Published online Jun 24, 2022. doi: 10.5306/wjco.v13.i6.423
Peer-review started: January 14, 2022
First decision: March 24, 2022
Revised: April 10, 2022
Accepted: June 4, 2022
Article in press: June 4, 2022
Published online: June 24, 2022
Processing time: 159 Days and 13.4 Hours
Given the increasing complexity of cancer care, multidisciplinary tumor boards have become essential in daily clinical oncology practice. The Project Extension for Community Healthcare Outcomes (ECHO) initiative developed an innovative telementoring model using a "hub and spoke" design consisting of a team of experts (hub) that offers a full service to multiple participants (the spokes) during regularly scheduled sessions discussing patients' clinical cases. The Alexander Fleming Cancer Institute in Buenos Aires was the first hub in Latin America to implement Project ECHO for gastrointestinal tumors. In our 3-year experience, 80 patients from 37 centers were evaluated within Project ECHO and a range of three to five cases were discussed in each meeting. From our perspective, the impact of this novel approach was a remarkable strategy to reduce care disparities by equalizing access to high-quality medical knowledge in a multidisciplinary environment for medical discussions. Additionally, it was shown to have a cost-effective impact directly on the patients and the local health system, since relevant costs were saved after unnecessary treatments, studies and travel expenses were avoided.
Core Tip: Tumor boards (TBs) have existed for the last 50 years, and at the present time, represent an essential strategy in daily clinical oncology practice. We reported our positive experience and perspective with a novel approach of multidisciplinary virtual TBs using an innovative telementoring model called Project Extension for Community Healthcare Outcomes. This first experience in Latin America for gastrointestinal tumors has shown to reduce care disparities by equalizing access to high-quality medical knowledge in a context of a multidisciplinary environment for medical discussions.
- Citation: Esteso F, Tissera NS, O'Connor JM, Luca R, Huertas E, Sánchez Loria F, Pedraza I, Pairola A, Brancato F, Paganini L, Kucharczyk M, Amat M, Pombo MT, Galli M, Bruno L, Caro L, Rodriguez A, Enrico D, Waisberg F, Chacón M. Implementation of a virtual multicenter gastrointestinal tumor board to reduce cancer disparities in Argentina. World J Clin Oncol 2022; 13(6): 423-428
- URL: https://www.wjgnet.com/2218-4333/full/v13/i6/423.htm
- DOI: https://dx.doi.org/10.5306/wjco.v13.i6.423
During recent decades, cancer care has become increasingly complex mainly due to the personalized approach for every single patient. Each patient requires a careful assessment which often involves a multidisciplinary effort and experienced physicians. However, many countries experience the centralization of tertiary referral cancer units in the most populated cities. In many urban centers in Argentina, medical oncologists provide care for patients with multiple types of cancer which challenges practitioners to stay current with the evidence that is necessary to deliver high-quality care. However, given the increasing knowledge of cancer, and the observed trend of subspecialization among oncologists, tumor boards (TBs) have become a widely accepted and successful strategy to promote discussion and evidence-based decisions in a scenario with unequal health access[1,2].
A TB is a multidisciplinary treatment planning approach in which health professionals with different specialties review and discuss the diagnosis and treatment strategies using an integrative approach[3]. In the past few years, TBs have incorporated virtual modalities to make them accessible in remote locations, promoting timely diagnostic and treatment planning for patients in different regions and socioeconomic settings.
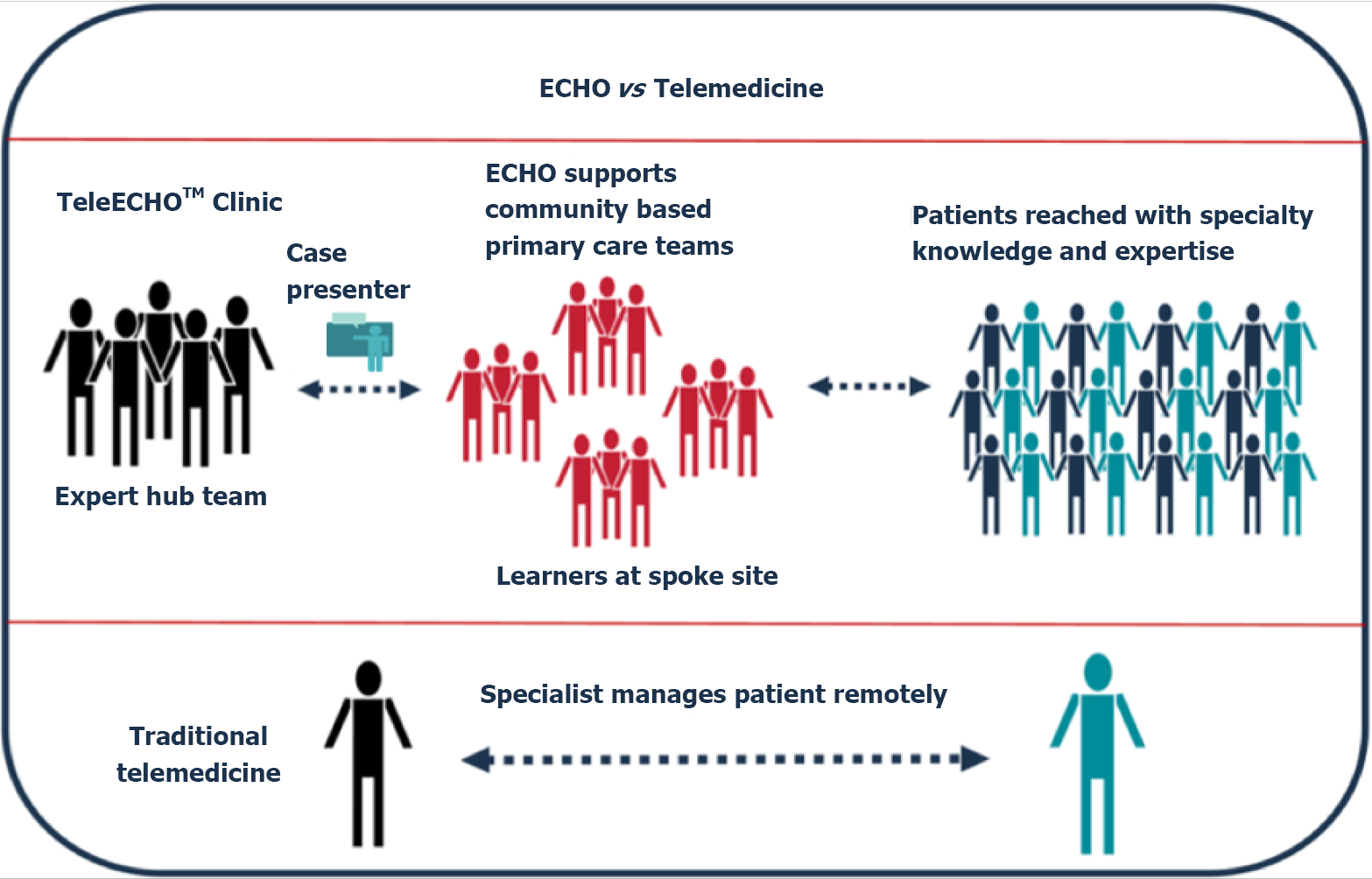
In this context, Project Extension for Community Healthcare Outcomes (ECHO) created by Dr. Sanjeev Arora in 2003 in New Mexico, EEUU, uses video conferencing technology to discuss cases and treat rural cases of hepatitis-C[4]. It aims to reduce health disparities by allowing clinicians to share current medical knowledge in underserved and remote areas to cooperate with the care of patients with hepatitis C through innovative telementoring. The ECHO model uses a hub-and-spoke knowledge-sharing approach where expert teams lead virtual meetings amplifying the capacity for providers to deliver best-in-practice care to underserved areas in their communities (Figure 1)[5]. This "hub and spoke" design consists of a model that arranges a network consisting of a team of experts (the hub) that offers a full service to multiple participants (the spokes) during regularly scheduled sessions where patients with clinical cases that need a more accurate treatment are discussed[6,7]. The use of this design also provides the capability to facilitate clinical mentoring and the implementation of regular educational sessions for medical training. Thus, the ECHO approach represents a completely different model than “telemedicine”, wherein a specialist assumes the care of a patient in a typical consultation by using remote technology.
Currently, over 373 academic centers serve as ECHO hubs for multiple severe medical conditions such as infectious diseases, rheumatologic diseases, chronic pain, addiction, human immunodeficiency virus, diabetes, complex multisystem diseases and cancer[8,9].
Multidisciplinary virtual TBs represent an opportunity to reduce the existing care disparities by information equality. Under this premise, the Alexander Fleming Cancer Institute in Buenos Aires was the first hub in Latin America to implement Project ECHO for gastrointestinal tumors. Since December 2017, monthly virtual meetings (an hour and a half long) using videoconferencing software have been performed to discuss cases of gastrointestinal cancer. The participating physicians had primary practices in academic and community general hospitals in at least 8 provinces of Argentina. The central hub staff was composed of surgeons, radiotherapists, imaging specialists, pathologists, genetic counselors, gastroenterologists and medical oncologists specifically dedicated to gastrointestinal cancer care. The modality included a case-based discussion followed by a moderated discussion with a final medical recommendation taking into account local available resources. The first 15 min of each meeting were dedicated to an educational lecture.
In our 3-year experience, 80 patients were evaluated within the Project ECHO, and a range of three to five cases was discussed in each meeting (Table 1). During the first 2 years, 15 health centers regularly participated in the virtual meetings. Notably, exponential growth was observed concurrently with the coronavirus disease 2019 (COVID-19) quarantine. Since June 2020, professionals from an average of 37 centers have habitually participated in these monthly meetings. Of note, each participating institution decided and proposed to the expert hub team the most relevant clinical cases that required a multidisciplinary discussion to the expert hub team. The median time from the first oncology visit until the ECHO referral was 16 d (range 12-19).
| Characteristics | n = 80 |
| Age (range) | 57 yr (48-68) |
| Sex | |
| Male | 45 (56.25%) |
| Female | 35 (43.75%) |
| Tumor type | |
| Colorectal cancer | 43 (53.75%) |
| Neuroendocrine | 14 (17.5%) |
| Esophagogastric | 12 (15%) |
| Biliodigestive | 7 (8.75%) |
| Anal | 3 (3.75%) |
| Appendix | 1 (1.25%) |
| Stage | |
| Locally/locally advanced | 52 (65%) |
| Metastatic | 28 (35%) |
| Treatment strategy management | |
| Local institution | 60 (75%) |
| Referred to specialized cancer center | 20 (25%) |
| Reference areas of Argentina (Province) | |
| North | 40 (50%) |
| Center | 24 (30%) |
| South | 16 (20%) |
Most patients included in the program were diagnosed with colorectal cancer (n = 43, 53.75%), followed by neuroendocrine (n = 14, 17.5%), esophagogastric (n = 12, 15%), biliodigestive (n = 7, 8.75%), anal (n = 3, 3.75%) and appendix (n = 1, 1.25%) tumors. Most patients had advanced disease at the time of presentation to the TB (n = 28, 40%). Case discussions included systemic treatment for the advanced scenario, surgical approaches, and adjuvant decisions. Of note, the suggested strategies were mostly managed at local places (n = 60, 75%); other patients were referred to the Alexander Fleming Cancer Institute or tertiary health care centers (n = 8, 10%) for surgery or chemotherapy (n = 10, 12.5%) and a minority of cases were referred for radiotherapy (n = 2, 2.5%). Notably, during the COVID-19 pandemic period, only 6% of the patients were suggested to receive centralized treatment at a tertiary center. In addition, participant satisfaction was evaluated by a centralized digital survey provided to 30 professionals showing the highest level of satisfaction in 25 (83%) participants.
TBs have existed for the last 50 years and have been proven to improve medical training and, in the long run, patient care[10]. Under current conditions, Project ECHO emerges as a collaborative and integrative networking environment for cancer management in remote locations. The impact of novel virtual TB approaches in Argentina is a remarkable strategy to reduce care disparities by equalizing access to a multidisciplinary environment for medical discussions. Furthermore, these models have proven to be consistently cost-effective. Available evidence has highlighted that relevant costs were saved after unnecessary treatments, studies and travel expenses were avoided. The latter is particularly relevant, considering the vast extensions of Argentina[11-14]. As a typical example, a patient with a specific gastrointestinal tumor who would need to travel and have a consultation at a reference cancer center in Argentina would have to spend approximately 500 USD regardless of the study and treatment. Additionally, in terms of saving time, this strategy could normally take approximately 3 more weeks in delaying the treatment plan decision in Argentina.
Our heal system is heterogeneous, including the private and public sub-systems. Under this circumstance, some patients have to be referred to tertiary or local centers for coverage of treatment and studies to become effective. We believe that the discussion of the clinical cases in a context such as the ECHO initiative represents one of the better chances for high-quality cancer care considering that the referral does not cause a significant delay in the treatment. In our health system context, the virtual ECHO initiative would be more accessible, accurate, affordable and properly developable than the strategy of extending more sub-specialized oncologists in urban and suburban areas.
Our Project ECHO experience has led us to address some important factors that should be improved upon in the future. Internet access, low-quality video-conferencing devices and protected time availability are some of the key areas to expand in the future. The participation of professionals with non-oncology medical specialties should also be promoted to facilitate a comprehensive discussion of the multiple dimensions that are involved in cancer care.
One of the potential limitations of the virtual TB approach could be the lack of complete information on the clinical case for proper and personalized clinical decision-making, given that the medical opinions of the board are based on the case presentation and not on the direct evaluation of the patient. Additionally, monthly meetings may not meet the demand, mainly in situations when a medical decision is urgent.
Although limited, our experience was extremely positive. We are convinced that this strong professional network also creates a unique opportunity to promote national evidence-based recommendations, academic collaborations and clinical cancer research, as well as continuing medical education programs.
In our view, multidisciplinary virtual experiences, such as the Project ECHO, should be carefully addressed by health care decision-makers given their popularity and their demonstrated cost-effectiveness. Many of the evaluated barriers require government participation to improve budget and technology access in health care facilities. The COVID-19 pandemic has led to a tremendous need to incorporate modern technology into different work scenarios. Under these circumstances, the implementation of virtual educational and medical activities may be one of the key elements that cannot be excluded in the design and execution of National Cancer Control Programs.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Argentina
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dhali A, India; El-Nakeep S, Egypt; Tsagkaris C, Switzerland A-Editor: Liu X, China S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Taberna M, Gil Moncayo F, Jané-Salas E, Antonio M, Arribas L, Vilajosana E, Peralvez Torres E, Mesía R. The Multidisciplinary Team (MDT) Approach and Quality of Care. Front Oncol. 2020;10:85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 226] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 2. | Specchia ML, Frisicale EM, Carini E, Di Pilla A, Cappa D, Barbara A, Ricciardi W, Damiani G. The impact of tumor board on cancer care: evidence from an umbrella review. BMC Health Serv Res. 2020;20:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 143] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 3. | Definition of tumor board review. NCI Dictionary of Cancer Terms - National Cancer Institute 2011. [cited 11 August 2021]. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/tumor-board-review. |
| 4. | Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, Parish B, Burke T, Pak W, Dunkelberg J, Kistin M, Brown J, Jenkusky S, Komaromy M, Qualls C. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-2207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 701] [Cited by in RCA: 810] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 5. | ECHO. Project ECHO. [cited 11 August 2021]. Available from: https://hsc.unm.edu/echo/. |
| 6. | Singh DA. Essentials of the U.S. Health Care System. Jones & Bartlett Publishers; 2015: 421. |
| 7. | Elrod JK, Fortenberry JL Jr. The hub-and-spoke organization design: an avenue for serving patients well. BMC Health Serv Res. 2017;17:457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 199] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 8. | ECHO. Hubs & Programs [Internet]. [cited 11 August 2021]. Available from: https://hsc.unm.edu/echo/data-marketplace/interactive-dashboards/. |
| 9. | ECHO. Superhubs: sitios de formación de ECHO [Internet]. [cited 11 August 2021]. Available from: https://es.hsc.unm.edu/echo/get-involved/superhubs.html. |
| 10. | Quero G, Salvatore L, Fiorillo C, Bagalà C, Menghi R, Maria B, Cina C, Laterza V, Di Stefano B, Maratta MG, Ribelli M, Galiandro F, Mattiucci GC, Brizi MG, Genco E, D'Aversa F, Zileri L, Attili F, Larghi A, Perri V, Inzani F, Gasbarrini A, Valentini V, Costamagna G, Manfredi R, Tortora G, Alfieri S. The impact of the multidisciplinary tumor board (MDTB) on the management of pancreatic diseases in a tertiary referral center. ESMO Open. 2021;6:100010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 11. | Eckman MH, Gordon SC, Talal A, Schiff ER, Sherman KE. Cost-Effectiveness of Screening for Chronic Hepatitis CInfection in the United States. Hepatology. 2012;56:191A-1144A. |
| 12. | Wong JB, Thornton KA, Carroll C, Arora S. Cost-effectiveness of Hepatitis C Treatment by PrimaryCare Providers Supported by the Extension for Commu-nity Healthcare Outcomes (ECHO) Model. Hepatology. 2013;58:328A-331A. |
| 13. | Brandão M, Guisseve A, Bata G, Firmino-Machado J, Alberto M, Ferro J, Garcia C, Zaqueu C, Jamisse A, Lorenzoni C, Piccart-Gebhart M, Leitão D, Come J, Soares O, Gudo-Morais A, Schmitt F, Tulsidás S, Carrilho C, Lunet N. Survival Impact and Cost-Effectiveness of a Multidisciplinary Tumor Board for Breast Cancer in Mozambique, Sub-Saharan Africa. Oncologist. 2021;26:e996-e1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Kočo L, Weekenstroo HHA, Lambregts DMJ, Sedelaar JPM, Prokop M, Fütterer JJ, Mann RM. The Effects of Multidisciplinary Team Meetings on Clinical Practice for Colorectal, Lung, Prostate and Breast Cancer: A Systematic Review. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |