Published online Jul 24, 2022. doi: 10.5306/wjco.v13.i7.609
Peer-review started: February 8, 2022
First decision: June 7, 2022
Revised: June 15, 2022
Accepted: July 6, 2022
Article in press: July 6, 2022
Published online: July 24, 2022
Processing time: 164 Days and 6.8 Hours
It has been theorized that 75%-80% of febrile neutropenia (FN) is caused by endogenous pathogens, while up to 20% of cases are thought to be caused by a viral infection. It is unknown if precautions such as masking and social distancing reduce the risk of FN in susceptible populations.
To determine whether coronavirus disease 2019 (COVID-19) infection mitigation efforts, namely masking and social distancing, were associated with a reduction in the incidence of FN.
This was a retrospective population based cohort study comparing the incidence of FN in the 13 mo prior to (Year 0) and 13 mo following (Year 1) the public health executive orders (PHEO) in Michigan. Data was queried for all emergency department (ED) visits from April 1, 2019 to March 31, 2021 from the National Syndromic Surveillance Program, a program which collects data that is voluntarily submitted by approximately 89% of Michigan EDs. The primary study outcome was the incidence of FN as a proportion of ED visits in the 13-mo before and 13-mo after COVID-19 mitigations efforts, namely masking and social distancing. We hypothesized that there would be a significant decrease in the incidence of FN in the period following the PHEO aimed at reducing the spread of the severe acute respiratory syndrome coronavirus 2 virus.
There was a total of 8979221 total ED visits captured during the study period. In Year 0 there were 5073081 recorded ED visits and 3906140 in Year 1. There was a significant reduction in the proportion of total ED visits with a diagnosis of FN, decreasing 13.3% across periods (0.15% vs 0.13%, P = 0.036). In patients with a hematologic malignancy a more impressive reduction in the incidence of FN was evident following PHEO (22% vs 17%, P = 0.02).
We found a significant association between social distancing and mask guidelines implemented on a large public scale with decreased rates of FN, particularly in those with a hematologic malignancy. These findings may be useful in the design of future research and recommendations regarding the prevention of FN.
Core Tip: There has been a proven reduction in respiratory viral infections (e.g., flu, common cold, etc.) with the implementation of social distancing and masking during coronavirus disease 2019 mitigation efforts. It has been theorized that up to 20% of febrile neutropenia is caused by viral infections. We found a significant reduction in the incidence of febrile neutropenia following the implementation of public health interventions, namely masking and social distancing, with the overall incidence of febrile neutropenia decreasing by approximately 13%. The largest reduction in febrile neutropenia was found for hematologic malignancies where the incidence of febrile neutropenia declined by 22%.
- Citation: Baracy Jr MG, Hagglund K, Kulkarni S, Afzal F, Arends K, Morris RT, Solomon LA, Aslam MF, Corey L. Decreased incidence of febrile neutropenia in Michigan following masking and social distancing orders for the COVID-19 pandemic: A population based cohort study. World J Clin Oncol 2022; 13(7): 609-615
- URL: https://www.wjgnet.com/2218-4333/full/v13/i7/609.htm
- DOI: https://dx.doi.org/10.5306/wjco.v13.i7.609
Febrile neutropenia (FN) is defined as neutropenia in the setting of a temperature greater than or equal to 100.4 degrees Fahrenheit and is one of the most common and costly complications associated with cancer treatment[1,2]. Granulocyte colony stimulating factor is the most effective prophylaxis against neutropenia and the progression to FN[3,4]. Yet, little is known about non-pharmacological strategies, such as masking, for the prevention of FN in at-risk populations.
Currently, FN prevention strategies include hand hygiene and the avoidance of sick contacts and crowds, however the impact of these efforts is uncertain[5]. Furthermore, the majority of FN with culture-proven bacteremia are thought to be the result of translocation of gut bacteria[6]. Although it has been theorized that 75%-80% of FN is caused by endogenous microorganisms, up to 20% of cases are thought to be caused by communicable pathogens, such as virions[7]. Accordingly, mitigating viral infection in at risks populations would theoretically reduce the incidence of FN. However, we are not aware of any population-based studies evaluating the impact of infection mitigation practices on the incidence of FN.
The public health crisis due to coronavirus disease 2019 (COVID-19) and its corresponding public health interventions provided a unique opportunity to evaluate the impact of social distancing and masking on the incidence of FN. In March of 2020, the state of Michigan issued an Executive Order that urged residents to remain at home and socially distance, which was amended shortly thereafter to include a mask mandate[8]. The aim of our study was to evaluate the association of these mitigation efforts and the incidence of FN in patients presenting to emergency departments (EDs) in the state of Michigan.
This is a retrospective cohort study comparing the incidence of FN in the 13 mo prior to (Year 0, March 1, 2019-March 31, 2020) and the 13 mo following (Year 1, April 1, 2020-April 31, 2021) the public health executive orders (PHEO) in Michigan. Approximately 89% of EDs across Michigan voluntarily submit encounter data (patient’s chief complaint, associated diagnoses, age, sex, intake temperature, intake percent oxygen saturation, and blood pressure) to the National Syndromic Surveillance Program (NSSP). A query was made for all encounters with a diagnosis of Neutropenia (ICD-10-CM D70) from March 1, 2019-April 31, 2021. FN was defined as an intake temperature greater than or equal to 100.4 degrees Fahrenheit and an ICD-10-CM D70. The incidence of FN in Year 0 was compared to the incidence of FN in Year 1. To account for the impact of the COVID-19 pandemic on total ED visits, the incidence of each ICD code was analyzed as a proportion of ED visits for the corresponding year. Associated ICD-10-CM codes were grouped according to Clinically Relevant Groups (CRG) (Supplementary Table 1), modified from the Healthcare Cost and Utilization Project[9]. Analysis of the incidence of FN in each CRG was also performed. A visit containing multiple ICD-10-CM diagnostic codes was included in multiple CRGs, if applicable. This study was deemed exempt by the responsible institutional review board.
Descriptive statistics were generated to characterize the study cohorts. Continuous variables are described as the mean with standard deviation or median with range or interquartile range. Categorical variables are described as frequency distributions. Univariable analysis of factors associated with FN were assessed using Student’s t-test, analysis of variance, and the chi-squared analysis. Multivariable analysis was done using logistic regression. Analyses were conducted using SPSS version 25.0 and a P value less than 0.05 was considered statistically significant.
From March 1, 2019 to April 31, 2021 there were 8979221 total ED visits in the state of Michigan with data submitted to the NSSP and at least one viable ICD-10 code. In Year 0, there were 5073081 recorded ED visits and 3906140 in Year 1, a decrease of 23% (Table 1). There was a total of 5717 encounters with a diagnosis consistent with neutropenia. There was a significant reduction in the proportion of total ED visits with a diagnosis of FN, decreasing 13.3% from Year 0 to Year 1 (0.15% vs 0.13%, P = 0.036).
| Year 0, n (%) | Year 1, n (%) | P value | |
| Total ED visits | 5073081 (56.4) | 3906140 (43.6) | - |
| Visits with neutropenia | |||
| Male | 1572 (48) | 1189 (49) | 0.59 |
| Female | 1704 (52) | 1252 (51) | |
| Age (yr) | 55.1 ± 23.6 | 54.7 ± 23.7 | 0.55 |
| Visits with febrile neutropenia | |||
| Male | 2145 (48) | 616 (50) | 0.35 |
| Female | 2327 (52) | 629 (50) | |
| Age (yr) | 56.2 ± 22.6 | 50.3 ± 26.6 | < 0.0001 |
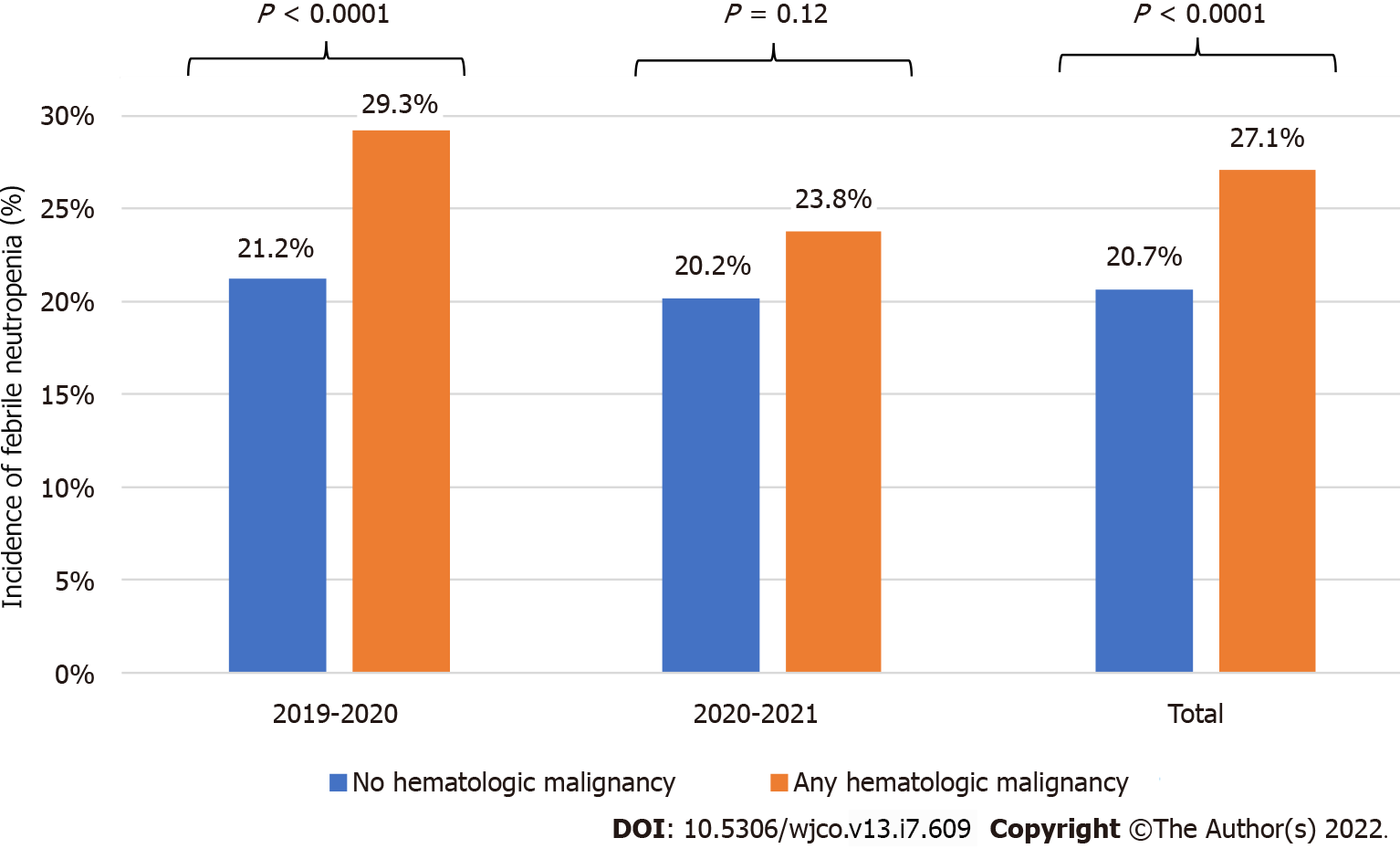
In a sub-analysis of all patients with FN, in patients with a concomitant diagnosis of hematologic malignancy, FN was significantly lower in the period following PHEO (22% vs 17%, P = 0.02, Table 2). In Year 0 there was a 29.3% incidence of FN in neutropenic patients with a CRG of hematologic malignancy, vs a 21.2% incidence in neutropenic patients without a CRG of hematologic malignancy (P < 0.0001, Figure 1). This difference was not observed in Year 1 (23.8% vs 20.2%, P = 0.12). Hematologic malignancy was the only CRG diagnosis to have a relatively higher rate of FN in Year 0 compared to Year 1.
| Neutropenia | Febrile neutropenia | |||||
| Year 01 | Year 12 | P value | Year 01 | Year 12 | P value | |
| Diagnoses | n = 3276 | n = 2441 | n = 740 | n = 505 | ||
| Common infections | 1482 (45) | 974 (40) | < 0.0001 | 403 (55) | 255 (51) | 0.17 |
| Any malignancy | 1237 (38) | 833 (34) | 0.01 | 276 (37) | 182 (36) | 0.65 |
| Solid malignancies | 722 (22) | 511 (21) | 0.32 | 120 (16) | 101 (20) | 0.09 |
| Hematologic malignancies | 564 (17) | 357 (15) | 0.01 | 165 (22) | 85 (17) | 0.02 |
| Benign neoplasms | 147 (5) | 111 (5) | 0.91 | 43 (6) | 17 (3) | 0.05 |
| Non-malignant blood dyscrasias | 1580 (48) | 1213 (50) | 0.27 | 315 (43) | 227 (45) | 0.41 |
| Endocrine, nutritional, and metabolic disorders | 1485 (45) | 1119 (46) | 0.70 | 268 (36) | 200 (40) | 0.23 |
| Skin, musculoskeletal, psychiatric, and nervous system disorders | 1224 (37) | 870 (36) | 0.18 | 211 (29) | 134 (27) | 0.44 |
| Disorders of the cardiopulmonary system | 1639 (50) | 1125 (46) | 0.003 | 324 (44) | 210 (42) | 0.44 |
| Disorders of the gastrointestinal and genitourinary systems | 1332 (41) | 952 (39) | 0.21 | 226 (31) | 159 (32) | 0.72 |
| Coronavirus disease 2019 | 6 (0) | 207 (9) | < 0.0001 | 0 (0) | 45 (9) | - |
The public health response to COVID-19 in the state of Michigan provided a unique opportunity to analyze the impact of social distancing and masking on the incidence of FN. Masking and social distancing designed to prevent the spread of COVID-19 have resulted in the decline of other non-covid viral illnesses[10,11]. Our study is the first to document an association between this phenomenon and a decline in the incidence of FN, both overall and in patients with an ICD-10-CM diagnosis consistent with hematologic malignancy.
In the majority of cases, the underlying cause of FN is unknown, and therefore little is known about the efficacy of non-pharmacological efforts to prevent development of FN in neutropenic patients[12]. We found a significant association between the implementation of public health measures to prevent the spread of communicable diseases and the incidence of FN associated with hematologic malignancies. This is an important finding as patients with hematologic cancers are particularly vulnerable to FN and its associated morbidity and mortality[13]. Our findings suggest that a significant proportion of FN in patients with malignancy may have a viral etiology. Accordingly, health measures, such as masking, may reduce the risk of FN in vulnerable patients.
The strengths of this study include a large number of encounters and associated accurate objective data points (ICD codes and temperature). Additionally, Michigan adopted the stay-at-home orders and mask mandates quickly and broadly, with one of the highest compliance rates of the country during Year 1 (Supplementary Figure 1)[14]. As a result, our results likely accurately reflect the effect of COVID-19 mitigation efforts on FN.
Our study has several limitations in addition to the inherent vulnerability to unmeasured biases found in retrospective studies: (1) There may be a small number of encounters of FN that are missed in this dataset; (2) Only the intake vital signs were available, and a temperature of 100.4°F was selected as the cutoff for diagnosing FN (rather than 101 F) in an effort to have a more inclusive cohort; (3) Each ED visit was treated as a separate encounter. Therefore, a patient with FN who presented to the ED on multiple occasions would be captured multiple times; (4) It is impossible to account for individual patient hesitancy on presenting to ED[14]; (5) Charts review was not possible, so the effect of active myelosuppressive therapy could not be assessed; and (6) The number and identify of facilities contributing data changes over time, and the use of diagnosis codes could be inconsistent across and within facilities.
Our study found a significant association between the implementation of social distancing and mask guidelines and the incidence of FN in ED patients with neutropenia. This reduction was most pronounced in those with a hematologic malignancy. These findings may be useful in the design of clinical trials as well as informing future recommendations for the prevention of FN in vulnerable patients.
It has been theorized that 75%-80% of febrile neutropenia (FN) is caused by endogenous pathogens, while up to 20% of cases are thought to be caused by a viral infection. It is unknown if precautions such as masking and social distancing reduce the risk of FN in susceptible populations.
There has been a proven reduction in respiratory viruses (e.g., flu, common cold, etc.) with the implementation of social distancing and masking in the effort to prevent the spread of coronavirus disease 2019 (COVID-19). We sought to elucidate whether such public health measures would concomitantly reduce the incidence of FN in susceptible populations, namely those with malignancies.
To determine whether COVID-19 infection mitigation efforts, namely masking and social distancing, was associated with a reduction in the incidence of FN.
This is a retrospective population based cohort study comparing the incidence of FN in the 13 mo prior to and 13 mo following the public health executive orders in Michigan. Data was queried for all emergency department visits from April 1, 2019 to March 31, 2021 from the National Syndromic Surveillance Program.
There was a significant reduction in the proportion of total ED visits with a diagnosis of FN, decreasing 13.3% across periods (0.15% vs 0.13%, P = 0.036). In patients with a hematologic malignancy a more impressive reduction in the incidence of FN was evident following PHEO (22% vs 17%, P = 0.02).
Masking and social distancing appear to decrease the risk of FN in susceptible populations, especially among patients with hematologic malignancies.
Masking and social distancing appear to decrease the risk of FN in patients with malignancies, supporting the theory that a proportion of FN may be secondary to communicable infectious particles. Well-designed studies and clinical trials are needed to guide recommendations regarding masking and social distancing for the prevention of FN in vulnerable patients.
We would like to acknowledge the staff from the MDHHS for their help in data collection and management, especially Henderson J.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Haque N, Bangladesh; Karnyoto AS, China S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Lyman GH, Michels SL, Reynolds MW, Barron R, Tomic KS, Yu J. Risk of mortality in patients with cancer who experience febrile neutropenia. Cancer. 2010;116:5555-5563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 171] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 2. | Tai E, Guy GP, Dunbar A, Richardson LC. Cost of Cancer-Related Neutropenia or Fever Hospitalizations, United States, 2012. J Oncol Pract. 2017;13:e552-e561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 3. | Averin A, Silvia A, Lamerato L, Richert-Boe K, Kaur M, Sundaresan D, Shah N, Hatfield M, Lawrence T, Lyman GH, Weycker D. Risk of chemotherapy-induced febrile neutropenia in patients with metastatic cancer not receiving granulocyte colony-stimulating factor prophylaxis in US clinical practice. Support Care Cancer. 2021;29:2179-2186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Mhaskar R, Clark OA, Lyman G, Engel Ayer Botrel T, Morganti Paladini L, Djulbegovic B. Colony-stimulating factors for chemotherapy-induced febrile neutropenia. Cochrane Database Syst Rev. 2014;CD003039. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Centers for Disease Control and Prevention. Information for Patients and Caregivers. [cited 13 July 2021]. In: Centers for Disease Control and Prevention [Internet]. Available from: https://www.cdc.gov/cancer/preventinfections/patients.htm. |
| 6. | Zimmer AJ, Freifeld AG. Optimal Management of Neutropenic Fever in Patients With Cancer. J Oncol Pract. 2019;15:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 7. | Pizzo PA. Management of Patients With Fever and Neutropenia Through the Arc of Time: A Narrative Review. Ann Intern Med. 2019;170:389-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Michigan. Executive Order 2020-153: Masks. [cited 5 June 2021]. In: Michigan [Internet]. Available from: https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-535105--,00.html. |
| 9. | Agency for Healthcare Research and Quality. Clinical Classifications Software Refined (CCSR). [cited 5 June 2021]. In: Agency for Healthcare Research and Quality [Internet]. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp. |
| 10. | Dezman ZDW, Stryckman B, Zachrison KS, Conrad RM, Marcozzi D, Pimentel L, Samuels-Kalow M, Cairns CB. Masking for COVID-19 Is Associated with Decreased Emergency Department Utilization for Non-COVID Viral Illnesses and Respiratory Conditions in Maryland. Am J Med. 2021;134:1247-1251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Chu DK, Duda S, Solo K, Yaacoub S, Schunemann H. Physical Distancing, Face Masks, and Eye Protection to Prevent Person-to-Person Transmission of SARS-CoV-2 and COVID-19: A Systematic Review and Meta-Analysis. J Vasc Surg. 2020;72:1500. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 129] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 12. | Kuderer NM, Dale DC, Crawford J, Cosler LE, Lyman GH. Mortality, morbidity, and cost associated with febrile neutropenia in adult cancer patients. Cancer. 2006;106:2258-2266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 768] [Cited by in RCA: 808] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 13. | Institute for Health Metrics and Evaluation. COVID-19 Projections. [cited 6 September 2021]. In: Institute for Health Metrics and Evaluation [Internet]. Available from: https://covid19.healthdata.org/united-states-of-america/michigan?view=mask-use&tab=trend. |
| 14. | Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 577] [Cited by in RCA: 833] [Article Influence: 166.6] [Reference Citation Analysis (0)] |