Published online Dec 24, 2024. doi: 10.5306/wjco.v15.i12.1491
Revised: September 5, 2024
Accepted: October 14, 2024
Published online: December 24, 2024
Processing time: 82 Days and 22.7 Hours
Cervical cancer is the second leading cause of death in women worldwide, second only to breast cancer. Around 80% of women have been infected with human papillomavirus (HPV) in their lifetime. Early screening and treatment are effective means of preventing cervical cancer, but due to economic reasons, many parts of the world do not have free screening programs to protect women’s health.
To increase HPV cervical cancer screening in Changsha and reduce the incidence of cervical cancer.
Cervical cancer screening included gynecological examination, vaginal secretion examination and HPV high-risk typing testing. Cervical cytology examination (ThinPrep cytology test) was performed for individuals who test positive for HPV types other than 16 and 18. Vaginal colposcopy examination was performed for HPV16 and 18 positive individuals, as well as for those who were positive for ThinPrep cytology test. If the results of vaginal colposcopy examination were abnormal, histopathological examination was performed. We conducted a cost-benefit analysis after 4 years.
From 2019 to 2022, 523437 women aged 35-64 years in Changsha city were screened and 73313 were positive, with a 14% positive rate. The detection rate of precancerous lesions of cervical cancer was 0.6% and the detection rate of cervical cancer was 0.037%. Among 311212 patients who underwent two cancers examinations, the incidence rate was reduced by more than half in the second examination. The average screening cost per woman was 120 RMB. The average cost of detecting early cases was 10619 RMB, with an early detection cost coefficient of 0.083.
Our screening strategy was effective and cost-effective, making it valuable for early diagnosis and treatment of cervical cancer. It is worth promoting in economically limited areas.
Core Tip: With limited funds, we designed a new strategy for human papillomavirus screening for all women in Changsha every 3 years, to increase screening coverage and reduce the incidence of cervical cancer. From 2019 to 2022, 523437 women aged 35-64 years were screened and there were 73313 human papillomavirus-positive women, with a 14% positive rate. The detection rate of precancerous lesions of cervical cancer was 0.6% and the detection rate of cervical cancer was 0.037%. The average screening cost per woman is 120 RMB, with an early detection cost coefficient of 0.15. Our screening strategy was effective and cost-effective.
- Citation: Zu YE, Wang SF, Peng XX, Wen YC, Shen XX, Wang XL, Liao WB, Jia D, Liu JY, Peng XW. New cheaper human papilloma virus mass screening strategy reduces cervical cancer incidence in Changsha city: A clinical trial. World J Clin Oncol 2024; 15(12): 1491-1500
- URL: https://www.wjgnet.com/2218-4333/full/v15/i12/1491.htm
- DOI: https://dx.doi.org/10.5306/wjco.v15.i12.1491
Cervical cancer is a leading cause of death in women with 530000 new cases and 275000 deaths worldwide each year[1]. The overall incidence of cervical cancer ranges from 7.5 cases per 100000 to 75.9 per 1000001[1]. About 630000 new cancers worldwide may be attributed to human papillomavirus (HPV) infection, including cervical and other cancers of the reproductive tract, with cervical cancer accounting for the highest proportion[2]. Most HPV infections are transient, but there are many HPV subtypes that are high-risk: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68. Medium-risk HPVs are 26, 53, 66, 73, and 82[3]. A meta-analysis of 423 studies from around the world showed that among 115789 HPV-positive women, HPV infection rates were 76% for women with low-grade cervical lesions and 85% for women with high-grade cervical lesions. In cervical lesions and cervical cancer, HPV16/18/31/33/45/52/58 were common[4]. An epidemiological study of HPV infection in 1.7 million women in China showed that the overall HPV infection rate in Chinese women was 15.54%, and the top five common HPV infection types were 16 (3.52%), 52 (2.20%), 58 (2.10%), 18 (1.20%) and 33 (1.02%). A multicenter study conducted in seven regions in China showed that HPV16/18/31/52/58 were the most common in cervical squamous cell carcinoma, with infection rates of 76.7%, 7.8%, 3.2%, 2.2% and 2.2%, respectively[5]. The prevalence of HPV16/18 in China is significantly higher than the global level of high-grade and low-grade cervical lesions and cervical cancer. According to the 2019 ICO China HPV and Related Diseases Report, HPV16/18 causes about 69% of cervical cancer in China; HPV types 31/33/45/52/58 cause about 23% of cervical cancers[5]. HPV screening is an effective means to prevent cervical cancer development. According to American Cancer Society 2020 guidelines, there are various screening strategies for cervical cancer, and authoritative recommended institutions include the World Health Organization, American Society of Vaginal and Cervical Pathology, and European Organization for Research on Genital Infections and Tumors. The main screening strategies are a combination of cytology and HPV screening, cytology screening, and HPV screening. The key point of screening is that women who have sex begin screening after the age of 21 years. Those who are negative for cytology and high-risk HPV screening have a low risk of cancer, and the screening interval is 3-5 years. The risk of cancer is increased in women who are negative for cytology and positive for HPV screening, which can be reviewed 1 year later. Those with atypical squamous cells of undetermined significance or above and positive for HPV, or low-grade squamous intraepithelial lesion or above, or positive for HPV16 or 18 need co
The inspection object must meet one of the following conditions: (1) Women aged 35-64 years who have not participated in the national, provincial and municipal cervical carcinoma free examinations from 2019 to 2022, and have a registered residence or residence permit in Changsha; and (2) Women who are found to be positive for HPV16 and 18 through free cervical carcinoma testing in 2019-2022 are eligible to participate in the free cervical carcinoma testing for eligible women in Changsha in 2024.
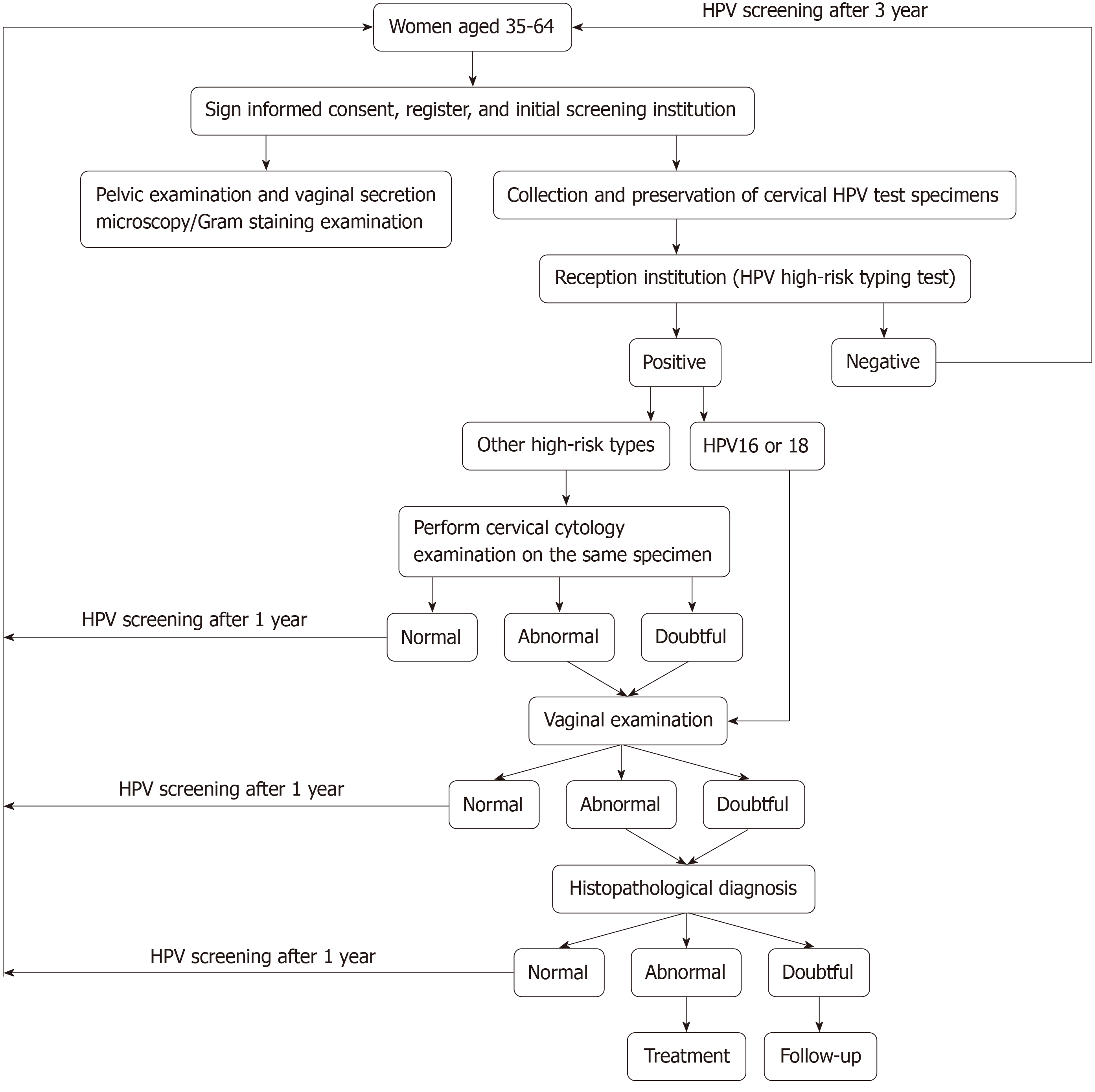
Cervical cancer screening included gynecological examination, vaginal secretion examination, and testing for high-risk HPV types. Cervical cytological examination (TCT) was performed for women who tested positive for HPV types other than 16 and 18. Vaginal colposcopy was performed for women who tested positive for HPV16 and 18, as well as for those who tested positive for TCT. If vaginal colposcopy examination was abnormal, histopathological examination was performed. The detailed process is shown in Figure 1.
All women who were screened in 2019-2022 were counted to calculate the average cost, incidence rate and detection rate. Early case detection cost (RMB) = total examination cost/number of early diagnosed patients. EDCI = average cost of detecting early cases/per capita GDP. Women aged 35-64 years were enrolled for HPV screening every 3 years. For women positive for high-risk subtypes HPV16 and 18, we performed colposcopy. For other subtypes of HPV, we performed TCT and positive individuals were examined with colposcopy. If colposcopy results were abnormal, his
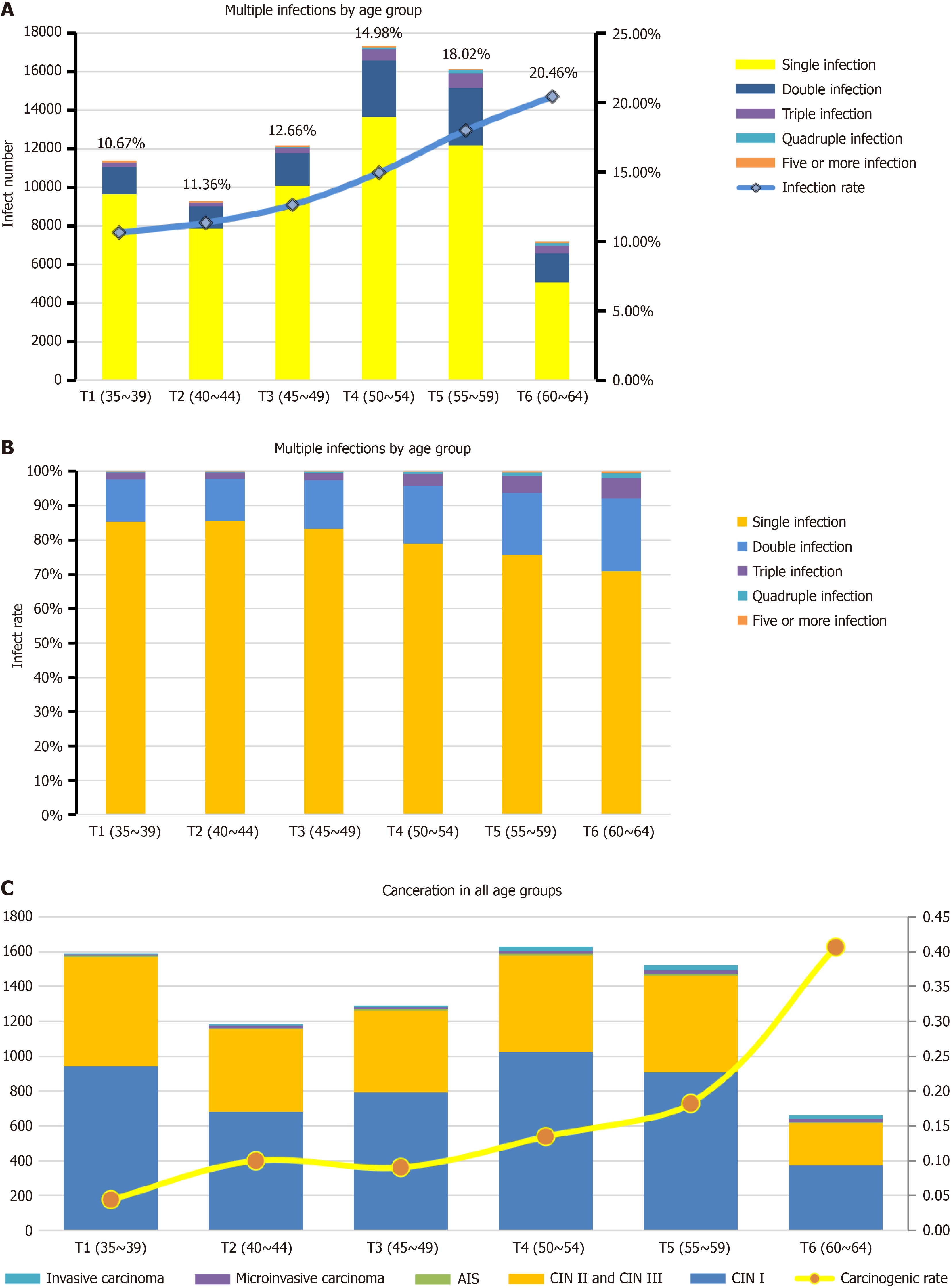
From 2019 to 2022, 523437 women aged 35-64 years in Changsha city were screened. The infection rate increased from 10.67% in women aged 35-39 years to 20.45% in women aged 60-64 years (Figure 2A). Consistent with other parts of China, the main infection was single and single infection rate in Changsha was > 70%[7-9]. However, we found that the multiple infection rate decreased with increase of age, from 85% in women aged 35-39 years to 71% in women aged 60-64 years (Figure 2B). In contrast, the carcinogenic rate increased from 0.04% in the younger group to 0.41% in the older group (Figure 2C).
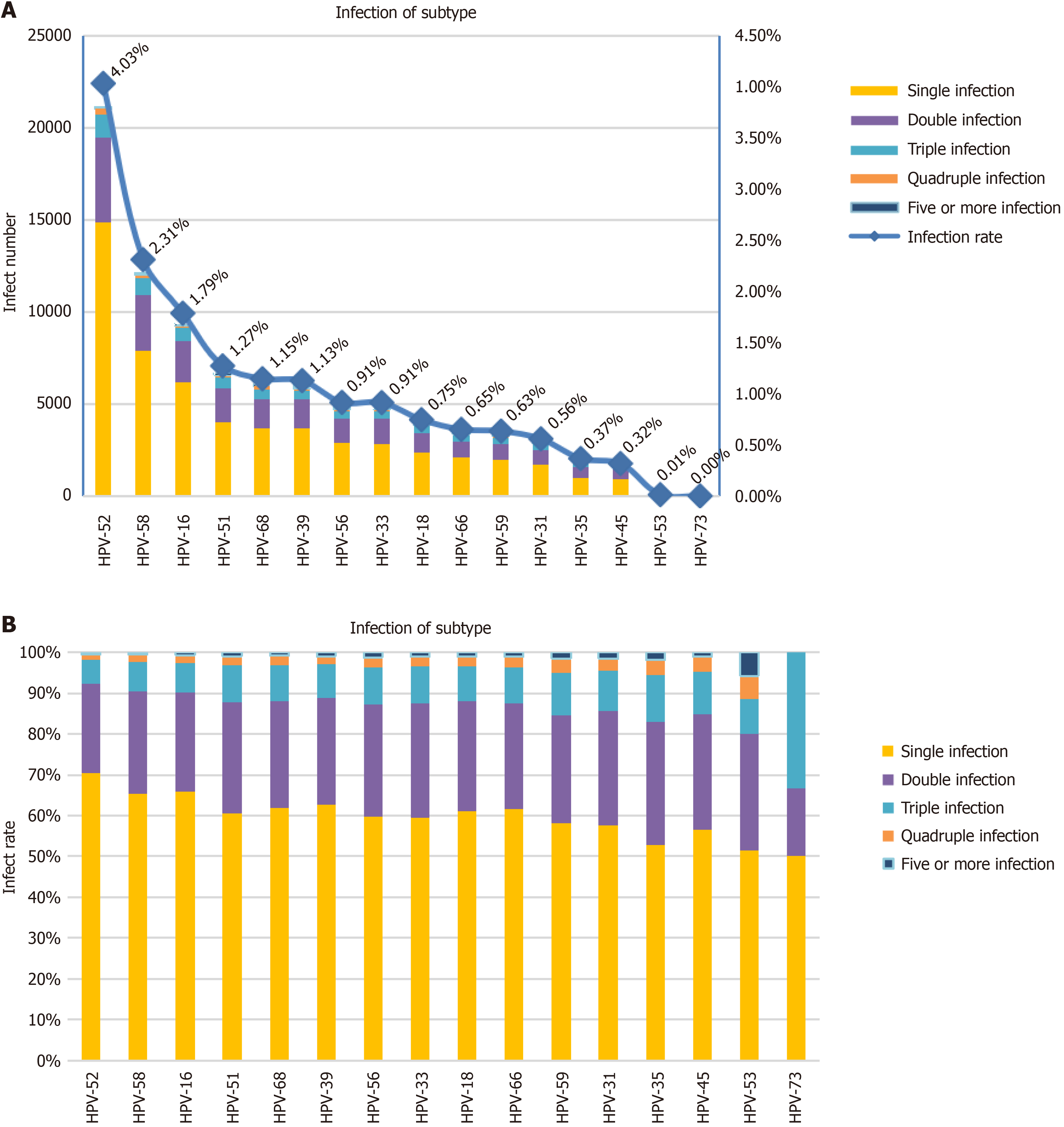
Among 52337 women, 73313 were infected with HPV, with a 14% positive rate. The infection rates of various HPV subtypes were 52 (4.03%), 58 (2.31%), 16 (1.79%), 51 (1.27%), 68 (1.15%), 39 (1.13%), 56 (0.91%), 33 (0.91%), 18 (0.75%), 66 (0.65%) and 59 (0.63%) (Figure 3A). Most cases were single infection (> 70%) or double infection (Figure 3B).
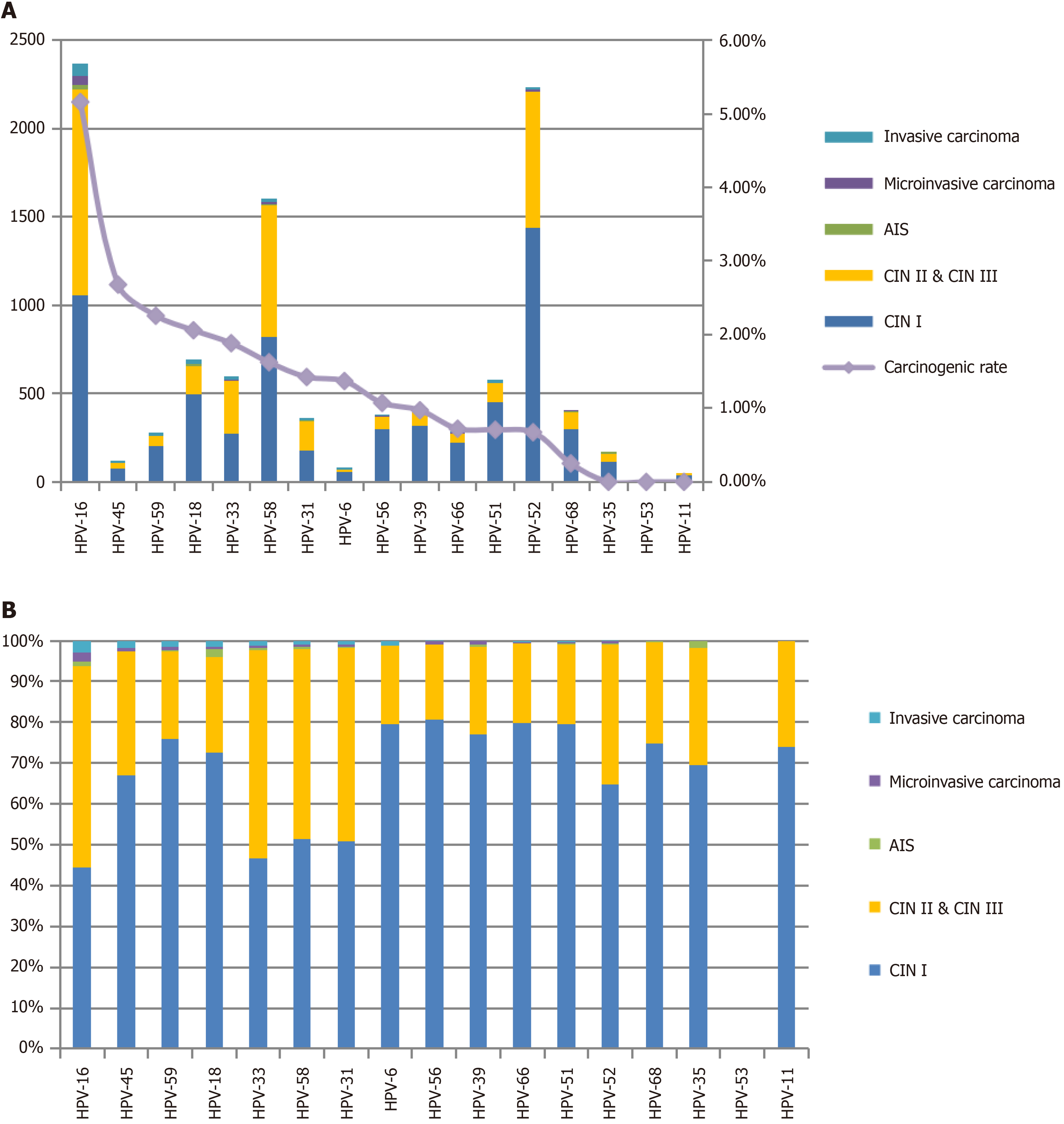
Cytological changes were observed in 10490 of the 73313 HPV-infected women, including 6329 with cervical intraepithelial neoplasia (CINI), 3879 with CINII and CINIII, 64 with adenocarcinoma in situ, 99 with microinvasive carcinoma, and 119 with invasive carcinoma. The rate of early diagnosis of cervical cancer was 98.87%, the detection rate of precancerous lesions of cervical cancer was 0.6%, and the detection rate of cervical cancer was 36.878 per 100000. The top three subtypes were HPV16, HPV52 and HPV58. The subtypes that caused cancer, from high to low, were HPV16, HPV45, HPV59, HPV18, HPV33, HPV58, HPV31, HPV6, HPV56 and HPV39 (Figure 4A and B). Although the infection rate of HPV59 was only 3.88%, its carcinogenic rate was as high as 2.26%. Since HPV59 is not covered by a nine-valent vaccine, our results suggest that a vaccine corresponding to HPV59 may be needed.
As HPV18 and HPV16 were the highest-risk subtypes, we performed colposcopy without cytological examination for positive patients to avoid missed diagnosis caused by specimen collection and false-positive or -negative results of TCT. Colposcopy is 114 RMB cheaper than TCT; therefore, our strategy saved 2739306 RMB for 24029 HPV16/18 infections in 4 years. The early diagnosis rates for HPV16 and HPV18 were 97.17% and 98.53%, respectively, which was comparable to the rate of early diagnosis of cervical cancer (98.87%), which showed no significant difference compared with other subtypes. This indicates that colposcopy without TCT is an economic and feasible option for HPV16- and HPV18-positive patients.
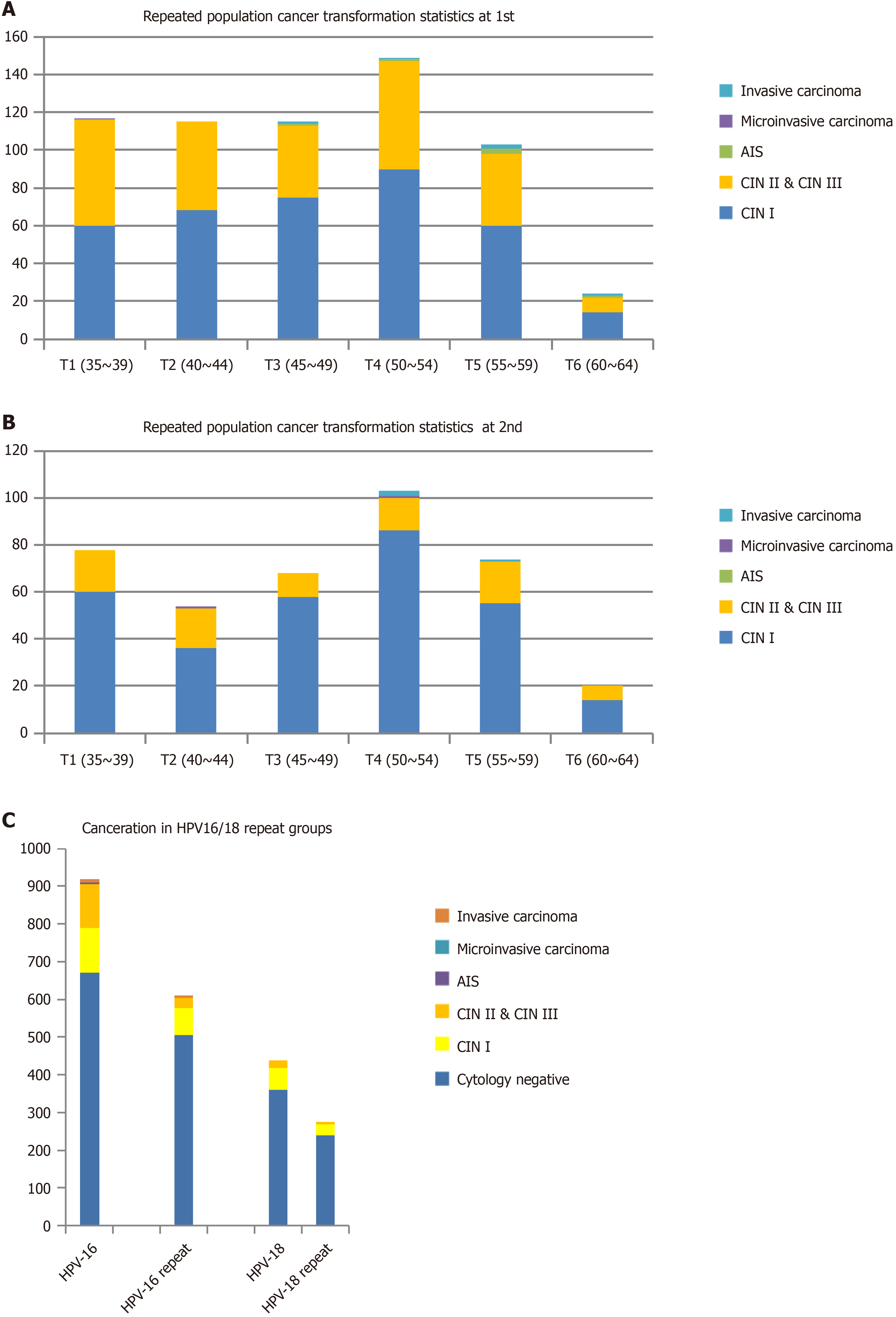
Our program ran for 4 years, and 311212 people were screened twice in 2022. We compared the two results and found that the number of cervical squamous epithelial lesions was significantly reduced, the number of CINII and CINIII lesions was reduced from 244 to 83, and the number of women with cancer was reduced from 12 to five (Figure 5A and B). When we compared the two results for HPV16/18-positive women, the number of CINII and CINIII lesions and women with cancer were also decreased significantly (Figure 5C). This indicates that colposcopy without TCT is an economic and feasible method for HPV16/18-positive patients. During the second examination, we found two HPV16-positive patients with invasive carcinoma. One was negative for HPV16 at the first examination and the other was HPV16 positive and had CINI lesions. This indicates that some women infected with HPV16 developed cancer rapidly and treatment and screening of cervical cancer should be conducted every year after infection. Therefore, we changed the screening strategy for HPV16/18-positive patients to once a year after 2023.
The per capita cost of testing was 120 RMB. The average cost of detecting early cases was 10619 RMB, and EDCI was 0.83. The smaller the EDCI, the more healthy life years were obtained from per capita GDP investment. When EDCI was < 10, screening was considered cost-effective. When EDCI was < 5, early diagnosis and treatment of cancer were considered highly cost-effective (Table 1).
| Total cost | Screening population | Per capita cost | Number of early diagnoses | 4 years per capita GDP | The average cost of detecting early cases | EDCI |
| 62812440 | 523437 | 120 RMB | 5915 | 127850 | 10619 | 0.083 |
Cytology-based cervical screening has had unequivocal success in reducing the incidence and mortality of cervical cancer in the last century[10]. Based on American Cancer Society 2020 guidelines, the strategy of HPV testing in combination with cytology examination is recommended[11]. In our strategy we combined primary human HPV testing with colposcopy in women with high-risk subtypes HPV16/18, for which early diagnosis rates showed no difference from other subtypes. Our results indicate that countries and regions with limited budgets could benefit from adopting our economically viable strategy. In Changsha city, infection rates and multiple infections increased with age, which was also found in other areas[12-16]. The highest infection rates were with HPV52, 58 and 16, but the highest carcinogenicity was with HPV16, 45 and 59[17-20]. HPV59 is not covered by the nine-valent vaccine; therefore, this subtype should be paid more attention in HPV screening.
The carcinogenic rates also increased with age. In women aged 60-65 years, the rate was 0.41%, compared with 0.04% in women aged 35-39 years. After the second screening, two HPV16-positive women with invasive carcinoma were negative on the first screening. This indicates that women aged 60-65 years need to pay more attention to examination for cervical cancer when infected with HPV16. Therefore, we propose to change the screening strategy for HPV16/18-positive patients to once a year.
For women not infected with HPV, our protocol does not include TCT screening, which may result in missed detection of cervical cancer unrelated to HPV. Despite offering free screening, participation in HPV screening among women of appropriate age is hindered by various factors such as cultural influences, education levels, public awareness, and individual beliefs. Although our strategy is limited, we have saved the cost of TCT for HPV-uninfected and HPV16/18 women (usually 200-250 yuan per person), so we can cover more people with this cost. Therefore, it is worth sacrificing some diagnostic accuracy for public health screening strategies.
Our screening strategy was effective and cost-effective, making it valuable for early diagnosis and treatment of cervical cancer. It is worth promoting in economically limited areas.
We thank all the persons who have made genuine contributions to the manuscript collected the data.
| 1. | Morse R, Brown J, Ríos López EJ, Prieto BA, Kohler-Smith A, Gonzales Díaz K, Figueredo Escudero M, Del Cuadro DL, Vásquez Del Aguila G, Daza Grandez H, Meza G, Tracy JK, Gravitt PE, Paz-Soldan VA; Proyecto Precancer Study Group. Challenges associated with follow-up care after implementation of an HPV screen-and-treat program with ablative therapy for cervical cancer prevention in Iquitos, Peru: a mixed methods study. Res Sq. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141:664-670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1331] [Cited by in RCA: 1516] [Article Influence: 189.5] [Reference Citation Analysis (0)] |
| 3. | World Health Organization. Human papillomavirus vaccines: WHO position paper, May 2017-Recommendations. Vaccine. 2017;35:5753-5755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 239] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 4. | Guan P, Howell-Jones R, Li N, Bruni L, de Sanjosé S, Franceschi S, Clifford GM. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer. 2012;131:2349-2359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 558] [Cited by in RCA: 687] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 5. | Chen W, Zhang X, Molijn A, Jenkins D, Shi JF, Quint W, Schmidt JE, Wang P, Liu YL, Li LK, Shi H, Liu JH, Xie X, Niyazi M, Yang P, Wei LH, Li LY, Li J, Liu JF, Zhou Q, Hong Y, Li L, Li Q, Zhou HL, Bian ML, Chen J, Qiao YL, Smith JS. Human papillomavirus type-distribution in cervical cancer in China: the importance of HPV 16 and 18. Cancer Causes Control. 2009;20:1705-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 91] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Saslow D, Andrews KS, Manassaram-Baptiste D, Smith RA, Fontham ETH; American Cancer Society Guideline Development Group. Human papillomavirus vaccination 2020 guideline update: American Cancer Society guideline adaptation. CA Cancer J Clin. 2020;70:274-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 110] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 7. | Lo KW, Wong YF, Chan MK, Li JC, Poon JS, Wang VW, Zhu SN, Zhang TM, He ZG, Wu QL, Li GD, Tam JS, Kahn T, Lam P, Cheung TH, Chung TK. Prevalence of human papillomavirus in cervical cancer: a multicenter study in China. Int J Cancer. 2002;100:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Liu L, Wang D, Dong H, Jin C, Jiang L, Song H, Jin C, Wang T, Shi C, Yang L, Wang Y. Characteristics of carcinogenic HPV genotypes in North China Plain and the association with cervical lesions. Medicine (Baltimore). 2019;98:e17087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Lin X, Chen L, Zheng Y, Yan F, Li J, Zhang J, Yang H. Age-specific prevalence and genotype distribution of human papillomavirus in women from Northwest China. Cancer Med. 2022;11:4366-4373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Strickler HD, Keller MJ, Hessol NA, Eltoum IE, Einstein MH, Castle PE, Massad LS, Flowers L, Rahangdale L, Atrio JM, Ramirez C, Minkoff H, Adimora AA, Ofotokun I, Colie C, Huchko MJ, Fischl M, Wright R, D'Souza G, Leider J, Diaz O, Sanchez-Keeland L, Shrestha S, Xie X, Xue X, Anastos K, Palefsky JM, Burk RD. Primary HPV and Molecular Cervical Cancer Screening in US Women Living With Human Immunodeficiency Virus. Clin Infect Dis. 2021;72:1529-1537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Fontham ETH, Wolf AMD, Church TR, Etzioni R, Flowers CR, Herzig A, Guerra CE, Oeffinger KC, Shih YT, Walter LC, Kim JJ, Andrews KS, DeSantis CE, Fedewa SA, Manassaram-Baptiste D, Saslow D, Wender RC, Smith RA. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70:321-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 543] [Article Influence: 108.6] [Reference Citation Analysis (0)] |
| 12. | Smith EM, Johnson SR, Ritchie JM, Feddersen D, Wang D, Turek LP, Haugen TH. Persistent HPV infection in postmenopausal age women. Int J Gynaecol Obstet. 2004;87:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | De Vuyst H, Clifford G, Li N, Franceschi S. HPV infection in Europe. Eur J Cancer. 2009;45:2632-2639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 125] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 14. | Muderris T, Afsar I, Yıldız A, Akpınar Varer C. HPV genotype distribution among women with normal and abnormal cervical cytology in Turkey. Rev Esp Quimioter. 2019;32:516-524. [PubMed] |
| 15. | Yan X, Shen L, Xiao Y, Wang Q, Li F, Qian Y. Prevalence, characteristics, and distribution of HPV genotypes in women from Zhejiang Province, 2016-2020. Virol J. 2021;18:208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 16. | Serretiello E, Corrado F, Santella B, Chianese A, Iervolino D, Coppola A, Grimaldi E, Galdiero M, Franci G. Prevalence and Distribution of High- and Low- Risk HPV Genotypes in Women Living in the Metropolitan Area of Naples: A Recent Update. Asian Pac J Cancer Prev. 2023;24:435-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 17. | Damgaard RK, Jenkins D, Stoler MH, van de Sandt MM, Lycke KD, de Koning MNC, Quint WGV, Steiniche T, Petersen LK, Hammer A. High prevalence of HPV16 and high-grade cytology in women undergoing active surveillance for cervical intraepithelial neoplasia grade 2. Acta Obstet Gynecol Scand. 2023;102:1227-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 18. | Camacho-Ureta EA, Mendez-Martínez RS, Vázquez-Vega S, Martínez UO, Arenas RS, Castillo-Ureta H, Ramírez IO, Torres Montoya EH, López Moreno HS, García-Carranca A, Rendón-Maldonado JG. High frequency of HPV16 European variant E350G among Mexican women from Sinaloa. Indian J Med Res. 2018;148:323-328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Ye F, Chan N, Feng T, Wu J, Jiang S, Sperling R, Zhang DY. High prevalence of HPV59 in cytologically abnormal cervical samples. Exp Mol Pathol. 2015;99:611-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Long W, Yang Z, Li X, Chen M, Liu J, Zhang Y, Sun X. HPV-16, HPV-58, and HPV-33 are the most carcinogenic HPV genotypes in Southwestern China and their viral loads are associated with severity of premalignant lesions in the cervix. Virol J. 2018;15:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |