Published online Apr 10, 2012. doi: 10.5306/wjco.v3.i4.57
Revised: February 15, 2012
Accepted: April 1, 2012
Published online: April 10, 2012
AIM: To prospectively compare volumetric intensity-modulated arc therapy (VMAT) and conventional intensity-modulated radiation therapy (IMRT) in coverage of planning target volumes and avoidance of multiple organs at risk (OARs) in patients undergoing definitive chemoradiotherapy for advanced (stage III or IV) squamous cell cancer of the head and neck.
METHODS: Computed tomography scans of 20 patients with advanced tumors of the larynx, naso-, oro- and hypopharynx were prospectively planned using IMRT (7 field) and VMAT using two arcs. Calculated doses to planning target volume (PTV) and OAR were compared between IMRT and VMAT plans. Dose-volume histograms (DVH) were utilized to obtain calculated doses to PTV and OAR, including parotids, cochlea, spinal cord, brainstem, anterior tongue, pituitary and brachial plexus. DVH’s for all structures were compared between IMRT and VMAT plans. In addition the plans were compared for dose conformity and homogeneity. The final treatment plan was chosen by the treating radiation oncologist.
RESULTS: VMAT was chosen as the ultimate plan in 18 of 20 patients (90%) because the plans were thought to be otherwise clinically equivalent. The IMRT plan was chosen in 2 of 20 patients because the VMAT plan produced concentric irradiation of the cord which was not overcome even with an avoidance structure. For all patients, VMAT plans had a lower number of average monitor units on average (MU = 542.85) than IMRT plans (MU = 1612.58) (P < 0.001). Using the conformity index (CI), defined as the 95% isodose volume divided by the PTV, the IMRT plan was more conformal with a lower conformity index (CI = 1.61) than the VMAT plan (CI = 2.00) (P = 0.003). Dose homogeneity, as measured by average standard deviation of dose distribution over the PTV, was not different with VMAT (1.45 Gy) or IMRT (1.73 Gy) (P = 0.069). There were no differences in sparing organs at risk.
CONCLUSION: In this prospective study, VMAT plans were chosen over IMRT 90% of the time. Compared to IMRT, VMAT plans used only one third of the MUs, had shorter treatment times, and similar sparing of OAR. Overall, VMAT provided similar dose homogeneity but less conformity in PTV irradiation compared to IMRT. This difference in conformity was not clinically significant.
-
Citation: Fung-Kee-Fung SD, Hackett R, Hales L, Warren G, Singh AK. A prospective trial of volumetric intensity-modulated arc therapy
vs conventional intensity modulated radiation therapy in advanced head and neck cancer. World J Clin Oncol 2012; 3(4): 57-62 - URL: https://www.wjgnet.com/2218-4333/full/v3/i4/57.htm
- DOI: https://dx.doi.org/10.5306/wjco.v3.i4.57
Radiation therapy is a mainstay of treatment for both early and advanced stage head and neck cancer. Traditional head and neck conformal radiation therapy, in addition to problems related to matching of multiple beams, was often associated with multiple toxicities including xerostomia (dry mouth) dysgeusia, hearing loss, brain necrosis, osteonecrosis of the mandible. To minimize the difficulties of matching multiple beams and ameliorate toxicities, radiation therapy for most head and neck cancer has shifted away from traditional conformal techniques (3DCRT) to fixed-angle intensity modulated radiation therapy (IMRT). IMRT uses multiple intensity-modulated beams to deliver non-uniform dose to the target. Beam modulation is created using a multi-leaf collimator (MLC). Superimposing numerous small beams produces a dose distribution with better target dose conformity and better sparing of critical structures than 3DCRT. IMRT allows the ability to escalate the target volume dose while reducing the dose to surrounding normal tissue and sparing organs at risk (OAR). Disadvantages of fixed angle IMRT compared to conformal therapy include: longer radiation delivery time and increased patient exposure to low dose radiation.
Recently, a new version of IMRT, volumetric modulated arc therapy (VMAT) has been developed. In VMAT, instead of using multiple fixed fields, the radiation is delivered in a continuous arc as the linear accelerator rotates around the patient, while the beam is modulated via the MLC, variable dose rate and variable gantry speed. Early reports suggest that VMAT produces dose-distributions comparable to IMRT for a variety of treatment sites[1-5]. While retrospective dosimetric planning studies have compared the techniques in head and neck cancer[6-8], no prospective clinical study had been done. As part of the institutional quality assurance/quality improvement process, a prospective study comparing VMAT and IMRT plans for dose homogeneity, dose conformality and ability to spare OAR was performed among 20 consecutive patients with advanced (stage III and IV) cancers of the head and neck. The clinically superior plan was selected for treatment by the treating radiation oncologist.
In 2009, 20 consecutive patients with advanced (stage III and IV) head and neck tumors were selected for this prospective study. The study was approved by the institutional review board. Computed tomography (CT) simulation was performed with patients in the supine position, a neck cradle was used for support and Aquaplast facemask was custom fit for immobilization. CT imaging was performed from vertex to 2 cm below the clavicle in 2.5 mm-thick slices. Scans were transferred to the Eclipse treatment planning station for simultaneous planning of both IMRT and VMAT treatment plans.
The extent of the primary tumor volume was based on physical examination of the head and neck, review of video laryngoscopy, and review of available diagnostic imaging. Gross tumor volume (GTV) was defined as the primary tumor volume and involved cervical lymph nodes (based on enlargement by CT imaging or abnormal uptake of radiolabeled [18F]-2-fluoro-deoxy-D-glucose (FDG) on PET/CT imaging). All treatment plans were prescribed to at least two dose levels, a high dose (HD) and a lower, elective dose (ED). Clinical target volume receiving a high dose (CTVHD) was defined as GTV plus a 1cm margin. Clinical target volume receiving an elective dose (CTVED) consisted of clinically-negative bilateral cervical lymph nodes at risk of metastatic disease plus a 3mm margin. In select cases, when the tumor was felt to be infiltrative (endophytic) or when the border was ill defined, an intermediate volume (CTVINT) was defined slightly larger than CTVHD to prescribe an intermediate dose between the high dose and elective dose. Planning target volumes (PTVHD, PTVED, PTVINT) were defined as respective clinical target volumes (CTVHD, CTVED, CTVINT) plus a 3 mm margin for setup errors. The uninvolved cervical lymph nodes at risk were contoured as defined by the Radiation Therapy Oncology Group (RTOG) consensus guidelines[9]. Segmented OAR were the parotid glands, spinal cord, brainstem, cerebellum, cochlea, brachial plexus, anterior half of tongue.
For patients with unresected tumor, PTVHD was prescribed to a total dose of 70 Gy in 35 fractions at 2 Gy per fraction. PTVED was prescribed 56 Gy in 35 fractions at 1.6 Gy per fraction. When indicated, PTVINT was prescribed to anywhere between 60-66 Gy in 35 fractions at 1.7-1.9 Gy per fraction. For patients receiving post-operative radiation, the primary tumor bed and involved nodes (PTVHD) was prescribed to a total dose of 66 Gy in 33 fractions at 2 Gy per fraction. PTVED was prescribed to 56 Gy in 33 fractions at 1.7 Gy per fraction. Constraints for volume coverage and dose limits for OAR used for IMRT and VMAT planning are described below.
IMRT plans were generated using 7-10 non-parallel, non-coplanar fields of 6MV photons using a dynamic or sliding window technique. Optimization and dose calculations were performed with Eclipse version 8.1. The PTVs were reduced to 3 mm below the skin surface to avoid acute dermal toxicity[10]. For optimization, the objective was to achieve all of the PTV volumes to receive > 95% of the prescribed dose. Dose constraints for the OAR were as per policy of the RPCI Radiation Medicine department as guided by Emami et al[11] as shown in Table 1. After optimization, the dose calculation was performed in Eclipse with the PBC algorithm using a calculation grid of 2.5 mm. Each VMAT plan consisted of two full arcs (-179 to 180 degrees), one clockwise and the second in the counter-clockwise direction. Collimator angle was selected between 30 and 45 degrees to cover the entire PTV. Dosing objectives for the PTV and OAR were as described for IMRT planning. VMAT planning was performed in Eclipse version 8.5, using the AAA calculation algorithm, and the Progressive Resolution optimization algorithm.
| Critical structure/organ at risk | Dose (Gy) |
| Ant tongue (1/2 or 1/3) | 70 |
| Brainstem | 54 |
| Brain - 50% | 54 |
| Brachial plexus | 60 |
| Spinal cord | 45 |
| Cochlea | 30 |
| Parotid – 50% | 30 |
Calculated doses to planning target volume (PTV) and OAR were compared between IMRT and VMAT plans. Dose-volume histograms (DVH) were utilized to obtain calculated doses to PTV and OAR, including parotids, cochlea, spinal cord, brainstem, anterior tongue, pituitary and brachial plexus, and were compared between IMRT and VMAT plans. In addition the plans were compared for dose conformity and homogeneity. The conformity index (CI), defined by RTOG 90-05 as the 95% isodose volume divided by the PTVHD was used to assess plan conformity[12-13]. Dose homogeneity was measured by the average standard deviation of dose distribution over the entire PTVHD. Ultimately, the clinically superior treatment plan was selected by the radiation oncologist and the prescription dose was normalized an isodose selected by the radiation oncologist to after review of the dose coverage of the PTV.
All patients included in the study had stage III or IV head and neck cancer. All but 1 of the patients had a squamous cell carcinoma of the head and neck. One patient had adenoid cystic carcinoma. Two of 20 patients had invasive disease or other high risk features that warranted the prescription of an intermediate dose to a clinically determined intermediate volume (PTVINT) and the average prescribed dose to this volume was 61.5 Gy. This information is summarized in Table 2.
| Pt | Pathology/site/stage | HD | ID | ED | Plan | ||
| 1 | SCC | Oropharynx | T3N3 | 70 | 56 | VMAT | |
| 2 | SCC | Larynx | T4N0 | 70 | 63 | 56 | VMAT |
| 3 | SCC | Oropharynx | T2N2A | 70 | 60 | VMAT | |
| 4 | SCC | Larynx | T3N2B | 66 | 66 | VMAT | |
| 5 | SCC | Larynx | T3N2C | 70 | 56 | VMAT | |
| 6 | SCC | Oropharynx | T2N2B | 70 | 56 | VMAT | |
| 7 | SCC | Oropharynx | T3N0 | 70 | 56 | VMAT | |
| 8 | SCC | Larynx | T4N2C | 70 | 56 | VMAT | |
| 9 | SCC | Nasopharynx | T1N3 | 70 | 60 | 55 | VMAT |
| 10 | SCC | Oropharynx | T1N1 | 66 | 56 | VMAT | |
| 11 | SCC | Larynx | T3N0 | 70 | 56 | VMAT | |
| 12 | Medullary | Thyroid | T4bN1b | 66 | 66 | VMAT | |
| 13 | SCC | Oropharynx | T4N2C | 70 | 63 | VMAT | |
| 14 | SCC | Oropharynx | T2N2C | 70 | 56 | VMAT | |
| 15 | SCC | Hypopharynx | T2N3 | 70 | 56 | VMAT | |
| 16 | SCC | Oropharynx | T2N3 | 70 | 60 | VMAT | |
| 17 | SCC | Larynx | T3N0 | 70 | 56 | IMRT | |
| 18 | SCC | Oropharynx | T3N2C | 70 | 56 | IMRT | |
| 19 | SCC | Oropharynx | T3N2B | 70 | 56 | VMAT | |
| 20 | SCC | Oropharynx | T2N1 | 70 | 56 | VMAT | |
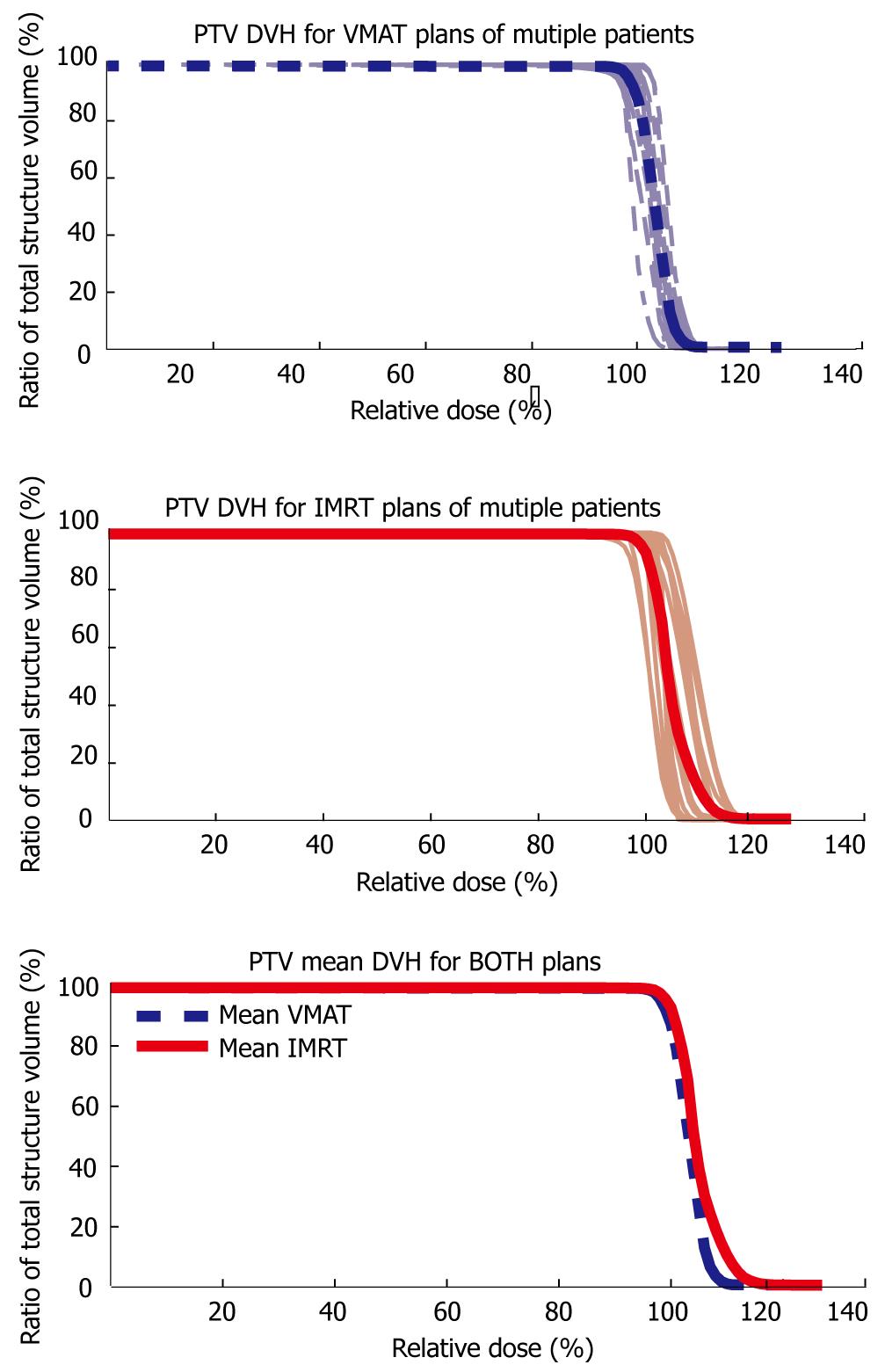
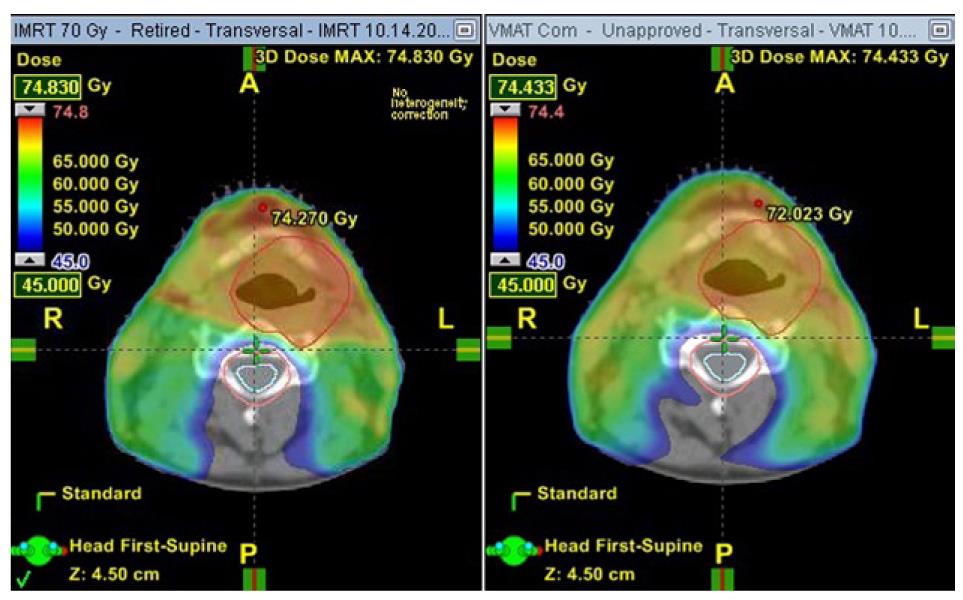
VMAT was chosen as the plan to deliver in 18 of 20 patients (90%) because the plans were deemed to be clinically superior or otherwise clinically equivalent. The IMRT plan was chosen in 2 of 20 patients because the VMAT plan produced concentric irradiation of the cord which was not overcome despite the use of a spinal cord avoidance structure. An example of a VMAT plan delivering concentric irradiation is shown in Figure 1. Table 3 summarizes the number of monitor units (MU) required by each beam or arc for each IMRT and VMAT plan respectively. For every patient, the VMAT plan had a lower number of monitor units when compared to the respective IMRT plan. Average VMAT MU = 542.85 vs IMRT MU = 1612.58 (P < 0.001). Utilizing the conformity index as a measure of plan conformity, a perfectly conformal plan is described as CI = 1. Therefore as the CI approaches 1 the plan is more conformal. In the 20 patients included in this study, the average conformity of the VMAT plans (CI = 2.00) were less conformal when compared to the average conformity of the IMRT plans (CI = 1.61). This finding was statistically significant (P = 0.003). Dose distribution over the PTVHD was on average, more homogeneous in the VMAT plans (average standard deviation of PTVHD dose = 1.45 Gy) when compared to the IMRT plans (average standard deviation of PTVHD dose = 1.73 Gy). Figure 1 shows the DVH curves for PTVHD for all patients. The mean IMRT and mean VMAT DVH curves are plotted against each other. As shown in this figure, the mean VMAT DVH has a more homogeneous dose compared to the mean IMRT DVH (as the VMAT DVH is steeper than the IMRT DVH). This finding approached, but did not meet statistical significance (P = 0.069). Table 4 summarizes the mean dose (Dmean) to each of the studied organs at risk. Statistical significant difference was noted for the cochlea, however for all other critical structures there was no clear difference in mean dose. Overall, there were no differences in sparing organs at risk.
| Monitor units | Conformity index | Dose Homogeneity | ||||
| Patient | VMAT | IMRT | VMAT | IMRT | VMAT | IMRT |
| 1 | 431 | 2211 | 1.15 | 1.19 | 2.47 | 2.59 |
| 2 | 530 | 1264 | 2.69 | 1.85 | 1.23 | 1.78 |
| 3 | 465 | 1853 | 1.74 | 1.97 | 1.31 | 2.34 |
| 4 | 584 | 1681 | 1.34 | 1.35 | 1.61 | 2.33 |
| 5 | 526 | 1423 | 1.69 | 1.38 | 1.15 | 1.95 |
| 6 | 593 | 1560 | 2.00 | 1.43 | 1.07 | 2.01 |
| 7 | 552 | 2046 | 1.79 | 1.66 | 1.08 | 2.34 |
| 8 | 522 | 1579 | 1.34 | 1.28 | 2.06 | 2.66 |
| 9 | 672 | 1473 | 1.72 | 1.70 | 0.98 | 2.46 |
| 10 | 668 | 1359 | 1.90 | 1.42 | 2.38 | 1.91 |
| 11 | 614 | 1000 | 3.07 | 1.67 | 1.05 | 0.79 |
| 12 | 533 | 2047 | 1.27 | 1.38 | 1.92 | 1.42 |
| 13 | 483 | 2087 | 1.86 | 1.58 | 1.41 | 2.05 |
| 14 | 531 | 1319 | 1.65 | 1.23 | 1.27 | 2.06 |
| 15 | 544 | 1188 | 2.41 | 1.67 | 1.58 | 1.27 |
| 16 | 520 | 1769 | 2.50 | 2.43 | 1.69 | 1.06 |
| 17 | 519 | 1114 | 3.27 | 2.39 | 1.11 | 1.19 |
| 18 | 542 | 1273 | 1.63 | 1.64 | 1.31 | 0.81 |
| 19 | 565 | 1258 | 2.16 | 1.84 | 1.44 | 1.01 |
| 20 | 463 | 1135 | 3.95 | 2.26 | 0.98 | 0.58 |
| Mean | 542.85 | 1612.58 | 2.00 | 1.61 | 1.45 | 1.73 |
| P value | < 0.001 | 0.003 | 0.069 | |||
| Mean dose (Gy) | P value | ||
| IMRT | VMAT | ||
| Ant tongue | 52.7 | 51.1 | 0.135 |
| Brainstem | 15.3 | 14.3 | 0.264 |
| Left cochlea | 23.7 | 18.8 | 0.002 |
| Right cochlea | 22.4 | 19.3 | < 0.001 |
| Left parotid | 46.8 | 46.5 | 0.68 |
| Right parotid | 47.3 | 46.7 | 0.373 |
| Spinal cord | 20.4 | 20.9 | 0.173 |
This study is the first prospective comparison of VMAT and IMRT in the actual treatment of advanced head and neck cancer patients. Ultimately, the VMAT plan was chosen for 18 of 20 (90%) patients. Compared to IMRT, VMAT plans used only one third of the MUs, had shorter treatment times, and similar sparing of OAR. Overall, VMAT plans trended towards better dose homogeneity but ultimately were found to have statistically significant less conformity in PTV irradiation compared to IMRT plans. This difference in conformality was not clinically significant.
In contrast to our prospective study which implemented the superior plan in the treatment of patients, all other reports comparing VMAT and IMRT for treatment planning in cancers of the head and neck have been retrospectively performed as theoretical exercises that were not intended to be directly implemented in patients. Overall, our results are consistent with the findings of several retrospective planning studies. Verbakel et al[7] found a statistically significant improvement in dose homogeneity with a similar compromise in conformity. However, unlike the findings reported here, Verbakel et al found an improved sparing of the parotid glands. A study by Alvarez-Moret et al[6] found comparable results between IMRT and double-arc VMAT in four patients. A third study by Bertelsen et al[8] compared IMRT to single-arc VMAT found no difference in dose homogeneity and equal or improved dose conformity with single-arc VMAT. Several of the metrics used in that study showed improved sparing of the parotids and spinal cord. The findings presented here show a significant improvement in MUs with VMAT using on average 66% of the MUs of the respective IMRT plan. A comparable reduction was shown by Verbakel et al[7] but not by Alvarez-Moret and Bertelsen. Some of these discrepancies may be explained by the fact that treatment planning was using the Eclipse planning system for a Varian linear accelerator in this study and that of Verbakel while the other two retrospective studies utilized Elekta systems.
The studies by Verbakel et al[7] and Alvarz-Monet et al[6]. compared IMRT plans with both single-arc and double-arc VMAT plans. Both reported that single-arc VMAT plans were inferior to double-arc plans and, unlike the findings of Bertelsen et al[8], single-arc VMAT plans were worse than IMRT. The double-arc plans were more comparable to IMRT plans, and as a consequence, single-arc plans were not included in this study.
In the past, some of the major issues raised with IMRT replacing the simpler 3D conformal RT plans were the more complicated treatment setup, and longer treatment times. However, the benefit to the patient in reducing xerostomia and other such side effects outweighed the drawbacks. With VMAT plans, treatment times are faster, beam-on times are shorter as evidenced by the lower number of monitor units on average with VMAT plans when compared to the IMRT plans. VMAT plans have less than a third of the number of monitor units as IMRT plans on average. This should decrease (though not eliminate) previous concerns about IMRT plans with higher monitor units leading to increased leakage radiation and increased risk of radiation induced second malignancies[14].
VMAT plans, on average, had a lower standard deviation of the dose delivered to the PTVHD when compared to the standard deviation of the IMRT plans. This is demonstrated by a steeper drop off in the DVH for the PTVHD. The VMAT plans, by virtue of a lower standard deviation, and steeper drop off, had greater dose homogeneity when compared to the IMRT plans. This result trended towards but did not achieve statistical significance likely due to the small number of patients accumulated by this study. The ability to produce a more homogenous dose could be clinically relevant, by eliminating “cold spots” within the PTV, may improve not only primary tumor control but improve loco-regional control.
However when the plans were compared for conformity, IMRT was found to be more conformal by having a lower CI when compared to VMAT plans. A review of the conformity index by Feuvret et al[15] discussed the potential inaccuracies of the conformity index as defined by the RTOG, compared to other potential formulae to define conformity. The RTOG CI was used for this study, as it is the most commonly used measure seen in the literature, and as the simplest formula, it is the easiest to conceptualize. While the flaws inherent to using a single number to the similarity between two complicated 3D shapes (PTVHD, 95% isodose volume) are obvious, the RTOG CI still provided a measure to compare the two plans. It is not clear whether a small loss of conformity between IMRT and VMAT planning is relevant to the overall clinical picture. In a review of the treatment plans, it was observed that for select patients there was spillage of the high dose well beyond the PTVHD and into the PTVED as shown in Figure 2. This overflow of dose was not observed in the respective IMRT plan. Certainly this contributes to the higher CI of the VMAT plans when compared to the IMRT plans. At this time, it is not clear why or how the optimizer allows this overflow. This is an issue that warrants further study, the results of which will be published in future follow-up study.
There was no statistically significant difference in the mean dose delivered by both plans across most OAR that were studied. Only the cochlea (both left and right) demonstrated a statistically significant improvement in sparing dose to a critical structure with VMAT when compared to IMRT. The apparent loss in conformity as described earlier does not appear to worsen the ability of VMAT to spare critical structures when compared to IMRT. From this study, VMAT does not underperform IMRT in sparing OAR and produces plans that are comparable to IMRT in sparing OAR. Based on the findings of this study, and the improvements afforded by VMAT, currently all head and neck treatment plans are initially created using VMAT. Fixed-angle IMRT was performed only when the VMAT plan was found to be clinically unacceptable. More recently, this has become an increasingly rare event. Since this initial experience with VMAT, several techniques have been utilized at our institution to eliminate some of the issues found here, and have resulted in an improvement in the conformity of the VMAT plans. These techniques will be utilized to retrospectively create new VMAT plans for the patients in this study and an update on this VMAT experience will be published in the near future.
In this prospective study, we set out to describe a single institution’s initial clinical implementation experience with VMAT compared to current standard IMRT for advanced stage head and neck carcinomas. VMAT allowed faster treatment times and used 66% lower monitor units when compared to IMRT. Analysis of the treatment plans showed that VMAT plans were less conformal than IMRT plans. This is possibly due to spillage of higher dose outside of the PTVHD and into the PTVED. The VMAT plans trended toward a more homogeneous dose, but did not meet statistical significance. OAR sparing by VMAT plans was comparable to IMRT plans. Ultimately, 90% of patients were treated with a VMAT plan that was either superior to, or comparable to its respective IMRT plan, as selected by the treating radiation oncologist.
Radiation is a fundamental aspect of definitive treatment for patients with cancers of the head and neck. In the head and neck, there are many important glands, muscles and organs in a very small space, often very close to the tumor.
Volumetric intensity modulated arc therapy (VMAT) is a recent novel advancement in the way radiation therapy is planned on the computer and delivered by the linear accelerator.
Prior studies of patients with head and neck cancer have shown excellent local control and an ability to avoid over-dosing adjacent organs at risk with conventional intensity modulated radiation therapy (IMRT). However, each treatment with IMRT can take a very long time to deliver. One of the benefits of using VMAT to deliver radiation is the ability to deliver a treatment in a much shorter time than IMRT. Dose heterogeneity was comparable, as was the sparing of critical organs at risk while delivering a treatment in a much shorter time.
This study suggests that head and neck radiation treatments previously delivered with IMRT can be delivered with VMAT, with a clinically insignificant decrease in conformity, over a much shorter treatment time. The major advantage of treatment delivery time can have theoretical improvements in patient comfort, and decreasing the risk of radiation-induced second malignancy.
Well written clinical study comparing IMRT and VMAT.
Peer reviewer: André Eckardt, MD, DDS, PhD, MBA, Associate Professor, Department of Oral and Maxillofacial Surgery, Hannover Medical School, Carl-Neuberg-Str.1, Hannover 30625, Germany
S- Editor Yang XC L- Editor A E- Editor Yang XC
| 1. | Davidson MT, Blake SJ, Batchelar DL, Cheung P, Mah K. Assessing the role of volumetric modulated arc therapy (VMAT) relative to IMRT and helical tomotherapy in the management of localized, locally advanced, and post-operative prostate cancer. Int J Radiat Oncol Biol Phys. 2011;80:1550-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 2. | Kuo YC, Chiu YM, Shih WP, Yu HW, Chen CW, Wong PF, Lin WC, Hwang JJ. Volumetric intensity-modulated Arc (RapidArc) therapy for primary hepatocellular carcinoma: comparison with intensity-modulated radiotherapy and 3-D conformal radiotherapy. Radiat Oncol. 2011;6:76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Yoo S. Treatment Plan Comparison between IMRT and Volumetric IMAT using One- and Two-arc Beams for Prostate Cancer. Int J Radiat Oncol Biol Phys. 2009;75 Supplement 1:S707-S707. |
| 4. | Yin Y, Ma C, Gao M, Chen J, Ma Y, Liu T, Lu J, Yu J. Dosimetric comparison of RapidArc with fixed gantry intensity-modulated radiotherapy treatment for multiple liver metastases radiotherapy. Med Dosim. 2011;36:448-454. [PubMed] |
| 5. | Wu QJ, Yoo S, Kirkpatrick JP, Thongphiew D, Yin FF. Volumetric arc intensity-modulated therapy for spine body radiotherapy: comparison with static intensity-modulated treatment. Int J Radiat Oncol Biol Phys. 2009;75:1596-1604. [PubMed] |
| 6. | Alvarez-Moret J, Pohl F, Koelbl O, Dobler B. Evaluation of volumetric modulated arc therapy (VMAT) with Oncentra MasterPlan® for the treatment of head and neck cancer. Radiat Oncol. 2010;5:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Verbakel WF, Cuijpers JP, Hoffmans D, Bieker M, Slotman BJ, Senan S. Volumetric intensity-modulated arc therapy vs. conventional IMRT in head-and-neck cancer: a comparative planning and dosimetric study. Int J Radiat Oncol Biol Phys. 2009;74:252-259. [PubMed] |
| 8. | Bertelsen A, Hansen CR, Johansen J, Brink C. Single Arc Volumetric Modulated Arc Therapy of head and neck cancer. Radiother Oncol. 2010;95:142-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Grégoire V, Levendag P, Ang KK, Bernier J, Braaksma M, Budach V, Chao C, Coche E, Cooper JS, Cosnard G. CT-based delineation of lymph node levels and related CTVs in the node-negative neck: DAHANCA, EORTC, GORTEC, NCIC,RTOG consensus guidelines. Radiother Oncol. 2003;69:227-236. |
| 10. | Chao KSC. Dose Prescription and Target Delineation for Nodal Volumes, in Intensity Modulated Radiation Therapy for Head and Neck Cancer. Lippincott Williams and Wilkins, 2003: 38-49. . |
| 11. | Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, Shank B, Solin LJ, Wesson M. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991;21:109-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3227] [Cited by in RCA: 3043] [Article Influence: 89.5] [Reference Citation Analysis (0)] |
| 12. | Shaw E, Kline R, Gillin M, Souhami L, Hirschfeld A, Dinapoli R, Martin L. Radiation Therapy Oncology Group: radiosurgery quality assurance guidelines. Int J Radiat Oncol Biol Phys. 1993;27:1231-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 486] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 13. | Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys. 2000;47:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1126] [Cited by in RCA: 1111] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 14. | Hall EJ, Wuu CS. Radiation-induced second cancers: the impact of 3D-CRT and IMRT. Int J Radiat Oncol Biol Phys. 2003;56:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 958] [Cited by in RCA: 932] [Article Influence: 42.4] [Reference Citation Analysis (0)] |
| 15. | Feuvret L, Noël G, Mazeron JJ, Bey P. Conformity index: a review. Int J Radiat Oncol Biol Phys. 2006;64:333-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 644] [Article Influence: 33.9] [Reference Citation Analysis (0)] |