Published online Jan 24, 2024. doi: 10.5306/wjco.v15.i1.9
Peer-review started: October 27, 2023
First decision: November 11, 2023
Revised: November 24, 2023
Accepted: December 19, 2023
Article in press: December 19, 2023
Published online: January 24, 2024
Processing time: 87 Days and 14.5 Hours
Chronic inflammation is known to increase the risk of gastrointestinal cancers (GICs), the common solid tumors worldwide. Precancerous lesions, such as chronic atrophic inflammation and ulcers, are related to inflammatory responses in vivo and likely to occur in hyperplasia and tumorigenesis. Unfortunately, due to the lack of effective therapeutic targets, the prognosis of patients with GICs is still unsatisfactory. Interestingly, it is found that six transmembrane epithelial antigens of the prostate (STEAPs), a group of metal reductases, are significantly associated with the progression of malignancies, playing a crucial role in systemic metabolic homeostasis and inflammatory responses. The structure and functions of STEAPs suggest that they are closely related to intracellular oxidative stress, responding to inflammatory reactions. Under the imbalance status of abnormal oxidative stress, STEAP members are involved in cell transformation and the development of GICs by inhibiting or activating inflammatory process. This review focuses on STEAPs in GICs along with exploring their potential molecular regulatory mechanisms, with an aim to provide a theoretical basis for diagnosis and treatment strategies for patients suffering from these types of cancers.
Core Tip: Six transmembrane epithelial antigens of the prostate (STEAPs), a group of metal reductases, are closely related to intracellular oxidative stress, responding to an inflammatory reaction, while chronic inflammation is known to increase the risk of gastrointestinal cancers (GICs). This review of STEAPs in GICs provides a theoretical basis for diagnosis and treatment strategies for patients.
- Citation: Fang ZX, Chen WJ, Wu Z, Hou YY, Lan YZ, Wu HT, Liu J. Inflammatory response in gastrointestinal cancers: Overview of six transmembrane epithelial antigens of the prostate in pathophysiology and clinical implications. World J Clin Oncol 2024; 15(1): 9-22
- URL: https://www.wjgnet.com/2218-4333/full/v15/i1/9.htm
- DOI: https://dx.doi.org/10.5306/wjco.v15.i1.9
Gastrointestinal cancers (GICs), such as colorectal cancer (CRC), gastric cancer (GC), and hepatocellular carcinoma (HCC), are one of the leading causes of cancer-related death worldwide, with many cases and wide lesions. Among them, CRC is not only the fourth most common malignancy but also the third main cause of cancer-related death in the United States[1]. GC is the fifth most common cancer and the third leading cause of cancer-related death worldwide[2], while HCC accounts for 90% of liver cancer with 850000 new cases each year[3]. Although effective colonoscopy and upper endoscopy screening can detect precancerous polyps and precancerous lesions in the gastrointestinal tract, many patients have an advanced stage at their first diagnosis and a poor prognosis with current treatment methods[4].
The gastrointestinal tract is exposed to diverse foods and/or drugs daily, which may be related to various degrees of inflammatory response and kinds of diseases. Chronic inflammation is a well-established risk factor for GICs, which is also the molecular and pathophysiological basis of gastritis, inflammatory bowel disease (IBD), and upper and lower GICs[5]. Chronic inflammation initiates tumorigenesis, and mechanisms by which tumor-induced and treatment-related inflammatory processes interact with cancer cells support that inflammatory responses may be closely related to the oncogenesis and/or development of GICs[6]. Inflammatory features involved in the development of CRCs include inflammasome activation and noncanonical nuclear factor-kappaB (NF-κB) pathway activation mediating the production of proinflammatory cytokines, both of which can be activated by changes in the mutant environment or stimulation by microorganisms such as the gut microbiota[7,8]. And smoking, alcohol consumption, various infections, susceptibility gene mutations, and epigenetic changes are associated with the occurrence of GICs[9-11]. Due to the high incidence rates and poor prognosis associated with GICs globally, they represent a significant public health challenge[12].
Recently, the six transmembrane epithelial antigen of the prostate (STEAP) family, a group of key metal oxidoreductases, has been associated with the overexpression of a range of proinflammatory cytokines[13], which are considered promising therapeutic targets for various cancers, especially prostate cancer, due to their role in regulating proinflammatory cytokines[14-16]. However, Gomes et al[17] also found that the localization of STEAPs on the cell membrane and their differential expression in normal tissues and gastric, colorectal, and liver cancers make them promising potential targets for the treatment of GICs. Therefore, this review aims to explore the role of STEAPs in inflammatory responses in GICs and provide a new strategy for the prevention and early intervention of GICs.
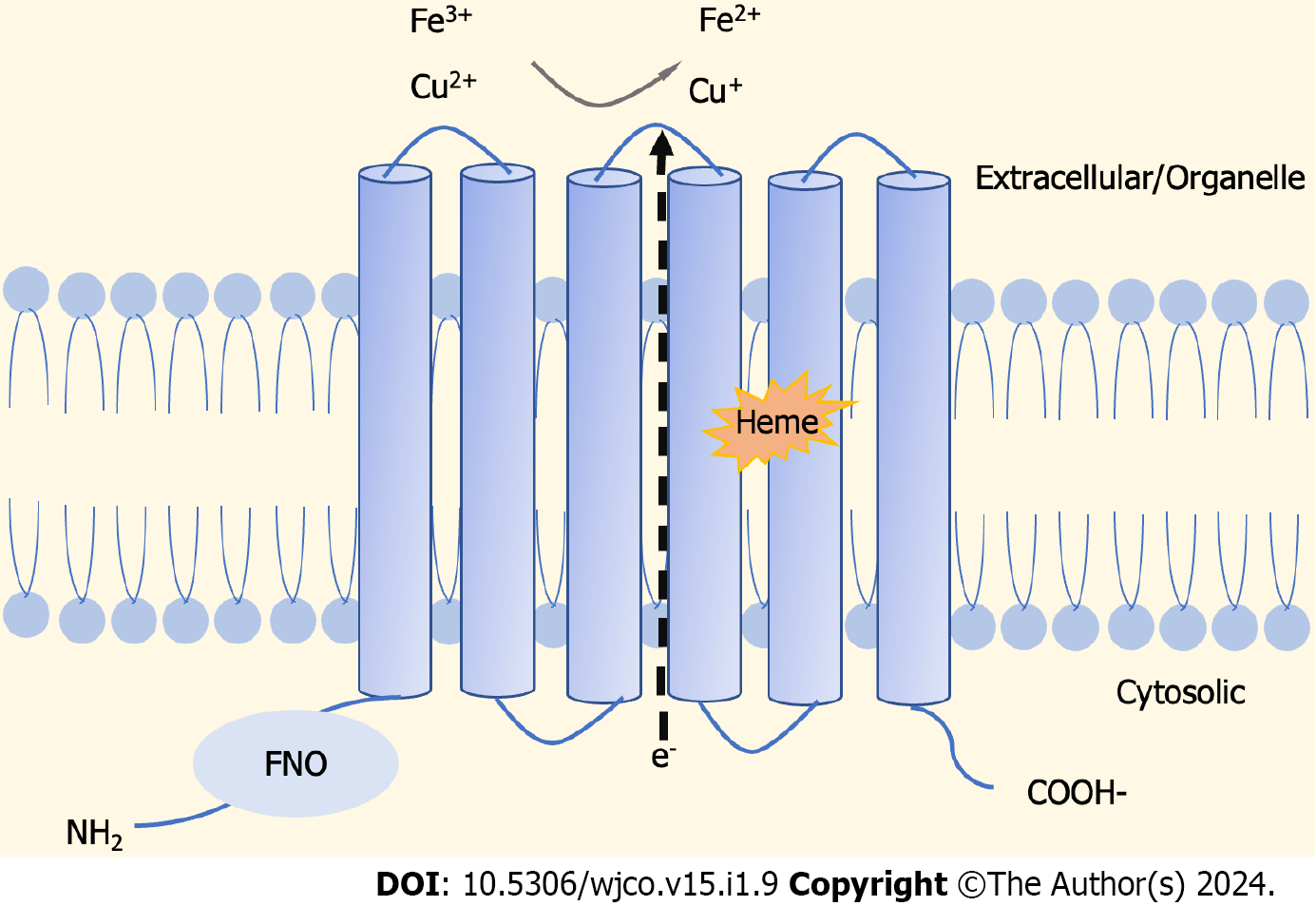
The STEAP family is composed of four structurally similar members, namely, STEAP1, STEAP2, STEAP3, and STEAP4[17], as cell-surface transmembrane proteins with six potential transmembrane regions, and intracellular amino and carboxyl termini[18]. It is shown that, unlike STEAP1, the C-terminal and conserved N-terminal domains of STEAP2-4 proteins are similar to the structures of yeast FRE metalloreductase and homologous to the paleontological and bacteriological F420H2:NADP+ oxidoreductase (FNO) binding protein domains, respectively[19]. Normally, STEAPs perform physiological functions as oxidoreductases, involved in the uptake and reduction of iron and copper[19,20] (Figure 1).
STEAP1 is the first reported STEAP family member with a molecular weight of 39.9 kDa (NP_036581.1) and an intramembrane heme binding site[18,21]. Although STEAP1 is widely expressed and co-localizes with transferrin (Tf) and Tf receptor 1 (TfR1), unlike other members, STEAP1 does not independently promote iron or copper reduction or uptake. Although it lacks the FNO-like reductase domain, which is thought to be essential for metal oxidoreductase activity, it is suggested that STEAP1 may play a role in iron or copper metabolism, which may be due to its interaction with the NAPDH-binding FNO domain of STEAP2 or STEAP4[19,22,23]. STEAP1B is a newly discovered member that has an extremely high (88%) identity with STEAP1. What distinguishes it from other proteins is that it only has four potential transmembrane domains without NADPH oxidoreductase domain or heme binding site. Hence, it is not expected to have oxidoreductase activity based on previous studies[15,24].
Besides STEAP1, STEAP2-4 are also composed of six transmembrane α-helices and intracellular hydrophilic N-and C-terminal domains, with the N-terminus containing the intracellular NADPH-binding FNO domain and the C-terminus containing bis-heme with the FRE domain. In vitro studies have found that STEAP2-4 perform Fe3+ and Cu2+ reductase activities and increase intracellular iron and copper uptake[20].
STEAP2 is known as STAMP1, which is composed of 490 amino acid residues. It is found that STEAP2 is highly expressed in the androgen-reactive prostate cancer cell line LNCaP, but not in androgen receptor-negative prostate cancer cell lines PC3 and DU145[25,26]. However, the expression of STEAP2 is not regulated by androgen receptors, but requires the presence of an intact androgen receptor[25]. In addition, the characteristics of STEAP2 expression and localization in human microvascular endothelial cells suggest that STEAP2 has a potential role in iron transport across the blood-brain barrier[27], which is further supported by the co-localization of STEAP2 and Tf in primary hippocampal neurons[28]. However, further research is needed to confirm this effect.
STEAP3 was first identified in prostate tissue and proposed as a candidate for prostate cancer immunotherapy, which is also known as tumor suppressor activating pathway 6[29]. STEAP3 co-localizes with Tf, TfR1, and divalent metal transporter 1 (DMT1) to participate in iron-uptake mediated by Tf endosome in erythroid cells and is thus an important component of the Tf-TfR1 cycle[20,30].
STEAP4 is also named STAMP2 because of its sequence similarity to STAMP1. STEAP2 and STEAP4 are highly expressed in the Golgi complex, trans-Golgi network, and plasma membrane, and co-localizes with endosome antigen 1, which is involved in the secretion-endocytosis pathway[25,26,31]. In addition to metal oxidoreductase activity, STEAP4 also plays a role in regulating inflammatory responses, fatty acid metabolism, and glucose metabolism[31-33]. To date, the possible effects of STAMP2 on iron metabolism have not been reported, and more studies are needed to directly evaluate the possible role of STAMP2 in human iron metabolism (Figure 2).
In mammals, iron and copper metabolism are related. Iron and copper, as important metal ions in vivo, are absorbed in the small intestine via reduction-state-specific DMT1[34-36] and copper transporter 1[37], respectively. Iron and copper often alternate between two oxidation states and participate in the redox process in vivo. Additionally, iron and copper can be used as cofactors of several enzymes to participate in the transformation of substances[34,38,39]. Iron and copper deficiencies are known to cause low-chromium microcell anemia in mammals, while excess iron or copper will lead to organ poisoning, particularly in the liver and brain. More importantly, since tumor cells have stronger proliferative ability than normal cells, their demand for iron and copper exceeds that of normal cells. The imbalance of iron and copper homeostasis is also closely related to cancer progression.
Under physiological conditions, STEAPs are a class of metalloproteinases that play an essential role in iron and copper homeostasis[19]. Iron and its homeostasis are closely related to inflammatory responses and provide a major protective mechanism in human physiology. In the past decades, a series of studies confirmed that iron overload can aggravate inflammatory responses and susceptibility to infection. Persons with hereditary hemochromatosis and iron overload are more susceptible to pathogens, whereas iron deficiency confers relative resistance to infection[40-42]. STEAPs are known to be a participant in iron-copper homeostasis, and their importance in protein functional activity, tissue expression patterns, and subcellular localization in cancer progression has been demonstrated. In addition, STEAPs have also been found to play a role in regulating cell proliferation and apoptosis, alleviating oxidative stress and mediating the Tf cycle[22,43].
Although inflammation is associated with an activated immune system (including immune cells and biological factors) under certain conditions, inflammation is a natural defense response, which is fundamentally different from the immune response[23]. Inflammation is a defense mechanism in vivo to remove invading foreign bodies such as bacteria, parasites, and viruses. In the process of inflammatory reaction, excessive or uncontrolled production of inflammatory products will lead to host cell damage, and even lead to chronic inflammation, chronic disease, and tumor transformation[44,45].
STEAP proteins are involved in the regulation of various physiological cellular functions, and plays a potentially important role in various metabolic processes, such as iron uptake and conversion, inflammatory stress response, and glucose metabolism in cells[15,43]. STEAPs have been suggested to play a role in iron metabolism in acute and chronic diseases associated with inflammation, as well as in the oncogenesis and development of malignancies. Liang et al[46] reported that STEAP1 and STEAP4 positively regulate the induction of proinflammatory, neutrophil-activated cytokines, such as chemokine (C-X-C motif) ligand (CXCL)1 and interleukin (IL)-8, in pustular skin disorders. More complexly, STEAP4 is found to be regulated by multiple cellular signaling pathways, revealing a positive association of STEAP1 and STEAP4 with the in vivo proinflammatory cytokines IL-1, IL-36, CXCL1, and CXCL8 in several neutrophil-driven diseases in humans. In addition, significant changes in genes related to iron biology were observed in patients with pustular skin disorders, suggesting that the inflammatory activity of STEAP has a causal relationship with its regulation of ion metabolism. Timmermans et al[47] found that STEAP2 plays a role in pathways involved in a chronic low-grade inflammatory disease state, namely, obesity, and lipid metabolism. Zhang et al[13] showed that STEAP3, the only member of this family that is highly expressed in macrophages that play a role in inflammatory immunity, regulates iron homeostasis during inflammatory stress through the translocation-associated membrane protein-dependent pathway. This study provides important insights into the function of STEAP3 as a coordinated regulator of iron homeostasis and inflammation.
In addition to its role as a metal oxidoreductase, STEAP4 is significantly overexpressed in low-grade inflammatory responses[48]. In a study by Gordon et al[49], STEAP4 was shown to play a protective role in the face of inflammatory stress in models of metabolic disorders. It is in turn up-regulated by acute inflammation or islet-level cytokine exposure. Even in septic patients, the expression of STEAP4 is elevated in the early stage of sepsis, which can be used to predict the clinical outcome of these patients[50]. These findings point to the complex regulation of STEAP4 that makes its protective role in inflammatory metabolic disorders. It is reported that iron and its homeostasis are closely related to the inflammatory response, which provides a major protective mechanism in human physiology, while iron overload worsens inflammation and infection susceptibility[13].
In recent years, a large amount of research data have revealed that inflammation is a key component of tumor progression. The oncogenesis of GICs, such as GC, CRC, and HCC, is related to infection and chronic inflammatory stimuli, and the tumor microenvironment, coordinated to a large extent by inflammatory cells, is to a large extent an indispensable participant in tumor formation, promoting tumor cell proliferation, survival, and migration[44]. Clinical studies have revealed that about 15%-20% of cancer patients have an infection, chronic inflammation, or autoimmune disease in the same tissue or organ site before the cancer development[44,51]. This suggests that the pre-cancerous inflammatory response is present before tumor formation. The strongest association between inflammation and malignancy is exemplified by CRC patients with IBD, including chronic ulcerative colitis and Crohn’s disease, predispositions to liver cancer in patients with hepatitis, and chronic Helicobacter pylori (H. pylori) infection as a major cause of GC[52].
Meanwhile, various environmental factors may induce and promote the development of cancer by inducing chronic inflammation, which may accompany tumor development and increase the risk of many different cancers such as liver, pancreatic, colon, and other malignancies[53,54]. So, how does the inflammatory response induce and promote tumorigenesis? It is well known that one of the causes of cancer is the loss of tumor suppressor function, with the most common mutation being the tumor suppressor p53. In the tumor microenvironment, loss of p53 function leads to increased expression of NF-κB dependent inflammatory genes[55,56], which promotes CRC progression and metastasis[56-58]. In addition, oncogene activation leading to excessive production of inflammatory cytokines and chemokines may be another mechanism by which chronic inflammation triggers cancer occurrence[59,60]. Activation of the oncogene K-Ras leads to increased secretion of cytokines and chemokines of “aging-associated secretory phenotypes”[60]. With increasing research on human symbiotic microbiomes, researchers have found that symbiotic microbiomes may be involved in the occurrence and development of many cancers, perhaps through microbial adhesion to cancer cells and translocation or long-distance release of microbial metabolites[61].
As mentioned above, the localization of STEAP proteins on the cell membrane, their differential expression in normal and cancer tissues, and their metal-oxidoreductase activity mechanism make them potential candidate targets for the biomarkers of a variety of cancers, as well as potential targets for the alleviation or treatment of these cancers[62,63]. STEAP4 has been shown to play an important role in the inflammatory response and other physiological metabolic processes[31-33]. Although the role of STEAP1, STEAP2, and STEAP3 in the inflammatory response is rarely reported, it is tempting to speculate that STEAP1-3 may also have similar functions.
GC is one of the most common GICs in humans, and chronic H. pylori infection is one of the main risk factors for GC occurrence[64]. The latency of H. pylori leads to a variety of changes in the gastric mucosa, such as gastritis, atrophic gastritis, intestinal metaplasia, dysplasia, and eventually GC[65]. Chronic infection with H. pylori in the gastric mucosa can occur freely in mucus, by attaching to cells, or intracellularly, requiring iron for bacterial growth[66]. In an iron-deficient medium, H. pylori can bind and extract iron from hemoglobin, Tf, and lactoferrin to support its growth, and preferentially bind the iron-free forms of Tf and lactoferrin, limiting its ability to extract iron from normal serum[67]. Hamedi Asl et al[68] investigated the expression of genes involved in iron homeostasis and their role in the pathogenesis of H. pylori infection. It is found that TfR and ferritin light chain were overexpressed in all H. pylori-positive tissues, while increased iron regulatory protein 2 expression was associated with H. pylori-positive chronic gastritis and intestinal metaplasia, confirming the role of iron acquisition-related genes in H. pylori attachment into the gastric mucosa. On the other hand, the colonization of H. pylori induces a substantial production of reactive oxygen species (ROS) and develops various strategies to quench the deleterious effects of ROS, resulting in persistent ROS production. However, excessive ROS will incur chronic inflammation and cellular damage, as the major risk factor for gastric carcinogenesis[69]. These investigations indicate the potential role of STEAPs in inflammatory responses for H. pylori-related GC.
The role of STEAP1 in GC was first reported by Wu et al[70], who defined the landscape of translationally regulated gene products with differential expression between non-metastatic and metastatic GC cohorts. Interestingly, STEAP1 was identified as the most translationally upregulated gene product, required for cell proliferation, migration/invasion, tumorigenesis, and chemoresistance to docetaxel treatment[70]. To explore the regulatory mechanism, the same research group focused on the potential regulators for STEAP1 expression[71]. They found that the RNA-binding protein poly r(C) binding protein 1 and miR-3978 function as repressors of peritoneal metastasis of GC, partially by downregulating STEAP1, while phosphorylated eIF4E upregulates STEAP1 expression at the level of cap-dependent translation initiation to facilitate the peritoneal metastasis of GC[71]. A similar result was found by Zhang et al[72], that STEAP1 performed an oncogenic role in the occurrence and metastasis of GC via activating the AKT/FoxO1 pathway and epithelial-mesenchymal transition process.
Besides STEAP1, STEAP4 was also found to be highly expressed in GC tissues, which is associated with advanced clinical stage and poor prognosis of GC patients. Importantly, the expression of STEAP4 was found to be positively correlated with the infiltration levels of B cells, CD4+ T cells, macrophages, neutrophils, and dendritic cells, indicating its contribution to the regulation of the tumor microenvironment[73]. Although the current investigation of STEAPs in GCs is limited, the potential role of STEAPs involved in immune response in GC is emerging and needs further exploration.
CRC is the third most common cause of cancer death in the United States and other developed countries[1]. It has been well-accepted that chronic inflammation is one of the recognized risk factors for the development of CRC, especially in colon cancer. The accumulation of immune cells and inflammatory factors in the intestinal mucosa constitute a complex chronic inflammatory environment and cause oxidative stress or DNA damage on the epithelial cells[74]. In patients with IBD, the risk for CRC is increased significantly, which is strongly associated with chronic inflammation, and such CRC was named colitis-associated CRC[74]. On the other hand, the gastrointestinal tract is the primary site to absorb copper, which is an essential micronutrient and critical enzyme cofactor for crucial copper-dependent enzymes. Elevated copper concentrations can cause multifaceted responses of pathogenic bacteria when invading the host[75], while in the fish model, Wang et al[76] found that copper exposure induced intestinal oxidative stress and inflammation, resulting in enrichment of potentially pathogenic bacteria and reduction of probiotic bacteria. Miller et al[77] found a significant difference in copper isotopic composition along with diverse bacterial populations, revealing a host-microbial interaction involved in the regulation of copper transport.
After being identified as a new target for preventative and/or therapeutic vaccine construction and immune monitoring in prostate cancer[78], STEAP1 was found to be highly expressed in CRC, predicting a poor overall survival in CRC patients[79]. Mechanistically, Nakamura et al[80] found that silencing STEAP1 suppressed CRC cell growth and increased ROS production, associated with decreased expression of antioxidant molecules regulated by the transcription factor nuclear erythroid 2-related factor. As an antigen present in various tumors, STEAP1 has the potential to stimulate cytotoxic T lymphocytes (CTLs) involved in antitumor immunotherapy. To explore the specific STEAP1 sequence capable of stimulating naïve HLA-A2-restricted CTLs, Rodeberg et al[81] used MHC peptide binding algorithms to predict the potential sequences and verified their abilities to induce antigen-specific CTLs to kill peptide-pulsed HLA-A2 target cells. They provided strong evidence that STEAP1-292 peptide (MIAVFLPIV) is naturally processed by many types of tumors, including CRC, and recognized by CTLs, and the modified STEAP1-292.2L peptide (MLAVFLPIV) is more immunogenic to induce CTL recognition, serving as a potential antitumor peptide vaccine. Soon, Rodeberg et al[82] reported another two peptides of STEAP1, which can be used for broad-spectrum-tumor immunotherapy.
As metalloreductases, STEAPs are involved in iron/copper homeostasis[21,83]. Among the copper homeostasis-related genes, STEAP3 was found to be increased in CRC in oligonucleotide microarray analysis, related to copper accumulation[83]. During the polarization of macrophages, the time-dependent change of intracellular Fe(II) during the inflammatory activation was consistent with the expression shifts of TfR, STEAP3, and Fe(II) exporter Slc40a1, indicating the role of Fe(II) in inflammatory-activated macrophages[84]. Even in hypoferric conditions, STEAP3 overexpression increased iron storage, causing resistance to iron deprivation-induced apoptosis[85]. In CRC cells, STEAP3 also facilitates exosomal trafficking to increase the secretion of exosomes[86], which are important interactors between tumor cells and their surroundings[87]. Interestingly, hypoxia-induced antisense long non-coding RNA STEAP3-AS1 increased the expression of STEAP3 by competitively interacting with YTH domain-containing family protein 2 (YTHDF2) and leading to the disassociation of YTHDF2 with STEAP3 mRNA and upregulated STEAP3 mRNA stability in CRC. The enhanced STEAP3 expression increased intracellular Fe(II), which induced the phosphorylation and inactivation of glycogen synthase kinase 3β, releasing β-catenin translocated into the nucleus to activate the Wnt signal with promoted CRC progression[88].
Different from other STEAP family members, STEAP4 expression was found to be low in CRC tissues compared with normal tissues, which is positively correlated with immune infiltration and immune-related biomarkers[89]. However, in colitis animal models and IBD patients, STEAP4 was also highly induced in a hypoxia-dependent manner, leading to a dysregulation in mitochondrial iron balance and enhanced ROS level. Using a colitis-associated colon cancer model, Xue et al[90] found that the mitochondrial iron dysregulation related to high STEAP4 level is a key mechanism by which inflammation impacts colon tumorigenesis, indicting STEAP4 as an important regulator of the inflammatory response. In the colitis-associated tumorigenesis model, the copper metabolism can also be mobilized by the pro-inflammatory cytokine IL-17, by inducing STEAP4-dependent cellular copper uptake, which is critical for colon tumor formation[91].
As mentioned above, STEAP1 and STEAP4 function as metalloreductases to regulate the iron/copper homeostasis during the oncogenesis and development of CRC related to inflammation. Although there are no reports of STEAP2 nor STEAP3 in CRC, the structural similarity of STEAP family proteins has prompted a further investigation of the potential role of STEAP2 or STEAP3 in CRC.
HCC is the most common type of primary liver cancer, listed as the third leading cause of cancer-related death worldwide[92]. The increased incidence of primary liver cancer in several developed countries will likely continue for decades. Since primary liver cancer is mostly related to the infection with hepatitis B and C viruses (HBV and HCV), it is the first human cancer enormously amendable to prevention with HBV vaccines[93,94]. Although serum copper concentration is not a specific diagnostic biomarker for liver disease, serum copper isotope ratio has been proven to be an assistant monitor for the diagnosis, prognosis, and follow-up of chronic liver diseases, as the imbalanced copper homeostasis exists in liver diseases[95,96].
Interestingly, STEAP1 was considered as a targeted tumor antigen with the cytotoxic potency of chemotherapeutic drugs for designing antibody-drug conjugates (ADCs). Boswell et al[97] constructed a humanized anti-STEAP1 antibody-linked ADC, and evaluated its pharmacokinetics, tissue distribution, and/or potential organ toxicity in rats, finding a general trend toward increased hepatic uptake and reduced levels in other highly vascularized organs. Another research group constructed a radio-labeled anti-STEAP1-conjugated probe for positron emission tomography detection, and the highest mean absorbed dose to the normal organ was found in the liver at 1.18 mGy/MBq[98]. The above results indicate the ability of uptake for anti-STEAP1 ADCs in the liver, predicting the therapeutic potential for liver malignancies. Not surprisingly, the expression of STEAP1 was found to be high in liver tumors and associated with poor clinical outcomes, suggesting that STEAP1 is a druggable target in liver cancer[99].
Related to inflammatory responses, STEAP3 is a mediator and protector of hepatic ischemia-reperfusion injury through TAK1-dependent activation of the JNK/p38 pathways in hepatocytes[100]. Interestingly, after HCV infection, STEAP3 was found to be downregulated in HCC and associated with the progression to cirrhosis and HCC, and it thus can be used as a potential monitoring biomarker for the development of HCC[101]. The decreased expression of STEAP3 in HCC was also confirmed by Yi et al[102], which is associated with the abnormal expression of ferroptosis-related genes. However, at the cellular level, Wang et al[101] found that nuclear STEAP3 was highly expressed in HCC, which was an independent prognostic factor for HCC patients. Mechanically, increased nuclear STEAP3 expression significantly promoted the stemness phenotype, cell cycle progression, and cellular proliferation of HCC cells, through RAC1-ERK-STAT3 and RAC1-JNK-STAT6 signaling axes, while STEAP3 also upregulated the expression and nuclear trafficking of epidermal growth factor receptor (EGFR) to promote EGFR-mediated STAT3 transcription activity in a positive feedback manner[101]. As the matrix stiffness is a key factor impairing tumor immunity, Wang et al[103] analyzed the effect of stiffness in HCV-infected cirrhotic HCC, finding that stiffer matrix decreased STEAP3 in the invasive front region of HCC and the cirrhotic tissue, suppressing STEAP3-mediated immune infiltration of CD4+ and CD8+ T cells, macrophages, neutrophils, and dendritic cells, along with decreased ferroptosis.
As a plasma membrane metalloreductase, STEAP4 is controlled by inflammatory cytokines in the liver, such as IL-6, which significantly induced the transcription activity of STEAP4 through STAT3 and CCAAT/enhancer-binding protein alpha, playing a critical role in the response to nutritional and inflammatory stress[104]. Hepatic STEAP4 decreases the stability of HBV X protein (HBx) by physically interacting with HBx, subsequentially suppressing HBx-mediated transcription of lipogenic and adipogenic genes and protecting hepatocytes from HBV gene expression[105]. In a non-alcoholic fatty liver disease (NAFLD) animal model, recombinant fibroblast growth factor 21 treatment ameliorated hepatic steatosis and insulin resistance by increasing STEAP4-mediated hepatic iron overload and ferroportin expression, indicating STEAP4 as a suitable therapeutic intervention for NAFLD patients[106]. However, in HCC tissues, genome-wide DNA methylation analysis revealed significantly hypermethylated and downregulated STEAP4 compared to the non-tumor liver tissues, which may be associated with the development of HCC[107], while STEAP4 methylation in plasma DNA was not associated with HCC risk[108]. Not surprisingly, Zhou et al[88] reported that the methylation level of the STEAP4 promoter was correlated with the downregulation of STEAP4, functioning as a tumor suppressor in HCC by inhibiting the PI3K/AKT/mTOR pathway. The reduced STEAP4 expression is significantly associated with tumor aggressiveness and poor prognosis in HCC patients, likely due to its link to various biological processes and induction of HCC immune evasion[109].
As mentioned above, STEAPs, through iron/copper metabolism or different cytokines, participate in the inflammatory process of the gastrointestinal tract, and then induce GIC occurrence and promote GIC development accordingly (Table 1).
| Protein | Organ | Function/mechanism | Ref. |
| STEAP1 | Stomach | Promoting peritoneal metastasis of GC | [113] |
| Regulated at the level of cap-dependent translation initiation by phosphorylated eIF4E in GC | [114] | ||
| Increasing cell proliferation, migration, and invasion of GC, via the activation of AKT/FoxO1 pathway and epithelial-mesenchymal transition | [72] | ||
| Colon/rectum | Inducing cytotoxic T lymphocytes to recognize colon cancer with STEAP1 by specific STEAP1 peptide | [81] | |
| Reducing ROS and preventing apoptosis of CRC cells via NRF2 pathway | [115] | ||
| Liver | Increased hepatic uptake of STEAP1 antibody-drug conjugates | [116] | |
| Accelerating cell proliferation by targeting c-Myc in liver cancer cells | [100] | ||
| STEAP3 | Colon/rectum | Increased in CRC, along with CTR1 to induce copper accumulation | [84] |
| Facilitating iron uptake and resistance to iron deprivation-induced apoptosis under hypoferric condition | [86] | ||
| Time-dependent change of STEAP3 during inflammatory activation, along with specific accumulation of Fe (II) in inflammatory-activated macrophages | [85] | ||
| Increasing exosome secretion in CRC, which can be cleaved by RHBDD1 in a dose/activity dependent manner | [87] | ||
| Protected by hypoxia-induced lncRNA STEAP3-AS1 by preventing m6A-mediated degradation of STEAP3 mRNA | [89] | ||
| Liver | Decreased expression in liver, associated with the transition from cirrhosis to HCC | [117] | |
| Increased in HCC cell nucleus, promoting proliferation via RAC1-ERK-STAT3 and RAC1-JNK-STAT6 signaling axes | [102] | ||
| Ferroptosis-related differential gene in HCV-infected cirrhotic HCC, impaired by matrix stiffness | [105] | ||
| STEAP4 | Stomach | Highly expressed in GC, associated with infiltration of immune cells | [73] |
| Colon/rectum | Decreased in CRC and positively correlated with immune-related biomarkers | [118] | |
| Highly induced in mouse models of colitis and inflammatory bowel disease patients, increasing ROS production in a hypoxia-dependent manner | [91] | ||
| Induced by the inflammatory cytokine IL-17 to drive copper uptake, critical for colon tumor formation | [119] | ||
| Liver | Lowly expressed in HCC, controlled by hypermethylation in STEAP4 promoter region | [109] | |
| Inhibiting proliferation and metastasis of HCC through PI3K/AKT/mTOR pathway inhibition | [111] | ||
| Low level in HCC, associated with advanced HCC stage, poor survival, and immunosuppressive microenvironment | [112] | ||
| Stimulated by the inflammatory cytokine IL-6, through STAT3 and CCAAT/enhancer-binding protein alpha in liver | [106] | ||
| Hepatic STEAP4 antagonizes HBx-mediated hepatocyte dysfunction by interacting with and decreasing the stability of HBx | [107] | ||
| Therapeutic effect of recombinant FGF21 on NAFLD is performed by increasing hepatic STEAP4 to protect hepatocytes | [108] |
The strict maintenance of a specific microbial consortium in the gastrointestinal tract is critical for health, while gut microbiota alteration and dysbiosis will cause inflammation and pathogenic intestinal conditions[110]. The connection between inflammation and tumorigenesis has been well-established for decades based on genetic, pharmacological, and epidemiological evidence. Even obstructive sleep apnea-induced hypertension is found to be associated with gut dysbiosis, which may serve as the trigger for gut and neuroinflammation, and preventing or reversing gut dysbiosis may reduce neuroinflammation and hypertension accordingly[111]. Therefore, monitoring microbiota alteration or inflammation in the gastrointestinal tract is a research hotspot for the diagnosis or treatment of gastrointestinal inflammation-related diseases, including GICs.
Gopalakrishnan et al[112] implemented a miniaturized smart capsule to monitor inflammatory lesions throughout the gastrointestinal tract by detecting ROS level, a biomarker of inflammation, which provided a new milestone of smart ingestible electronics for improving the diagnosis and treatment of digestive disease. The exosomes derived from human placental mesenchymal stem cells used in the myocardial infarction model, notably modulated gut microbial community, increased the gut microbiota metabolites short chain fatty acids (SCFAs), and decreased lipopolysaccharide[113]. By sorting and sequencing of immunoglobulin (Ig) A-coated microbiota to define immune-reactive microbiota, Lima et al[114] identified that transferable IgA-coated Odoribacter splanchnicus in responders to fecal microbiota transplantation for patients with ulcerative colitis increases mucosal regulatory T cells, and induces the production of IL-10 and SCFAs, resulting in the resolution of colitis. Such investigation provided potential strategies or vectors for the treatment of the gastrointestinal tract, as well as inflammation-related GICs.
As a common oncogene in diverse malignancies, STEAP1 was considered a promising candidate therapeutic target, with abundant expression in malignancies[17,18]. Importantly, STEAP1 is also found to be a transporter, participating in intercellular communication[115,116]. Since the first prostate cancer-specific immunotherapy was licensed in 2010, immunotherapy represents a promising approach to harness the host’s immune system with an anti-tumor effect[117,118]. 89Zr-DFO-MSTP2109A, a radiolabeled antibody targeting STEAP1, was well tolerated and showed good visualization in the study, thus establishing its potential role as a potential biomarker for STEAP1 directed therapy and confirming its diagnostic value[119]. Given STEAP1’s mechanism in cancers, therapeutic strategies targeting STEAP1, such as monoclonal antibodies (mAbs), DNA vaccines, and ADCs, have been developed. Challita-Eid et al[115] identified STEAP1 mediating the transfer of small molecules between adjacent cells and first generated two mAbs that bind to STEAP1 epitopes at the cell surface, which significantly inhibited STEAP-1-induced intercellular communication in a dose-dependent manner. Soon, an anti-STEAP4 mAb that binds to the extracellular domain of STEAP4 was also shown to cause insulin resistance in adipocytes by disrupting cellular mitochondrial function, in addition to inducing apoptosis and inhibiting preadipocyte proliferation and glucose uptake without affecting human preadipocyte differentiation[120], while anti-STEAP1 based ADCs performed exciting anti-tumor function by regulating the immune response[97,121].
One of the goals of current tumor immunotherapy research is to design and validate multi-epitope/multi-antigen vaccines that can induce multi-specific anti-tumor responses and reduce the risk of selection of antigen loss escape variants in vivo[122,123]. The multivalent vaccine should be composed of a variety of epitopes of widely expressed tumor antigens for the purpose of wide application. Recently, many of the same tumor antigens expressed in most human tumors have been described, such as survivin[124], EphA2[125], pan-MAGE-A HLA-A* 0201-restricted epitopes, and Hsp70[126,127]. STEAP1 protein was found to be overexpressed in prostate cancer, pancreatic cancer, CRC, HCC, breast cancer, bladder cancer, ovarian cancer, acute lymphoblastic leukemia, and Ewing sarcoma[18]. This wide expression pattern strongly suggests the utility of this tumor antigen in broad-spectrum antitumor immunotherapy. It has been demonstrated that STEAP1 is a tumor antigen target of CD8+ T cells by identifying two HLA-A* 0201-restricted antigen peptides, STEAP86-94 and STEAP262-270[82].
In addition, immunotherapy has proved to be an effective treatment for a variety of cancers, especially for patients with tumors with overexpressed antigens that can be recognized by immune T/B cells. The use of STEAP peptides to induce helper T cells in the context of multiple major histocompatibility complex class II alleles have been studied for T cell immunotherapy against STEAP-expressing renal cell carcinoma and bladder cancer[128]. These studies confirm that targeting STEAP family proteins in a variety of solid tumors is an attractive and promising effective approach. Although current therapeutic strategies targeting STEAPs have not been applied in clinical practice, their molecular transport mechanism and involvement in cancer progression make them promising targets for the treatment of patients with GICs.
STEAP family members share similar structural features and function as metal oxidoreductases involved in a variety of cellular processes, such as copper/iron uptake, response to inflammation, fatty acid and glucose metabolism, and oxidative stress regulation. STEAPs are irregularly expressed in different cancers, which are involved in the proliferation, migration, invasion, and metastasis of cancer cells, and play a role in promoting or suppressing cancer. In addition, the inflammatory response may be caused by necrosis of rapidly growing tumor cells due to hypoxia and lack of nutrients. ROS and reactive nitrogen species produced by inflammatory cells can cause oxidative DNA damage in gastrointestinal cells, leading to the activation of oncogenes and/or inactivation of tumor suppressor genes, as well as various epigenetic changes that are conducive to the progression of GICs. Thus, molecules that affect cell survival or the subsequent inflammatory response are likely to have an impact on the course of GIC development. In conclusion, based on the increasing use of STEAPs as cancer therapeutic targets, inflammatory therapeutic strategies in GICs will be more considered in the future, most likely including STEAP family proteins.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Gutiérrez-Cuevas J, Mexico; Tantau AI, Romania S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Zhang XD
| 1. | Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4235] [Cited by in RCA: 11436] [Article Influence: 3812.0] [Reference Citation Analysis (4)] |
| 2. | Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020;396:635-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1150] [Cited by in RCA: 2859] [Article Influence: 571.8] [Reference Citation Analysis (5)] |
| 3. | Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2800] [Cited by in RCA: 4110] [Article Influence: 587.1] [Reference Citation Analysis (6)] |
| 4. | Wang D, Cabalag CS, Clemons NJ, DuBois RN. Cyclooxygenases and Prostaglandins in Tumor Immunology and Microenvironment of Gastrointestinal Cancer. Gastroenterology. 2021;161:1813-1829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 88] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 5. | Man SM. Inflammasomes in the gastrointestinal tract: infection, cancer and gut microbiota homeostasis. Nat Rev Gastroenterol Hepatol. 2018;15:721-737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 215] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 6. | Schmitt M, Greten FR. The inflammatory pathogenesis of colorectal cancer. Nat Rev Immunol. 2021;21:653-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 425] [Article Influence: 106.3] [Reference Citation Analysis (0)] |
| 7. | Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13:759-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1198] [Cited by in RCA: 1503] [Article Influence: 125.3] [Reference Citation Analysis (0)] |
| 8. | Karin M, Greten FR. NF-kappaB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol. 2005;5:749-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2227] [Cited by in RCA: 2420] [Article Influence: 121.0] [Reference Citation Analysis (0)] |
| 9. | Duan F, Song C, Zhang J, Wang P, Ye H, Dai L, Wang K. Evaluation of the Epidemiologic Efficacy of Eradicating Helicobacter pylori on Development of Gastric Cancer. Epidemiol Rev. 2019;41:97-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Jin G, Lv J, Yang M, Wang M, Zhu M, Wang T, Yan C, Yu C, Ding Y, Li G, Ren C, Ni J, Zhang R, Guo Y, Bian Z, Zheng Y, Zhang N, Jiang Y, Chen J, Wang Y, Xu D, Zheng H, Yang L, Chen Y, Walters R, Millwood IY, Dai J, Ma H, Chen K, Chen Z, Hu Z, Wei Q, Shen H, Li L. Genetic risk, incident gastric cancer, and healthy lifestyle: a meta-analysis of genome-wide association studies and prospective cohort study. Lancet Oncol. 2020;21:1378-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 160] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 11. | Ponziani FR, Bhoori S, Castelli C, Putignani L, Rivoltini L, Del Chierico F, Sanguinetti M, Morelli D, Paroni Sterbini F, Petito V, Reddel S, Calvani R, Camisaschi C, Picca A, Tuccitto A, Gasbarrini A, Pompili M, Mazzaferro V. Hepatocellular Carcinoma Is Associated With Gut Microbiota Profile and Inflammation in Nonalcoholic Fatty Liver Disease. Hepatology. 2019;69:107-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 475] [Article Influence: 79.2] [Reference Citation Analysis (1)] |
| 12. | Tourelle KM, Boutin S, Weigand MA, Schmitt FCF. The Association of Gut Microbiota and Complications in Gastrointestinal-Cancer Therapies. Biomedicines. 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Zhang F, Tao Y, Zhang Z, Guo X, An P, Shen Y, Wu Q, Yu Y, Wang F. Metalloreductase Steap3 coordinates the regulation of iron homeostasis and inflammatory responses. Haematologica. 2012;97:1826-1835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Wu HT, Chen WJ, Xu Y, Shen JX, Chen WT, Liu J. The Tumor Suppressive Roles and Prognostic Values of STEAP Family Members in Breast Cancer. Biomed Res Int. 2020;2020:9578484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 15. | Grunewald TG, Bach H, Cossarizza A, Matsumoto I. The STEAP protein family: versatile oxidoreductases and targets for cancer immunotherapy with overlapping and distinct cellular functions. Biol Cell. 2012;104:641-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Xu M, Evans L, Bizzaro CL, Quaglia F, Verrillo CE, Li L, Stieglmaier J, Schiewer MJ, Languino LR, Kelly WK. STEAP1-4 (Six-Transmembrane Epithelial Antigen of the Prostate 1-4) and Their Clinical Implications for Prostate Cancer. Cancers (Basel). 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 17. | Gomes IM, Maia CJ, Santos CR. STEAP proteins: from structure to applications in cancer therapy. Mol Cancer Res. 2012;10:573-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 141] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 18. | Hubert RS, Vivanco I, Chen E, Rastegar S, Leong K, Mitchell SC, Madraswala R, Zhou Y, Kuo J, Raitano AB, Jakobovits A, Saffran DC, Afar DE. STEAP: a prostate-specific cell-surface antigen highly expressed in human prostate tumors. Proc Natl Acad Sci U S A. 1999;96:14523-14528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 262] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 19. | Ohgami RS, Campagna DR, McDonald A, Fleming MD. The Steap proteins are metalloreductases. Blood. 2006;108:1388-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 502] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 20. | Ohgami RS, Campagna DR, Greer EL, Antiochos B, McDonald A, Chen J, Sharp JJ, Fujiwara Y, Barker JE, Fleming MD. Identification of a ferrireductase required for efficient transferrin-dependent iron uptake in erythroid cells. Nat Genet. 2005;37:1264-1269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 580] [Cited by in RCA: 533] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 21. | Chen WJ, Wu HT, Li CL, Lin YK, Fang ZX, Lin WT, Liu J. Regulatory Roles of Six-Transmembrane Epithelial Antigen of the Prostate Family Members in the Occurrence and Development of Malignant Tumors. Front Cell Dev Biol. 2021;9:752426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 22. | Gomes IM, Rocha SM, Gaspar C, Alvelos MI, Santos CR, Socorro S, Maia CJ. Knockdown of STEAP1 inhibits cell growth and induces apoptosis in LNCaP prostate cancer cells counteracting the effect of androgens. Med Oncol. 2018;35:40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 23. | Amaral L, Viveiros M, Kristiansen JE. "Non-Antibiotics": alternative therapy for the management of MDRTB and MRSA in economically disadvantaged countries. Curr Drug Targets. 2006;7:887-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Gomes IM, Santos CR, Maia CJ. Expression of STEAP1 and STEAP1B in prostate cell lines, and the putative regulation of STEAP1 by post-transcriptional and post-translational mechanisms. Genes Cancer. 2014;5:142-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Korkmaz KS, Elbi C, Korkmaz CG, Loda M, Hager GL, Saatcioglu F. Molecular cloning and characterization of STAMP1, a highly prostate-specific six transmembrane protein that is overexpressed in prostate cancer. J Biol Chem. 2002;277:36689-36696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Porkka KP, Helenius MA, Visakorpi T. Cloning and characterization of a novel six-transmembrane protein STEAP2, expressed in normal and malignant prostate. Lab Invest. 2002;82:1573-1582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | McCarthy RC, Kosman DJ. Mechanistic analysis of iron accumulation by endothelial cells of the BBB. Biometals. 2012;25:665-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 28. | Ji C, Kosman DJ. Molecular mechanisms of non-transferrin-bound and transferring-bound iron uptake in primary hippocampal neurons. J Neurochem. 2015;133:668-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 29. | Machlenkin A, Paz A, Bar Haim E, Goldberger O, Finkel E, Tirosh B, Volovitz I, Vadai E, Lugassy G, Cytron S, Lemonnier F, Tzehoval E, Eisenbach L. Human CTL epitopes prostatic acid phosphatase-3 and six-transmembrane epithelial antigen of prostate-3 as candidates for prostate cancer immunotherapy. Cancer Res. 2005;65:6435-6442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Yanatori I, Kishi F. DMT1 and iron transport. Free Radic Biol Med. 2019;133:55-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 231] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 31. | Korkmaz CG, Korkmaz KS, Kurys P, Elbi C, Wang L, Klokk TI, Hammarstrom C, Troen G, Svindland A, Hager GL, Saatcioglu F. Molecular cloning and characterization of STAMP2, an androgen-regulated six transmembrane protein that is overexpressed in prostate cancer. Oncogene. 2005;24:4934-4945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 107] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 32. | Scarl RT, Lawrence CM, Gordon HM, Nunemaker CS. STEAP4: its emerging role in metabolism and homeostasis of cellular iron and copper. J Endocrinol. 2017;234:R123-R134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 33. | Moldes M, Lasnier F, Gauthereau X, Klein C, Pairault J, Fève B, Chambaut-Guérin AM. Tumor necrosis factor-alpha-induced adipose-related protein (TIARP), a cell-surface protein that is highly induced by tumor necrosis factor-alpha and adipose conversion. J Biol Chem. 2001;276:33938-33946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 34. | Gunshin H, Mackenzie B, Berger UV, Gunshin Y, Romero MF, Boron WF, Nussberger S, Gollan JL, Hediger MA. Cloning and characterization of a mammalian proton-coupled metal-ion transporter. Nature. 1997;388:482-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2383] [Cited by in RCA: 2303] [Article Influence: 82.3] [Reference Citation Analysis (0)] |
| 35. | Fleming MD, Romano MA, Su MA, Garrick LM, Garrick MD, Andrews NC. Nramp2 is mutated in the anemic Belgrade (b) rat: evidence of a role for Nramp2 in endosomal iron transport. Proc Natl Acad Sci U S A. 1998;95:1148-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 710] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 36. | Fleming MD, Trenor CC 3rd, Su MA, Foernzler D, Beier DR, Dietrich WF, Andrews NC. Microcytic anaemia mice have a mutation in Nramp2, a candidate iron transporter gene. Nat Genet. 1997;16:383-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 904] [Cited by in RCA: 854] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 37. | Kuo YM, Zhou B, Cosco D, Gitschier J. The copper transporter CTR1 provides an essential function in mammalian embryonic development. Proc Natl Acad Sci U S A. 2001;98:6836-6841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 288] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 38. | Lee PL, Gelbart T, West C, Halloran C, Beutler E. The human Nramp2 gene: characterization of the gene structure, alternative splicing, promoter region and polymorphisms. Blood Cells Mol Dis. 1998;24:199-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 238] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 39. | Harris ED. Iron-copper interactions: some new revelations. Nutr Rev. 1994;52:311-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Bullen JJ, Spalding PB, Ward CG, Gutteridge JM. Hemochromatosis, iron and septicemia caused by Vibrio vulnificus. Arch Intern Med. 1991;151:1606-1609. [PubMed] |
| 41. | Doherty CP. Host-pathogen interactions: the role of iron. J Nutr. 2007;137:1341-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 126] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 42. | Gerhard GS, Levin KA, Price Goldstein J, Wojnar MM, Chorney MJ, Belchis DA. Vibrio vulnificus septicemia in a patient with the hemochromatosis HFE C282Y mutation. Arch Pathol Lab Med. 2001;125:1107-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Gakis G. The role of inflammation in bladder cancer. Adv Exp Med Biol. 2014;816:183-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 44. | Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8581] [Cited by in RCA: 8327] [Article Influence: 489.8] [Reference Citation Analysis (0)] |
| 45. | Simmons DL. What makes a good anti-inflammatory drug target? Drug Discov Today. 2006;11:210-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 46. | Liang Y, Xing X, Beamer MA, Swindell WR, Sarkar MK, Roberts LW, Voorhees JJ, Kahlenberg JM, Harms PW, Johnston A, Gudjonsson JE. Six-transmembrane epithelial antigens of the prostate comprise a novel inflammatory nexus in patients with pustular skin disorders. J Allergy Clin Immunol. 2017;139:1217-1227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 47. | Timmermans S, Van Hauwermeiren F, Puimège L, Dejager L, Van Wonterghem E, Vanhooren V, Mestdagh P, Libert C, Vandenbroucke RE. Determining differentially expressed miRNAs and validating miRNA--target relationships using the SPRET/Ei mouse strain. Mamm Genome. 2015;26:94-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Sharma PR, Mackey AJ, Dejene EA, Ramadan JW, Langefeld CD, Palmer ND, Taylor KD, Wagenknecht LE, Watanabe RM, Rich SS, Nunemaker CS. An Islet-Targeted Genome-Wide Association Scan Identifies Novel Genes Implicated in Cytokine-Mediated Islet Stress in Type 2 Diabetes. Endocrinology. 2015;156:3147-3156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 49. | Gordon HM, Majithia N, MacDonald PE, Fox JEM, Sharma PR, Byrne FL, Hoehn KL, Evans-Molina C, Langman L, Brayman KL, Nunemaker CS. STEAP4 expression in human islets is associated with differences in body mass index, sex, HbA1c, and inflammation. Endocrine. 2017;56:528-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 50. | Jiang H, Dong Y, Yan D, Wu Y, Wang Y, Ren Y, Mao G, Liang G, Liu W, Zhou Y, Huang Z, Qi L. The expression of STEAP4 in peripheral blood predicts the outcome of septic patients. Ann Transl Med. 2021;9:1519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 51. | Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883-899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8437] [Cited by in RCA: 8184] [Article Influence: 545.6] [Reference Citation Analysis (0)] |
| 52. | Macarthur M, Hold GL, El-Omar EM. Inflammation and Cancer II. Role of chronic inflammation and cytokine gene polymorphisms in the pathogenesis of gastrointestinal malignancy. Am J Physiol Gastrointest Liver Physiol. 2004;286:G515-G520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 253] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 53. | Quail DF, Dannenberg AJ. The obese adipose tissue microenvironment in cancer development and progression. Nat Rev Endocrinol. 2019;15:139-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 366] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 54. | Quail DF, Olson OC, Bhardwaj P, Walsh LA, Akkari L, Quick ML, Chen IC, Wendel N, Ben-Chetrit N, Walker J, Holt PR, Dannenberg AJ, Joyce JA. Obesity alters the lung myeloid cell landscape to enhance breast cancer metastasis through IL5 and GM-CSF. Nat Cell Biol. 2017;19:974-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 211] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 55. | Komarova EA, Krivokrysenko V, Wang K, Neznanov N, Chernov MV, Komarov PG, Brennan ML, Golovkina TV, Rokhlin OW, Kuprash DV, Nedospasov SA, Hazen SL, Feinstein E, Gudkov AV. p53 is a suppressor of inflammatory response in mice. FASEB J. 2005;19:1030-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 194] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 56. | Schwitalla S, Ziegler PK, Horst D, Becker V, Kerle I, Begus-Nahrmann Y, Lechel A, Rudolph KL, Langer R, Slotta-Huspenina J, Bader FG, Prazeres da Costa O, Neurath MF, Meining A, Kirchner T, Greten FR. Loss of p53 in enterocytes generates an inflammatory microenvironment enabling invasion and lymph node metastasis of carcinogen-induced colorectal tumors. Cancer Cell. 2013;23:93-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 235] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 57. | Elyada E, Pribluda A, Goldstein RE, Morgenstern Y, Brachya G, Cojocaru G, Snir-Alkalay I, Burstain I, Haffner-Krausz R, Jung S, Wiener Z, Alitalo K, Oren M, Pikarsky E, Ben-Neriah Y. CKIα ablation highlights a critical role for p53 in invasiveness control. Nature. 2011;470:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 161] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 58. | Pribluda A, Elyada E, Wiener Z, Hamza H, Goldstein RE, Biton M, Burstain I, Morgenstern Y, Brachya G, Billauer H, Biton S, Snir-Alkalay I, Vucic D, Schlereth K, Mernberger M, Stiewe T, Oren M, Alitalo K, Pikarsky E, Ben-Neriah Y. A senescence-inflammatory switch from cancer-inhibitory to cancer-promoting mechanism. Cancer Cell. 2013;24:242-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 187] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 59. | Liao W, Overman MJ, Boutin AT, Shang X, Zhao D, Dey P, Li J, Wang G, Lan Z, Tang M, Jiang S, Ma X, Chen P, Katkhuda R, Korphaisarn K, Chakravarti D, Chang A, Spring DJ, Chang Q, Zhang J, Maru DM, Maeda DY, Zebala JA, Kopetz S, Wang YA, DePinho RA. KRAS-IRF2 Axis Drives Immune Suppression and Immune Therapy Resistance in Colorectal Cancer. Cancer Cell. 2019;35:559-572.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 455] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 60. | Davalos AR, Coppe JP, Campisi J, Desprez PY. Senescent cells as a source of inflammatory factors for tumor progression. Cancer Metastasis Rev. 2010;29:273-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 412] [Cited by in RCA: 487] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 61. | Bullman S, Pedamallu CS, Sicinska E, Clancy TE, Zhang X, Cai D, Neuberg D, Huang K, Guevara F, Nelson T, Chipashvili O, Hagan T, Walker M, Ramachandran A, Diosdado B, Serna G, Mulet N, Landolfi S, Ramon Y Cajal S, Fasani R, Aguirre AJ, Ng K, Élez E, Ogino S, Tabernero J, Fuchs CS, Hahn WC, Nuciforo P, Meyerson M. Analysis of Fusobacterium persistence and antibiotic response in colorectal cancer. Science. 2017;358:1443-1448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 649] [Cited by in RCA: 1064] [Article Influence: 133.0] [Reference Citation Analysis (0)] |
| 62. | Finegold AA, Shatwell KP, Segal AW, Klausner RD, Dancis A. Intramembrane bis-heme motif for transmembrane electron transport conserved in a yeast iron reductase and the human NADPH oxidase. J Biol Chem. 1996;271:31021-31024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 149] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 63. | Valenti MT, Dalle Carbonare L, Donatelli L, Bertoldo F, Giovanazzi B, Caliari F, Lo Cascio V. STEAP mRNA detection in serum of patients with solid tumours. Cancer Lett. 2009;273:122-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 64. | Krzysiek-Maczka G, Brzozowski T, Ptak-Belowska A. Helicobacter pylori-activated fibroblasts as a silent partner in gastric cancer development. Cancer Metastasis Rev. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 65. | Ajani JA, D'Amico TA, Bentrem DJ, Chao J, Cooke D, Corvera C, Das P, Enzinger PC, Enzler T, Fanta P, Farjah F, Gerdes H, Gibson MK, Hochwald S, Hofstetter WL, Ilson DH, Keswani RN, Kim S, Kleinberg LR, Klempner SJ, Lacy J, Ly QP, Matkowskyj KA, McNamara M, Mulcahy MF, Outlaw D, Park H, Perry KA, Pimiento J, Poultsides GA, Reznik S, Roses RE, Strong VE, Su S, Wang HL, Wiesner G, Willett CG, Yakoub D, Yoon H, McMillian N, Pluchino LA. Gastric Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022;20:167-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 961] [Article Influence: 320.3] [Reference Citation Analysis (0)] |
| 66. | Boyanova L. Role of Helicobacter pylori virulence factors for iron acquisition from gastric epithelial cells of the host and impact on bacterial colonization. Future Microbiol. 2011;6:843-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 67. | Senkovich O, Ceaser S, McGee DJ, Testerman TL. Unique host iron utilization mechanisms of Helicobacter pylori revealed with iron-deficient chemically defined media. Infect Immun. 2010;78:1841-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 68. | Hamedi Asl D, Naserpour Farivar T, Rahmani B, Hajmanoochehri F, Emami Razavi AN, Jahanbin B, Soleimani Dodaran M, Peymani A. The role of transferrin receptor in the Helicobacter pylori pathogenesis; L-ferritin as a novel marker for intestinal metaplasia. Microb Pathog. 2019;126:157-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 69. | Wu S, Chen Y, Chen Z, Wei F, Zhou Q, Li P, Gu Q. Reactive oxygen species and gastric carcinogenesis: The complex interaction between Helicobacter pylori and host. Helicobacter. 2023;28:e13024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 70. | Wu YY, Jiang JN, Fang XD, Ji FJ. STEAP1 Regulates Tumorigenesis and Chemoresistance During Peritoneal Metastasis of Gastric Cancer. Front Physiol. 2018;9:1132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 71. | Jiang JN, Wu YY, Fang XD, Ji FJ. EIF4E regulates STEAP1 expression in peritoneal metastasis. J Cancer. 2020;11:990-996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 72. | Zhang Z, Hou WB, Zhang C, Tan YE, Zhang DD, An W, Pan SW, Wu WD, Chen QC, Xu HM. A research of STEAP1 regulated gastric cancer cell proliferation, migration and invasion in vitro and in vivos. J Cell Mol Med. 2020;24:14217-14230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 73. | Fang ZX, Hou YY, Wu Z, Wu BX, Deng Y, Wu HT, Liu J. Immune responses of six-transmembrane epithelial antigen of the prostate 4 functions as a novel biomarker in gastric cancer. World J Clin Oncol. 2023;14:297-310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Reference Citation Analysis (2)] |
| 74. | Yin Y, Wan J, Yu J, Wu K. Molecular Pathogenesis of Colitis-associated Colorectal Cancer: Immunity, Genetics, and Intestinal Microecology. Inflamm Bowel Dis. 2023;29:1648-1657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 75. | Focarelli F, Giachino A, Waldron KJ. Copper microenvironments in the human body define patterns of copper adaptation in pathogenic bacteria. PLoS Pathog. 2022;18:e1010617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 49] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 76. | Wang L, Hu C, Wang B, Wang H, Wang C, Shu Y, Gao C, Yan Y. Chronic environmentally relevant concentration of copper exposure induces intestinal oxidative stress, inflammation, and microbiota disturbance in freshwater grouper (Acrossocheilus fasciatus). Aquat Toxicol. 2023;263:106702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 77. | Miller KA, Vicentini FA, Hirota SA, Sharkey KA, Wieser ME. Antibiotic treatment affects the expression levels of copper transporters and the isotopic composition of copper in the colon of mice. Proc Natl Acad Sci U S A. 2019;116:5955-5960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 78. | Yang D, Holt GE, Velders MP, Kwon ED, Kast WM. Murine six-transmembrane epithelial antigen of the prostate, prostate stem cell antigen, and prostate-specific membrane antigen: prostate-specific cell-surface antigens highly expressed in prostate cancer of transgenic adenocarcinoma mouse prostate mice. Cancer Res. 2001;61:5857-5860. [PubMed] |
| 79. | Moreaux J, Kassambara A, Hose D, Klein B. STEAP1 is overexpressed in cancers: a promising therapeutic target. Biochem Biophys Res Commun. 2012;429:148-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 80. | Nakamura H, Takada K, Arihara Y, Hayasaka N, Murase K, Iyama S, Kobune M, Miyanishi K, Kato J. Six-transmembrane epithelial antigen of the prostate 1 protects against increased oxidative stress via a nuclear erythroid 2-related factor pathway in colorectal cancer. Cancer Gene Ther. 2019;26:313-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 81. | Rodeberg DA, Nuss RA, Elsawa SF, Celis E. Recognition of six-transmembrane epithelial antigen of the prostate-expressing tumor cells by peptide antigen-induced cytotoxic T lymphocytes. Clin Cancer Res. 2005;11:4545-4552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 82. | Alves PM, Faure O, Graff-Dubois S, Cornet S, Bolonakis I, Gross DA, Miconnet I, Chouaib S, Fizazi K, Soria JC, Lemonnier FA, Kosmatopoulos K. STEAP, a prostate tumor antigen, is a target of human CD8+ T cells. Cancer Immunol Immunother. 2006;55:1515-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 83. | Barresi V, Trovato-Salinaro A, Spampinato G, Musso N, Castorina S, Rizzarelli E, Condorelli DF. Transcriptome analysis of copper homeostasis genes reveals coordinated upregulation of SLC31A1,SCO1, and COX11 in colorectal cancer. FEBS Open Bio. 2016;6:794-806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 84. | Ma H, Shu Q, Li D, Wang T, Li L, Song X, Lou K, Xu H. Accumulation of Intracellular Ferrous Iron in Inflammatory-Activated Macrophages. Biol Trace Elem Res. 2023;201:2303-2310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 85. | Isobe T, Baba E, Arita S, Komoda M, Tamura S, Shirakawa T, Ariyama H, Takaishi S, Kusaba H, Ueki T, Akashi K. Human STEAP3 maintains tumor growth under hypoferric condition. Exp Cell Res. 2011;317:2582-2591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 86. | Wan C, Fu J, Wang Y, Miao S, Song W, Wang L. Exosome-related multi-pass transmembrane protein TSAP6 is a target of rhomboid protease RHBDD1-induced proteolysis. PLoS One. 2012;7:e37452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 87. | Wu Z, Fang ZX, Hou YY, Wu BX, Deng Y, Wu HT, Liu J. Exosomes in metastasis of colorectal cancers: Friends or foes? World J Gastrointest Oncol. 2023;15:731-756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 88. | Zhou L, Jiang J, Huang Z, Jin P, Peng L, Luo M, Zhang Z, Chen Y, Xie N, Gao W, Nice EC, Li JQ, Chen HN, Huang C. Hypoxia-induced lncRNA STEAP3-AS1 activates Wnt/β-catenin signaling to promote colorectal cancer progression by preventing m(6)A-mediated degradation of STEAP3 mRNA. Mol Cancer. 2022;21:168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 99] [Reference Citation Analysis (0)] |
| 89. | Fang ZX, Li CL, Chen WJ, Wu HT, Liu J. Potential of six-transmembrane epithelial antigen of the prostate 4 as a prognostic marker for colorectal cancer. World J Gastrointest Oncol. 2022;14:1675-1688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 90. | Xue X, Bredell BX, Anderson ER, Martin A, Mays C, Nagao-Kitamoto H, Huang S, Győrffy B, Greenson JK, Hardiman K, Spence JR, Kamada N, Shah YM. Quantitative proteomics identifies STEAP4 as a critical regulator of mitochondrial dysfunction linking inflammation and colon cancer. Proc Natl Acad Sci U S A. 2017;114:E9608-E9617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 91. | Liao Y, Zhao J, Bulek K, Tang F, Chen X, Cai G, Jia S, Fox PL, Huang E, Pizarro TT, Kalady MF, Jackson MW, Bao S, Sen GC, Stark GR, Chang CJ, Li X. Inflammation mobilizes copper metabolism to promote colon tumorigenesis via an IL-17-STEAP4-XIAP axis. Nat Commun. 2020;11:900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 148] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 92. | Gutiérrez-Cuevas J, Lucano-Landeros S, López-Cifuentes D, Santos A, Armendariz-Borunda J. Epidemiologic, Genetic, Pathogenic, Metabolic, Epigenetic Aspects Involved in NASH-HCC: Current Therapeutic Strategies. Cancers (Basel). 2022;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 93. | Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004;127:S5-S16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1799] [Cited by in RCA: 1816] [Article Influence: 86.5] [Reference Citation Analysis (0)] |
| 94. | Tong MJ, el-Farra NS, Reikes AR, Co RL. Clinical outcomes after transfusion-associated hepatitis C. N Engl J Med. 1995;332:1463-1466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 855] [Cited by in RCA: 819] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 95. | Costas-Rodríguez M, Anoshkina Y, Lauwens S, Van Vlierberghe H, Delanghe J, Vanhaecke F. Isotopic analysis of Cu in blood serum by multi-collector ICP-mass spectrometry: a new approach for the diagnosis and prognosis of liver cirrhosis? Metallomics. 2015;7:491-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 96. | Lauwens S, Costas-Rodríguez M, Van Vlierberghe H, Vanhaecke F. Cu isotopic signature in blood serum of liver transplant patients: a follow-up study. Sci Rep. 2016;6:30683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 97. | Boswell CA, Mundo EE, Zhang C, Bumbaca D, Valle NR, Kozak KR, Fourie A, Chuh J, Koppada N, Saad O, Gill H, Shen BQ, Rubinfeld B, Tibbitts J, Kaur S, Theil FP, Fielder PJ, Khawli LA, Lin K. Impact of drug conjugation on pharmacokinetics and tissue distribution of anti-STEAP1 antibody-drug conjugates in rats. Bioconjug Chem. 2011;22:1994-2004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 155] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 98. | O'Donoghue JA, Danila DC, Pandit-Taskar N, Beylergil V, Cheal SM, Fleming SE, Fox JJ, Ruan S, Zanzonico PB, Ragupathi G, Lyashchenko SK, Williams SP, Scher HI, Fine BM, Humm JL, Larson SM, Morris MJ, Carrasquillo JA. Pharmacokinetics and Biodistribution of a [(89)Zr]Zr-DFO-MSTP2109A Anti-STEAP1 Antibody in Metastatic Castration-Resistant Prostate Cancer Patients. Mol Pharm. 2019;16:3083-3090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 99. | Iijima K, Nakamura H, Takada K, Hayasaka N, Kubo T, Umeyama Y, Iyama S, Miyanishi K, Kobune M, Kato J. Six-transmembrane epithelial antigen of the prostate 1 accelerates cell proliferation by targeting c-Myc in liver cancer cells. Oncol Lett. 2021;22:546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 100. | Guo WZ, Fang HB, Cao SL, Chen SY, Li J, Shi JH, Tang HW, Zhang Y, Wen PH, Zhang JK, Wang ZH, Shi XY, Pang C, Yang H, Hu BW, Zhang SJ. Six-Transmembrane Epithelial Antigen of the Prostate 3 Deficiency in Hepatocytes Protects the Liver Against Ischemia-Reperfusion Injury by Suppressing Transforming Growth Factor-β-Activated Kinase 1. Hepatology. 2020;71:1037-1054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 101. | Wang LL, Luo J, He ZH, Liu YQ, Li HG, Xie D, Cai MY. STEAP3 promotes cancer cell proliferation by facilitating nuclear trafficking of EGFR to enhance RAC1-ERK-STAT3 signaling in hepatocellular carcinoma. Cell Death Dis. 2021;12:1052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 102. | Yi Q, Liang Q, Liu Y, Gong Z, Yan Y. Application of genomic selection and experimental techniques to predict cell death and immunotherapeutic efficacy of ferroptosis-related CXCL2 in hepatocellular carcinoma. Front Oncol. 2022;12:998736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 103. | Wang S, Chen L, Liu W. Matrix stiffness-dependent STEAP3 coordinated with PD-L2 identify tumor responding to sorafenib treatment in hepatocellular carcinoma. Cancer Cell Int. 2022;22:318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 104. | Ramadoss P, Chiappini F, Bilban M, Hollenberg AN. Regulation of hepatic six transmembrane epithelial antigen of prostate 4 (STEAP4) expression by STAT3 and CCAAT/enhancer-binding protein alpha. J Biol Chem. 2010;285:16453-16466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 105. | Kim HY, Cho HK, Yoo SK, Cheong JH. Hepatic STAMP2 decreases hepatitis B virus X protein-associated metabolic deregulation. Exp Mol Med. 2012;44:622-632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 106. | Kim HY, Kwon WY, Park JB, Lee MH, Oh YJ, Suh S, Baek YH, Jeong JS, Yoo YH. Hepatic STAMP2 mediates recombinant FGF21-induced improvement of hepatic iron overload in nonalcoholic fatty liver disease. FASEB J. 2020;34:12354-12366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 107. | Yamada N, Yasui K, Dohi O, Gen Y, Tomie A, Kitaichi T, Iwai N, Mitsuyoshi H, Sumida Y, Moriguchi M, Yamaguchi K, Nishikawa T, Umemura A, Naito Y, Tanaka S, Arii S, Itoh Y. Genome-wide DNA methylation analysis in hepatocellular carcinoma. Oncol Rep. 2016;35:2228-2236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 108. | Wu HC, Yang HI, Wang Q, Chen CJ, Santella RM. Plasma DNA methylation marker and hepatocellular carcinoma risk prediction model for the general population. Carcinogenesis. 2017;38:1021-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 109. | Ju MH, Jang EJ, Kang SH, Roh YH, Jeong JS, Han SH. Six-Transmembrane Epithelial Antigen of Prostate 4: An Indicator of Prognosis and Tumor Immunity in Hepatocellular Carcinoma. J Hepatocell Carcinoma. 2023;10:643-658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 110. | Abril AG, Carrera M, Sánchez-Pérez Á, Villa TG. Gut Microbiome Proteomics in Food Allergies. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 111. | Ayyaswamy S, Shi H, Zhang B, Bryan RM Jr, Durgan DJ. Obstructive Sleep Apnea-Induced Hypertension Is Associated With Increased Gut and Neuroinflammation. J Am Heart Assoc. 2023;12:e029218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 112. | Gopalakrishnan S, Thomas R, Sedaghat S, Krishnakumar A, Khan S, Meyer T, Ajieren H, Nejati S, Wang J, Verma MS, Irazoqui P, Rahimi R. Smart capsule for monitoring inflammation profile throughout the gastrointestinal tract. Biosens Bioelectron X. 2023;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 113. | Yang L, Wang T, Zhang X, Zhang H, Yan N, Zhang G, Yan R, Li Y, Yu J, He J, Jia S, Wang H. Exosomes derived from human placental mesenchymal stem cells ameliorate myocardial infarction via anti-inflammation and restoring gut dysbiosis. BMC Cardiovasc Disord. 2022;22:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 114. | Lima SF, Gogokhia L, Viladomiu M, Chou L, Putzel G, Jin WB, Pires S, Guo CJ, Gerardin Y, Crawford CV, Jacob V, Scherl E, Brown SE, Hambor J, Longman RS. Transferable Immunoglobulin A-Coated Odoribacter splanchnicus in Responders to Fecal Microbiota Transplantation for Ulcerative Colitis Limits Colonic Inflammation. Gastroenterology. 2022;162:166-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 106] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 115. | Challita-Eid PM, Morrison K, Etessami S, An Z, Morrison KJ, Perez-Villar JJ, Raitano AB, Jia XC, Gudas JM, Kanner SB, Jakobovits A. Monoclonal antibodies to six-transmembrane epithelial antigen of the prostate-1 inhibit intercellular communication in vitro and growth of human tumor xenografts in vivo. Cancer Res. 2007;67:5798-5805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 81] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 116. | Yamamoto T, Tamura Y, Kobayashi J, Kamiguchi K, Hirohashi Y, Miyazaki A, Torigoe T, Asanuma H, Hiratsuka H, Sato N. Six-transmembrane epithelial antigen of the prostate-1 plays a role for in vivo tumor growth via intercellular communication. Exp Cell Res. 2013;319:2617-2626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 117. | Barroca-Ferreira J, Pais JP, Santos MM, Goncalves AM, Gomes IM, Sousa I, Rocha SM, Passarinha LA, Maia CJ. Targeting STEAP1 Protein in Human Cancer: Current Trends and Future Challenges. Curr Cancer Drug Targets. 2018;18:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 118. | Cole G, McCaffrey J, Ali AA, McCarthy HO. DNA vaccination for prostate cancer: key concepts and considerations. Cancer Nanotechnol. 2015;6:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 119. | Carrasquillo JA, Fine BM, Pandit-Taskar N, Larson SM, Fleming SE, Fox JJ, Cheal SM, O'Donoghue JA, Ruan S, Ragupathi G, Lyashchenko SK, Humm JL, Scher HI, Gönen M, Williams SP, Danila DC, Morris MJ. Imaging Patients with Metastatic Castration-Resistant Prostate Cancer Using (89)Zr-DFO-MSTP2109A Anti-STEAP1 Antibody. J Nucl Med. 2019;60:1517-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 120. | Qin DN, Kou CZ, Ni YH, Zhang CM, Zhu JG, Zhu C, Wang YP, Zhu GZ, Shi C, Ji CB, Guo XR. Monoclonal antibody to the six-transmembrane epithelial antigen of prostate 4 promotes apoptosis and inhibits proliferation and glucose uptake in human adipocytes. Int J Mol Med. 2010;26:803-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 121. | Lin TY, Park JA, Long A, Guo HF, Cheung NV. Novel potent anti-STEAP1 bispecific antibody to redirect T cells for cancer immunotherapy. J Immunother Cancer. 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 122. | Bai XF, Liu J, Li O, Zheng P, Liu Y. Antigenic drift as a mechanism for tumor evasion of destruction by cytolytic T lymphocytes. J Clin Invest. 2003;111:1487-1496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 123. | Melief CJ, Toes RE, Medema JP, van der Burg SH, Ossendorp F, Offringa R. Strategies for immunotherapy of cancer. Adv Immunol. 2000;75:235-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 114] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 124. | Andersen MH, Pedersen LO, Becker JC, Straten PT. Identification of a cytotoxic T lymphocyte response to the apoptosis inhibitor protein survivin in cancer patients. Cancer Res. 2001;61:869-872. [PubMed] |
| 125. | Alves PM, Faure O, Graff-Dubois S, Gross DA, Cornet S, Chouaib S, Miconnet I, Lemonnier FA, Kosmatopoulos K. EphA2 as target of anticancer immunotherapy: identification of HLA-A*0201-restricted epitopes. Cancer Res. 2003;63:8476-8480. [PubMed] |
| 126. | Faure O, Graff-Dubois S, Bretaudeau L, Derré L, Gross DA, Alves PM, Cornet S, Duffour MT, Chouaib S, Miconnet I, Grégoire M, Jotereau F, Lemonnier FA, Abastado JP, Kosmatopoulos K. Inducible Hsp70 as target of anticancer immunotherapy: Identification of HLA-A*0201-restricted epitopes. Int J Cancer. 2004;108:863-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 127. | Graff-Dubois S, Faure O, Gross DA, Alves P, Scardino A, Chouaib S, Lemonnier FA, Kosmatopoulos K. Generation of CTL recognizing an HLA-A*0201-restricted epitope shared by MAGE-A1, -A2, -A3, -A4, -A6, -A10, and -A12 tumor antigens: implication in a broad-spectrum tumor immunotherapy. J Immunol. 2002;169:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 128. | Azumi M, Kobayashi H, Aoki N, Sato K, Kimura S, Kakizaki H, Tateno M. Six-transmembrane epithelial antigen of the prostate as an immunotherapeutic target for renal cell and bladder cancer. J Urol. 2010;183:2036-2044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |