Published online May 24, 2024. doi: 10.5306/wjco.v15.i5.644
Peer-review started: January 6, 2024
First decision: January 17, 2024
Revised: February 12, 2024
Accepted: March 27, 2024
Article in press: March 27, 2024
Published online: May 24, 2024
Processing time: 135 Days and 19 Hours
As a consequence of the economic crisis, the sociopolitical instability and the advent of the coronavirus disease-19 pandemic, nested challenges faced the Lebanese healthcare system. These have resulted in critical shortages of essential resources, including medications vital for oncologic patients.
To assess the ramifications of the ongoing economic crisis on oncology patient care focusing on our outpatient oncology department.
A questionnaire was distributed during the month of February 2022 to oncology patients in Hôtel Dieu de France University Hospital in Beirut during their outpatient therapy. The primary objective was to assess the far-reaching impact of the economic crisis on patient care and the resulting psychological implications.
Among 182 interviewed patients, 31.87% experienced treatment interruption mainly due to acute drug shortages. Despite 87.91% of the patients benefiting from third-party coverage, 69.60% had to self-pay for their medications leading to 69.78% of patients perceiving that healthcare was more difficult to access after 2020. Psychologically, one-third of the patients exhibited symptoms of anxiety and/or depression, with 7 patients reporting suicidal ideations. Notably, 37.93% of patients who interrupted cancer treatment reported a history of comorbidities, and 89.66% who altered their treatment cited financial difficulties.
Lebanese cancer patients face complex challenges spanning economic, healthcare, and psychological realms. Income inequalities exacerbated by the economic crisis hindered healthcare access.
Core Tip: The Lebanese healthcare system, strained by economic crisis, sociopolitical unrest, and the coronavirus disease 2019 pandemic, faces critical shortages, impacting vital oncology medications. In February 2022, a questionnaire was administered to 182 oncologic patients at Hôtel Dieu de France University Hospital, Beirut during outpatient therapy. Results revealed that 31.87% experienced treatment interruptions due to acute drug scarcities. Despite 87.91% having third-party coverage, 69.60% self-funded medications, leading to 69.78% perceiving limited healthcare access post-2020. Psychologically, one-third exhibited anxiety/depression symptoms, and 7 patients reported suicidal thoughts. Most patients altered their treatment plan, citing financial strains.
- Citation: Eid D, Jabbour J, Moujaes E, Kourie HR, Safieddine M, Kattan J. Impact of the economic crisis and drug shortage on Lebanese cancer patients’ care. World J Clin Oncol 2024; 15(5): 644-652
- URL: https://www.wjgnet.com/2218-4333/full/v15/i5/644.htm
- DOI: https://dx.doi.org/10.5306/wjco.v15.i5.644
Since the onset of the coronavirus disease 2019 (COVID-19) pandemic in March 2020, the global landscape has grappled with a profound economic downturn[1]. Lebanon, amidst this worldwide crisis, has faced a multitude of deficiencies across various sectors. As per the World Bank, the economic upheaval in Lebanon stands among the foremost three significant global economic crises since the mid-19th century[2]. The Lebanese Pound (LBP) experienced unprecedented fluctuations, plummeting from 1500 LBP to 93000 LBP for 1 United States Dollar[3], notably exacerbated after the catastrophic Beirut blast on August 4, 2020. Despite 82% of the country’s healthcare sector being reliant on private hospitals, the Lebanese government is indebted to them for a staggering 1.3 trillion dollars, a sum escalating perpetually[4].
The dearth of funds, resources, and foreign currency has placed the country in a precarious position in confronting the challenges posed by the COVID-19 pandemic. Furthermore, the government’s inability to allocate a stimulus package has left both public and private hospitals ill-equipped with necessary resources[5]. Consequently, hospitals are grappling with financial constraints in procuring supplies and equipment and meeting the salaries of healthcare workers[4]. This strain on the socioeconomic health system has impacted patient care in various fields (infectious disease, cardiovascular disease, and others)[6,7].
Amidst this economic instability within the healthcare sector, the Lebanese oncology patient also faces formidable barriers in accessing adequate healthcare. Not only is treatment inherently expensive, but it has also become susceptible to smuggling across neighboring countries, hoarding by individuals and local warehouses, illicit trafficking of counterfeit drugs, and the collapse of third-party payer coverage[8].
In this backdrop, we assessed the ramifications of the ongoing economic crisis on oncology patient care at the outpatient oncology department at Hôtel Dieu de France University Hospital, a tertiary multidisciplinary university hospital located at the heart of Beirut, Lebanon. This hospital serves 15% of the Lebanese population and hosts almost 20% of cancer patients on a national scale.
This study was based on a questionnaire that we established and distributed during the month of February 2022 to Lebanese oncology patients treated in the 1-d oncology ward at Hôtel Dieu de France University Hospital. The aim of the questionnaire was to assess their access to medical care as well as the physical and psychological impacts of the crisis and the lack of medication. Patients were questioned during their outpatient course of therapy, for around 10 min. They received an explanation of the study objectives, consented to fill out the questionnaire, and were assisted by one of the interns (who are also authors of this manuscript) during its completion on-site.
The study and the questionnaire were approved by the department’s Institutional Review Board (No. CEHDF 1903).
The following data were obtained for each patient: Age; sex; nationality; work status; marital status; educational level; and monthly income. The presence of other chronic illnesses in the patient and their family members and the presence or absence of healthcare coverage were also reported. Patients were questioned about social and financial difficulties that they have faced during the period of economic crisis and about difficulties in accessing healthcare or getting financial coverage for their healthcare expenses. The questionnaire also contained the Patient Health Questionnaire-4 (PHQ-4) items[9] that addressed the impact of the crisis on the patients’ mental health (Supplementary Table 1) and one question about any suicidal thoughts the patient had during the prior 3 month. The Arabic and English versions of the ques
We estimated descriptive statistics to study the sociodemographic characteristics of patients. Patient characteristics were presented as mean and standard deviation in the cases of continuous data and absolute and relative frequencies in the cases of categorical data. Pearson’s χ2 and Student’s t test were performed to determine statistical significance. Results were considered significant with a P value < 0.05.
The data collection was conducted through a Google Form. Statistical analyses were performed using R statistical software version 3.5.3 (packages: PrettyR, tableone).
A total of 182 patients were interviewed, consisting of 79 males (43.41%) and 103 females (56.59%) with an average age of 61.18 ± 13.32 years. Among them, 173 were Lebanese nationals (95.05%), while the remaining individuals hailed from diverse backgrounds such as France (n = 4), Iraq (n = 1), the Philippines (n = 1), Morocco (n = 1), Palestine (n = 1), and South Africa (n = 1).
Regarding residency, 122 participants (67.03%) lived within urban areas. Notably, the majority of the participants were non-working individuals during the survey period (63.38%) and were married (78.02%). Approximately half of the participants held university degrees, while 8.79% were characterized as being illiterate (Table 1).
| Sociodemographic variables | Total, n = 182 |
| Age, mean ± SD | 61.18 ± 13.32 |
| Sex | |
| Male | 79 (43.41) |
| Female | 103 (56.59) |
| Nationality | |
| Lebanese | 173 (95.05) |
| Other | 9 (4.95) |
| Place of residency | |
| City | 122 (67.03) |
| Outside of the city | 60 (32.97) |
| Work status | |
| Worker | 63 (34.62) |
| Non-worker | 119 (63.38) |
| Educational level | |
| Illiterate | 16 (8.79) |
| Less than high school | 11 (6.04) |
| High school | 25 (13.74) |
| College | 35 (19.23) |
| University | 95 (52.20) |
| Status | |
| Married | 142 (78.02) |
| Single | 29 (15.93) |
| Divorced | 1 (0.55) |
| Widowed | 10 (5.50) |
Concerning monthly household income, 78 patients (42.86%) reported earnings below $300, while 56 patients (30.77%) fell within the $300-$1000 bracket. Forty-eight patients (26.37%) reported incomes exceeding $1000 per month. On average, this income supported 3.00 ± 1.54 individuals within the same household.
Around 34.07% of patients identified a family member with a severe chronic illness managed within the same income used for their own treatment (Table 2).
| Characteristics | Total, n = 182 |
| Total household income/month in USD | |
| < 300 | 78 (42.86) |
| Between 300 and 1000 | 56 (30.77) |
| > 1000 | 48 (26.37) |
| Number of people in household | 3.00 ± 1.54 |
| Household members-excluding the patient-suffering from serious chronic disease | |
| Yes | 62 (34.07) |
| No | 120 (65.93) |
Approximately 31.87% of patients recently halted or interrupted at least one oncological treatment, predominantly chemotherapy. Primary reasons cited were drug scarcity (70.69%) and unaffordable prices compounded by insurance coverage rejections (13.79%). These factors significantly influenced 44.51% of the population to change at least one medication (Table 3).
| Characteristics | Value, n = 182 |
| Stopped or interrupted any drugs including chemotherapy | |
| Yes | 58 (31.87) |
| Reason: | |
| Shortage | 41 (70.69) |
| Price/coverage | 8 (13.79) |
| COVID-19 | 1 (1.72) |
| Other | 8 (13.79) |
| No | 124 (68.13) |
| Changed any of their medications | |
| Yes | 81 (44.51) |
| Reason: | |
| Shortage | 74 (91.36) |
| Price | 3 (3.70) |
| Coverage | 4 (4.94) |
| No | 101 (55.49) |
| Had a third-party payer | |
| Yes | 160 (87.91) |
| Syndicate | 4 (2.50) |
| Insurance | 82 (51.25) |
| CNSS | 52 (32.50) |
| CFE | 4 (2.50) |
| Ministry of Public Health | 13 (8.13) |
| Army | 5 (3.12) |
| No | 22 (12.09) |
| Source of medication payment | |
| Out-of-pocket | 87 (69.60) |
| Donations | 14 (11.20) |
| Family | 9 (7.20) |
| Primary healthcare centers | 14 (11.20) |
| Ministry of Public Health | 1 (0.80) |
The vast majority (87.91%) of patients benefited from third-party payer coverage through either public social coverage or private insurance, the latter being the predominant means of insurance (51.25%). The remaining coverage included the National Social Security Fund or Caisse Nationale de Sécurité Sociale (32.5%), the Ministry of Public Health (8.13%), the Lebanese army (3.12%), the syndicate (2.5%), and the Caisse Française de l’Etranger (2.5%; Table 3).
Third-party payer limitations forced 69.60% of patients to self-finance their medication, with 11.20% relying on donations. Therefore, 79.12% of the population reported facing financial challenges due to healthcare expenses, and 23.08% resorted to self-medication instead of seeking professional care or emergency room assistance due to financial constraints. Also, 25 individuals (13.74%) had to forego treatments, surgeries, or procedures due to cost considerations, with 12 patients canceling chemotherapy sessions. Moreover, nearly half of the patients (51.65%) grappled with additional chronic illnesses, and 76% of these encountered barriers accessing specific treatments (Table 4).
| Characteristics | Total, n = 182 |
| Changing third-party payer due to coverage problems | |
| Yes | 11 (6.04) |
| No | 171 (93.96) |
| Reporting financial difficulties due to health care spending | |
| Yes | 144 (79.12) |
| No | 38 (20.88) |
| Self-medication instead of seeking medical treatment due to financial difficulties | |
| Yes | 42 (23.08) |
| No | 140 (76.92) |
| Cancelled a treatment, surgery, or any procedure because of its cost during the last year | |
| Yes | 25 (13.74)1 |
| No | 157 (86.26) |
| Suffering from other chronic diseases necessitating chronic treatments | |
| Yes | 94 (51.65) |
| No | 88 (48.35) |
| Any problems accessing specific treatments for other chronic diseases | |
| Yes | 76 (80.85) |
| No | 18 (19.15) |
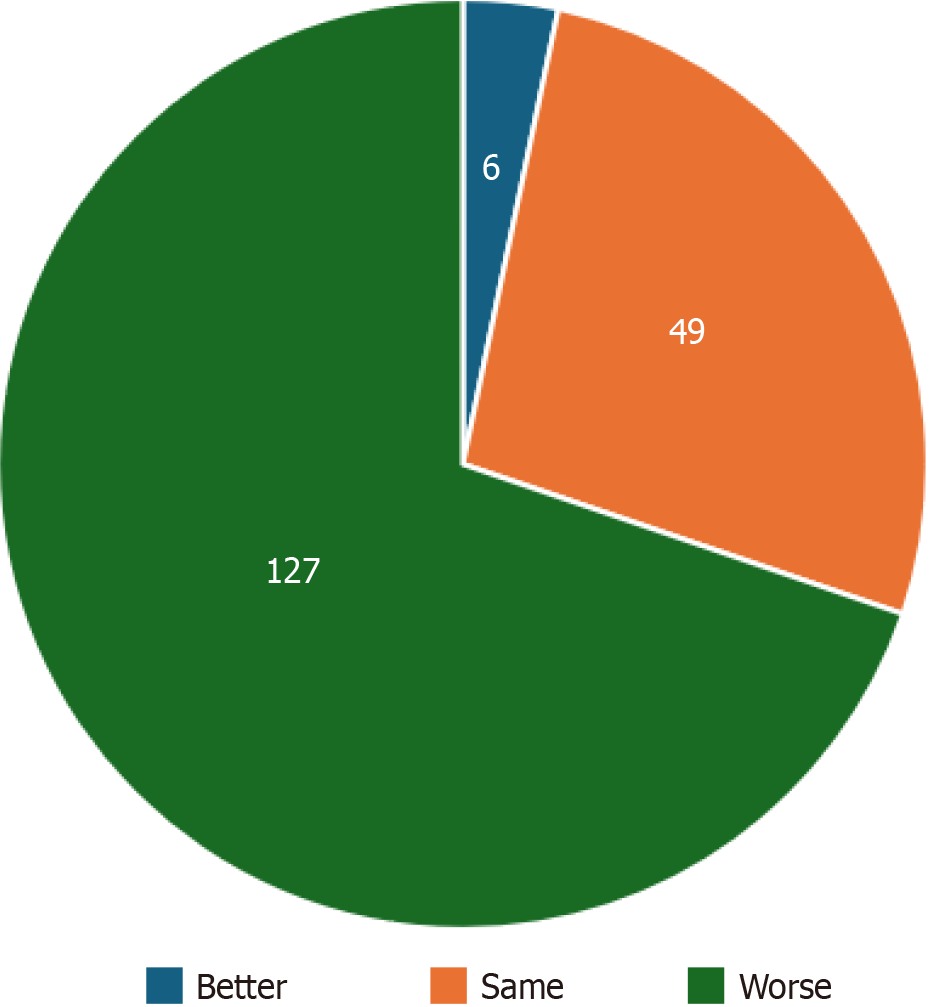
The perceived access to healthcare post-2020 was considered more difficult by 69.78% of respondents. Yet, a quarter of patients (26.92%) noticed no changes before and after 2020, with only 3.30% perceiving healthcare as more accessible after 2020 (Figure 1).
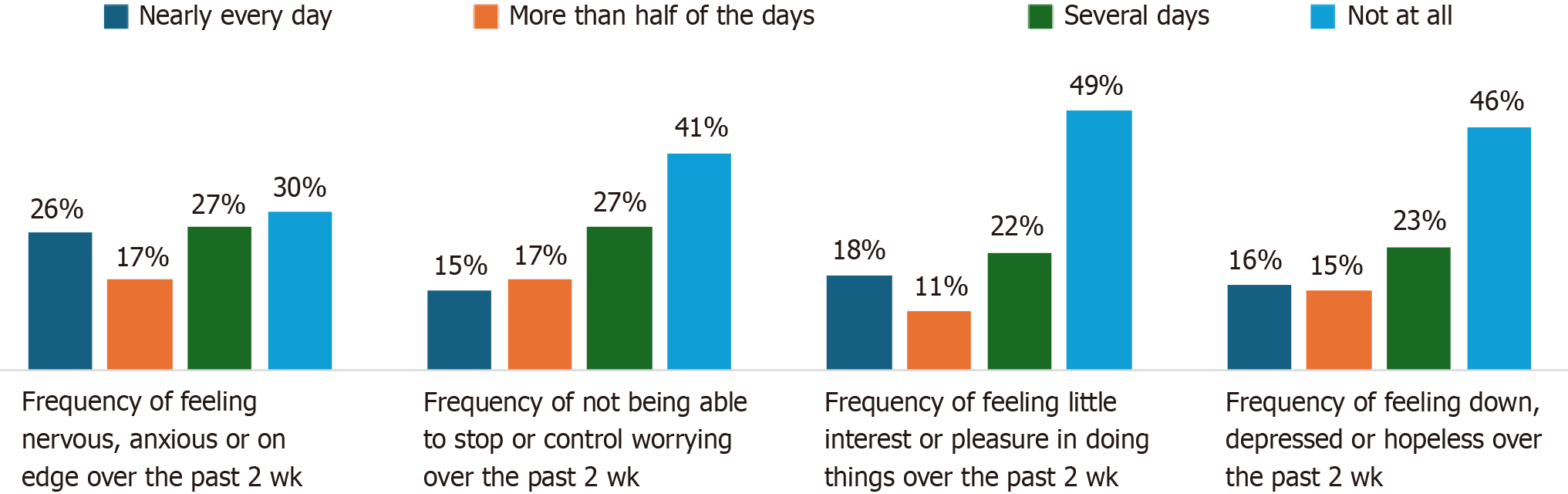
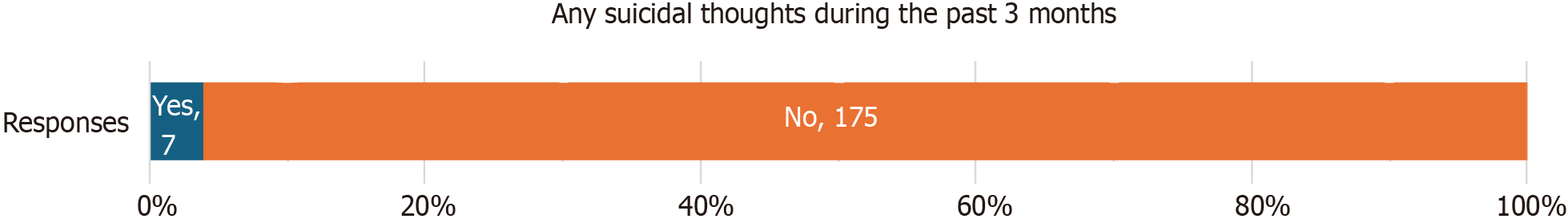
We assessed the mental health status of patients during the crisis period through their responses to the 4-item PHQ-4 questionnaire. One-third of the patients expressed at least one symptom of anxiety and/or depression (Figure 2). Seven patients (4%) acknowledged suicidal ideations (Figure 3), of whom two patients had a PHQ-4 within the normal range.
Analyzing these findings using the χ2 test revealed significant relationships. Notably, a link between other personal comorbidities and interrupting cancer treatment (P = 0.01) emerged, with 37.93% of patients who interrupted cancer treatment reporting a history of comorbidities.
Interruptions in cancer treatment correlated significantly with patient financial status (P = 0.017): 89.66% who altered their treatment cited financial issues compared to 15.79% who maintained their original medication.
Our data analysis also showed that individuals earning less than $300 were more prone to healthcare access-related financial difficulties compared to those earning more ($300 or above) with a statistically significant P value of 0.0022.
For those encountering financial distress, a notable association existed with patients avoiding consultations. Spe
Additionally, among patients identified as severely prone to depression and/or anxiety via the PHQ-4 questionnaire, a significant link emerged with the presence of comorbidities. Nevertheless, no substantial correlation was observed between mental health status and financial situations or judgments regarding healthcare access.
The enduring economic crisis in Lebanon continues to exert profound strain, particularly on chronically ill patients. Within our cohort, these individuals represent a minority but are among the most susceptible to the ramifications of this economic upheaval. Despite this, it is evident that the COVID-19 pandemic has significantly exacerbated the challenges associated with accessing healthcare in Lebanon.
Our investigation was tailored to measure the impact of this economic crisis specifically on cancer patients’ healthcare access. Our objective was to analyze different material-related and mental health-related aspects of this impact and seek any discernable links between them.
While certain relationships yielded statistically significant findings, others proved inconsequential. For instance, we showed that individuals earning less than $300 were more susceptible to healthcare access-related financial difficulties compared to those earning more. However, when juxtaposing their healthcare system judgment (worse or not) with their household income, the study unveiled no statistically proven correlation, suggesting a nuanced relationship between income and access to treatment.
Moreover, Lebanon grapples with medication shortages and treatment unavailability, independent of financial means, thereby impeding access even for affluent individuals. Notably, the burden of cancer treatment poses a significant strain on the country’s economic fabric[10].
A study published by Elias et al[11] in 2016 demonstrated the impact of government-financed cancer treatment between 2008 and 2013. The Ministry of Public Health financed cancer medication for all patients who did not have private insurance, which amounted to an average of 6475 United States Dollars over the 5 years. Interestingly, the cost exponentially increased during the study period due to excellent compliance of the patients to the treatment program. Our investigation revealed that since 2019 cancer drugs are no longer covered by the Ministry of Public Health due to the collapse of the government’s financial structure. This forced patients to either pay out of pocket or interrupt their treatment.
Another study by Kattan et al[12] showcased how Lebanese oncologists struggle with drug shortages and coverage issues by resorting to switching brands, using on/off prescription policies and suboptimal drug doses, and deviating from recommended drug intake modes. However, these coping strategies adversely affect cancer patients.
Our findings revealed a prevalent trend of avoiding doctor consultations among the studied population, which was significantly associated with financial struggles. Surprisingly, no significant relationship emerged between skipping appointments due to financial issues and total household income. This could imply that affording medical expenses is difficult, even for people with a better income, due to paying out of pocket in the absence of third-party coverage.
Interestingly, perceptions of poor healthcare access did not align with the presence of a third-party payer, suggesting complexities within the policies of private insurance in Lebanon, particularly in covering cancer-related medications. Affording medication out of pocket did not directly impact perceptions of healthcare access.
Of note, the Caisse Nationale de Sécurité Sociale covered almost 90% of health expenses before the crisis, whereas the Ministry of Public Health used to cover all the expenses of patients who did not have any other coverage means. However, these policies were subject to perpetual changes since the beginning of inflation and with the daily change in currency rates. Some measures included tightening the area of coverage.
Moreover, our analyses underscored a noteworthy connection between personal comorbidities and discontinuation of cancer treatment. This could be attributed to patients diverting resources from cancer treatment to address other medical conditions. However, external factors, such as the country’s ability to provide adequate treatment, could also influence treatment discontinuation.
Additionally, a worse mental health status was significantly correlated to the presence of comorbidities but was not correlated with the perception of worse healthcare access. This highlights the multifaceted nature of patients’ mental health influenced by Lebanon’s ongoing challenges. Not all 7 patients who expressed suicidal thoughts were within the severe risk range for anxiety and/or depression per the PHQ-4 test. This discrepancy raises queries about the sources of suicidal thoughts beyond mental health concerns, emphasizing the need for comprehensive evaluations beyond the PHQ-4 test.
According to the World Health Organization, suicide is tightly linked to mental health conditions such as depression. However, many suicide attempts are reported in situations of crisis (financial difficulties, interpersonal problems, chronic illness) without previous mental health disorder. This is related to an impaired ability to handle life stress[13]. The suicidal rate among Lebanese people was 2.76 per 100000 in 2019[14] and according to the 2022 annual report of EMBRACE Lebanon one person in Lebanon attempts suicide every 6 h[15].
In our establishment, cancer patients who report suicidal thoughts are systematically referred to the psychiatry de
Ultimately, our study underscored the intricate interplay between economic, healthcare, and mental health challenges in Lebanon. Addressing these multifaceted issues demands a comprehensive approach, integrating economic reforms, healthcare policy revisions, and tailored mental health interventions for better patient outcomes in this challenging landscape[16]. This could be achieved by promoting local potential and local manufacturers, standardizing medical consultation tariffs and private insurance packages, and implementing the national mental health strategy vision for 2023-2030 without delay[17]. Better supervision of healthcare structures and parties by the government is needed to identify corruption, and a wider cooperation with the private sector to shift medical aid to the most deprived patients would be beneficial.
The robustness of our study lies in the substantial number of patients interviewed, allowing for the collection of com
However, certain limitations are inherent in the study, primarily attributable to the ongoing instability and fluidity of circumstances during data collection. Factors such as fluctuating medication pricing, accessibility issues, and volatile exchange rates pose challenges in capturing a complete and static snapshot. A crucial aspect to acknowledge is that our study encompassed patients who could access hospitals and maintain their treatment regimen. Yet, it is imperative to note that a subset of patients discontinued hospital visits, which remains unaccounted for in our research. This group’s absence from our study potentially alters the findings. Obtaining data from these patients would allow a more comprehensive view of the state of cancer patients in Lebanon.
Given this perspective and the continuously evolving economic landscape, the elaboration and implementation of a national cancer plan is imperative to enhance access to healthcare systems in Lebanon. These guidelines should address the multifaceted challenges faced by cancer patients, ensuring equitable access to essential treatments and support systems amidst these turbulent times. In the meantime, patients will continue to rely on individual donations, fundraising organized on social media, telethons that support cancer patients/cancer organizations, and remittances from the Lebanese diaspora[19].
Undoubtedly, the emergence of COVID-19 as a global pandemic has significantly impacted various sectors worldwide and notably the medical field. In Lebanon, the concurrent onset of the COVID-19 outbreak and the accompanying economic crisis has compounded the challenges faced by patients, particularly those battling cancer. These individuals, already navigating a challenging journey due to their medical condition, are now confronted with additional hurdles stemming from the pandemic and economic turmoil. Our study provided a glimpse into the collective experiences of cancer patients, highlighting how the economic crisis, exacerbated by the pandemic, has profoundly affected them both financially and psychologically.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Lebanon
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Griesemer I, United States; Khalil G, Lebanon S-Editor: Li L L-Editor: A P-Editor: Zhao YQ
| 1. | Borio C. The Covid-19 economic crisis: dangerously unique. Bus Econ. 2020;55:181-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 2. | The World Bank. Lebanon Sinking into One of the Most Severe Global Crises Episodes, amidst Deliberate Inaction. [cited 6 December 2023]. Available from: https://www.worldbank.org/en/news/press-release/2021/05/01/lebanon-sinking-into-one-of-the-most-severe-global-crises-episodes. |
| 3. | Baff S. The Fluctuation of Lebanese Lira Against the US Dollar In the Parallel Market. Sep 8, 2021. [cited 6 December 2023]. Available from: https://blog.blominvestbank.com/41472/. |
| 4. | Devi S. Economic crisis hits Lebanese health care. Lancet. 2020;395:548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Mansour HA, Bitar E, Fares Y, Makdessi AA, Maalouf A, Ghoul ME, Mansour MA, Chami A, Khalil M, Jalkh A, Cherfan D, Fares J, Khuri FR, Mansour AM; Beirut Port Ammonium Nitrate Explosion Consortium. The Beirut Port explosion: injury trends from a mass survey of emergency admissions. Lancet. 2021;398:21-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Isma'eel H, El Jamal N, Al-Chaer E, Haj-Ali W, Hamadeh G. Reforming Healthcare Practice in View of the Economic Crisis in Lebanon: The Case of Cardiovascular Care. Mediterr J Emerg Med Acute Care. 2020;1:1-12. [DOI] [Full Text] |
| 7. | Khalil G, Marty P, Hage K, Sfeir S, El Hage J, Bou Assi T, Rassam M, Pomares C, Mikhael E. Could the re-emerging practice of wild boar hunting linked to the recent economic crisis lead to new outbreaks of trichinellosis in Lebanon? Parasite. 2022;29:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Fleifel M, Abi Farraj K. The Lebanese Healthcare Crisis: An Infinite Calamity. Cureus. 2022;14:e25367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 9. | Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 457] [Cited by in RCA: 1278] [Article Influence: 85.2] [Reference Citation Analysis (0)] |
| 10. | Prasad V, De Jesús K, Mailankody S. The high price of anticancer drugs: origins, implications, barriers, solutions. Nat Rev Clin Oncol. 2017;14:381-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 279] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 11. | Elias F, Khuri FR, Adib SM, Karam R, Harb H, Awar M, Zalloua P, Ammar W. Financial Burden of Cancer Drug Treatment in Lebanon. Asian Pac J Cancer Prev. 2016;17:3173-3177. [PubMed] |
| 12. | Kattan C, Kattan J. Accommodation with anticancer drug shortage: A Lebanese harmful solution. Front Oncol. 2022;12:1055113. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | World Health Organization. Suicide. Aug 23, 2023. [Cited 1 February 2024]. Available from: https://www.who.int/news-room/fact-sheets/detail/suicide. |
| 14. | Lew B, Lester D, Kõlves K, Yip PSF, Chen YY, Chen WS, Hasan MT, Koenig HG, Wang ZZ, Fariduddin MN, Zeyrek-Rios EY, Chan CMH, Mustapha F, Fitriana M, Dolo H, Gönültaş BM, Dadfar M, Davoudi M, Abdel-Khalek AM, Chan LF, Siau CS, Ibrahim N. An analysis of age-standardized suicide rates in Muslim-majority countries in 2000-2019. BMC Public Health. 2022;22:882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 15. | Embrace. Embrace Lebanon. [Cited 2 February 2024]. Available from: https://www.embracelebanon.org/home. |
| 16. | El-Jardali F, Masri R, Sleem Z. Rethinking Lebanon's Healthcare System Amid the Economic Crisis. LCPS. Jul 27, 2023. [Cited 1 February 2024]. Available from: https://www.lcps-lebanon.org/articles/details/4799/rethinking-lebanon's-healthcare-system-amid-the-economic-crisis. |
| 17. | Republic of Lebanon Ministry of Public Health. Lebanon National Health Strategy-Vision 2030. [Cited 1 February 2024]. Available from: https://www.moph.gov.lb/en/Pages/0/67043/Lebanon-national-health-strategy-vision-2030. |
| 18. | Mohty R, Tfayli A. General Oncology Care in Lebanon. In: Al-Shamsi HO, Abu-Gheida IH, Iqbal F, Al-Awadhi A, editors. Cancer in the Arab World. Singapore: Springer, 2022: 115-132. [DOI] [Full Text] |
| 19. | UNDP. The increasing role and importance of remittances in Lebanon. Jun 9, 2023. [Cited 1 February 2024]. Available from: https://www.undp.org/arab-states/publications/increasing-role-and-importance-remittances-lebanon. |