lymphoma nasal/nasal type, NK cell leukemia and chronic lymphoproliferative disorders of NK cells[4,5]. Of the NHL subtypes, NK/T-cell lymphoma nasal type is very rare, predominantly found in East Asia, and there it makes up 2%-10% of NHL[6]. It is primarily located in the nasal/nasopharyngeal region (75%), the skin (4%), the gastrointestinal tract (6%), the bone marrow and the spleen[7]. NK/T-cell lymphomas in the gastrointestinal tract, especially those occurring in the duodenum, are rare. Herein, we report a rare case of primary duodenal NK/T-cell lymphoma with massive bleeding.
A 26-year-old man was admitted to our hospital due to a 2 mo history of abdominal pain with weight loss. He had a medical history of hyperlipidemia and hypertension, but denied history of alcohol consumption or drug abuse. Both his grandfather and uncle had a history of pulmonary tuberculosis (TB). Two months prior to admission, he developed symptoms of early satiety, poor appetite, and abdominal fullness. Thereafter, he developed a dry cough, malaise, and dyspnea on exertion. Low fever, night sweats, and a 14 kg weight loss were also noted during this period. On physical examination, his chest showed bilateral decreased breath sounds at the lung bases. His abdomen was hard and tender without organomegaly. Shifting dullness and rebound tenderness were also noted. Enlargement of the cervical or axillary lymph nodes were identified. Laboratory tests revealed the presence of occult blood in his stools, microcytic anemia (Hb: 11.1 g/dL, normal 13.1-17.2 g/dL), and hypoalbuminemia (albumin: 2.3 g/dL, normal 3.6-5.1 g/dL). The white blood cell count, platelet count, results of coagulation studies, liver and renal function tests, and levels of electrolytes were normal. The fecal occult blood test using an enzyme immunoassay was 214.6 ng/mL (normal, < 12 ng/mL).
A chest radiograph and thoracic ultrasonography revealed bilateral moderate pleural effusions. Abdominal ultrasonography demonstrated thickened peritoneum with a moderate amount of ascites without liver cirrhosis. Diagnostic paracentesis and thoracocentesis both yielded exudative fluid that predominantly contained mononuclear cells. The serum level of CA-125 was 727.2 U/mL (normal, < 35 U/mL), while the serum carcinoembryonic antigen and CA-199 levels were within the normal range. Serum anti-immunodeficiency virus was negative. The level of CA-125 in the ascitic fluid was markedly elevated at 2008.5 U/mL. Although the results of acidfast staining tests were negative in the ascites and pleural effusions, TB peritonitis was initially suspected on the basis of the patient’s symptoms, and elevated CA-125 level in the serum and ascites. However, the adenosine deaminase level in the ascitic fluid was 30 U/mL. In addition, TB-PCR and TB culture of ascitic fluid yielded negative findings. Analysis of ascites did not reveal growth of common microorganisms or the presence of malignant cells.
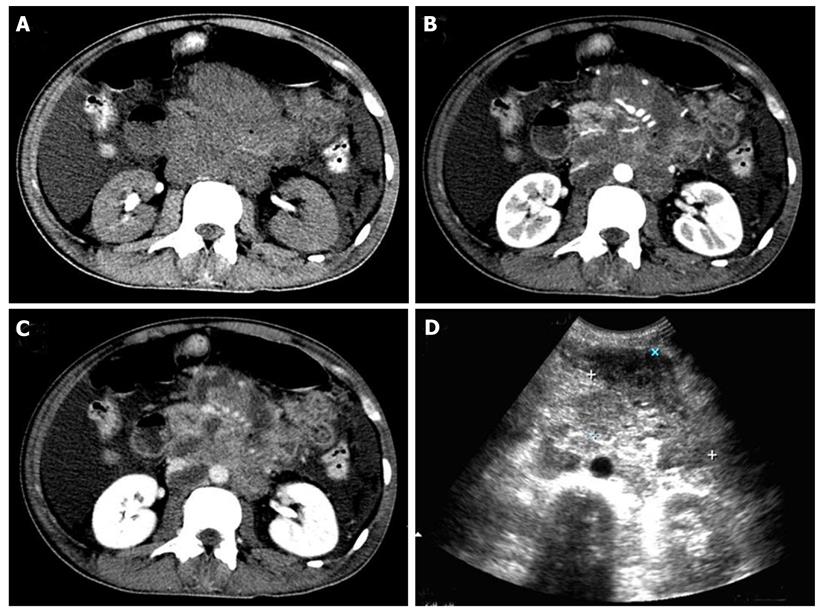
Abdominal computed tomography scan revealed multiple enlarged retroperitoneal lymph nodes, surrounding the abdominal blood vessels and organs (Figure 1A-C). Abdominal ultrasonography examination indicated a cavitary mass between the distal jejunum and proximal ileum (Figure 1D). A barium study of the small intestine also showed a cavitary mass lesion with mucosal destruction between the distal jejunum and proximal ileum, and focal segmental jejunal wall rigidity with loss of mucosal folds (data not shown). Bone marrow laboratory testing showed tumor infiltration.
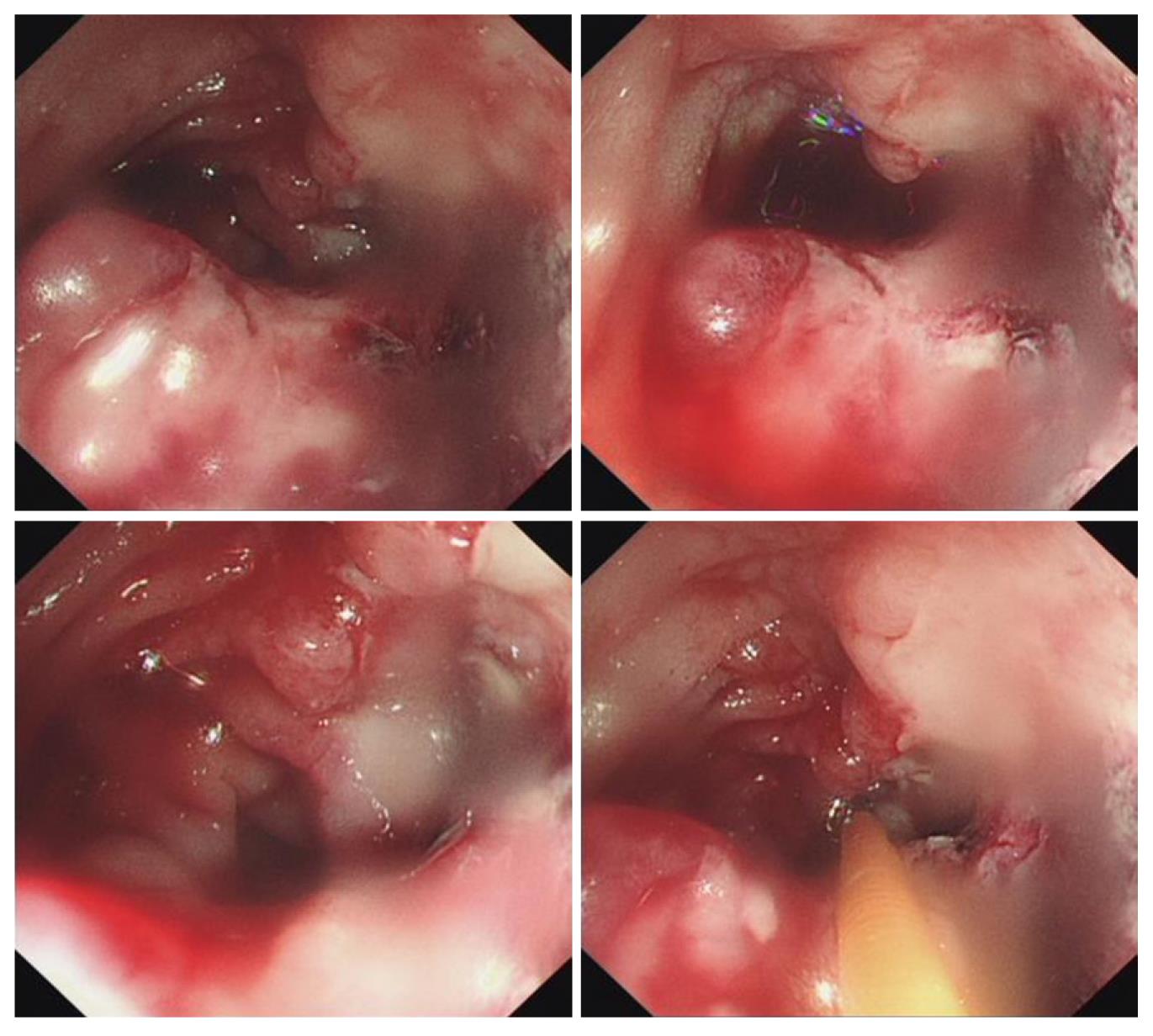
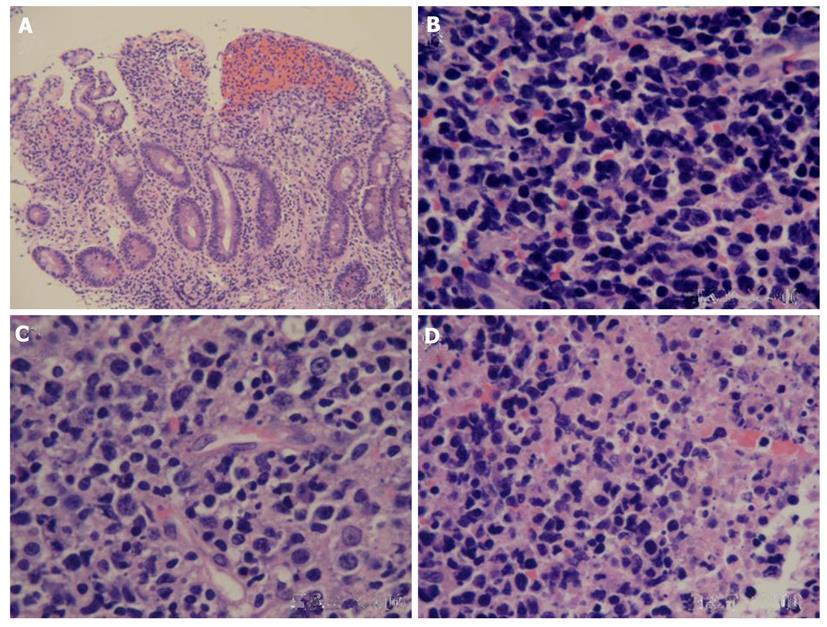
After two weeks of hospitalization, abdominal pain progressed markedly within a few days, with the development of hematemesis and melena. Thus, emergency upper gastrointestinal endoscopy was carried out in our endoscopy unit. The upper gastrointestinal endoscopy showed a large amount of fresh blood in the stomach without a bleeding site or mucosal lesion. Vascular deformity and erosive or active ulcers were not observed in the duodenal bulb. When the endoscope was placed in the descendent duodenum and horizontal junction, an irregular ulcer with mucosal edema, destruction, necrosis, a hyperplastic nodule and active bleeding were observed in the duodenal posterior wall (Figure 2). After endoscopic hemostasis, a biopsy was obtained for pathological evaluation. Colonoscopy showed a smooth mucosa without erosion, ulcer or neoplasm (data not shown). Microscopically, the biopsy specimens revealed a monotonous population of atypical lymphoid cells with scanty cytoplasm, mucosal glands widely spaced or lost, mucosal necrosis and hemorrhage (Figure 3). Pathologic features did not support Crohn’s disease. The immunohistochemical study was positive for CD3, CD56 and T cell intracytoplasmic antigen 1 (TIA1), but negative for CD20 and CD23 (Figure 4A-E). The in situ hybridization of Epstein-Barr virus encoded small nuclear RNAs was positive (Figure 4F). On the basis of the pathological characteristics, a diagnosis of NK/T-cell lymphoma was made. A whole body fluorodeoxyglucose (FDG) positron emission tomography scan showed intensely increased FDG uptake involving most of the intra-abdominal region (omentum/mesentary/peritoneum) and in the lumbar pre/para-vertebral region (retroperitoneal lymph nodes) (data not shown). Ann Arbor staging in this patient was stage IV. Hemorrhage was controlled following esophagogastroscopy. He received several courses of EPCOH formula chemotherapy, but died of disease progression and consequential severe infections 2 mo later.
Primary extranodal lymphomas are a heterogeneous group of diseases which have diverse etiology, pathogenesis, patterns of presentation and outcomes. The commonest site of extranodal NHL is the gastrointestinal tract, but virtually every extranodal location has been reported[8]. Of these 50%-60% occur in the stomach and 20%-30% in the small intestine. The most common site in the small intestine is the ileocecal region, and the least common site is the duodenum. The incidence of lymphoma in the gastrointestinal tract depends on the amount of lymphoid tissue present in a particular segment[9]. The most common pathology types are diffuse large B-cell lymphoma, marginal zone B cell lymphoma-mucosa associated tissue and mantle cell lymphoma[10]. As only a few gastrointestinal NK/T-cell lymphomas have been reported to date, duodenal NK/T-cell lymphoma is extremely rare.
NK/T-cell lymphoma is an aggressive malignancy with vascular destruction and tissue necrosis, and is an unusual type of NHL which is categorized as nasal and extranodal NK/T-cell lymphoma by the primary tumor lesion. The nasal cavity is the most common location, while the others show an extranodal presentation such as the skin, soft tissue, testis, lung, gastrointestinal tract, and central nervous system[5]. Lymphomas in the gastrointestinal tract are difficult to diagnose early due to their nonspecific symptoms[11]. Gastric and colonic lymphomas can be diagnosed via conventional endoscopy[12]. However, NK/T-cell lymphoma derived from the small intestine, which has a low incidence, is mostly diagnosed incidentally or when the patient presents with abdominal pain. Vigilance against “hints” of small bowel tumors and proper diagnostic tools are the key to preventing complications including perforation, massive bleeding, ileus, and to treat the disease when its spread is limited and it is easy to cure.
Most patients with gastrointestinal lymphoma present with vomiting, abdominal pain, weight loss, and fever. Other features such as early satiety, symptoms of peptic ulceration, bleeding in the form of hematemesis, melena, anemia or non-specific symptoms like loss of appetite may also be present. Bleeding duodenal ulcer is rarely a presentation of duodenal lymphoma. Cases of primary gastrointestinal lymphoma, particularly primary duodenal lymphoma can also present as jaundice. Most gastrointestinal tract lymphomas are initially asymptomatic until the tumor causes abdominal pain, abdominal mass, bleeding and obstruction. Usually, patients do not pay much attention to mild gastrointestinal tract discomfort or changes in bowel habits. The lack of specific clinical symptoms and signs probably accounts for the delay in diagnosis. In our case, as the tumor grew in the duodenum the patient experienced abdominal pain initially and the tumor was identified by endoscopy when upper gastrointestinal tract bleeding appeared. Although the diagnosis was very clear then, the disease was incurable.
In patients with primary gastrointestinal lymphoma, the overall 5-year survival rate is 47%, 5-year disease-free survival is 40%, and 79% of patients die within the first year of diagnosis. Important prognostic factors include stage of the disease, extent of surgical resection, response to treatment, serosal involvement, multimodality treatment, and performance status of the patient. Therefore, the best outcome for the patient depends on early diagnosis and treatment. The most effective standard treatment has not been established for this tumor[13-15]. A better response might be achieved in some cases with accurate diagnosis in the early stage (stage I/II), after intensive systemic chemotherapy-assisted radiotherapy. In summary, the presenting symptoms of primary duodenal NK-/T-cell lymphoma in our patient were abdominal pain and gastrointestinal bleeding. The duodenal NK-/T-cell lymphoma was endoscopically characterized by mucosal superficial erosion, irregular ulcer, edema, destruction, necrosis, a hyperplastic nodule and active bleeding.
Peer reviewers: Luis F Porrata, MD, Assistant Professor, Department of Hematology and Internal Medicine, Mayo Clinic, 200 First Street SW, Rochester, MN 55905, United States; Luca Arcaini, MD, Assistant Professor, Department of Oncohematology, Division of Hematology, Fondazione IRCCS Policlinico San Matteo, University of Pavia, Viale Golgi 19, 27100 Pavia, Italy
S- Editor Yang XC L- Editor Webster JR E- Editor Yang XC
| 1. | Hansen PB, Vogt KC, Skov RL, Pedersen-Bjergaard U, Jacobsen M, Ralfkiaer E. Primary gastrointestinal non-Hodgkin's lymphoma in adults: a population-based clinical and histopathologic study. J Intern Med. 1998;244:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Muchmore JH, Haddad CG, Goldwag S. Primary non-Hodgkin's lymphoma of the duodenum. Am Surg. 1994;60:924-928. [PubMed] |
| 3. | Tari A, Asaoku H, Kunihiro M, Tanaka S, Fujihara M, Yoshino T. Clinical features of gastrointestinal follicular lymphoma: comparison with nodal follicular lymphoma and gastrointestinal MALT lymphoma. Digestion. 2011;83:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Semenzato G, Marino F, Zambello R. State of the art in natural killer cell malignancies. Int J Lab Hematol. 2012;34:117-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Chan JKC, Quintanilla-Martinez L, Ferry JA, Peh SC. Extra-nodal NK/T-cell lymphoma nasal type. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon, France: IARC; 2008; 285-288. |
| 6. | Wu X, Li P, Zhao J, Yang X, Wang F, Yang YQ, Fang F, Xu Y, Zhang H, Wang WY. A clinical study of 115 patients with extranodal natural killer/T-cell lymphoma, nasal type. Clin Oncol (R Coll Radiol). 2008;20:619-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 83] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 7. | Ko YH, Ree HJ, Kim WS, Choi WH, Moon WS, Kim SW. Clinicopathologic and genotypic study of extranodal nasal-type natural killer/T-cell lymphoma and natural killer precursor lymphoma among Koreans. Cancer. 2000;89:2106-2116. [PubMed] |
| 8. | Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol. 2011;17:697-707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 245] [Cited by in RCA: 265] [Article Influence: 18.9] [Reference Citation Analysis (3)] |
| 9. | Bandyopadhyay SK, Moulick A, Dutta A. Primary duodenal lymphoma producing obstructive jaundice. J Assoc Physicians India. 2007;55:76-77. [PubMed] |
| 10. | Radić-Kristo D, Planinc-Peraica A, Ostojić S, Vrhovac R, Kardum-Skelin I, Jaksić B. Primary gastrointestinal non-Hodgkin lymphoma in adults: clinicopathologic and survival characteristics. Coll Antropol. 2010;34:413-417. [PubMed] |
| 11. | Kala Z, Válek V, Kysela P, Svoboda T. A shift in the diagnostics of the small intestine tumors. Eur J Radiol. 2007;62:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Kakimoto K, Inoue T, Nishikawa T, Ishida K, Kawakami K, Kuramoto T, Abe Y, Morita E, Murano N, Toshina K. Primary CD56+ NK/T-cell lymphoma of the rectum accompanied with refractory ulcerative colitis. J Gastroenterol. 2008;43:576-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Jaccard A, Hermine O. Extranodal natural killer/T-cell lymphoma: advances in the management. Curr Opin Oncol. 2011;23:429-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Shimada K, Suzuki R. Concurrent chemoradiotherapy for limited-stage extranodal natural killer/t-cell lymphoma, nasal type. J Clin Oncol. 2010;28:e229; author reply e230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Li YX, Yao B, Jin J, Wang WH, Liu YP, Song YW, Wang SL, Liu XF, Zhou LQ, He XH. Radiotherapy as primary treatment for stage IE and IIE nasal natural killer/T-cell lymphoma. J Clin Oncol. 2006;24:181-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 280] [Article Influence: 14.7] [Reference Citation Analysis (0)] |