Published online Mar 24, 2019. doi: 10.5306/wjco.v10.i3.161
Peer-review started: November 10, 2018
First decision: December 7, 2018
Revised: January 30, 2019
Accepted: February 27, 2019
Article in press: February 27, 2019
Published online: March 24, 2019
Processing time: 133 Days and 14.3 Hours
Plasma cell leukemia (PCL) is diagnosed by the presence of an absolute plasma cell count of > 2 × 109/L or 20% plasma cells in the peripheral blood. Because the incidence of PCL is relatively low, our case report study presents a rare opportunity to describe the clinical and pathological characteristics of this leukemia, as well as different modalities of treatment and outcomes of primary PCL (pPCL).
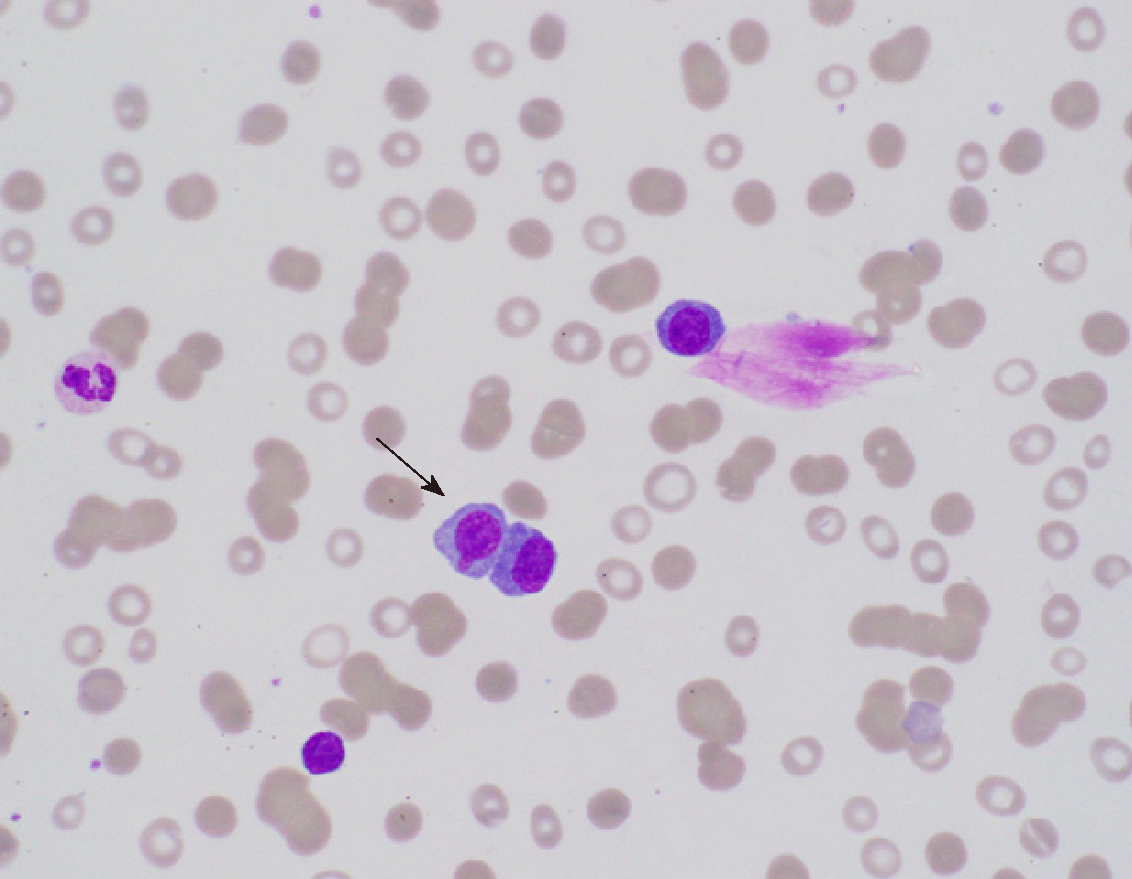
A 56-year-old male with a history of hypertension complained of pain in the left flank area which started four months prior to admission. On admission, his vital signs were stable, and physical examination was completely benign. Laboratory evaluation showed hemoglobin of 5.1 g/dL, white blood cell count of 6.6 cells per cubic millimeter with 16% atypical lymphocytes, and platelet count of 51000 per microliter. Peripheral smear showed more than 10%-15% of plasma cells (Figure 1), and flow cytometry of peripheral blood confirmed PCL with 24% plasma cells CD138+. Bone marrow biopsy demonstrated 80% plasma cells (38+, 138+, 117+, 10-, 19-, 20-, 56-) with 90% cellularity. The Oncology team was consulted, and VCD therapy was started. After completing therapy at 1, 4, 8, and 11 d, the patient was discharged home. The patient was being considered for a bone marrow transplant evaluation within two months of discharge.
PCL is a rare and aggressive form of leukemia with a poor prognosis. Multi-center studies and clinical trials should be conducted to develop accurate criteria for the initial diagnosis and prompt treatment of this disease.
Core tip: Always review a peripheral blood film in all cases of multiple myeloma and be aware of an entity called plasma cell leukemia, a rare and aggressive form of leukemia.
- Citation: Jain AG, Faisal-Uddin M, Khan AK, Wazir M, Shen Q, Manoucheri M. Plasma cell leukemia - one in a million: A case report. World J Clin Oncol 2019; 10(3): 161-165
- URL: https://www.wjgnet.com/2218-4333/full/v10/i3/161.htm
- DOI: https://dx.doi.org/10.5306/wjco.v10.i3.161
Primary plasma cell leukemia (pPCL) is a malignant plasma cell disorder characterized by the presence of 2 × 109/μL peripheral blood clonal plasma cells or > 20% plasma cells in the peripheral blood. It is very rare, accounting for 0.6%-4% of all plasma cell neoplasms, and is reported to occur in < 1 in a million. PCL has a relatively poor prognosis, due to its very aggressive nature involving extramedullary organs, lytic bone lesions, destruction of red blood cells, and bone marrow failure. Treatment includes immunomodulators, proteasome inhibitors, and autologous stem cell transplantation. Outcomes are not promising, however, even after treatment; median survival after rigorous chemotherapy and transplant is not more than three years[1]. It is important to consider PCL as a possible diagnosis as well as multiple myeloma (MM), whenever we encounter the typical constellation of “Hypercalcemia, Renal Failure, Anemia, and Lytic Bone lesions”, and to contemplate the peripheral smear, a basic test, which, in our case study, showed > 20% plasma cells, hence leading to the diagnosis of PCL.
A 56-year-old male with a history of hypertension was referred to the hospital by his primary care physician after a routine, yearly laboratory exam showed abnormal hemoglobin of 5.1 mg/dL.
The patient complained of some pain in the left flank area, which started around four months prior to admission.
He denied any history of smoking and did not have any significant family history.
On admission, his vital signs were stable and physical exam was completely benign.
His laboratory evaluation revealed hemoglobin of 5.1 mg/dL, white blood cell count 6.6 × 109/μL with 16% atypical lymphocytes, and platelet count of 51000/μL. Chemistries were significant for a sodium of 125 meq/L, creatinine of 2.79 mg/dL, calcium of 8.3 mg/dL, and normal liver enzymes with a total bilirubin of 3.1 mg/dL. Total protein was 15.3 g/dL.
A Computed tomography (CT) scan was ordered to evaluate the left flank pain, which showed a lytic lesion at T11 (11th thoracic vertebra), right anterior 7th rib with a pathological fracture, and multiple small lucencies in the vertebrae.
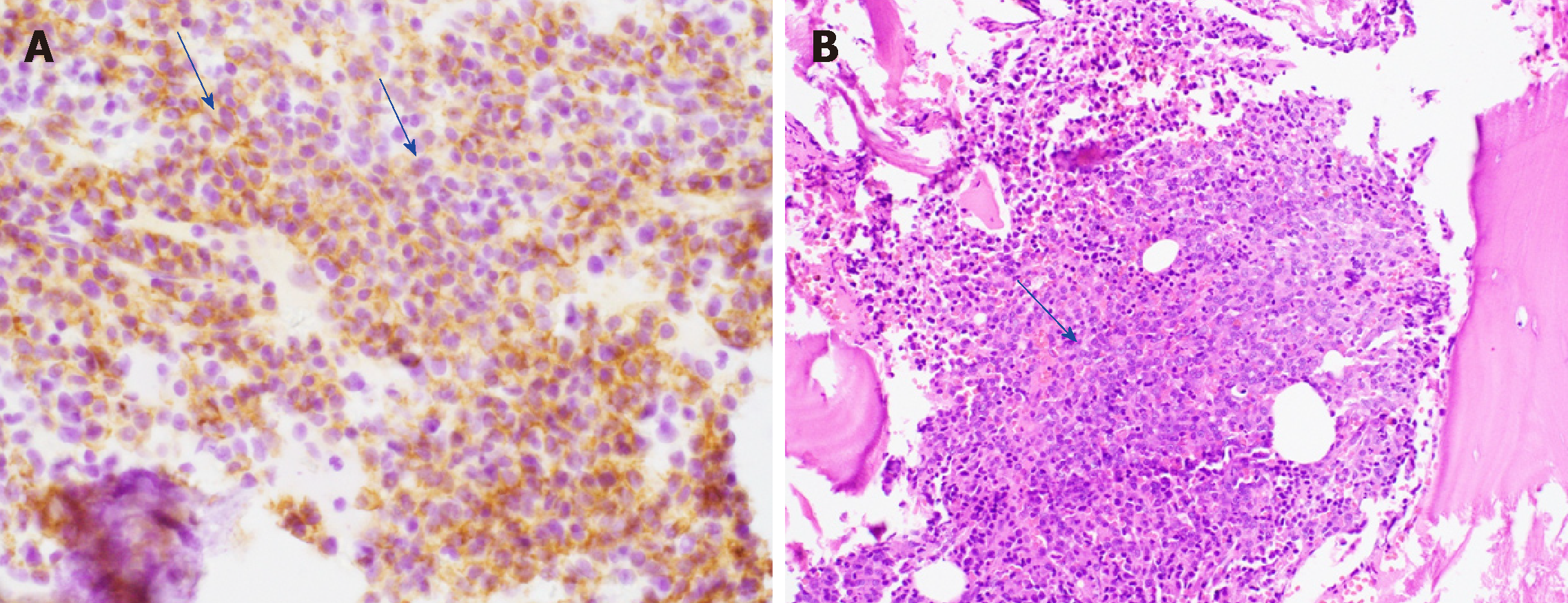
Peripheral smear showed more than 10%-15% plasma cells (Figure 1), and flow cytometry of peripheral blood confirmed PCL with 24% plasma cells (CD138+). Serum protein electrophoresis showed a kappa/lambda ratio of 43 and a monoclonal spike of 8.44 g/dL in the IgG kappa region on immunofixation. Beta-2 microglobulin was also high at 19 μg/mL. A 24-h urine collection showed a total protein of 1557 mg and urine protein electrophoresis (UPEP) showed two spikes of 15 g/dL (IgG kappa) and 2 g/dL (free kappa). Bone marrow biopsy (Figure 2A and B) demonstrated 80% plasma cells (38+, 138+, 117+, 10-, 19-, 20-, 56-) with 90% cellularity. Fluorescence in situ hybridization (FISH) and chromosome analysis showed 13q deletion among many other aberrancies.
pPCL.
VCD therapy was started [cytoxan (750 mg/m2), velcade (0.7 mg/m2 on day 1, 4, 8, 11) with dexamethasone (40 mg)]. The patient received a total of five units of blood transfused during his 15-d hospital stay. After completing therapy at 1, 4, 8, and 11 days, the patient was discharged home.
The patient responded well to chemotherapy and on discharge he was being considered for bone marrow transplant evaluation within two months.
PCL is established by the presence of > 20% circulating plasma cells or an absolute plasma cell count > 2 × 109/L on peripheral smear. It is a very uncommon and aggressive form of monoclonal gammopathy characterized by a poor prognosis with a rapidly fatal outcome. Complications usually lead to death within the first few months of diagnosis. Outcome is thought to be poor because of the absence of effective treatment for this condition[1]. PCL is classified as “primary” (occurring de novo), or “secondary” (occurring in patients with MM).
There are a few differences between these two disease processes. Patients with PCL are usually younger (aged 50-59 years). PCL has a predisposition to develop malignant plasma cells, which circulate in peripheral blood and lead to extramedullary spread involving the liver, spleen, lymph nodes, pleura, peritoneum, and less often the bone, resulting in lytic lesions. The extramedullary spread is explained by negative CD56, a cell adhesion molecule which anchors plasma cells to the bone marrow stroma in contrast to MM, where most of the plasma cell population is found in bone marrow[2]. Hypercalcemia, low platelet count, and destruction of erythrocytes is found in both diseases, but it is more pronounced in PCL than in MM. PCL differs in biology compared to MM with more immature cells in the bone marrow. Most PCL patients have abnormal karyotypes. The FISH probes should be directed against genetic abnormalities, such as del(17p13), del(13q), del(1p21), and (1q21) amplification, and chromosome 14 abnormalities, such as t(11;14), t(4;14), t(14;20) and t(14;16). About 87% of the PCL cases can be attributed to IGH (14q32) translocation, which is hence the most common mutation, followed by t(11;14), which accounts for 25%-65%. In our patient, however, 13q deletion was observed, which is seen in < 20% of patients[3,4]. Plasma cell markers, which can be identified in PCL on immunophenotyping, include CD38 and CD138, which were both present in our patient. Flow cytometry should be performed on peripheral blood to confirm the presence of plasma cells that typically have immunophenotypes of CD138+, CD38+, CD19–, and CD45+/–. Our finding of negative expression of CD10, CD19, CD20, CD56 was consistent with previously published cases[5,6].
Patients having pPCL must undergo a detailed history and physical examination. A comprehensive laboratory evaluation of their blood should be performed, including a complete blood count with differential, peripheral blood smear, electrolyte panel, urea and creatinine levels, liver enzymes, bilirubin, lactate dehydrogenase, uric acid, β2 microglobulin, albumin, serum protein electrophoresis, and serum free light chain analysis. Chest X-ray along with whole body imaging with either MRI or CT should be performed to look for metastasis. Sometimes 18F-FDG PET/CT imaging to look for both lytic bone lesions and extramedullary plasmacytomas is necessary. A 24-h urine collection for electrophoresis and total protein assessment should also be obtained. Finally, it is imperative to perform a bone marrow biopsy and aspiration to assess morphology, proliferation rate, immunophenotyping, and cytogenetic analysis by FISH[7].
Managing patients with PCL requires an intensive risk-adapted approach. Induction therapy with novel triplet therapy using immunomodulators and proteasome inhibitors such as VRd (bortezomib, lenalidomide, and dexamethasone) or KRd (carfilzomib, lenalidomide, and dexamethasone), is usually a satisfactory choice. In some patients with pPCL who have an aggressive form of disease, more aggressive combination regimen, such as VDT-PACE (bortezomib, dexamethasone, thalidomide or lenalidomide, cisplatin, doxorubicin, cyclophosphamide, and etoposide) or HyperCVAD (High dose Cyclophosphamide, vincristine, adriamycin and thalidomide or lenalidomide) should be used, because cyclophosphamide and doxorubicin are particularly effective in proliferative disease. For elderly patients who may not be able to tolerate such an intense regimen, CyBorD (cyclophosphamide, bortezomib, and dexamethasone) or PAD (bortezomib, doxorubicin, and dexa-methasone) can be used as a milder alternative[8].
After induction therapy, autologous stem cell transplant is recommended (for transplant-eligible pPCL patients) to achieve prolonged disease control. Standard antiviral and bacterial prophylaxis should be used mainly because the patients are immunocompromised. The patients may also develop tumor lysis syndrome, so appropriate prophylaxis with allopurinol and appropriate hydration may be indicated. Adequate antithrombotic prophylaxis as well as platelet, red blood cell monitoring, and replacement is also crucial. Finally, although osteolytic bone lesions are less common in pPCL than in MM, all patients with pPCL should be started on bisphosphonate therapy along with vitamin D[9].
Median survival has been estimated to be around 6-7 years with conventional chemotherapy. With autologous or allogeneic stem cell transplantation, survival has shown improvement to around three years. Less than 10% patients survive for more than five years.
PCL is the most aggressive variant of monoclonal gammopathy and is a rare form of clonal plasma cell dyscrasia. Around 60%-70% PCL are primary and 30%-40% are secondary. Median age of diagnosis is 52 to 65 years which is ten years younger than the usual myeloma population. PCL and MM are distinct clinico-pathologic entities with different treatment options and most important, different prognoses. Multi-center studies and clinical trials should be conducted to develop accurate criteria for the initial diagnosis and prompt treatment of this disease.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Hosseini M, Ali I S- Editor: Dou Y L- Editor: A E- Editor: Wu YXJ
| 1. | International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol. 2003;121:749-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1610] [Cited by in RCA: 1513] [Article Influence: 68.8] [Reference Citation Analysis (1)] |
| 2. | Bladé J, Kyle RA. Nonsecretory myeloma, immunoglobulin D myeloma, and plasma cell leukemia. Hematol Oncol Clin North Am. 1999;13:1259-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 129] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Tiedemann RE, Gonzalez-Paz N, Kyle RA, Santana-Davila R, Price-Troska T, Van Wier SA, Chng WJ, Ketterling RP, Gertz MA, Henderson K, Greipp PR, Dispenzieri A, Lacy MQ, Rajkumar SV, Bergsagel PL, Stewart AK, Fonseca R. Genetic aberrations and survival in plasma cell leukemia. Leukemia. 2008;22:1044-1052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 266] [Cited by in RCA: 226] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 4. | Noel P, Kyle RA. Plasma cell leukemia: an evaluation of response to therapy. Am J Med. 1987;83:1062-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 117] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Kraj M, Kopeć-Szlęzak J, Pogłód R, Kruk B. Flow cytometric immunophenotypic characteristics of 36 cases of plasma cell leukemia. Leuk Res. 2011;35:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | García-Sanz R, Orfão A, González M, Tabernero MD, Bladé J, Moro MJ, Fernández-Calvo J, Sanz MA, Pérez-Simón JA, Rasillo A, Miguel JF. Primary plasma cell leukemia: clinical, immunophenotypic, DNA ploidy, and cytogenetic characteristics. Blood. 1999;93:1032-1037. [PubMed] |
| 7. | Fernández de Larrea C, Kyle RA, Durie BG, Ludwig H, Usmani S, Vesole DH, Hajek R, San Miguel JF, Sezer O, Sonneveld P, Kumar SK, Mahindra A, Comenzo R, Palumbo A, Mazumber A, Anderson KC, Richardson PG, Badros AZ, Caers J, Cavo M, LeLeu X, Dimopoulos MA, Chim CS, Schots R, Noeul A, Fantl D, Mellqvist UH, Landgren O, Chanan-Khan A, Moreau P, Fonseca R, Merlini G, Lahuerta JJ, Bladé J, Orlowski RZ, Shah JJ; International Myeloma Working Group. Plasma cell leukemia: consensus statement on diagnostic requirements, response criteria and treatment recommendations by the International Myeloma Working Group. Leukemia. 2013;27:780-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 260] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 8. | D'Arena G, Valentini CG, Pietrantuono G, Guariglia R, Martorelli MC, Mansueto G, Villani O, Onofrillo D, Falcone A, Specchia G, Semenzato G, Di Renzo N, Mastrullo L, Venditti A, Ferrara F, Palumbo A, Pagano L, Musto P. Frontline chemotherapy with bortezomib-containing combinations improves response rate and survival in primary plasma cell leukemia: a retrospective study from GIMEMA Multiple Myeloma Working Party. Ann Oncol. 2012;23:1499-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Avet-Loiseau H, Roussel M, Campion L, Leleu X, Marit G, Jardel H, Dib M, Decaux O, Lamy T, Tiab M, Cony-Makhoul P, Banos A, Lepeu G, Lifermann F, Macro M, Kolb B, Hulin C, Caillot D, Traulle C, Mathiot C, Royer B. Cytogenetic and therapeutic characterization of primary plasma cell leukemia: the IFM experience. Leukemia. 2012;26:158-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |