Published online Dec 24, 2024. doi: 10.5306/wjco.v15.i12.1507
Revised: September 5, 2024
Accepted: September 30, 2024
Published online: December 24, 2024
Processing time: 95 Days and 23 Hours
Both rhabdomyosarcoma (RMS) and central retinal artery occlusion (CRAO) are rare medical diseases, and their simultaneous occurrence in the same patient is extraordinarily uncommon. This study presents a comprehensive overview of the clinical manifestations, diagnostic imaging results, and therapeutic interventions of a patient with both conditions.
In this report, we present a 30-year-old male who presented with significant protrusion, pain and vision loss and was diagnosed with RMS in the orbit and sinus with CRAO. Following resection of the sinus and orbital mass and enuclea
This article provides an in-depth analysis of the patient’s clinical manifestations, the tumor’s anatomical origin, and the etiology of CRAO. The concurrent manife
Core Tip: Rhabdomyosarcoma is a highly malignant tumor that rarely occurs in young adults. We report a case of a 30-year-old male diagnosed with rhabdomyosarcoma involving the orbit and sinus complicated by central retinal artery occlusion. We investigated the causes of these conditions in this patient using the clinical presentation and signs, pathologic exa
- Citation: Ma Y, Jia B, He XJ, Cai YX, Chen JY, Zhong JX. Orbital and sinus rhabdomyosarcoma with concurrent central retinal artery occlusion: A case report. World J Clin Oncol 2024; 15(12): 1507-1513
- URL: https://www.wjgnet.com/2218-4333/full/v15/i12/1507.htm
- DOI: https://dx.doi.org/10.5306/wjco.v15.i12.1507
Rhabdomyosarcoma (RMS) is an aggressive soft tissue sarcoma characterized by the uncontrolled proliferation of undifferentiated mesenchymal stem cells or embryonic muscle tissue. The head and neck region is the most common site of occurrence, with the orbit accounting for 75% of these cases. Morphologically, RMS can be categorized into four types: Embryonal (60%), alveolar (20%), pleomorphic, and spindle cell/sclerosing[1]. Alveolar RMS (ARMS), which is predominantly observed in late childhood and adolescence, is known for its high malignancy rate. In contrast, central retinal artery occlusion (CRAO), a leading cause of sudden blindness, typically occurs due to arterial spasm, embolism, arteritis, or atherosclerosis. The average age of patients affected by CRAO is around 60 years. The incidence of CRAO in in
A 30-year-old male patient was admitted to our hospital with pain, swelling and blurred vision in the right eye, accom
He described an incident from two weeks prior, where he accidentally struck the back of his head. He subsequently experienced progressively worsening symptoms in his right eye, including pain, swelling, blurred vision without double vision, right-sided nasal pain, intermittent bleeding, nasal congestion, and no loss of smell.
The patient was otherwise healthy but tested positive for hepatitis B virus surface antigen.
The patient had no specific family or personal history.
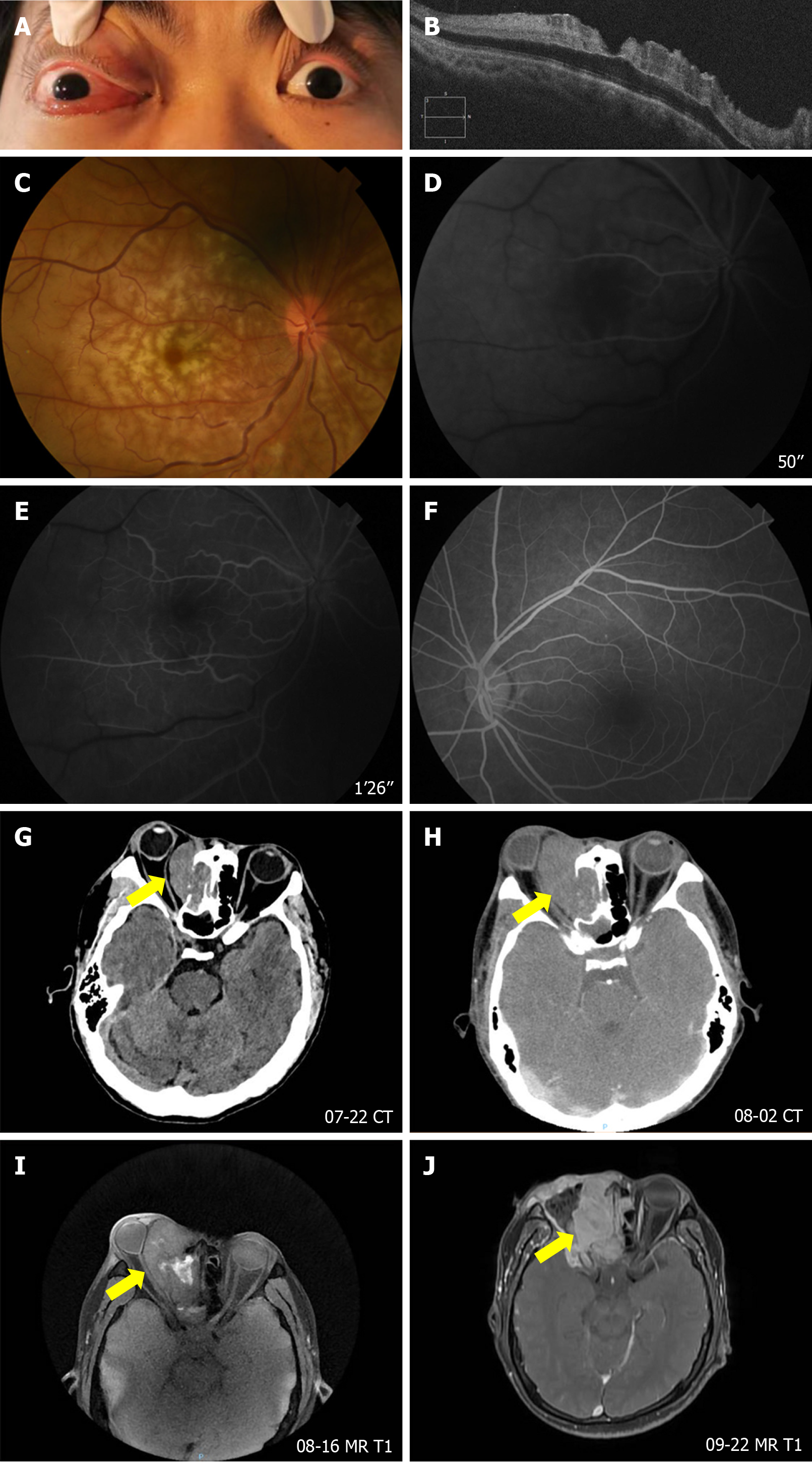
Ophthalmic examination revealed a visual acuity of 0.1 in the right eye compared with 0.9 in the left eye and intraocular pressure of 40 mmHg in the right eye compared with 16 mmHg in the left eye. The right eye exhibited proptosis, restricted mobility, significant eyelid congestion and swelling and conjunctival edema (Figure 1A). Optical coherence tomography of the right eye revealed augmented reflectance within the neuroepithelial layer of the macula and diffuse thickening of the retinal layers (Figure 1B). Fundoscopic examination of the right eye revealed tortuous retinal vessels, gray-white retinal edema, and a cherry-red spot in the macula (Figure 1C). Additionally, fundus fluorescein angiography demonstrated delayed filling of retinal arterial and venous blood flow in the right eye, whereas the left eye exhibited normal angiographic findings. This observation was consistent with a diagnosis of CRAO (Figure 1D-F).
Upon admission, a comprehensive evaluation was conducted, revealing elevations in blood viscosity at high and medium shear rates, as well as an increased erythrocyte electrophoresis index. Routine blood tests, urine tests, biochemical function tests, coagulation tests, and cerebrospinal fluid examinations revealed no abnormalities. Additionally, chest anteroposterior and lateral radiographs and electrocardiogram examinations revealed no abnormalities.
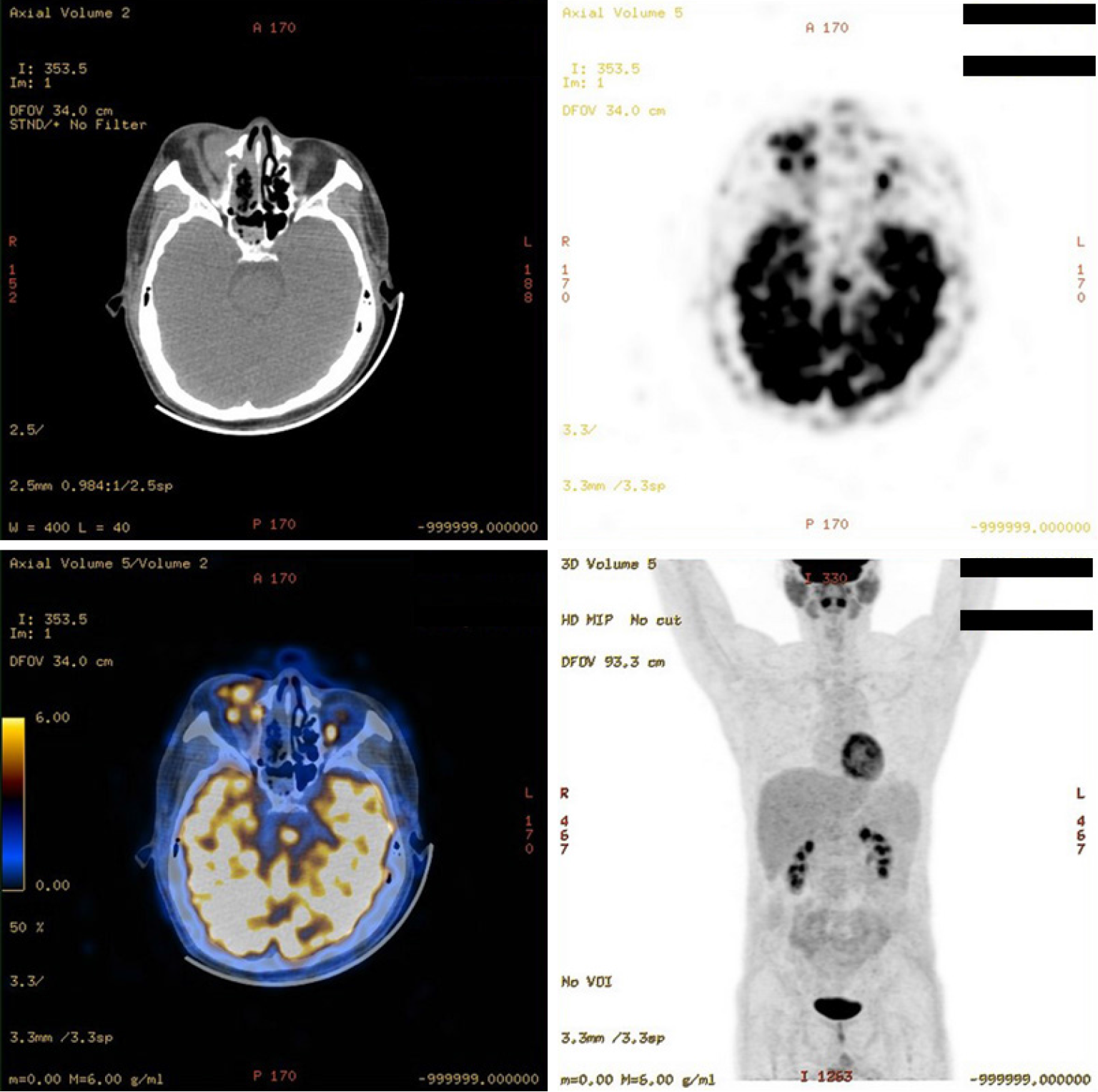
A computed tomography (CT) scan of the orbit, conducted after admission to the hospital, revealed a heterogeneous, slightly hyperdense mass in the right maxillary sinus-orbital-frontal region, with associated bone destruction and compression of the right medial rectus muscle and optic nerve, with progressive enlargement observed over time (Figure 1G and H). Enhanced magnetic resonance imaging (MRI) since the first operation revealed an irregular signal shadow on the right side with indistinct boundaries, and T2-weighted imaging revealed a mildly mixed signal (Figure 1I). Positron emission tomography/CT revealed a right orbital and frontal lesion demonstrating increased glucose metabo
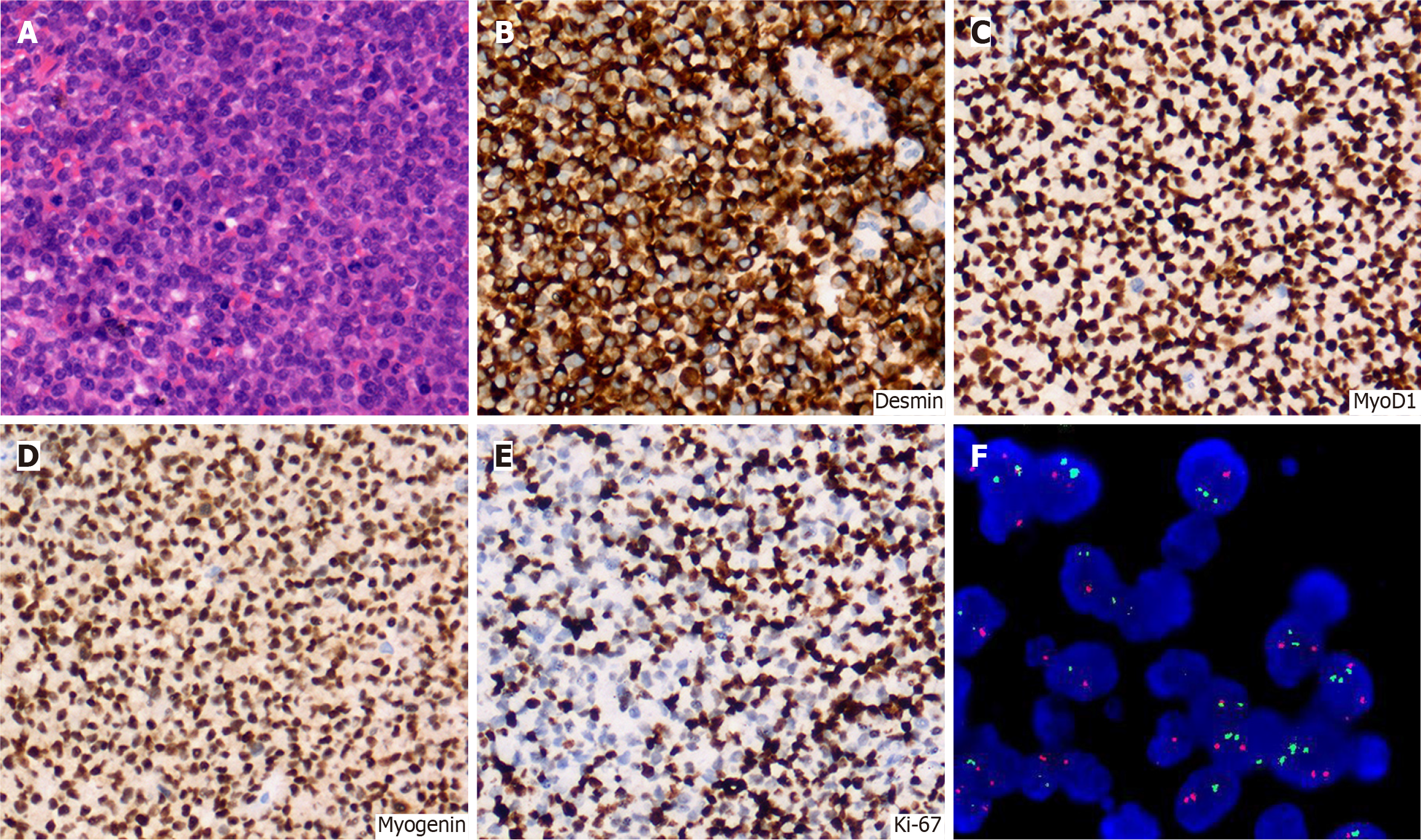
The patient underwent endoscopic resection of the tumor involving the right paranasal sinus and orbit. During the procedure, a portion of the ethmoid sinus tumor was clamped for pathological biopsy. Microscopic examination of the pathological specimen revealed solid sheets and nests of neoplastic cells infiltrating the stroma, resembling small round blue cells (Figure 3A). Immunohistochemistry results were positive for Desmin, MyoD1, Myogenin, CD56, and Ki-67 (approximately 50%) (Figure 3B-E). The fluorescence in situ hybridization (FISH) assay yielded positive results, indicating breaks in the EWSR1 gene, with 82% exhibiting separation of red and green signals, significantly exceeding the 15% threshold (Figure 3F).
Many sarcomas classified as "small round blue cell tumors" exhibit round cells with a distinctive appearance but often lack distinguishing features visible through optical microscopy. Combining the immunohistochemical results with tissue biopsy findings allowed for the exclusion of other tumor types, making the diagnosis of ARMS the most likely. However, a definitive diagnosis requires further genetic testing. FISH analysis revealed a break in the EWSR1 gene but didn’t specify which gene EWSR1 was fused with. Detection of the PAX3-FOXO1 or PAX7-FOXO1 fusion genes, while in
Since the patient only received palliative care and no other treatments, we briefly described the operation performed on the patient in the article.
The patient's pain experienced marked attenuation. Regrettably, due to financial constraints, the patient opted to forego further chemotherapy and radiation therapy.
RMS, a prototypical mesenchymal-originating malignancy, is commonly postulated to originate from the developmental hierarchy of skeletal muscle precursor cells. According to the World Health Organization's classification of soft tissue and bone tumors, RMS is categorized into embryonal, alveolar, pleomorphic, and spindle cell/sclerosing subtypes[1]. Notably, ARMS, characterized by a high degree of malignancy and an unfavorable prognosis, can be definitively diagnosed through histopathological examination, with the tumor tissue exhibiting undifferentiated small round blue cells arranged in an alveolar pattern[1]. RMS has the potential to manifest in any region of the body; however, it has a particular predilection for the head and neck area, with possible occurrences in the orbit, periorbital areas and non-periorbital areas. RMS in the head and neck is relatively rare in adults and is typically associated with a poor prognosis[4]. Symptoms of orbital RMS frequently include severe eye pain, proptosis, and visual impairment; however, the specific cause of underlying vision loss is infrequently reported. Diagnosing RMS poses significant challenges and primarily depends on radiographic studies, histopathological biopsies, and immunohistochemistry[5,6]. Treatment regimens for RMS adhere to a standard multimodal strategy, encompassing surgical resection, radiation therapy, and chemotherapy[1].
CRAO is defined by abrupt blockage of the central retinal artery, resulting in inadequate retinal perfusion, swift and progressive cellular deterioration, and subsequent visual impairment[2]. The predominant cause of CRAO is platelet-fibrin thrombi and emboli originating from atherosclerotic disease, which account for more than two-thirds of all cases. Externally compressive forces exerted on the vessel wall, such as those from trauma, surgery, or hematoma after retrobulbar anesthesia, can also precipitate CRAO. Additionally, neoplasms have the potential to induce vascular occlusion[7,8]. Upon ophthalmoscopic examination, the retina manifests as diffusely pale with centrally located cherry red spots. Prompt diagnosis and expeditious intervention aimed at eliminating or dissolving the obstructive embolus or thrombus are imperative to prevent irreversible retinal injury and mitigate the risk of blindness[2].
In the present case, the origin of the embolus causing the CRAO was undetermined. The embolus could be attributed to hemodynamic alterations due to tumor compression and resultant endothelial damage, leading to thrombosis, or a hypercoagulable state induced by the malignancy[8,9]. Previously, a case of CRAO was attributed to retinal melanoma. Tumor growth and subsequent necrosis caused vascular occlusion, resulting in severe visual loss[10]. Similarly, exo
ARMS and CRAO in younger individuals are relatively rare. Here, we report a young adult patient with orbital and sinus RMS complicated by CRAO. The purpose of this study is to increase awareness of similar cases and assist clinicians in timely and accurate diagnosis and effective treatment, ultimately improving patient outcomes and the management of this complex condition.
| 1. | Zarrabi A, Perrin D, Kavoosi M, Sommer M, Sezen S, Mehrbod P, Bhushan B, Machaj F, Rosik J, Kawalec P, Afifi S, Bolandi SM, Koleini P, Taheri M, Madrakian T, Łos MJ, Lindsey B, Cakir N, Zarepour A, Hushmandi K, Fallah A, Koc B, Khosravi A, Ahmadi M, Logue S, Orive G, Pecic S, Gordon JW, Ghavami S. Rhabdomyosarcoma: Current Therapy, Challenges, and Future Approaches to Treatment Strategies. Cancers (Basel). 2023;15:5269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 2. | Liu W, Bai D, Kou L. Progress in central retinal artery occlusion: a narrative review. J Int Med Res. 2023;51:3000605231198388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 3. | Brown GC, Magargal LE, Shields JA, Goldberg RE, Walsh PN. Retinal arterial obstruction in children and young adults. Ophthalmology. 1981;88:18-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 166] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Lofgren DH, Gillette B, Knight BB, Succar E. Induction Chemotherapy Prior to Endoscopic Resection of Alveolar Rhabdomyosarcoma. Cureus. 2023;15:e48761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Rodriguez-Beato F, De Jesus O, Sanchez-Ortiz J, Delgado P, Perez-Berenguer JL, Labat EJ. Alveolar rhabdomyosarcoma metastatic to the brain. BMJ Case Rep. 2021;14:e240516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Jawad N, McHugh K. The clinical and radiologic features of paediatric rhabdomyosarcoma. Pediatr Radiol. 2019;49:1516-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Ansari-Astaneh MR, Raoufi F, Shokoohirad S, Shoeibi N, Abrishami M. Central Retinal Artery Occlusion after Rhinoplasty Surgery: A Case Report and Literature Review. Case Rep Ophthalmol Med. 2022;2022:9997298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 8. | Rubin PA, Rumelt S. Central retinal artery occlusion due to rapidly expanding orbital lymphoma. Eye (Lond). 1998;12 (Pt 1):159-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Kim MS, Byun SJ, Woo SJ, Park KH, Park SJ. A 12-year nationwide cohort study on the association between central retinal artery occlusion and cancer. Graefes Arch Clin Exp Ophthalmol. 2023;261:1893-1900. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Khadka S, Byanju R, Pradhan S. Central retinal artery occlusion in optic disk melanocytoma. Clin Case Rep. 2021;9:e04927. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Carey AR. Central Retinal Artery Occlusion Due to Intraorbital Ophthalmic Artery Aneurysm. J Neuroophthalmol. 2019;39:125-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Takeuchi Y, Nakahara K, Nakajima M, Inoue Y, Matsumura R, Yamaguchi M, Katabuchi H, Ando Y. A 23-Year-Old Woman with Sudden-Onset Blindness of the Right Eye. J Stroke Cerebrovasc Dis. 2019;28:e12-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |