Published online Dec 24, 2024. doi: 10.5306/wjco.v15.i12.1514
Revised: September 2, 2024
Accepted: September 10, 2024
Published online: December 24, 2024
Processing time: 87 Days and 6.9 Hours
Chronic skin ulcers are a risk factor for the development of skin tumors. In patients with diabetes, chronic refractory ulcers may also contribute to higher susceptibility to skin tumors. Timely surgical removal of chronic and nonhealing diabetic foot ulcers can effectively prevent progression to squamous cell car
An 84-year-old male patient with diabetes presented with a significantly ulcerated area on his foot. The ulcer had been present to varying degrees since 1996. Be
Potentially malignant lesions in chronic ulcer wounds should be identified and treated in a timely manner to prevent their progression.
Core Tip: Chronic skin ulcers are considered a risk factor for developing skin tumors. In people with diabetes, chronic refractory ulcers may also increase susceptibility to skin tumors. From a clinical perspective, raising awareness of their potential progression to malignant lesions is essential.
- Citation: Luo Y, Li CY, Wang YQ, Xiang SM, Zhao C. Diabetic ulcer with cutaneous squamous cell carcinoma: A case report. World J Clin Oncol 2024; 15(12): 1514-1519
- URL: https://www.wjgnet.com/2218-4333/full/v15/i12/1514.htm
- DOI: https://dx.doi.org/10.5306/wjco.v15.i12.1514
Chronic skin ulcers are considered a risk factor for developing skin tumors. In patients with diabetes, chronic refractory ulcers may contribute to increased susceptibility to skin tumors[1]. Patients with diabetes are at risk of developing ulcers, with the main contributing factors being loss of protective sensation, peripheral artery disease, foot deformities, and a history of lower-limb amputation[2,3]. Poor blood sugar control and circulatory disorders further increase the risk of ulcer development in patients with diabetes, leading to high recurrence rates or chronic nonhealing of skin ulcers[4]. Repeated diabetic ulcers may transform into malignant lesions such as cutaneous squamous cell carcinoma (cSCC)[5,6]. Therefore, routine skin tissue biopsy can help avoid misdiagnosing local skin wounds that exhibit infiltrative or exophytic growth of granulation tissue. Timely surgical debridement and treatment of recurrent diabetic ulcers may prevent their development and progression to cSCC[6].
An 84-year-old male patient (born in October 1939) with diabetes presented with a significantly ulcerated area on his foot.
The ulcer had been present to varying degrees since 1996.
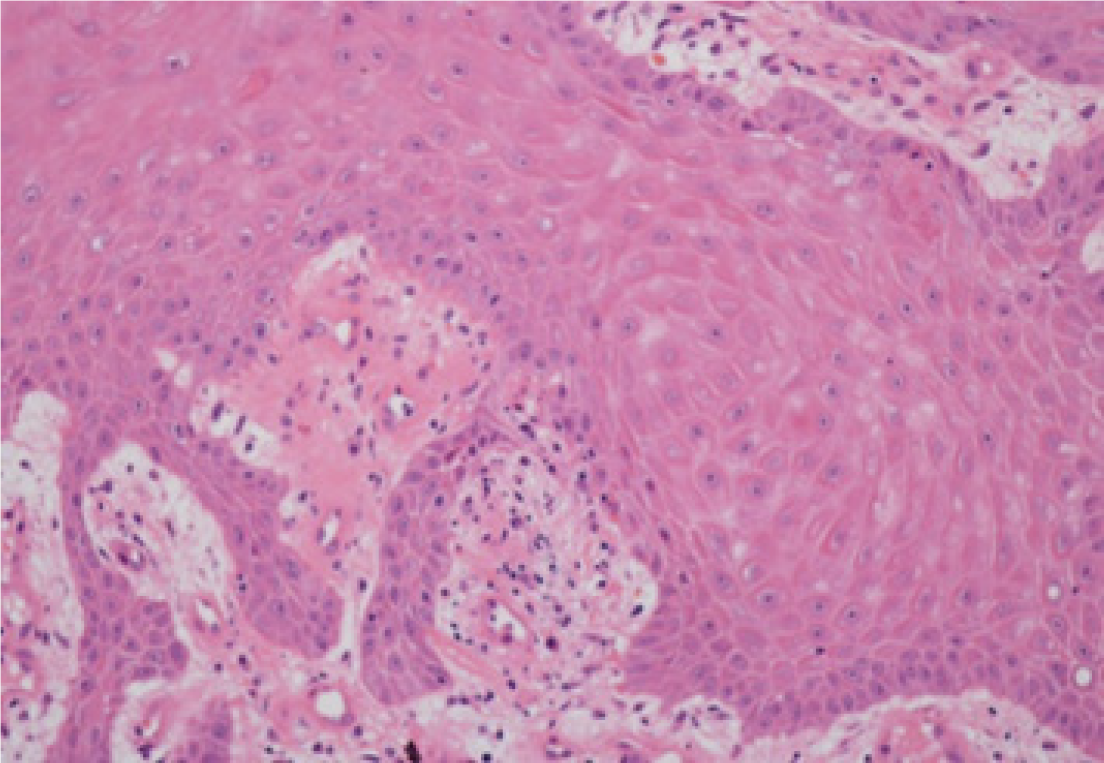
The patient was diagnosed with diabetes in 1990. Between 1996–1998, he experienced the breakdown of the ulceration on the posterior aspect of his right foot. Anti-infection treatment and traditional Chinese medicine for heat were then administered. The main herbal medicine used was Chen Lanhua Granule (main ingredients: Yinchen, Zehlan, and Chonglou), taken orally. The external medicine used was Jiangjun Powder (main ingredients: Dahuang, Mangxiao, and Gancao). After the dampness was cleared, the wound healed after a local operation to purify and clear the muscles, followed by wound-dressing. However, in 2012, the original wound ruptured on the dorsal aspect of the patient’s right foot. Between 2012–2018, despite improvements in the recurrent ulcers on his foot with treatment interventions, complete healing was not achieved. The wound exhibited noticeable granulation, edema, and prominence. By August 2018, there was gradual enlargement of the ulcerated area on his foot with an irregular shape resembling a rotten vegetable pattern accompanied by soybean curd secretions-as well as increased blood and liquid oozing, and a strong foul odor (Figure 1). Pathology results obtained on December 30, 2018 indicated partial hyperplasia and keratosis of the squamous epithelium at the site (right dorsum of foot), resulting in a pathological diagnosis of squamous epithelial hyperplasia. Further pathological examination conducted on February 21st, 2019 revealed pseudo-epitheliomatous hyperplasia of the squamous epithelium (right foot) with partial atypical hyperplasia (Figure 2). Between 2012 and July 2019, several corrective surgeries were performed for the chronic ulcers present on his right foot at our hospital. However, even after receiving treatments such as the herbal medicines Chen Lanhua Granule, Dahuang, Mangxiao, Gancao, and others for heat clearance and detoxification—which did result in sufficient symptom improvement to discharge the patient from hospital care—complete healing of the wound was not achieved.
The patient had a history of diabetes and denied other family history.
The ulcer had an irregular shape resembling a rotten vegetable pattern accompanied by soybean curd secretions—as well as increased blood and liquid oozing, and a strong foul odor.
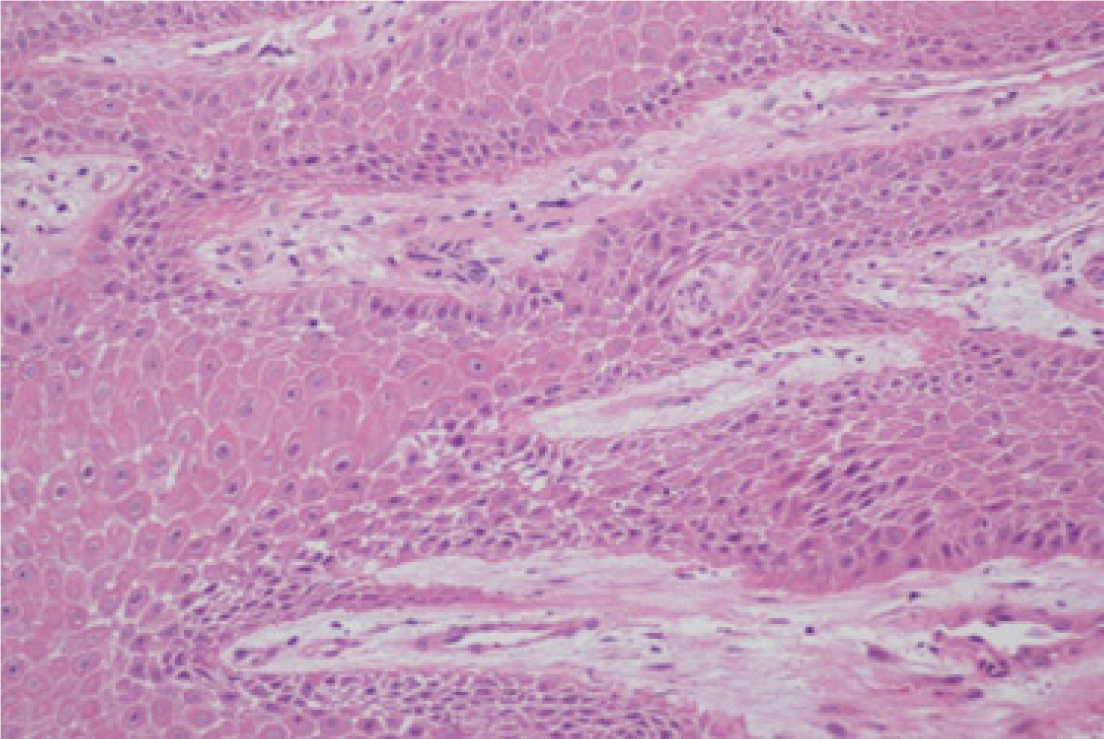
In July 2020, histopathological analysis confirmed a well-differentiated cSCC within a tissue sample from the wound (Figure 3).
On February 13, 2020, radiographic examination revealed misalignment of the fifth metatarsophalangeal joint in the right foot, accompanied by osteoporosis and soft tissue edema in the same region.
The patient was diagnosed with well-differentiated cSCC of the foot.
Local tissue excision surgery was performed, followed by appropriate cleaning. Nano-silver excipients were used to promote ulcer wound healing, in conjunction with Chinese herbal decoctions to clear heat, detoxify, and remove saprophytic muscle. Simiao and Tuoli Xiaodu powders were used as the main prescriptions for addition and subtraction treatments.
After the treatments were administered, the ulcer wound healed slowly and did not expand.
Recurrent ulcers can lead to cSCC. Previous case reports have highlighted instances where toe SCCs in patients with diabetes were initially misdiagnosed as diabetic foot ulcer(DFU)[5-7]. Neglected chronic wounds and long-term scar tissue complications of cSCC have also been documented[8,9]. Additionally, there are reports in the literature of diabetic lipoid necrosis (NLD) in the legs that progressed to ulcerations and eventually degenerated into cSCC[10]. The NLD environment provides a favorable setting for the development of cSCC, emphasizing the importance of considering non-healing ulcers as potential indicators. Early biopsy is recommended for such lesions[11]. A growing number of studies have reported clinical cases in which malignant tumors were initially misdiagnosed as DFU. A review of these cases revealed subsequent diagnoses, including melanoma (68%), Kaposi's sarcoma (14%), cSCC (11%), mantle cell lymphoma, and diffuse B-cell lymphoma (4%). Notably, older age (≥ 65 years) was associated with an increased risk of malignancy masked by DFU. The suspected risk in older patients was 145% higher than that in younger ones (< 65 years). Clinicians should remain vigilant for potentially malignant foot lesions in older patients with diabetes aged ≥ 65 years[12].
Increasing evidence has demonstrated a correlation between abnormal glucose homeostasis and the development and prognosis of certain tumors[13]. Elevated blood sugar levels can independently, directly, or indirectly increase the risk of cancer[14]. In addition, diabetes-related oxidative stress damage is believed to contribute to oncogenic transformation and cancer progression[15]. The aforementioned cases are not known to have been misdiagnosed or induced because of insufficient current clinical evidence. However, in cases of chronic ulcer wounds resembling those mentioned above, it is crucial to enhance clinical awareness of their potential progression to malignant lesions. Needle biopsies represent a simple and effective diagnostic technique for treating wounds that are resistant to healing. Histological examination can rule out cancer in the wound bed and diagnose difficult-to-cure or suspicious ulcers[16]. Studies have found that the incidence of nonvascular ulcers is 5%, to the majority of which are skin cancers. Marginal eminence and abnormal growth of granulation tissue represent the most common features of these ulcers. Therefore, a timely skin biopsy is warranted[17]. Regardless of the duration of chronic ulcer recurrence, routine skin tissue biopsies can prevent misdiagnosis. Timely surgical removal of chronic nonhealing DFU may impede the development of cSCC. Physicians should remain vigilant regarding the possibility of malignancy in patients with diabetes who present with persistent and refractory ulcerative foot lesions. Furthermore, it is anticipated that future research will uncover additional clinical evidence elucidating this "misdiagnosis", thereby preventing further instances while offering more effective and beneficial treatment options for these patients.
In case of chronic ulcer wounds, attention should be paid to potential malignant lesions and timely treatment should prevent their malignant progression.
| 1. | Dobrică EC, Banciu ML, Kipkorir V, Khazeei Tabari MA, Cox MJ, Simhachalam Kutikuppala LV, Găman MA. Diabetes and skin cancers: Risk factors, molecular mechanisms and impact on prognosis. World J Clin Cases. 2022;10:11214-11225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (2)] |
| 2. | Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017;376:2367-2375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1953] [Cited by in RCA: 2333] [Article Influence: 291.6] [Reference Citation Analysis (2)] |
| 3. | Crawford F, Cezard G, Chappell FM, Murray GD, Price JF, Sheikh A, Simpson CR, Stansby GP, Young MJ. A systematic review and individual patient data meta-analysis of prognostic factors for foot ulceration in people with diabetes: the international research collaboration for the prediction of diabetic foot ulcerations (PODUS). Health Technol Assess. 2015;19:1-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 128] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 4. | Fu XL, Ding H, Miao WW, Mao CX, Zhan MQ, Chen HL. Global recurrence rates in diabetic foot ulcers: A systematic review and meta-analysis. Diabetes Metab Res Rev. 2019;35:e3160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 5. | Larijani B, Tavangar SM, Bandarian F. Squamous Cell Carcinoma Arising in a Chronic, Nonhealing Diabetic Foot Ulcer. Wounds. 2017;29:E48-E50. [PubMed] |
| 6. | Mantovani A, Teobaldi I, Stoico V, Perrone F, Zannoni M, Cima L, Bruti M, Mingolla L, Trombetta M, Bonora E. Cutaneous squamous carcinoma in a patient with diabetic foot: an unusual evolution of a frequent complication. Endocrinol Diabetes Metab Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Park HC, Kwon HI, Kim HW, Kim JE, Ro YS, Ko JY. A Digital Squamous Cell Carcinoma Mimicking a Diabetic Foot Ulcer, With Early Inguinal Metastasis and Cancer-Related Lymphedema. Am J Dermatopathol. 2016;38:e18-e21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Moe TT, Gürgen M, Undersrud E, Klepp R, Sola H. [A man in his forties with rapid exacerbation of chronic foot ulcers]. Tidsskr Nor Laegeforen. 2021;141. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Dörr S, Lucke-Paulig L, Vollmer C, Lobmann R. Malignant Transformation in Diabetic Foot Ulcers-Case Reports and Review of the Literature. Geriatrics (Basel). 2019;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. |
Akioud F, Abainou LH, El-Hadri S, AyoubIdrissi, Meftah A, Baizri H, Necrosislipoidica in type 2 diabetes mellitus: clinical cases and review of the literature.
|
| 11. | Lefkovits Y, Adler A. Fatal squamous cell carcinoma from necrobiosis lipoidica diabeticorum in a diabetic patient. Endocrinol Diabetes Metab Case Rep. 2019;2019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Lyundup AV, Balyasin MV, Maksimova NV, Kovina MV, Krasheninnikov ME, Dyuzheva TG, Yakovenko SA, Appolonova SA, Schiöth HB, Klabukov ID. Misdiagnosis of diabetic foot ulcer in patients with undiagnosed skin malignancies. Int Wound J. 2022;19:871-887. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R. Diabetes and cancer. Endocr Relat Cancer. 2009;16:1103-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 722] [Cited by in RCA: 765] [Article Influence: 47.8] [Reference Citation Analysis (0)] |
| 14. | Xu CX, Zhu HH, Zhu YM. Diabetes and cancer: Associations, mechanisms, and implications for medical practice. World J Diabetes. 2014;5:372-380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 89] [Cited by in RCA: 100] [Article Influence: 9.1] [Reference Citation Analysis (1)] |
| 15. | Lee SC, Chan JC. Evidence for DNA damage as a biological link between diabetes and cancer. Chin Med J (Engl). 2015;128:1543-1548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Serena TE, Cole W, Coe S, Harrell K, Serena L, Yaakov R, Rennie MY. The safety of punch biopsies on hard-to-heal wounds: a large multicentre clinical trial. J Wound Care. 2020;29:S4-S7. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Stansal A, Khayat K, Duchatelle V, Tella E, Gautier V, Sfeir D, Attal R, Lazareth I, Priollet P. [When to ask for a skin biopsy in a patient with leg ulcer? Retrospective study of 143 consecutive biopsies]. J Med Vasc. 2018;43:4-9. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |