Published online Nov 24, 2023. doi: 10.5306/wjco.v14.i11.471
Peer-review started: August 29, 2023
First decision: September 14, 2023
Revised: September 24, 2023
Accepted: October 13, 2023
Article in press: October 13, 2023
Published online: November 24, 2023
Processing time: 84 Days and 17.6 Hours
Flap reconstruction after resection of a superficial malignant soft tissue tumor extends the surgical field and is an indicator for potential recurrence sites.
To describe a grading system for surgical field extension of soft tissue sarcomas.
Grading system: CD-grading is a description system consisting of C and D values in the surgical field extension, which are related to the compartmental position of the flap beyond the nearby large joint and deeper extension for the pedicle, respectively. C1/D1 are positive values and C0/D0 are negative. With a known location, 1/0 values can be "p" (proximal), "d" (distal), and "b" (in the tumor bed), and the description method is as follows: flap type, CxDx [x = 0, 1, p, d or b].
Four representative patients with subcutaneous sarcomas who underwent reconstruction using fasciocutaneous flaps are presented. The cases involved a distal upper arm (elbow) synovial sarcoma reconstructed using a pedicled latissimus dorsi (pedicled flap: CpDp); a distal upper arm (elbow) pleomorphic rhabdomyosarcoma reconstructed using a transpositional flap from the forearm (transpositional flap: CdD0); an undifferentiated pleomorphic sarcoma in the buttocks reconstructed using a transpositional flap (transpositional flap: C0D0); and a myxofibrosarcoma in the buttocks reconstructed using a propeller flap from the thigh (pedicled flap: CdDd).
The reconstruction method is chosen by the surgeon based on size, location, and other tumor characteristics; however, the final surgical field cannot be determined based on preoperative images alone. CD-grading is a description system consisting of C and D values in the surgical field extension that are related to the compartmental position of the flap beyond the nearby large joint and deeper extension for the pedicle, respectively. The CD-grading system gives a new perspective to the flap reconstruction classification. The CD-grading system also provides important information for follow-up imaging of a possible recurrence.
Core Tip: Flap reconstruction after resection of a superficial malignant soft tissue tumor extends the surgical field and is an indicator for potential recurrence sites. CD-grading is a description system consisting of C and D values in the surgical field extension that are related to the compartmental position of the flap beyond the nearby large joint and deeper extension for the pedicle, respectively. C1/D1 and C0/D0 are positive and negative values, respectively. The CD-grading system gives a new perspective to flap reconstruction classification. The CD-grading system also provides important information for follow-up imaging of a possible recurrence.
- Citation: Sakamoto A, Noguchi T, Matsuda S. System describing surgical field extension associated with flap reconstruction after resection of a superficial malignant soft tissue tumor. World J Clin Oncol 2023; 14(11): 471-478
- URL: https://www.wjgnet.com/2218-4333/full/v14/i11/471.htm
- DOI: https://dx.doi.org/10.5306/wjco.v14.i11.471
Soft tissue sarcomas comprise a group of rare heterogeneous neoplasms that account for < 1% of all cancers[1]. Soft tissue sarcomas can occur in any soft tissue, but are most common in the extremities. Wide resection of the sarcoma and the surrounding normal tissue is necessary to reduce the recurrence rate[2]. Flap reconstruction is used to repair soft tissue defects after resection of a soft tissue sarcoma, especially a superficial soft tissue sarcoma[3,4].
The term “tumor bed” refers to the area of tissue remaining after a malignant tumor is removed. The tumor bed includes the tumor and surrounding healthy tissues where cancer cells may exist[5]. Use of a reconstruction flap following soft tissue sarcoma resection can extend the surgical field or tumor bed because of flap elevation or dissection of recipient vessels.
The current Cancer Staging Manual of the American Joint Committee on Cancer (AJCC) of soft tissue sarcoma is widely used based upon tumor size, histologic grade, and the presence of metastasis[6]. AJCC supports the R classification, which categorizes surgical margins as negative (R0), microscopically positive (R1), or grossly positive (R2)[7,8]. Flaps can be classified based on several factors (pedicled, free, or the tissue type from which the flap is made). Classification of flaps according to clinical complications has also been reported[9]; however, there is no system describing surgical field extension related to flap reconstruction.
In the current report we propose a grading classification, the CD-grading system, to describe extension of the surgical field related to flap reconstruction after superficial soft tissue sarcoma resection. Representative cases are also presented.
The new grading system (CD-grading system) was used herein for superficial soft tissue sarcomas with extremity resection reconstructed by fascio-(musculo)-cutaneous flaps. Upper extremity tumors are defined as lesions arising distal to the acromioclavicular joint and include tumors of the shoulder girdle and axilla. Lower extremity tumors are defined as lesions arising distal to the iliac crest, including tumors of the gluteal region[9]. Additional skin grafting does not affect the grade; the skin grafting cases were not excluded.
The CD-grading system consists of C- and D-values. The C-value indicates the "compartmental position of the flap beyond the nearby large joint " and when the flap crosses a nearby large joint, the C-value is positive (C1). When the flap is within the compartment, the C-value is negative (C0). Large joints include the shoulders, elbows, wrists, hips, knees, and ankles. If the location of a flap crossing the joint location is proximal, the C-value is Cp (p = proximal) and when crossing a distal large joint the C-value is Cd (d = distal).
D-value means “deeper extension for the pedicle.” The pedicle is already exposed, and the negative D-value is D0. If dissection of the pedicle is necessary, the positive D-value is D1. When the dissected pedicle is located proximal to the surgical field, the D-value is Dp (p = proximal), when the dissected pedicle is located distally, the D-value is Dd (d = distal), and when the pedicle dissection is within the surgical bed, the D-value is Db (b = surgical bed; Tables 1 and 2).
| C-value | Description | |
| Within the compartment | 0 | C0 |
| Extra compartment | 1: any | C1 |
| p: proximal | Cp | |
| d: distal | Cd |
| Pedicle | D-value | Description |
| Already exposed | 0 | D0 |
| Dissection of the pedicle | 1: Any | D1 |
| p: Proximal | Dp | |
| d: Distal | Dd | |
| b: Within tumor bed | Db |
The flap type is described before the CD-values as “flap type, CxDx,” in which x can be 0, 1, p, d, or b. There is no strict rule in the description of the flap type; however, an easy and understandable description, such as distinguishing between a local or free flap, would be required.
In cases involving transpositional fasciocutaneous or propeller flaps[10], the flap is located within the compartment, the C-value is C0, the D-value is D0, and the CD-grade is C0D0. When the flap is from the extra compartment across the large joint, the C-value is C1, the D-value is D0, and the CD-grade is C1D0. When the flap is obtained proximally and crosses a large joint, the CD-grade is CpD0, and when the flap is derived distally and crosses a large joint, the CD-grade is CdD0 (Tables 3 and 4).
| CD-grade | Transpositional flap | Pedicled flap | Free flap |
| C0D0 | C0D0 | Not applied | C0D0 |
| C0D1 | NA | C0Dp, C0Dd | C0Dp, C0Dd, C0Db |
| C1D0 | CpD0, CdD0 | NA | NA |
| C1D1 | NA | CpDp, CdDd | NA |
| Flap location | C-value | D-value | CD-grade |
| Within the compartment | 0 | 0 | C0D0 |
| Extra compartment: from any | 1 | 0 | C1D0 |
| From proximal | p | 0 | CpD0 |
| From distal | d | 0 | CdD0 |
The C-value in the pedicle flap is the same as the transpositional flap. The flap is located within the compartment and the C-value is C0. When the flap comes from the extra compartment across the joint, the C-value is C1. C1 can be Cp or Cd depending on the flap location (proximal or distal). The D-value reflects the location of the pedicle. The pedicle flap needs extension of the surgical field to deeper tissues, therefore the D-value is always D1. When the pedicle is located proximal to the surgical field, D1 can be Dp (p = proximal), and when the pedicle is located distal to the surgical field, the D1 can be Dd (d = distal; Tables 3 and 5).
| Flap location | C-value | D-value (pedicle location) | CD-grade |
| Within the compartment | 0 | 1 (any) | C0D1 |
| From proximal | 0 | p (proximal) | C0Dp |
| From distal | 0 | d (distal) | C0Dd |
| Extra compartment | 1 | 1 (any) | C1D1 |
| From proximal | p | p (proximal) | CpDp |
| From distal | d | d (distal) | CdDd |
The donated area of the flap does not affect the surgical field in terms of tumor contamination, and the C-value in the free flap is always C0. When the pedicle is already exposed at the surgical field, the D-value is D0. When the pedicle is not exposed, and the pedicle needs to be exposed, then the D-value is D1. When the pedicle is located proximal to the surgical field, D1 can be Dp (p = proximal), and when the pedicle is located distal to the surgical field, the D1 can be Dd (d = distal). When the pedicle is exposed at the deeper tissues within the surgical field, the D-value is Db (Tables 3 and 6).
| Pedicle location | C-value | D-value (pedicle location) | CD-grade |
| Already exposed | 0 | 0 | C0D0 |
| Necessary for dissection | 0 | 1 (any) | C0D1 |
| From proximal | 0 | p (proximal) | C0Dp |
| From distal | 0 | d (distal) | C0Dd |
| Within tumor bed | 0 | b (within tumor bed) | C0Db |
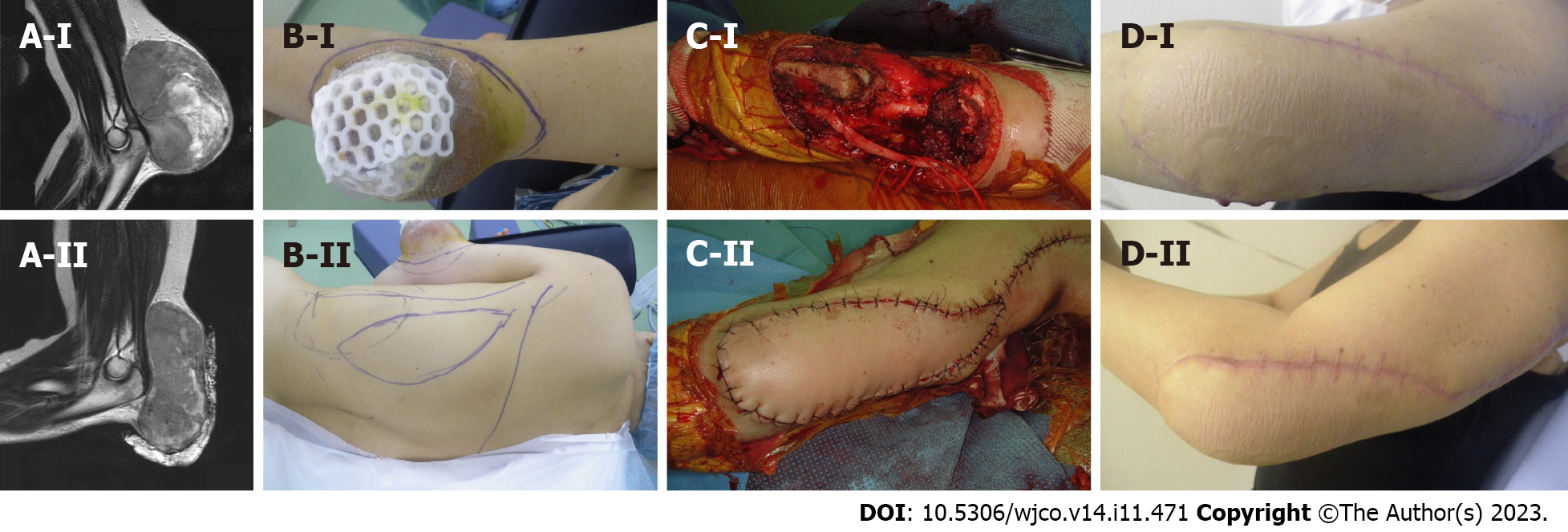
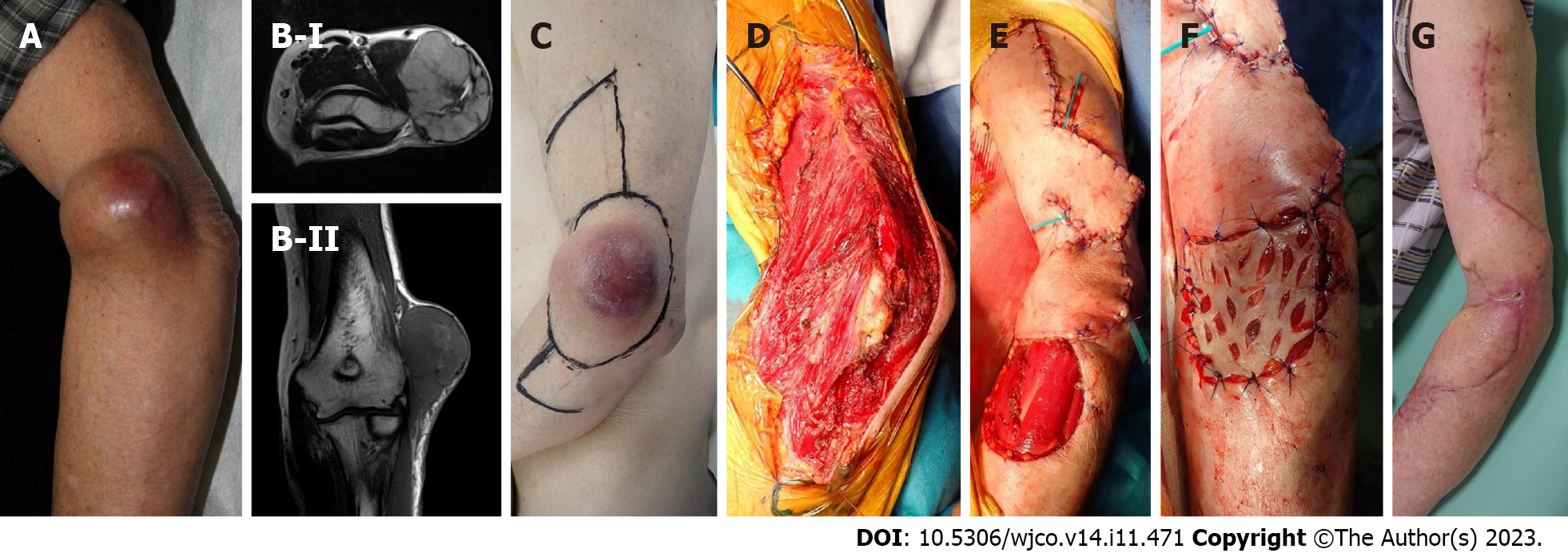
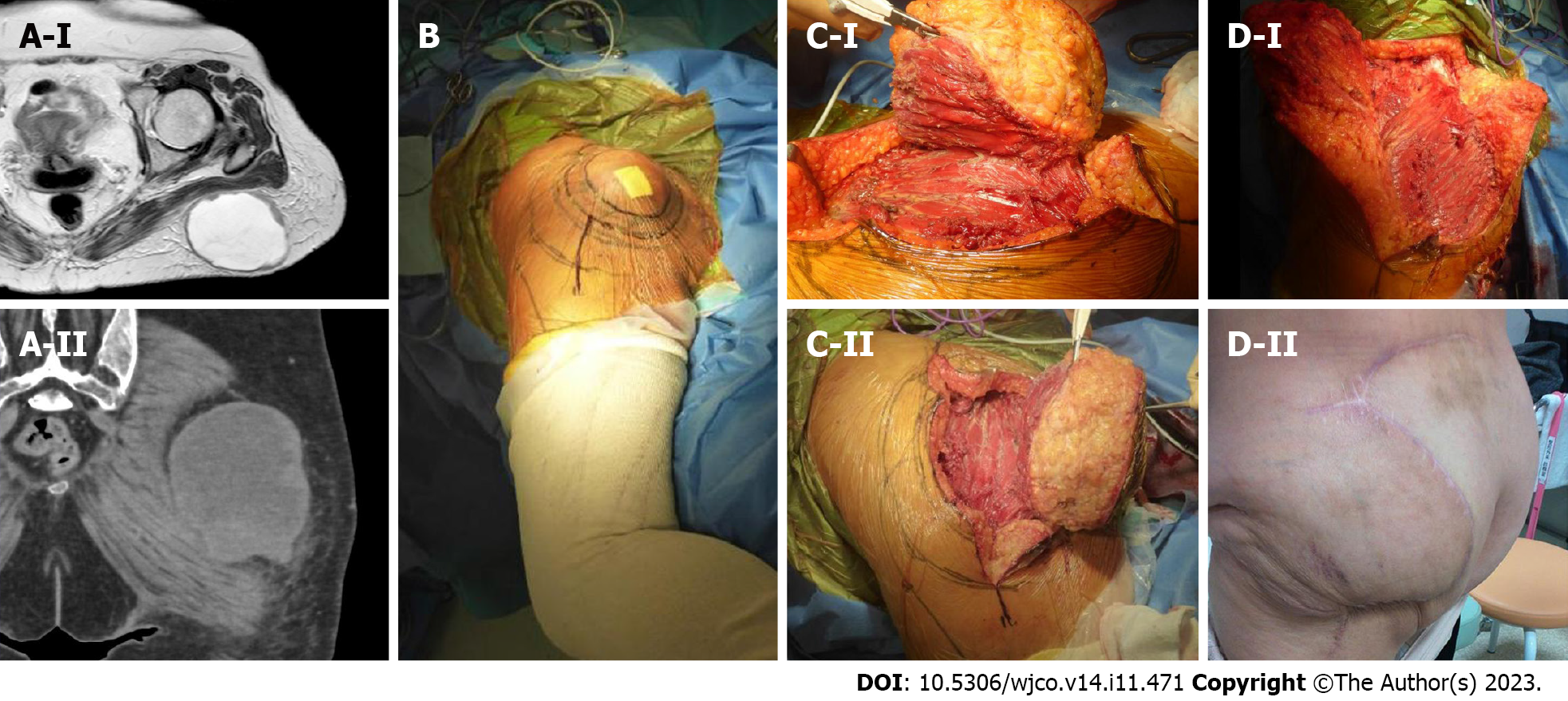
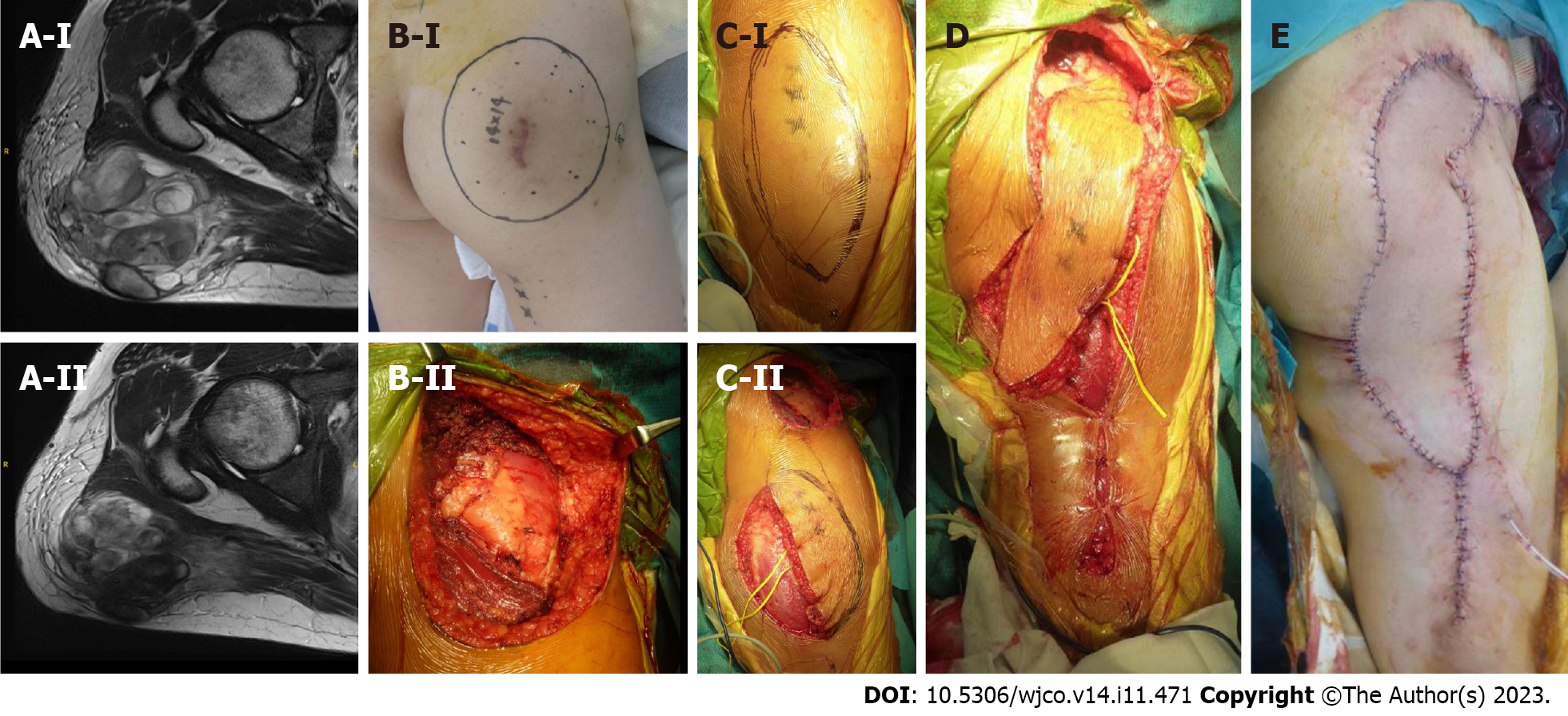
Herein we present four cases of superficial soft tissue sarcomas. Two elbow soft tissue sarcomas and two buttock soft-tissue sarcomas are presented. One elbow soft tissue sarcoma patient was a 47-year-old female with a synovial sarcoma at the elbow (distal upper arm) reconstructed with a pedicled latissimus dorsi; the CD-grade was CpDp (pedicled flap, CpDp; Figure 1). The second elbow soft tissue sarcoma patient was an 85-year-old male with a pleomorphic rhabdomyosarcoma at the elbow (distal upper arm) reconstructed using a transpositional flap from the forearm; the CD-grade was CdD0 (transpositional flap, CdD0; Figure 2). The first patient with a buttock soft tissue sarcoma was a 65-year-old female with an undifferentiated pleomorphic sarcoma at the buttock reconstructed using a transpositional flap; the CD-grade was C0D0 (transpositional flap, C0D0[11]; Figure 3). The second patient with a buttock sarcoma was a 46-year-old male with a myxofibrosarcoma that was reconstructed using a propeller flap from the thigh; the CD-grade was CdDd (pedicled flap, CdDd; Figure 4).
Soft tissue sarcomas require wide resection with healthy tissue margins[12,13]. Thus, the surgical field is wider than the tumor size. The extension of the tumor bed has the possibility of tumor contamination. Therefore, recognition of tumor bed extension is necessary. Discrepancies between the preoperative tumor burden and postoperative tumor bed contour have been identified after tumor burden replacement with a latissimus dorsi flap[14]. Flap reconstruction increases the surgical field during superficial soft tissue sarcoma resection[15].
A flap is applied to the defect after resection of a soft tissue sarcoma, especially a superficial soft tissue sarcoma. The choice of flap is often determined by the surgeon's preference, as well as the location of the tumor. The tumor bed after resection of soft tissue sarcomas cannot be predicted solely based on preoperative imaging. If amputation is necessary in the case of a re-occurrence, the level of amputation is important. Extension of the tumor bed due to flap reconstruction carries the risk of tumor contamination and may require more proximal amputation. The C-value gives information that indicates the likelihood of tumor contamination across the greater joint.
There is a risk of tumor contamination if deep tissues are created in the surgical field. The D-value represents the location of the pedicle. Dissection of the pedicle and recipient vessels requires dissection to the deeper layers, resulting in extension of the surgical field, with a D-value of D1. Transposition flaps in the compartment do not require exposure of the donor vessels, therefore less deep tissue exposure is advantageous in terms of reducing the potential for tumor recurrence, with a D-value of D0. Similarly, even in cases of a free flap requiring microsurgery, if the recipient vessels are already exposed, the D-value is D0 because deeper tissue dissection is not necessary.
The AJCC Staging of Soft Tissue Sarcomas (eighth edition) is based upon the tumor size, histologic grade, and the presence of metastasis. Tumor size is classified into four categories with border values of 5, 10, and 15 cm. The notation regarding tumor depth (superficial or deep from the superficial fascia) has been eliminated from the seventh edition of the AJCC Staging of Soft Tissue Sarcomas[6]. The surgical staging of musculoskeletal sarcomas has 4 types of surgical margins [intralesional, marginal, wide, and radical (compartmental)], as proposed by Enneking et al[16]. A 2-3 cm surgical margin provides reasonable local control of soft tissue sarcomas[17]. The AJCC supports the R classification, which categorizes margins as negative (R0), microscopically positive (R1), or grossly positive (R2)[7,8]. Furthermore, the Union Against Cancer (UICC) proposed a R + 1 mm classification that requires 1 mm of healthy tissue between the tumor and margin to define a negative margin (R0)[18,19], thus resulting in more resections being considered microscopically positive (R1). Radiation therapy can be performed as adjuvant therapy, especially if cancer cells remain after the resection. Radiation has a role in reducing the risk of recurrence in soft tissue sarcoma resection[5]. The term, tumor bed, refers to the area of tissue remaining after a malignant tumor is removed. The tumor bed may have cancer cells[5]. Recognition of tumor bed extension is necessary for postoperative radiation. Without flap reconstruction following soft tissue sarcoma resection, the tumor bed can largely be predicted with the preoperative staging based upon the images and the histologic findings. With flap reconstruction, tumor bed prediction is difficult without the surgical method information. Indeed, the new grading system can give information of surgical field extension associated with flap reconstruction.
There are several limitations in the new grading system. First, this classification is completely new and still theoretical. Clinical use of the assembled clinical data would be necessary, and some modification may be required for improvement. Second, the new grading system was used for superficial soft tissue sarcomas resected in the extremities and fascio-(musculo)-cutaneous flaps, in which hands and feet were not included. The new grading system might be modified for any part of bones and soft tissue sarcomas. Third, flap type description is not strictly defined in the new grading system, which may result in ambiguity; however, according to the flap technique improvement, description of the flap would be diverse. Therefore, no flap description restrictions were used in the new grading system. Finally, the new grading system cannot describe the length or area required for postoperative radiation. Excessive information in the grading system, however, would make the new grading system difficult for clinical use.
We have proposed a method to describe extension of the surgical field in reconstruction after superficial soft tissue sarcoma resection. The method described can give values for tumor bed extension after flap reconstruction. The description of whether or not the operative field has been extended due to reconstruction is considered to be important information for image evaluation of recurrence.
Flap reconstruction can extend the surgical field or tumor bed because of flap elevation or dissection of recipient vessels during resection of superficial soft tissue sarcomas. There is currently no method describing extension of the surgical field.
Extension of the surgical field cannot be predicted based on preoperative images for flap reconstruction after superficial soft tissue sarcoma resection. Knowledge of the surgical field extension is important information for evaluation of recurrence images or possible postoperative radiation.
A theoretical CD-grading system was developed consisting of C and D values in the surgical field extension. The C-value represents the flap beyond the nearby large joint and the D-value pertains to a deeper extension.
C1/D1 and C0/D0 are positive and negative values, respectively. With a known location, C values are "p" (proximal), "d" (distal), and "b" (in the tumor bed). The description method is as follows: flap type, CxDx [x = 0, 1, p, d or b].
Classification and possible values are shown in the tables (transpositional fascial flap/propeller, pedicled, and free flaps). Four representative patients with subcutaneous sarcomas who underwent reconstruction using fasciocutaneous flaps are presented.
The new grading system can give values for tumor bed extension after flap reconstruction following superficial soft tissue sarcoma resection. The description of whether or not the operative field has been extended due to reconstruction is thought to be important information for evaluation of recurrence images.
Clinical use of assembled clinical data would be necessary and some modification may be required for improvement, especially if the new grading system is modified for any part of bone and soft tissue sarcomas.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta R, India S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Nijhuis PH, Schaapveld M, Otter R, Molenaar WM, van der Graaf WT, Hoekstra HJ. Epidemiological aspects of soft tissue sarcomas (STS)--consequences for the design of clinical STS trials. Eur J Cancer. 1999;35:1705-1710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Samà L, Binder JP, Darrigues L, Couturaud B, Boura B, Helfre S, Chiche L, Nicolas N, Tzanis D, Bouhadiba T, Gentile D, Perlbarg-Samson J, Bonvalot S. Safe-margin surgery by plastic reconstruction in extremities or parietal trunk soft tissue sarcoma: A tertiary single centre experience. Eur J Surg Oncol. 2022;48:526-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Slump J, Hofer SOP, Ferguson PC, Wunder JS, Griffin AM, Hoekstra HJ, Bastiaannet E, O'Neill AC. Flap choice does not affect complication rates or functional outcomes following extremity soft tissue sarcoma reconstruction. J Plast Reconstr Aesthet Surg. 2018;71:989-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Koulaxouzidis G, Schlagnitweit P, Anderl C, Braig D, Märdian S. Microsurgical Reconstruction in Orthopedic Tumor Resections as Part of a Multidisciplinary Surgical Approach for Sarcomas of the Extremities. Life (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Brinkmann EJ, Ahmed SK, Houdek MT. Extremity Soft Tissue Sarcoma: Role of Local Control. Curr Treat Options Oncol. 2020;21:13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Tanaka K, Ozaki T. New TNM classification (AJCC eighth edition) of bone and soft tissue sarcomas: JCOG Bone and Soft Tissue Tumor Study Group. Jpn J Clin Oncol. 2019;49:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 90] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 7. | Hermanek P, Wittekind C. The pathologist and the residual tumor (R) classification. Pathol Res Pract. 1994;190:115-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 150] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Hoang K, Gao Y, Miller BJ. The Variability in Surgical Margin Reporting in Limb Salvage Surgery for Sarcoma. Iowa Orthop J. 2015;35:181-186. [PubMed] |
| 9. | O'Neill AC, Roy M, Boucher A, Fitzpatrick AM, Griffin AM, Tsoi K, Ferguson PC, Wunder JS, Hofer SOP. The Toronto Sarcoma Flap Score: A Validated Wound Complication Classification System for Extremity Soft Tissue Sarcoma Flap Reconstruction. Ann Surg Oncol. 2021;28:3345-3353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Pignatti M, Ogawa R, Mateev M, Georgescu AV, Balakrishnan G, Ono S, Cubison T, Pinto V, D'Arpa S, Koshima I, Hyakusoku H, Hallock GG. Our Definition of Propeller Flaps and Their Classification. Semin Plast Surg. 2020;34:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Sakamoto A, Noguchi T, Matsuda S. A Transposition Flap Reconstruction after Resection of a Soft-Tissue Sarcoma in the Buttock. J Orthop Case Rep. 2021;11:38-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Garreffa E, Hughes-Davies L, Russell S, Lightowlers S, Agrawal A. Definition of Tumor Bed Boost in Oncoplastic Breast Surgery: An Understanding and Approach. Clin Breast Cancer. 2020;20:e510-e515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Tse T, Knowles S, Bélec J, Caudrelier JM, Lock M, Brackstone M, Arnaout A. Consensus statement on tumour bed localization for radiation after oncoplastic breast surgery. Curr Oncol. 2020;27:e326-e331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Alço G, Igdem S, Okkan S, Dincer M, Sarsenov D, Ilgun AS, Agacayak F, Elbüken F, Ercan T, Selamoglu D, Ozmen V. Replacement of the tumor bed following oncoplastic breast-conserving surgery with immediate latissimus dorsi mini-flap. Mol Clin Oncol. 2016;5:365-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Pu LL. Reconstruction of a large gluteal soft-tissue defect with the double-opposing V-Y fasciocutaneous advancement flap. Plast Reconstr Surg. 2007;119:599-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;106-120. [PubMed] |
| 17. | Sampo M, Tarkkanen M, Huuhtanen R, Tukiainen E, Böhling T, Blomqvist C. Impact of the smallest surgical margin on local control in soft tissue sarcoma. Br J Surg. 2008;95:237-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Gronchi A, Miceli R, Fiore M, Collini P, Lozza L, Grosso F, Mariani L, Casali PG. Extremity soft tissue sarcoma: adding to the prognostic meaning of local failure. Ann Surg Oncol. 2007;14:1583-1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Wittekind C, Compton CC, Greene FL, Sobin LH. TNM residual tumor classification revisited. Cancer. 2002;94:2511-2516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 341] [Article Influence: 14.8] [Reference Citation Analysis (0)] |