Published online Aug 24, 2023. doi: 10.5306/wjco.v14.i8.311
Peer-review started: May 7, 2023
First decision: July 4, 2023
Revised: July 12, 2023
Accepted: August 8, 2023
Article in press: August 8, 2023
Published online: August 24, 2023
Processing time: 106 Days and 5 Hours
The coronavirus disease 2019 (COVID-19) pandemic has received considerable attention in the scientific community due to its impact on healthcare systems and various diseases. However, little focus has been given to its effect on cancer treatment.
To determine the effect of COVID-19 pandemic on cancer patients’ care.
A retrospective review of a Nationwide Readmission Database (NRD) was conducted to analyze hospitalization patterns of patients receiving inpatient chemotherapy (IPCT) during the COVID-19 pandemic in 2020. Two cohorts were defined based on readmission within 30 d and 90 d. Demographic information, readmission rates, hospital-specific variables, length of hospital stay (LOS), and treatment costs were analyzed. Comorbidities were assessed using the Elixhauser comorbidity index. Multivariate Cox regression analysis was performed to identify independent predictors of readmission. Statistical analysis was conducted using Stata® Version 16 software. As the NRD data is anonymous and cannot be used to identify patients, institutional review board approval was not required for this study.
A total of 87755 hospitalizations for IPCT were identified during the pandemic. Among the 30-day index admission cohort, 55005 patients were included, with 32903 readmissions observed, resulting in a readmission rate of 59.8%. For the 90-day index admission cohort, 33142 patients were included, with 24503 readmissions observed, leading to a readmission rate of 73.93%. The most common causes of readmission included encounters with chemotherapy (66.7%), neutropenia (4.36%), and sepsis (3.3%). Comorbidities were significantly higher among readmitted hospitalizations compared to index hospitalizations in both readmission cohorts. The total cost of readmission for both cohorts amounted to 1193000000.00 dollars. Major predictors of 30-day readmission included peripheral vascular disorders [Hazard ratio (HR) = 1.09, P < 0.05], paralysis (HR = 1.26, P < 0.001), and human immunodeficiency virus/acquired immuno-deficiency syndrome (HR = 1.14, P = 0.03). Predictors of 90-day readmission included lymphoma (HR = 1.14, P < 0.01), paralysis (HR = 1.21, P = 0.02), and peripheral vascular disorders (HR = 1.15, P < 0.01).
The COVID-19 pandemic has significantly impacted the management of patients undergoing IPCT. These findings highlight the urgent need for a more strategic approach to the care of patients receiving IPCT during pandemics.
Core Tip: Our nationwide study explored care for patients undergoing inpatient chemotherapy during the coronavirus disease 2019 (COVID-19) pandemic. It is the first to analyze factors surrounding hospitalization for such patients. We found a higher readmission rate during the pandemic, with comorbidities posing a greater risk. Surprisingly, COVID-19 infection was not significantly linked to readmission. Hospitalization costs rose, averaging 22952.00 dollars. Our findings would interest the scientific community, hospital managers, and health policymakers. Understanding the pandemic's impact on cancer patients' care can lead to mitigating health policies.
- Citation: Kanemo P, Musa KM, Deenadayalan V, Litvin R, Odeyemi OE, Shaka A, Baskaran N, Shaka H. Readmission rates and outcomes in adults with and without COVID-19 following inpatient chemotherapy admission: A nationwide analysis. World J Clin Oncol 2023; 14(8): 311-323
- URL: https://www.wjgnet.com/2218-4333/full/v14/i8/311.htm
- DOI: https://dx.doi.org/10.5306/wjco.v14.i8.311
On the 11th of March 2020, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) a global pandemic following its discovery in December 2019 in Wuhan, China[1,2]. Since then, WHO has reported over 756 million cases and 6.8 million deaths worldwide[3], with the United States alone accounting for over 100 million cases and 1 million deaths[3]. COVID-19 is caused by a virus known as severe acute respiratory syndrome coronavirus 2[4], which results in a range of respiratory symptoms from mild to severe[4]. However, the introduction and widespread administration of COVID-19 vaccines have contributed to a decline in infection rates[5].
The COVID-19 pandemic has had a profound impact on various aspects of human life[6], with healthcare services and delivery being particularly affected[7,8]. The 30-day readmission rate serves as a crucial metric used by the Center for Medicare and Medicaid Services to evaluate hospitals and assess the quality of healthcare services[9,10]. In 2012, the Center for Medicare and Medicaid Services introduced the Hospital Readmission Reduction Program to enhance healthcare quality and reduce costs[11]. The annual cost associated with readmissions averages between 15 and 20 billion dollars[12]. Reducing the 30-day readmission rates can significantly decrease healthcare costs and alleviate the strain on healthcare facilities[13]. Assessing readmission rates becomes even more important for patients undergoing chemotherapy, as chemotherapy often entails extended periods of treatment and substantial healthcare expenses[13]. A systematic review conducted prior to the COVID-19 pandemic revealed readmission rates ranging from 3% to 34% for patients undergoing chemotherapy[14]. Another study by Tennison et al[14] reported a 55% readmission rate for patients undergoing chemotherapy in United States hospitals. However, since the onset of the COVID-19 pandemic, there has been a scarcity of data regarding the hospitalization and care of patients receiving chemotherapy during this period.
This study aims to investigate the impact of the COVID-19 pandemic on 30-day and 90-day readmission rates among patients hospitalized for inpatient chemotherapy (IPCT). We also aim to identify common causes and independent predictors of readmission in this patient population. By conducting this study, we aim to gain a deeper understanding of the effects of COVID-19 on the management of cancer patients. Furthermore, the findings of this study can contribute to the development of strategies that improve the care of cancer patients. Finally, we believe that this study will pave the way for further research on the effects of pandemics on healthcare infrastructure and services.
We conducted a retrospective cross-sectional review of hospitalizations for IPCT across the United States during a one-year period in 2020. Hospitalization data for 2020 was retrieved from the Nationwide Readmission Database (NRD). The NRD is a national database that captures patients' hospitalization, readmissions, and other relevant discharge histories from over 31 different states in the United States. The NRD is a product of the Healthcare Cost and Utilization Project (HCUP), State Inpatient Databases, and the Agency for Healthcare Research and Quality[9]. The database records over 40 International Classification of Diseases-10 (ICD-10) recognized diagnoses and 25 procedures[9]. It covers approximately 62.2% of the United States population and 60.8% of total hospitalizations in the country[15]. It contains unique, verified de-identified patient linkage that enables tracking of individual hospitalizations and readmissions. Data within the NRD is available from January 1 to December 31 each year, and information outside of these dates cannot be accessed[16]. With over 18 million hospital stays recorded, the NRD provides ample and suitable data for our study.
We collected data on adult hospitalizations (age >18 years) for IPCT during the COVID-19 pandemic in 2020. Hospitalizations for conditions other than IPCT and those involving patients under 18 years of age were excluded from the study. Additionally, hospitalizations in December were excluded due to the lack of an adjoining 30-day period to determine 30-day readmission. The hospitalizations were divided into two groups: The 30-day readmission cohort (30DRC) and the 90-day readmission cohort (90DRC). Within each cohort, we identified and tagged each case that met our inclusion criteria as an index case on the first admission. Each index case was traced for readmission within 30 d of admission and tagged as a 30-day readmission in the 30DRC. Similarly, each index case was traced for readmission within 90 d of admission and tagged as a 90-day readmission in the 90DRC. Specific patient data, including demographics (age, sex, health insurance type, household income), mortality on readmission, LOS, and cost of admission, were collected. Hospital-specific variables, such as type of hospital, bed size, and hospital location, were also obtained. To account for the effects of comorbid conditions, we utilized the Elixhauser Comorbidity Index (ECI) to assess the level of comorbidities in the hospitalizations. The ECI is a software tool developed as part of HCUP, which identifies 38 different pre-existing comorbidities in hospital administrative data[15]. The ECI software has been refined for ICD-10 comorbidities and is available in nationwide HCUP databases for years 2019 onwards[15]. The ECI demonstrates a better prognostic value compared to the Charlson comorbidity index[16].
The primary outcome of our study was the all-cause 30-day and 90-day readmission rates. Secondary outcomes included demographic characteristics, insurance type, mortality rate during readmission, average LOS, average cost of readmission, and independent predictors of readmission.
All analyses were performed using weighted samples for national estimates in accordance with HCUP regulations for using the NRD[17]. Data analysis was conducted using Stata® Version 16 software (StataCorp, Texas, United States). We examined demographic characteristics and calculated mean age, sex distribution, and mean household income. Additionally, we analyzed hospital-specific features, including hospital location, teaching status, and bed size. Comorbidities were calculated as proportions in our cohorts using the 31 ECI comorbidities, and the chi-square test was employed to compare characteristics between index hospitalizations and readmissions in 2020. A multivariate Cox regression analysis was performed to identify independent variables associated with readmission.
As with other HCUP databases, the NRD data is anonymous and cannot be used to identify individual patients. Therefore, institutional review board approval was not required for our study.
We identified a total of 87756 hospitalizations for IPCT in the 2020 NRD database. In the 30DRC, we identified 55005 index hospitalizations during the study period. Among these, there were 32904 readmissions within 30 d, resulting in a 30-day readmission rate of 59.8%. Table 1 provides a comparison of the demographics of hospitalized patients between index hospitalizations and readmission cohort. Among the 90DRC, we identified 33636 index hospitalizations, of which 24503 patients were readmitted within 90 d of admission. The 90-day readmission rate was 73.93%. In both readmission cohorts, the proportion of male patients was higher than female patients. The majority of hospitalized patients in both cohorts were in their middle age. Private health insurance was the primary payer for hospital bills in most cases. A significant number of patients in both readmission cohorts belonged to the 26th-50th quantile of the national median household income. The rates of 30-day and 90-day readmission were higher in patients with Medicaid and private insurance, as well as those with a higher comorbidity burden (ECI score ≥ 4).
| Variables (unit) | Index admission | 30 d readmission | P value |
| Mean age ± SD (yr) | 54.7 ± 17.71 | 53.53 ± 17.94 | |
| Age range categories (%) | < 0.001 | ||
| 18-44 yr | 26.86 | 29.5 | |
| 45-64 yr | 40.06 | 39.62 | |
| 65 yr and above | 33.08 | 30.89 | |
| Sex (%) | 0.182 | ||
| Male | 58.07 | 58.47 | |
| Female | 41.93 | 41.53 | |
| Payer type (%) | < 0.001 | ||
| Medicare | 34.43 | 32.33 | |
| Medicaid | 17.06 | 18.14 | |
| Private insurance | 46.14 | 47.25 | |
| Self pay | 2.36 | 2.28 | |
| Median household income (%) | 0.617 | ||
| 0-25th quintile | 22.28 | 21.96 | |
| 26th-50th quintile | 27.91 | 28.02 | |
| 50th-75th quintile | 25.61 | 25.85 | |
| > 75th quintile | 24.19 | 24.18 | |
| ECI score (%) | < 0.001 | ||
| 0 | 4.88 | 4.14 | |
| 1 | 18.61 | 17.7 | |
| 2 | 23.75 | 23.35 | |
| 3 | 20.61 | 20.53 | |
| ≥ 4 | 32.15 | 34.28 |
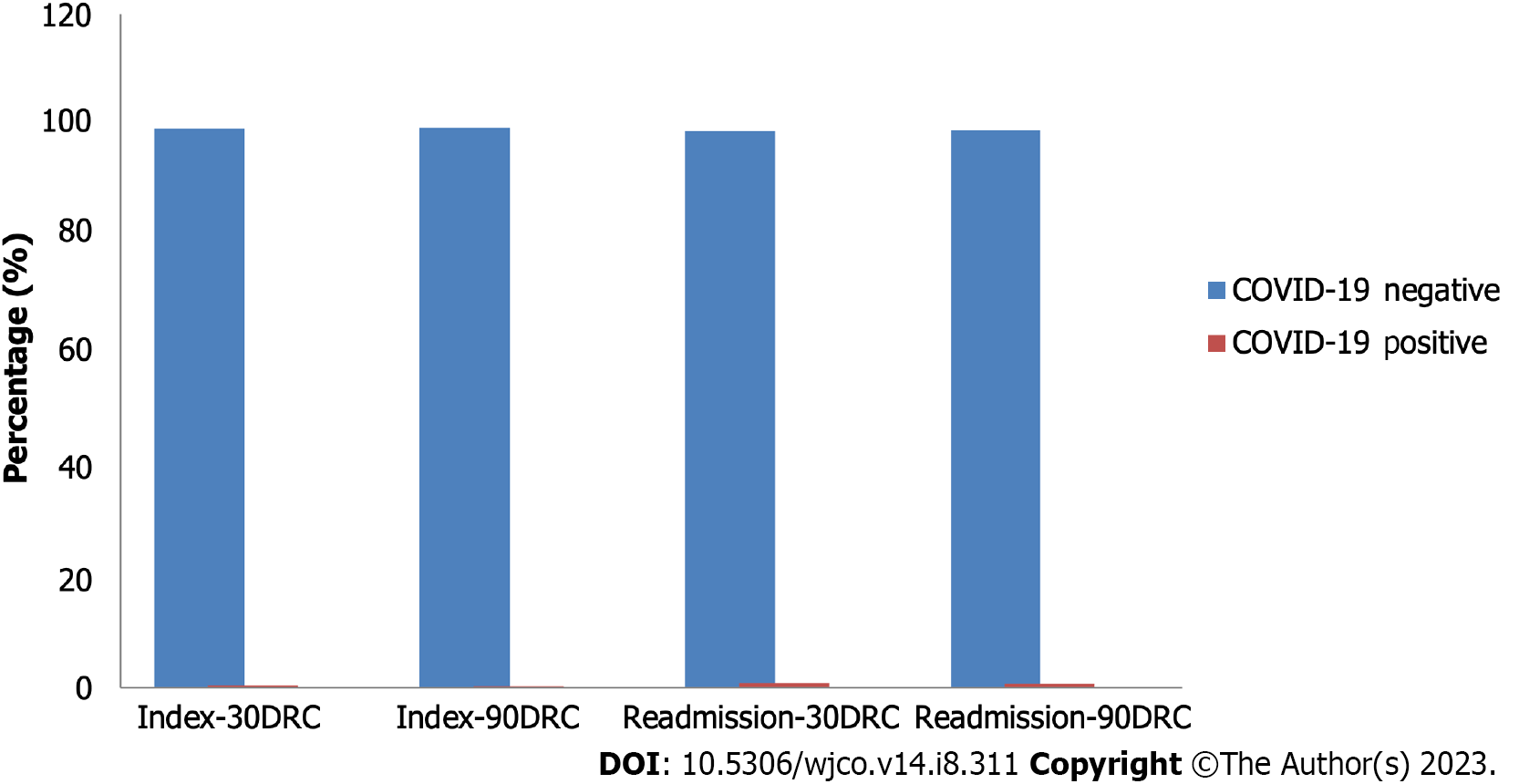
Comorbidities analyzed were significantly more prevalent in readmissions compared to index hospitalizations in both readmission cohorts. Detailed comparisons of comorbidities between index hospitalizations and readmissions in the 30DRCs and 90DRCs are listed in Tables 2 and 3, respectively. The majority of patients tested negative for COVID-19 in both index hospitalizations and readmissions, as depicted in Figure 1. Metropolitan teaching hospitals had the highest number of admissions in both cohorts. Table 4 summarizes the hospital characteristics among index hospitalizations and readmissions.
| Variables (%) | Index | Readmission | P value |
| Congestive heart failure | 5.45 | 5.83 | 0.02 |
| Cardiac arrhythmias | 12.14 | 13.13 | < 0.001 |
| Valvular diseases | 2.48 | 2.12 | 0.001 |
| Pulmonary circulation disorders | 2.1 | 2.47 | 0.001 |
| Peripheral vascular disorders | 4.81 | 5.1 | 0.141 |
| Hypertension, uncomplicated | 34.12 | 32.88 | 0.001 |
| Paralysis | 1.06 | 1.17 | 0.181 |
| Other neurologic disorders | 4.72 | 5.72 | < 0.001 |
| Chronic pulmonary disease | 11.07 | 10.5 | 0.012 |
| Diabetics, uncomplicated | 8.44 | 8.5 | 0.757 |
| Diabetics, complicated | 8.63 | 8.28 | 0.105 |
| Hypothyroidism | 9.88 | 9.61 | 0.134 |
| Renal failure | 7.75 | 6.89 | < 0.001 |
| Liver disease | 4.06 | 4.09 | 0.854 |
| Peptic ulcer disease | 0.34 | 0.33 | 0.859 |
| HIV/AIDS | 1.26 | 1.44 | 0.003 |
| Lymphoma | 45.89 | 48.77 | < 0.001 |
| Metastatic cancer | 14.93 | 14.78 | 0.637 |
| Solid tumor without metastasis | 24.4 | 24.84 | 0.255 |
| RA/collagen vascular disease | 2.03 | 1.9 | 0.226 |
| Coagulopathy | 12.64 | 14.41 | < 0.001 |
| Obesity | 10.33 | 9.81 | 0.159 |
| Weight loss | 10.76 | 11.12 | 0.207 |
| Fluid and electrolyte disorders | 23.17 | 28.16 | < 0.001 |
| Blood loss anemia | 0.39 | 0.35 | 0.497 |
| Deficiency anemia | 3.09 | 2.63 | 0.001 |
| Alcohol abuse | 1.13 | 0.98 | 0.103 |
| Drug abuse | 2.32 | 2.35 | 0.832 |
| Psychosis | 0.68 | 0.76 | 0.089 |
| Depression | 12.39 | 12.59 | 0.429 |
| Hypertension, complicated | 8.04 | 7.66 | 0.063 |
| Variables (%) | Index | Readmission | P value |
| Congestive heart failure | 5.88 | 6.59 | 0.002 |
| Cardiac arrhythmias | 13.16 | 14.17 | 0.001 |
| Valvular diseases | 2.69 | 2.19 | 0.001 |
| Pulmonary circulation disorders | 2.28 | 2.57 | 0.052 |
| Peripheral vascular disorders | 4.72 | 5.19 | 0.024 |
| Hypertension, uncomplicated | 34.58 | 33.12 | < 0.001 |
| Paralysis | 1.09 | 1.13 | 0.645 |
| Other neurologic disorders | 4.81 | 5.91 | < 0.001 |
| Chronic pulmonary disease | 11.68 | 11.09 | 0.026 |
| Diabetics, uncomplicated | 8.54 | 8.51 | 0.908 |
| Diabetics, complicated | 8.86 | 8.7 | 0.539 |
| Hypothyroidism | 10.31 | 9.77 | 0.003 |
| Renal failure | 8.38 | 7.88 | 0.033 |
| Liver disease | 4.36 | 4.42 | 0.814 |
| Peptic ulcer disease | 0.29 | 0.37 | 0.196 |
| HIV/AIDS | 1.09 | 1.12 | 0.667 |
| Lymphoma | 43.95 | 44.89 | 0.012 |
| Metastatic cancer | 15.5 | 14.48 | < 0.001 |
| Solid tumor without metastasis | 24.39 | 23.94 | 0.181 |
| RA/collagen vascular disease | 2.13 | 1.91 | 0.077 |
| Coagulopathy | 13.27 | 15.73 | < 0.001 |
| Obesity | 10.41 | 9.77 | 0.166 |
| Weight loss | 11.8 | 12.44 | 0.055 |
| Fluid and electrolyte disorders | 24.87 | 30.26 | < 0.001 |
| Blood loss anemia | 0.44 | 0.42 | 0.876 |
| Deficiency anemia | 3.16 | 2.51 | < 0.001 |
| Alcohol abuse | 1.29 | 1.13 | 0.144 |
| Drug abuse | 2.33 | 2.31 | 0.922 |
| Psychosis | 0.71 | 0.77 | 0.269 |
| Depression | 12.23 | 12.95 | 0.015 |
| Hypertension, complicated | 8.81 | 8.75 | 0.785 |
| Variables | Index | Readmission | P value |
| Hospital bed size (%) | 0.002 | ||
| Small | 7.51 | 8.49 | |
| Medium | 15.96 | 16.01 | |
| Large | 76.53 | 75.5 | |
| Teaching status of hospital (%) | 0.002 | ||
| Metropolitan, non teaching | 5.51 | 6.09 | |
| Metropolitan teaching | 93.48 | 92.27 | |
| Non-metropolitan | 1.01 | 1.64 |
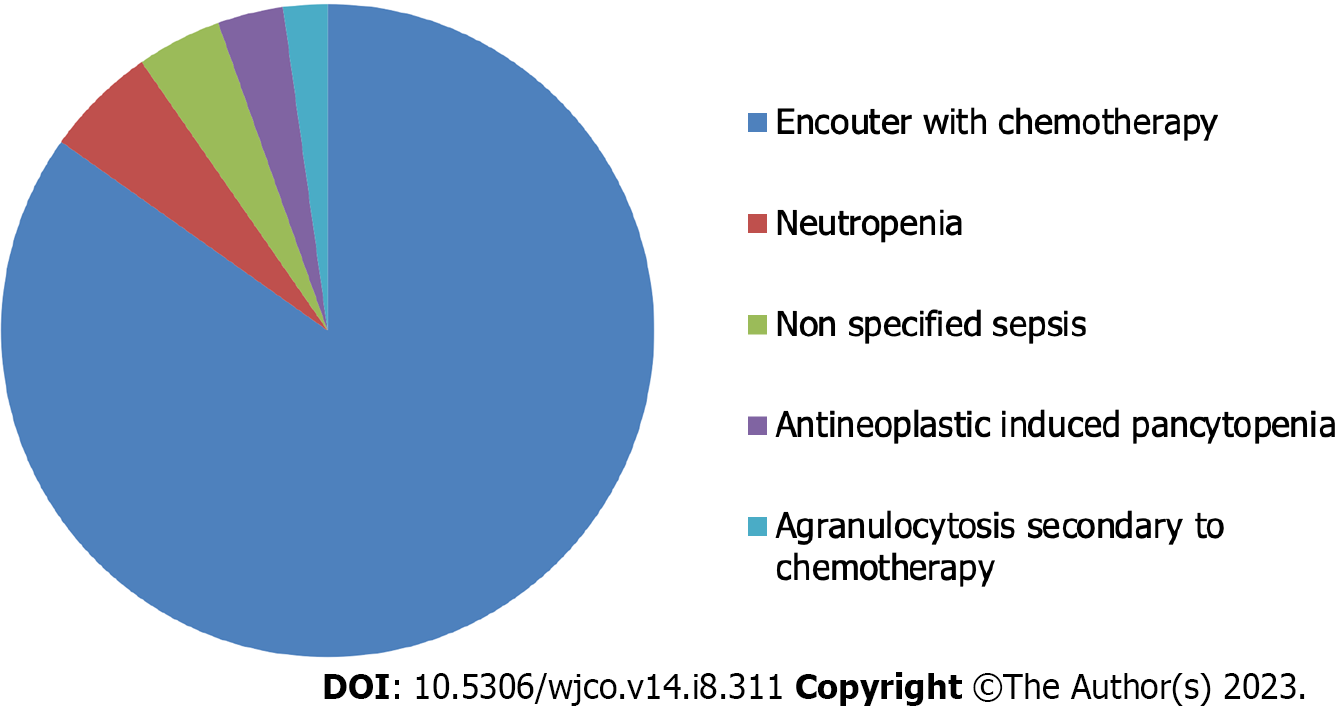
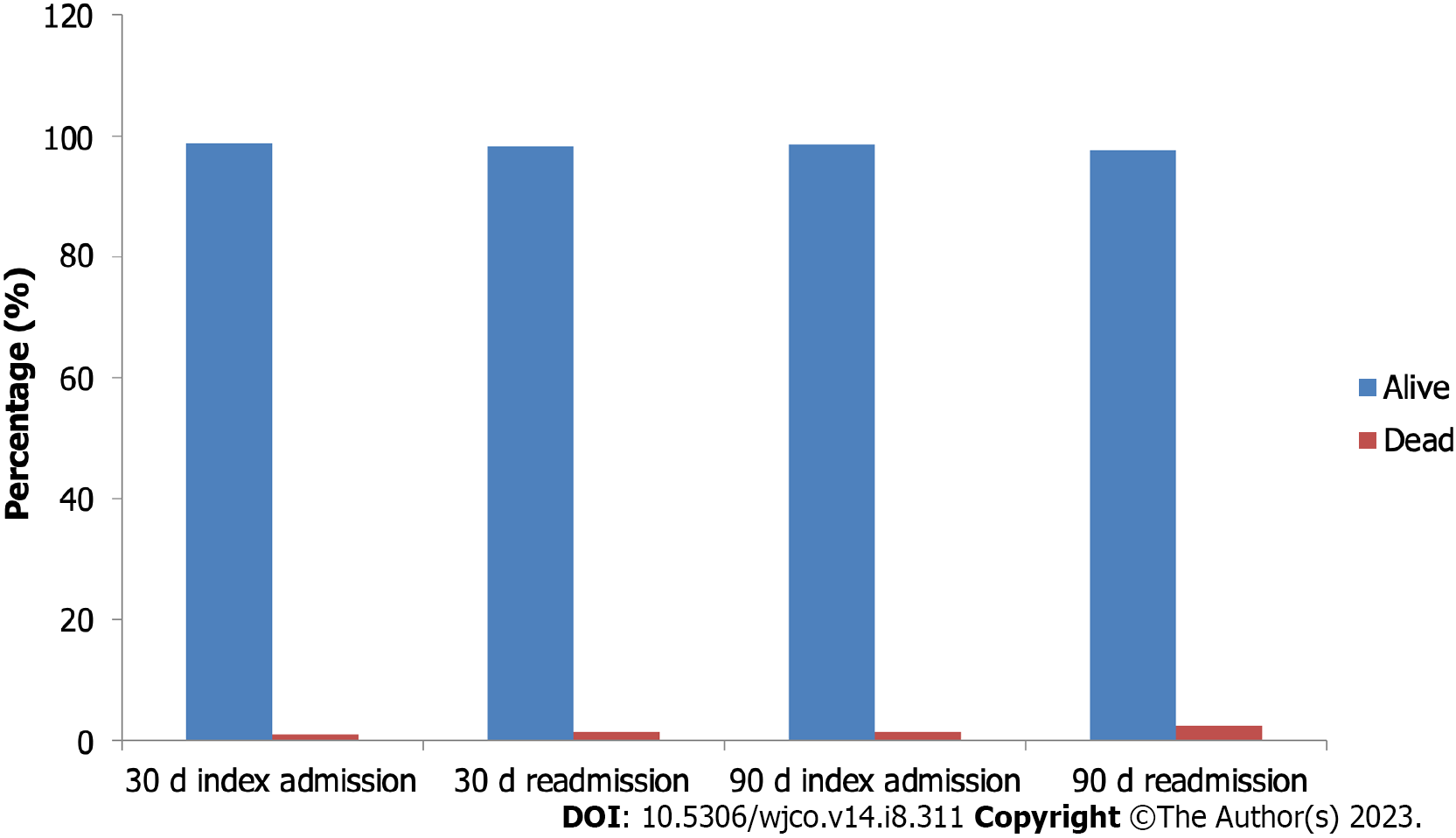
Common causes of readmission in both readmission cohorts included admissions for chemotherapy, neutropenia, non-specified sepsis, antineoplastic-induced pancytopenia, agranulocytosis secondary to chemotherapy, sepsis due to Escherichia coli, admissions for immunotherapy, acute myeloblastic leukemia, specified sepsis, and acute kidney failure. Figure 2 demonstrates the top causes of 30-day readmission during the COVID-19 pandemic. Mortality was higher among readmitted patients in both readmission cohorts. Figure 3 compares the mortality in index hospitalizations and 30DRCs and 90DRCs, respectively.
In both cohorts, readmissions had a shorter average LOS compared to index hospitalizations. The average LOS for readmitted patients was 5.60 d in the 30DRC, compared to 6.77 d for index cases (P < 0.001). In the 90DRC, the mean LOS for readmitted patients was 6.37 d, while index hospitalizations had a mean LOS of 7.51 d (P < 0.001). The total number of days lost due to hospitalization was higher in the 30DRC, totaling 184277 d compared to 156086 d in the 90-day cohort. The mean adjusted cost of hospitalization was higher in the 90-day cohort, with an average of 25646.4 dollars spent per index admission and 23477.0 dollars spent per readmission. In the 30DRC, the average cost per index admission was 22951.9 dollars, and 19220.8 dollars per readmission. The total cost incurred due to readmission across the country was 625 million dollars for the 30DRC and 568 million dollars for the 90DRC.
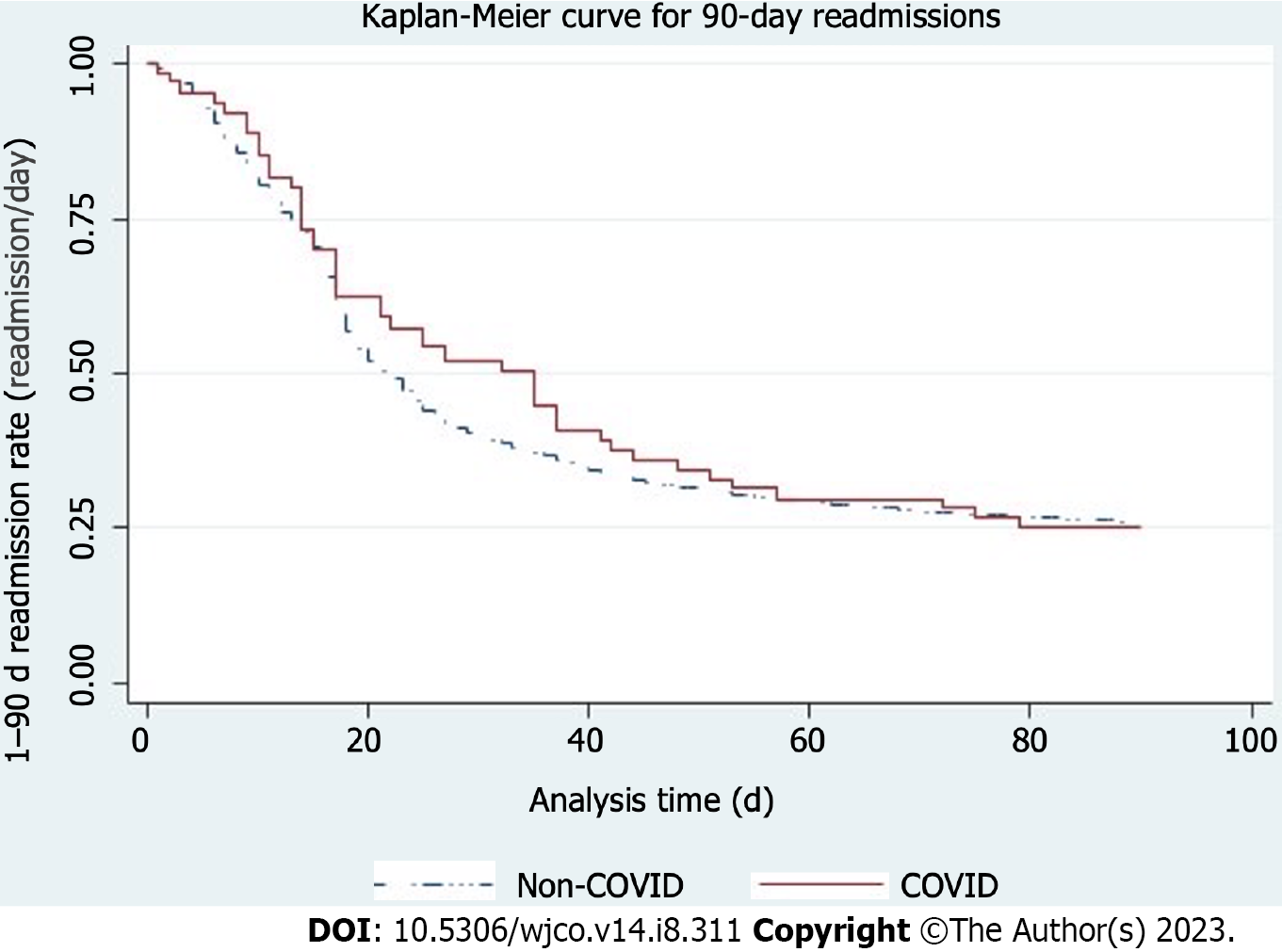
The results of the multivariable Cox regression analysis to identify independent predictors of 30-day and 90-day readmission are shown in Tables 5 and 6, respectively. Presence of comorbidities, including peripheral vascular disorder [Hazard ratio (HR) = 1.09, P = 0.048], paralysis (HR = 1.26, P < 0.001), human immunodeficiency virus/acquired immuno-deficiency syndrome (HIV/AIDS) (HR = 1.14, P = 0.03), and lymphoma (HR = 1.23, P < 0.001), were associated with an increased risk of readmission for IPCT within 30 d of discharge during the COVID-19 pandemic. Being in the middle age group (HR = 0.83, P < 0.001), elderly age groups (HR = 0.78, P < 0.001), discharge against medical advice (HR = 0.69, P = 0.031), renal failure (HR = 0.89, P = 0.004), liver disease (HR = 0.9, P = 0.02), and coagulopathy (HR = 0.91, P = 0.002) were associated with a decreased risk of readmission within 30 d of discharge. Figure 4 shows a Kaplan-Meier readmission curve for 30-day readmissions by COVID-19 status, with a P-value < 0.01.
| Variables | Hazard ratio | Confidence interval | P value |
| Age category | |||
| 45-64 years | 0.83 | 0.79-0.87 | < 0.001 |
| 65 years and above | 0.78 | 0.72-0.85 | < 0.001 |
| Discharge AMA | 0.69 | 0.49-0.97 | 0.031 |
| Payer type | |||
| Medicaid | 1.04 | 0.97-1.12 | 0.299 |
| Private insurance | 1.02 | 0.99-1.09 | 0.564 |
| Self pay | 1.05 | 0.90-1.23 | 0.522 |
| Median household income | |||
| 25th-50th quantile | 1.04 | 0.97-1.12 | 0.137 |
| 50th-75th quantile | 1.04 | 0.96-1.09 | 0.103 |
| > 75th quantile | 1.03 | 0.90-1.09 | 0.263 |
| COVID-19 | 0.91 | 0.68-1.22 | 0.543 |
| Comorbidities | |||
| Congestive heart failure | 0.92 | 0.85-1.00 | 0.059 |
| Cardiac arrhythmias | 0.96 | 0.91-1.01 | 0.147 |
| Peripheral vascular disorders | 1.09 | 1.00-1.19 | 0.048 |
| Hypertension, uncomplicated | 1.03 | 0.99-1.07 | 0.111 |
| Paralysis | 1.26 | 1.08-1.47 | 0.003 |
| Chronic pulmonary disease | 0.96 | 0.91-1.02 | 0.233 |
| Diabetics, uncomplicated | 0.94 | 0.89-1.00 | 0.058 |
| Renal failure | 0.89 | 0.82-0.96 | 0.004 |
| Liver disease | 0.9 | 0.82-0.98 | 0.023 |
| HIV/AIDS | 1.14 | 1.01-1.30 | 0.038 |
| Lymphoma | 1.23 | 1.17-1.28 | < 0.001 |
| Coagulopathy | 0.91 | 0.86-0.97 | 0.002 |
| Weight loss | 0.97 | 0.92-1.04 | 0.457 |
| Hypertension, complicated | 1.05 | 0.96-1.15 | 0.28 |
| Variables | Hazard ratio | Confidence interval | P value |
| Age category | |||
| 45-64 yr | 0.84 | 0.80-0.89 | < 0.001 |
| 65 yr and above | 0.74 | 0.68-0.80 | < 0.001 |
| Discharge AMA | 0.65 | 0.47-0.90 | 0.01 |
| Payer type | |||
| Medicaid | 1.02 | 0.95-1.09 | 0.633 |
| Private insurance | 1.02 | 0.95-1.08 | 0.631 |
| Self pay | 1.15 | 0.99-1.33 | 0.056 |
| Median household income | |||
| 25th-50th quintile | 1.03 | 0.97-1.09 | 0.329 |
| 50th-75th quintile | 1.04 | 0.98-1.11 | 0.166 |
| > 75th quintile | 1.03 | 0.96-1.10 | 0.471 |
| COVID-19 | 0.88 | 0.66-1.18 | 0.396 |
| Comorbidities | |||
| Congestive heart failure | 0.93 | 0.85-1.01 | 0.086 |
| Cardiac arrhythmias | 0.97 | 0.92-1.02 | 0.198 |
| Peripheral vascular disorders | 1.15 | 1.04-1.26 | 0.004 |
| Hypertension, uncomplicated | 1.02 | 0.98-1.07 | 0.296 |
| Paralysis | 1.21 | 1.02-1.43 | 0.027 |
| Chronic pulmonary disease | 0.97 | 0.92-1.03 | 0.386 |
| Diabetics, uncomplicated | 0.92 | 0.87-0.99 | 0.01 |
| Renal failure | 0.91 | 0.83-0.99 | 0.046 |
| Liver disease | 0.89 | 0.82-0.98 | 0.017 |
| HIV/AIDS | 1.1 | 0.94-1.29 | 0.211 |
| Lymphoma | 1.14 | 1.09-1.20 | < 0.001 |
| Coagulopathy | 0.95 | 0.90-1.00 | 0.093 |
| Weight loss | 0.93 | 0.88-0.99 | 0.019 |
| Hypertension, complicated | 1.03 | 0.93-1.14 | 0.604 |
A similar profile of comorbidities increased the risk of 90-day readmission as observed in the 30DRC, except for HIV/AIDS (HR = 1.1, P = 0.211). Other variables analyzed for the risk of 90-day readmission followed the same trend as the 30DRC, except for coagulopathy (HR = 0.95, P = 0.093).
Our study provides a comprehensive nationwide view of the care received by patients undergoing IPCT during the COVID-19 pandemic. To the best of our knowledge, this is the first study that specifically focused on and analyzed factors related to hospitalization for patients receiving IPCT during the pandemic. We observed a 30-day readmission rate of 58.9% and a 90-day readmission rate of 73.93%, both of which are significantly higher than rates reported in previous similar studies[18,19]. This increase can be attributed to the strain imposed on the healthcare system by the pandemic. Similar findings were reported by Loo et al[20] and Matthews et al[21], who also observed an increase in readmission rates during the COVID-19 pandemic. The demographics of our patients were comparable and consistent with those reported in studies conducted before the pandemic[11,22].
Several studies conducted during the pandemic have reported higher costs of hospitalization, and our study aligns with these findings[23,24]. With an average cost of re-hospitalization of 22952.0 dollars observed in our study, the cost was significantly higher than the average cost of 17035 dollars reported in similar hospitalizations before the pandemic[25]. However, contrary to the findings of higher readmission costs compared to index admissions reported by Kwei-Nsoro et al[9], our study revealed a higher cost of index admission.
The ECI scores were higher among readmitted hospitalizations compared to index hospitalizations due to the higher comorbidity burden among readmitted patients. Higher ECI scores are associated with higher mortality[26,27], which was also observed in our study, consistent with previous studies[28,29].
The most common cause of readmission was admission for chemotherapy. The Kaplan-Meier curve (Figure 4) demonstrated a shorter time to 50% readmission in the non-COVID-19 group (20 d) compared to the COVID-19 group (36 d). This could be explained by the fact that COVID-19 positivity delayed the admission for chemotherapy, which was the most common cause of readmissions. Other causes of readmissions included neutropenia, sepsis, and acute kidney injury, in line with previous studies[13,30].
We observed a significant number of patients undergoing IPCT being managed in medium-sized metropolitan teaching hospitals. However, we did not observe any significant difference in the type of treatment center between index hospitalizations and readmissions. Middle-aged and elderly patients had a decreased risk of readmission, likely due to the higher prevalence of comorbidities in these age groups. Our results showed that comorbidities were associated with an increased risk of readmission, consistent with findings in other studies[31,32].
Previous studies have indicated that discharge against medical advice increases the risk of readmission, but our results were contrary to this[16,32]. This could be explained by the possibility that patients who left the hospital against medical advice had limited access to the healthcare system, which was heavily impacted by the pandemic[8,33]. However, further research is needed to explore this area. We found weight loss to be an independent predictor of 90-day readmission, which is consistent with a survey of approximately 10000 general medicine discharges where weight loss was identified as a significant predictor of 30-day readmissions, aligning with our findings in the 90DRC[33]. However, we did not find weight loss to be an independent predictor of 30-day readmission, and the reason for this remains unclear. Additionally, contrary to our expectations and findings in similar studies[21,34], COVID-19 was not identified as an independent predictor of readmission. This could be due to the smaller percentage of COVID-19-infected patients in our study population or could be an area for further investigation.
Finally, we acknowledge some limitations in our study. The readmission rates may vary across different states, but the NRD does not provide state-specific data, preventing us from drawing conclusions at the state level. Our study excluded elective hospitalizations in December, potentially leading to a missed number of readmissions during that month.
The COVID-19 pandemic has significantly impacted the management of patients receiving IPCT. There is a need for a more strategic approach in the care of patients undergoing IPCT during pandemics.
The coronavirus disease 2019 (COVID-19) pandemic has had a profound impact on healthcare services and has resulted in modifications to the management of various diseases.
The treatment of cancer has undergone significant changes during the COVID-19 pandemic. Understanding the effects of these changes can provide valuable insights to better prepare for future pandemics.
This study aims to provide insights into the outcomes of hospitalization for in hospital chemotherapy during the COVID-19 pandemic.
We conducted a retrospective review of a Nationwide Readmission Database for patients undergoing inpatient chemotherapy (IPCT) during the COVID-19 pandemic. We analyzed data on readmission rates, causes of readmission, and predictors of readmission.
We found a 90-day readmission rate of 59.8% and a 30-day readmission rate of 73.93%. The most common cause of readmission was chemotherapy encounters (66.7%). Predictors of readmission included peripheral vascular disorders [Hazard ratio (HR) = 1.09, P = 0.04] and paralysis (HR = 1.26, P < 0.001). The total cost incurred due to readmission during the pandemic was 1193000000.00 dollars.
The COVID-19 pandemic has had a significant impact on the management of cancer patients. There is a need for a more strategic approach to the care of patients undergoing IPCT during pandemics.
This study opens the door for further investigation into the effects of pandemics on disease management.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Haddadi S, Algeria; Wang LH, China S-Editor: Lin C L-Editor: A P-Editor: Zhang XD
| 1. | World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Mar 11, 2020. [cited Feb 23, 2023]. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. |
| 2. | Umakanthan S, Sahu P, Ranade AV, Bukelo MM, Rao JS, Abrahao-Machado LF, Dahal S, Kumar H, Kv D. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad Med J. 2020;96:753-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 207] [Reference Citation Analysis (0)] |
| 3. | World Health Organization; WHO Coronavirus (COVID-19) Dashboard. Feb 23, 2022. [cited Feb 25, 2022]. Available from: https://covid19.who.int. |
| 4. | Sharma A, Ahmad Farouk I, Lal SK. COVID-19: A Review on the Novel Coronavirus Disease Evolution, Transmission, Detection, Control and Prevention. Viruses. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 245] [Cited by in RCA: 324] [Article Influence: 81.0] [Reference Citation Analysis (0)] |
| 5. | da Silva SJR, do Nascimento JCF, Germano Mendes RP, Guarines KM, Targino Alves da Silva C, da Silva PG, de Magalhães JJF, Vigar JRJ, Silva-Júnior A, Kohl A, Pardee K, Pena L. Two Years into the COVID-19 Pandemic: Lessons Learned. ACS Infect Dis. 2022;8:1758-1814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 53] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 6. | Haleem A, Javaid M, Vaishya R. Effects of COVID-19 pandemic in daily life. Curr Med Res Pract. 2020;10:78-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 323] [Cited by in RCA: 318] [Article Influence: 63.6] [Reference Citation Analysis (0)] |
| 7. | Kirchberg TN, Costantini TW, Santorelli J, Doucet JJ, Godat LN. Predictors of Readmission Following Treatment for Traumatic Hemothorax. J Surg Res. 2022;277:365-371. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Global Health Research Group on Children’s Non-Communicable Diseases Collaborative. Impact of the COVID-19 pandemic on patients with paediatric cancer in low-income, middle-income and high-income countries: a multicentre, international, observational cohort study. BMJ Open. 2022;12:e054690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Kwei-Nsoro R, Ojemolon P, Laswi H, Ebhohon E, Shaka A, Mir WA, Siddiqui AH, Philipose J, Shaka H. Rates, Reasons, and Independent Predictors of Readmissions in Portal Venous Thrombosis Hospitalizations in the USA. Gastroenterology Res. 2022;15:253-262. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306:1794-1795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 353] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 11. | Wang S, Zhu X. Nationwide hospital admission data statistics and disease-specific 30-day readmission prediction. Health Inf Sci Syst. 2022;10:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Brooks GA, Li L, Sharma DB, Weeks JC, Hassett MJ, Yabroff KR, Schrag D. Regional variation in spending and survival for older adults with advanced cancer. J Natl Cancer Inst. 2013;105:634-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 13. | Bell JF, Whitney RL, Reed SC, Poghosyan H, Lash RS, Kim KK, Davis A, Bold RJ, Joseph JG. Systematic Review of Hospital Readmissions Among Patients With Cancer in the United States. Oncol Nurs Forum. 2017;44:176-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 14. | Tennison JM, Rianon NJ, Manzano JG, Munsell MF, George MC, Bruera E. Thirty-day hospital readmission rate, reasons, and risk factors after acute inpatient cancer rehabilitation. Cancer Med. 2021;10:6199-6206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 15. | Agency for Healthcare Research and Quality. HCUP Nationwide Readmission Database (NRD). 2018. Healthcare Cost and Utilization Project (HCUP). [cited 3 August 2022]. Available from: https://www.hcup-us.ahrq.gov/nrdoverview.jsp.. |
| 16. | Khan MS, Sreenivasan J, Lateef N, Abougergi MS, Greene SJ, Ahmad T, Anker SD, Fonarow GC, Butler J. Trends in 30- and 90-Day Readmission Rates for Heart Failure. Circ Heart Fail. 2021;14:e008335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 164] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 17. | Agency for Healthcare Research and Quality. Methodological Issues when Studying Readmissions and Revisits Using Hospital Administrative Data. 2011. HCUP Methods Series Report # 2011-01. Mar 9, 2011. [cited 3 August 2022]. Available from: http://www.hcupus.ahrq.gov/reports/methods/methods.jsp. |
| 18. | Shivani Handa, MBBS, Kamesh Gupta, Jasdeep Singh Sidhu, Giulia Petrone, MD MBBS, Sridevi Rajeeve, MD, Karan Jatwani. Etiologies and Predictors of 30-Day Readmission in Patients Undergoing Induction Chemotherapy for Acute Myeloid Leukemia. Blood. 2019;134 Suppl 1:4759. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Martin AS, Abbott DE, Hanseman D, Sussman JE, Kenkel A, Greiwe P, Saeed N, Ahmad SH, Sussman JJ, Ahmad SA. Factors Associated with Readmission After Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy for Peritoneal Carcinomatosis. Ann Surg Oncol. 2016;23:1941-1947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Loo WK, Hasikin K, Suhaimi A, Yee PL, Teo K, Xia K, Qian P, Jiang Y, Zhang Y, Dhanalakshmi S, Azizan MM, Lai KW. Systematic Review on COVID-19 Readmission and Risk Factors: Future of Machine Learning in COVID-19 Readmission Studies. Front Public Health. 2022;10:898254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Matthews A, Kramer RA, Peterson CM, Mitan L. Higher admission and rapid readmission rates among medically hospitalized youth with anorexia nervosa/atypical anorexia nervosa during COVID-19. Eat Behavh. 2021;43:101573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 22. | Shen Y, Tang S, Xu J, Xie X, Chen Z. Modified Intraperitoneal Chemotherapy Without Bevacizumab as a First-Line Therapy for Newly Diagnosed Advanced Epithelial Ovarian Cancer-Two Centers Experiences. Front Med (Lausanne). 2022;9:846352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 23. | Graves JA, Baig K, Buntin M. The Financial Effects and Consequences of COVID-19: A Gathering Storm. JAMA. 2021;326:1909-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 24. | Iwashyna TJ, Kamphuis LA, Gundel SJ, Hope AA, Jolley S, Admon AJ, Caldwell E, Monahan ML, Hauschildt K, Thompson BT, Hough CL; NHLBI Prevention and Early Treatment of Acute Lung Injury (PETAL) Network. Continuing Cardiopulmonary Symptoms, Disability, and Financial Toxicity 1 Month After Hospitalization for Third-Wave COVID-19: Early Results From a US Nationwide Cohort. J Hosp Med. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 25. | J I. PCN41 - Hospital Cancer BurdenIn Argentina: Costs, Mortality And Readmissions. Value Health. 2015;18:A196. [DOI] [Full Text] |
| 26. | Kumar A, Karmarkar A, Downer B, Vashist A, Adhikari D, Al Snih S, Ottenbacher K. Current Risk Adjustment and Comorbidity Index Underperformance in Predicting Post-Acute Utilization and Hospital Readmissions After Joint Replacements: Implications for Comprehensive Care for Joint Replacement Model. Arthritis Care Res (Hoboken). 2017;69:1668-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Menendez ME, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014;472:2878-2886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 413] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 28. | Shaw JA, Stiliannoudakis S, Qaiser R, Layman E, Sima A, Ali A. Thirty-Day Hospital Readmissions: A Predictor of Higher All-cause Mortality for Up to Two Years. Cureus. 2020;12:e9308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 29. | Krumholz HM, Lin Z, Keenan PS, Chen J, Ross JS, Drye EE, Bernheim SM, Wang Y, Bradley EH, Han LF, Normand SL. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309:587-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 287] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 30. | Jairam V, Lee V, Park HS, Thomas CR Jr, Melnick ER, Gross CP, Presley CJ, Adelson KB, Yu JB. Treatment-Related Complications of Systemic Therapy and Radiotherapy. JAMA Oncol. 2019;5:1028-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 31. | Chakrabarti B, Lane S, Jenks T, Higgins J, Kanwar E, Allen M, Wotton D. Predictors of 30-day readmission following hospitalisation with community-acquired pneumonia. BMJ Open Respir Res. 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Yong TY, Fok JS, Hakendorf P, Ben-Tovim D, Thompson CH, Li JY. Characteristics and outcomes of discharges against medical advice among hospitalised patients. Intern Med J. 2013;43:798-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 33. | Tessema GA, Kinfu Y, Dachew BA, Tesema AG, Assefa Y, Alene KA, Aregay AF, Ayalew MB, Bezabhe WM, Bali AG, Dadi AF, Duko B, Erku D, Gebrekidan K, Gebremariam KT, Gebremichael LG, Gebreyohannes EA, Gelaw YA, Gesesew HA, Kibret GD, Leshargie CT, Meazew MW, Mekonnen A, Mirkuzie AH, Mohammed H, Tekle DY, Tesfay FH. The COVID-19 pandemic and healthcare systems in Africa: a scoping review of preparedness, impact and response. BMJ Glob Health. 2021;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 150] [Cited by in RCA: 136] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 34. | Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, Jones M, Kitchener E, Fox M, Johansson M, Lang E, Duggan A, Scott L, Albarqouni L. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11:e045343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 748] [Cited by in RCA: 772] [Article Influence: 193.0] [Reference Citation Analysis (1)] |