Published online Dec 24, 2020. doi: 10.5306/wjco.v11.i12.968
Peer-review started: June 4, 2020
First decision: October 6, 2020
Revised: October 9, 2020
Accepted: October 30, 2020
Article in press: October 30, 2020
Published online: December 24, 2020
Processing time: 196 Days and 20.7 Hours
Due to coronavirus disease 2019 pandemic caused by severe acute respiratory syndrome coronavirus 2, there has been a major reallocation of resources that has impacted the treatment of many diseases, including cancer. The growing use of information and communication technologies (ICT), together with a new approach to work aimed at ensuring the safety of health care professionals and patients alike, has allowed us to maintain the quality of care while ensuring biosecurity. The application of ICT to health care (eHealth) aims to significantly improve the quality, access to, and effectiveness of medical care. In fact, the expanded use of ICT has been recognized as a key, cost-effective priority for health care by the World Health Organisation. The medical speciality of radiation oncology is closely linked to technology and as a consequence of coronavirus disease 2019, ICT has been widely employed by radiation oncologists worldwide, providing new opportunities for interaction among professionals, including telemedicine and e-learning, while also minimizing treatment interruptions. Future research should concentrate on this emerging paradigm, which offers new opportunities, including faster and more diverse exchange of scientific knowledge, organizational improvements, and more efficient workflows. Moreover, these efficiencies will allow professionals to dedicate more time to patient care, with a better work-life balance. In the present editorial, we discuss the opportunities provided by these digital tools, as well as barriers to their implementation, and a vision of the future.
Core Tip: We believe that the current crisis is an opportunity to take advantage of the momentum towards the greater implementation of electronic health, to improve care through telemedicine, remote work, and e-learning. The emergence of information and communication technologies has transformed the speciality of radiation oncology into teleradiotherapy. Future research should focus on this emerging paradigm, which allows greater flexibility, thereby freeing up time for more efficient and humane patient care.
- Citation: Fernández C, Ruiz V, Couñago F. COVID-19 and information and communication technology in radiation oncology: A new paradigm. World J Clin Oncol 2020; 11(12): 968-975
- URL: https://www.wjgnet.com/2218-4333/full/v11/i12/968.htm
- DOI: https://dx.doi.org/10.5306/wjco.v11.i12.968
Progress is impossible without change, and those who cannot change their minds cannot change anything (George Bernard Shaw).
During coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2, technologies are playing a crucial role in keeping our society functional. And these technologies may have a long-lasting impact beyond COVID-19.
We start from the advantage the medical speciality of radiation oncology is closely linked to technology, which continues to advance at a rapid pace. The advent of computed-tomography based contouring led to the transition from two-dimensional to three-dimensional treatment planning in the 1980s and 1990s. Due to continuous technological progress, the field of radiation oncology has had to continually evolve and adapt to changing technologies[1], which include advances in radiological imaging, engineering, and computerization. This has led to remarkable advances in the precision of radiotherapy delivery, including novel modalities such as intensity-modulated radiotherapy, volumetric intensity-modulated arc therapy, stereotactic radiosurgery, stereotactic body radiotherapy, and proton therapy. Moreover, all of these advanced techniques are guided by imaging or surface-guided radiotherapy.
Despite the important role of technology in radiation oncology, this speciality involves much more than just machines[2], which are no substitute for real people in clinical practice. Behind increasingly sophisticated linear accelerators are dedicated professionals who continually work to keep up to date with the latest tools and treatments provide patients with the best possible care. The clinical setting requires close teamwork and an established workflow, which starts with the initial consultation followed by computed-tomography simulation, dosimetry and planning, treatment administration, follow-up for potential toxicity, and post-treatment consultations.
Information and communication technologies (ICT) have become an essential component of our profession, leading to changes in how we communicate with each other and with patients. Telemedicine and telehealth services facilitated through videoconferencing software are becoming increasingly accepted in routine medical practice. Although most professional training continues to be done in person (e.g., at medical congresses), a growing number of health care professionals and medical associations now use social media and other online or offline channels, with a good example being the use of Twitter at congresses[3,4].
The COVID-19 pandemic has altered many aspects of our personal and professional lives, and health care systems are no exception. This pandemic has forced hospitals and clinics to reorganize their health care activity practically overnight. Most health care professionals in primary care, the emergency department, and intensive care units have successfully adapted to meet the unprecedented demands imposed by the crisis.
The clinical management of life-threatening illnesses unrelated to COVID-19, such as cancer, has required a profound and highly challenging redistribution of resources[5]. This has been especially relevant in oncology due to the immunosuppressive effects of many cancer treatments, as cancer patients have an elevated risk of infection with the syndrome coronavirus 2 virus and of developing serious complications from COVID-19[6]. Moreover, given that cancer patients tend to be older with more comorbidities than younger people, the risks posed by COVID-19 are even greater.
Approximately 50% of all cancer patients are treated with radiotherapy. During the COVID-19 epidemic, the role of radiotherapy in the management of oncological patients has become even more important due to delays in chemotherapy and surgery. To minimize treatment interruptions, radiation oncology departments have adopted a range of solutions, including prioritization of treatment according to the urgency, and an increased use of ICT and shorter treatment schemes (hypofractionated or ultrahypofractionated)[7]. Other measures include personal protective equipment, shift changes, and remote work from home, all of which have helped to maintain the quality of care while ensuring the safety of both patients and health care professionals. Clinical trials have even been performed to evaluate a role for radiotherapy outside of cancer therapy, such as the use of low-dose radiotherapy to treat pneumonia associated with COVID-19[8]. Recommendations to optimize radiotherapy during the epidemic can be summarized by the acronym RADS[9] (Remote, Avoid, Defer, Shorten), which recommends performing remote consultations when possible, and avoiding (if clinically appropriate or an effective alternative exists), deferring (when clinical feasible), or shortening radiotherapy treatments.
Once the mitigation phase of the COVID-19 pandemic has passed, the next phase is containment. In this phase, it is essential to prevent crowded waiting areas, which means that patients must come unaccompanied, and masks are essential. Before a patient is allowed to enter the waiting area, it is important to continue to check for fever, and to ask patients about symptoms (fever, cough, respiratory distress, anosmia) and/or contact with symptomatic individuals. Proper hand hygiene and disinfection of common spaces will also continue. Clearly, given the need for these precautionary measures, we cannot immediately return to the previous status quo, and thus we are forced to rethink how we organize our departmental workflows and processes.
Electronic health (eHealth) has been defined as ICT applied to health care. Its objective is to significantly improve the quality, access, and effectiveness of health care for all. The World Health Organization has recognized eHealth as a fundamental and cost-effective priority. The 58th World Health Assembly[10] took a historic step in support of eHealth when it approved a resolution to recognize the role of ICT to strengthen health care systems[11,12]. Following this resolution, the use of eHealth-related terminology[13] has exploded, with the most common terms being telemedicine; telehealth; mobile health; electronic medical or health records; digital imaging and communication in medicine; videoconferences and distance learning; Big Data; “wearables” (internet of things); and artificial intelligence. The general term that encompasses all the other concepts is eHealth. According to the European Coordination Committee of the Radiological, Electro-medical and Healthcare IT Industry[14], telemedicine encompasses concepts such as telehealth, telecare, and teledisciplines. Telehealth refers to the diagnosis, monitoring, management and empowerment of patients with chronic conditions.
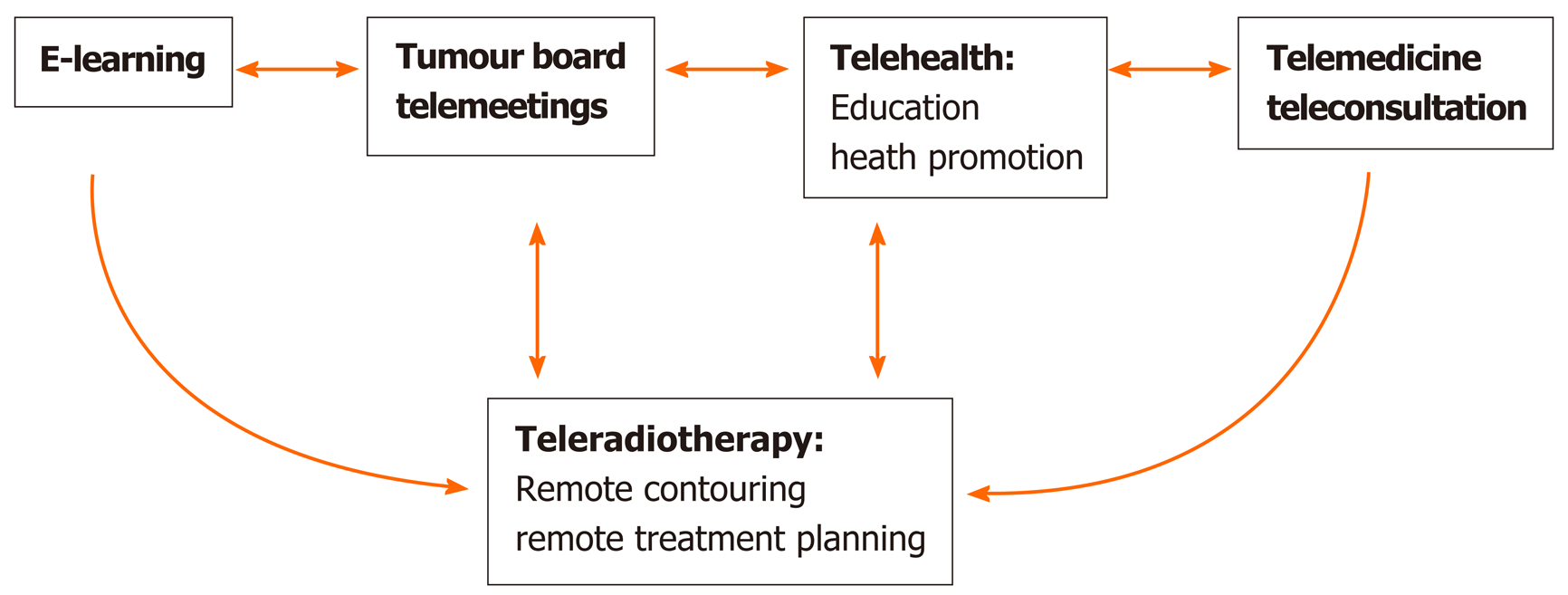
The increasing use of social networks and eHealth in oncology (Figure 1) offers new opportunities for health care professionals and institutions to interact with patients or other professionals through various different channels: (1) Distance learning[15] (e-learning), which offers the opportunity for professional development and knowledge exchange among professionals through both telephone and videoconferences; (2) Tumour board telemeetings; (3) Telehealth including education and health promotion; and (4) Telemedicine and teleconsultation.
The speciality of radiation oncology is currently undergoing a paradigm shift due to the growing use of ICT. Radiation oncology is transforming into a telediscipline known as teleradiotherapy (Figure 1), which allows specialists to conduct consultations, contouring, and treatment planning remotely. In some centres, this teleradiotherapy model was already in place prior to the pandemic, mainly to manage patients who live at a great distance from the cancer treatment centre[16]. The teleradiotherapy model can reduce the number of patient consultations requiring a physical presence by combining, in a single visit, the initial consultation with treatment simulation. In addition, follow-up can also be performed remotely through the use of imaging tests, blood tests, and biopsy result in patients in who do not require a physical examination. During the COVID-19 pandemic, we have also witnessed and participated in new ways of working, including online congresses, videoconferences with other professionals, remote management and treatment of patients, and new forms of healthcare management.
The COVID-19 pandemic has precipitated a series of changes in the physician-patient relationship[17], as well as in the work environment of radiation oncology departments[18,19]. Due to the high risk of contagion in the hospital setting, especially during the mitigation phase of the epidemic, it is important to minimize exposure to the hospital environment in order to reduce the risk of infection with this novel virus. As a result, there has been an increased use of existing tools (e.g., remote contouring, remote planning, teleconsultation, telemeetings.) that were previously underutilized, mainly due to the inertia (resistance to change) that is common in many large institutions, including hospitals.
In these exceptional circumstances, working from home has enabled healthcare professionals to minimize physical contact with patients (who could be infected with the virus), and also allowed patients to avoid unnecessary travel. The conditions imposed by the pandemic have obliged us to take a much more flexible and proactive attitude to health care, pushing us ever closer towards the telemedicine model, which offers greater flexibility for both physicians and patients. In short, in this context, the availability of ICT has been a blessing that will surely continue to provide benefits in the future, even after the pandemic has passed.
Social networks such as Twitter have proven to be powerful tools, with an immense potential to transform continuing medical education[20], which has also been accelerated by COVID-19[21]. Nor can we overlook the emergence of mobile health applications[22] used for patient follow-up. These applications have proven invaluable to assess side effects, quality of life, and treatment satisfaction, thus improving workflows[23].
Given the highly technical nature of our speciality, radiation oncologists are accustomed to adapting to continuous technological advances in equipment, planning systems, imaging devices, and software. Nevertheless, our workflow and clinical practices remain practically unchanged and conventional.
The unprecedented historical impact of the COVID-19 epidemic will require a profound analysis in the near future. However, this crisis has provided us with an opportunity to reinterpret the physician-patient relationship, as well as to rethink our approach to work as radiation oncologists. Clearly, without the assistance of ICT, the consequences of the epidemic would have been much more severe. Paradoxically, in this time of forced confinement, mobile technology, the possibility of videoconferencing and telephone calls have brought us closer together. The availability of electronic devices such as smartphones has provided the means for isolated patients to communicate with their physicians and their families. We have even been able to obtain real-time information from other countries going through similar circumstances. Radiation oncologists have learned to create telematic (i.e., online and mobile) communication and work networks, to receive training sessions through webinars and social networks, as well as to access emerging research through open access publications. All of these tools have contributed to our knowledge about COVID-19 and the dimensions of the epidemic.
Despite the many advantages of telemedicine, there are numerous potential barriers to consider[24,25]. Barriers to implementing remote consultations are summarized in Table 1.
| Technological barriers |
| Availability of smart phones or mobile devices |
| Mobile network coverage |
| Lack of a dedicated, properly-equipped office in the hospital to conveniently and rapidly program and conduct a remote visit that is comparable to a real-life consultation. This equipment would include videoconferencing software to allow for a proper anamnesis, with hands-free headphones to allow the physician to record data on the eMR, and automatic telephone dialling |
| Electronic medical record formats and the capability to order complementary tests through the software |
| Physical barriers |
| Telephone consultation and difficult anamnesis in some cases, such as patients with a laryngectomy, cognitive impairment, hearing loss, neurological diseases, or poor language skills (i.e., foreigners), etc; |
| Impossibility of performing a correct physical examination of patients |
| Communication barriers |
| Physicians |
| Use of technical jargon |
| Semantic barriers: Inability to understand the language used by the sender or the receiver |
| Lack of body language signals (telephone consultations) |
| Potential lack of empathy in telephone consultations |
| External interruptions |
| Patients |
| Mental (“not thinking clearly”) and emotional blocks |
| Fear of asking questions |
| Lack of family support during the teleconsultation |
| Potential misinterpretation of the message |
| Feelings of inferiority |
| Misinformed or “overinformed” (infodemia) |
| External interruptions |
| Difficulties in understanding how to behave in this unique setting: Respect, cordiality and a collaborative attitude |
| Psychological barriers |
| Physicians |
| Feelings of insecurity due to work processes outside of routine practices; |
| Perceived deterioration in the doctor-patient relationship, in which it is necessary to cede more power and autonomy to the patient with more open dialogue (and a less paternalistic relationship) |
| The need to use an appropriate tone of voice, ask clear and concise questions, use warm and friendly language, and practice active listening when communicating with patients |
| Potential to perceive a certain loss of humanity due to the lack of physical presence |
| Patients |
| If the patient cannot see the physician (e.g., telephone call), this can produce feelings of depersonalization |
| The patient may be accustomed to letting the physician make health-related decisions |
| The patient may have difficulties describing symptoms in a virtual setting |
| Bioethical barriers |
| Confidentiality and privacy |
| Data protection |
| The remote consultation cannot replace a face-to-face visit, but rather complements it |
| Risks related to computer security and hacking |
Once these barriers have been overcome, then we will be ready to develop new models of healthcare that are more efficient, versatile, convenient, and welcoming. The key is to learn new skills, to improve access to the available technology, and simply to get started.
Areas to target for improvement and improvements specific to radiation oncology are summarized in Table 2.
| Areas to target for improvement |
| Specific agenda only for remote consultations that is separate from face-to-face consultations |
| Ensure that video-assisted consultations include automatic dialling, headphones, a camera and a microphone |
| Implementation of electronic prescriptions |
| Ability to directly order complementary tests telematically |
| Possibility of sending notifications and reminders to the patient's mobile phone |
| Health care education and promotion directly from primary care |
| Increased digital literacy in the general population |
| Computer security measures |
| Provision of technology in rural areas: Mobile coverage, access to devices, etc |
| Remote consultations considered as a complement to face-to-face visits |
| Emotional support for the patient, family involvement, motivation and commitment |
| Provide legal safeguards for these tools |
| Improvements specific to radiation oncology |
| Regulation of remote work (“work from home”) options in the radiation oncology. For example, it would be feasible to work from home one day each week to perform remote contouring or other work that does not require a physical presence. Working from home should be considered a natural extension of our work, although potential disadvantages must be considered: Failure to disconnect from work, lack of clarity regarding work organization, and difficulties in the work-life balance |
| To apply Big Data in our work, we need appropriate electronic medical records and data reporting formats that provide us with feedback on our results, which can then be used to improve clinical care |
We believe that telemedicine is here to stay. It would be wrong to believe that telemedicine is only a temporary response to a crisis and that we will return to the pre-epidemic status quo. We must seize the opportunity to improve our healthcare work processes in a new era. Numerous health care issues (unrelated to COVID-19) can be resolved online or through mobile devices, thus reducing unnecessary travel and saving valuable time. Studies have found that patients are highly satisfied with remote consultations. For example, a survey conducted by Hamilton et al[16] found that 54.7% of patients preferred telemedicine for future consultations, while 34.9% preferred a mix of online and in-person consultations, with less than 1% expressing a preference for in-person access only.
Our work experience during the COVID-19 crisis has largely been positive. Patients generally feel that they are well-cared for and that their physicians listen to them, both of which give patients peace of mind. They have even congratulated professionals, thanking them for making the effort to transform their usual clinical practices in record time. Patients appear to understand that, in this new world, they need to be more proactive in regard to their own health, and they are more aware of the benefits of self-care. For physicians, remote work has allowed us to continue our clinical practice without causing major delays in treatment or in accumulating pending visits. It has also allowed us to more clearly identify what is urgent and what is not. In short, this crisis has allowed us to eliminate practices that add little value.
In radiation oncology, radiotherapy treatment planning can be performed remotely, with no need to be physically present at the hospital. By enabling physicians to work from home (i.e., teleconsultations or remote treatment planning), we have been able to continue our clinical practice uninterrupted. This versatility and convenience has undoubtedly reduced stress levels. The option to work remotely has been especially critical for professionals in quarantine and for those who needed to stay home for family or personal reasons. Moreover, it has allowed us to avoid prolonged exposure to the hospital environment, thus minimizing the risk of contagion. Future research should concentrate on evaluating this new paradigm, which offers new opportunities, including faster and more diverse exchange of scientific knowledge, organizational improvements, more efficient workflows, and more time to dedicate to patient care. Importantly, this new paradigm allows us to better balance our personal and professional lives, something that is always difficult to achieve. The digitization of our work will make it more flexible, faster, safer, and more efficient. In short, this shift marks a revolution for the better for all parties involved.
Information and communication technologies allow us to offer patients more frequent and more efficient clinical consultations. Patients now have the ability to contact us through a wide range of different channels: Face-to-face, online (videoconference or telephone consultation), or offline (email), eliminating classic space/time barriers. However, it is essential that we continue striving to be good communicators, innovators, and creative people. We must also, first and foremost, be good, humane providers of quality health care for our patients. ICT can help us achieve all of these aims by strengthening the bonds between health care professionals and patients using a novel and dynamic approach.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Georgiev T, Patel HR S-Editor: Zhang H L-Editor: A P-Editor: Zhang YL
| 1. | Jawerth N. Killing more cancer cells than ever before: A new era in radiotherapy. IAEA Bull. 2018;59:4-5. |
| 2. | Swisher-McClure S, Bekelman JE. It's the Team, Not the Beam. Int J Radiat Oncol Biol Phys. 2019;104:734-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Pemmaraju N, Thompson MA, Mesa RA, Desai T. Analysis of the Use and Impact of Twitter during American Society of Clinical Oncology Annual Meetings from 2011 to 2016: Focus on Advanced Metrics and User Trends. J Oncol Pract. 2017;13:e623-e631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | Pereira I, Turner S, Siva S, Pereira I, Albert A. A, Loblaw DA, Simcock .A, Zaorsky NG, Katz, MS. Development of Structured Radiation Oncology Hashtags to Improve Online Communication. Int J Radiat Oncol. 2019;105:E143. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, Wolff RA, Ibrahim NK, Chua MLK, Hotte SJ, Meyers BM, Elfiki T, Curigliano G, Eng C, Grothey A, Xie C. A Practical Approach to the Management of Cancer Patients during the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group. Oncologist. 2020;25:e936-e945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 443] [Cited by in RCA: 458] [Article Influence: 91.6] [Reference Citation Analysis (0)] |
| 6. | Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3332] [Cited by in RCA: 3123] [Article Influence: 624.6] [Reference Citation Analysis (0)] |
| 7. | Simcock R, Thomas TV, Estes C, Filippi AR, Katz MA, Pereira IJ, Saeed H. COVID-19: Global radiation oncology's targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 155] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 8. | Lara PC, Burgos J, Macias D. Low dose lung radiotherapy for COVID-19 pneumonia. The rationale for a cost-effective anti-inflammatory treatment. Clin Transl Radiat Oncol. 2020;23:27-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 9. | Zaorsky NG, Yu JB, McBride SM, Dess RT, Jackson WC, Mahal BA, Chen R, Choudhury A, Henry A, Syndikus I, Mitin T, Tree A, Kishan AU, Spratt DE. Prostate Cancer Radiation Therapy Recommendations in Response to COVID-19. Adv Radiat Oncol. 2020;5:659-665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 139] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 10. | World Health Organization. Fifty-Eighth World Health Assembly 2005. Available from: https://www.who.int/mediacentre/multimedia/2005/wha58/en/index1.html. |
| 11. | Omotosho A, Emuoyibofarhe J, Adegbola O. ICT in Health care delivery system: A Framework for developing nations. ICT4A. In: Covenant University and Bells University of Technology, Ota, 2011. [DOI] [Full Text] |
| 12. | World Health Organization. Global diffusion of eHealth: Making universal health coverage achievable 2016. Available from: https://www.who.int/goe/publications/global_diffusion/en/. |
| 13. | Fisk M, Rudel D, Roze R. Definitions of Terms in Telehealth. Informatica Medica Slovenica. 2011;16:28-46. |
| 14. | European Coordination Committee of the Radiological. COCIR eHealth TOOLKIT contributing to the Edropean Digital Agenda. Electromedical and Healthcare IT Industry May 2012. Available from: https://cn.bing.com/search?q=https://www.cocir.org/fileadmin/Publications_2012/...&form=IPRV10. |
| 15. | Masic I. E-learning as new method of medical education. Acta Inform Med. 2008;16:102-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Hamilton E, Van Veldhuizen E, Brown A, Brennan S, Sabesan S. Telehealth in radiation oncology at the Townsville Cancer Centre: Service evaluation and patient satisfaction. Clin Transl Radiat Oncol. 2019;15:20-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Nekhlyudov L, Duijts S, Hudson SV, Jones JM, Keogh J, Love B, Lustberg M, Smith KC, Tevaarwerk A, Yu X, Feuerstein M. Addressing the needs of cancer survivors during the COVID-19 pandemic. J Cancer Surviv. 2020;14:601-606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 97] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 18. | Buckstein M, Skubish S, Smith K, Braccia I, Green S, Rosenzweig K. Experiencing the Surge: Report From a Large New York Radiation Oncology Department During the COVID-19 Pandemic. Adv Radiat Oncol. 2020;5:610-616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Jereczek-Fossa BA, Pepa M, Marvaso G, Bruni A, Buglione di Monale E Bastia M, Catalano G, Filippi AR, Franco P, Gambacorta MA, Genovesi D, Iatì G, Magli A, Marafioti L, Meattini I, Merlotti A, Mignogna M, Musio D, Pacelli R, Pergolizzi S, Tombolini V, Trovò M, Ricardi U, Magrini SM, Corvò R, Donato V; AIRO (Italian Association of Radiotherapy and Clinical Oncology). COVID-19 outbreak and cancer radiotherapy disruption in Italy: Survey endorsed by the Italian Association of Radiotherapy and Clinical Oncology (AIRO). Radiother Oncol. 2020;149:89-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 20. | Chan T, Trueger NS, Roland D, Thoma B. Evidence-based medicine in the era of social media: Scholarly engagement through participation and online interaction. CJEM. 2018;20:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Thamman R, Gulati M, Narang A, Utengen A, Mamas MA, Bhatt DL. Twitter-based learning for continuing medical education? Eur Heart J. 2020. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 22. | Birkhoff SD, Cantrell MA, Moriarty H, Lustig R. The Usability and Acceptability of a Patient-Centered Mobile Health Tracking App among a Sample of Adult Radiation Oncology Patients. ANS Adv Nurs Sci. 2018;41:243-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Kessel KA, Vogel MME, Schmidt-Graf F, Combs SE. Mobile Apps in Oncology: A Survey on Health Care Professionals' Attitude toward Telemedicine, mHealth, and Oncological Apps. J Med Internet Res. 2016;18:e312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 24. | Almathami HKY, Win KT, Vlahu-Gjorgievska E. Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients' Homes: Systematic Literature Review. J Med Internet Res. 2020;22:e16407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 407] [Article Influence: 81.4] [Reference Citation Analysis (0)] |
| 25. | Nguyen MH, Bol N, van Weert JCM, Loos EF, Tytgat KMAJ, Geijsen D, Drenth E, Janse M, Smets EMA. Optimising eHealth tools for older patients: Collaborative redesign of a hospital website. Eur J Cancer Care (Engl). 2019;28:e12882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |