Copyright
©2014 Baishideng Publishing Group Inc.
World J Clin Oncol. Oct 10, 2014; 5(4): 753-763
Published online Oct 10, 2014. doi: 10.5306/wjco.v5.i4.753
Published online Oct 10, 2014. doi: 10.5306/wjco.v5.i4.753
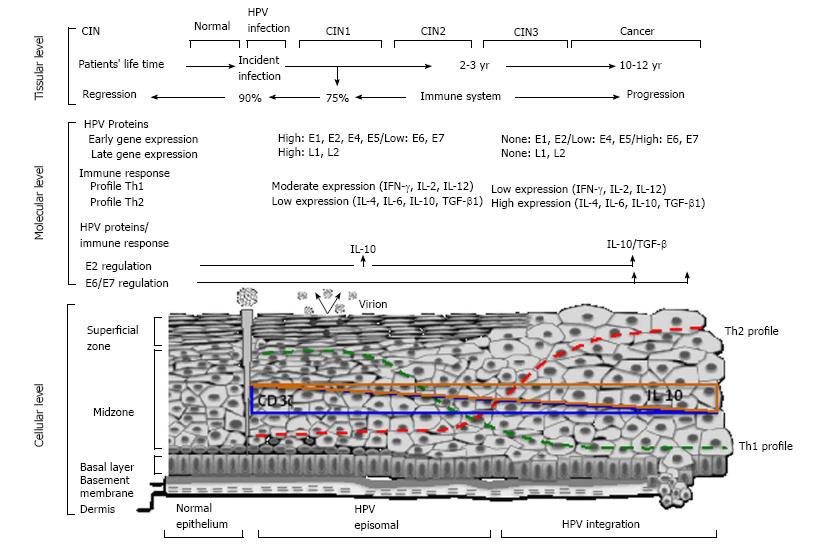
Figure 1 Systematic representation for cervical human Papillomavirus-carcinogenesis: Role of immune response.
The main event is the human Papillomavirus (HPV) infection of epithelial cells in the basal membrane. HPV can turn into episomal bodies, which will be in charge of, on one part, producing infective virions and, on the other, integrating into the genome of epithelial cells. Upon infection, an average of 2-3 yr are necessary to develop of CIN 1/2 and/or high-grade (CIN3), often characterized by the integration of the viral genome, one key event for disease progression as this frequently triggers the deregulation of the E6 and E7 oncogenes, major chromosomal alterations and cellular immortalization[10]. The immune system plays a key role during HPV-carcinogenesis since the majority of high-risk HPV infections (90%), as well as most of low-grade lesions (75%) regress[5,6]. Due to this, and the long periods of time between viral infection and the progression to invasive disease, the fail of immune response is necessary to cancer development. Since the beginning of HPV infection, there are augment in the immunosuppressive cytokine IL-10 at the cervical level, and this increased according with the grade of lesion, being the highest concentration at cancer stage[25]. A shift to Th2-type cytokines in the course of development of cervical cancer is reflected with an increased serum concentration of Th2-type cytokines[22,23]. Inversely, the presence of CD3zeta chain in the tumor infiltrating T-lymphocytes, decreases as the grade of lesion progress, this is due to a reduction of Th1-type cytokines at the late stages of the disease[24]. These are key elements for the impairment of immune responses that allows HPV-persistence, viral integration into the genome epithelial cells, and cellular transformation and immortalization.
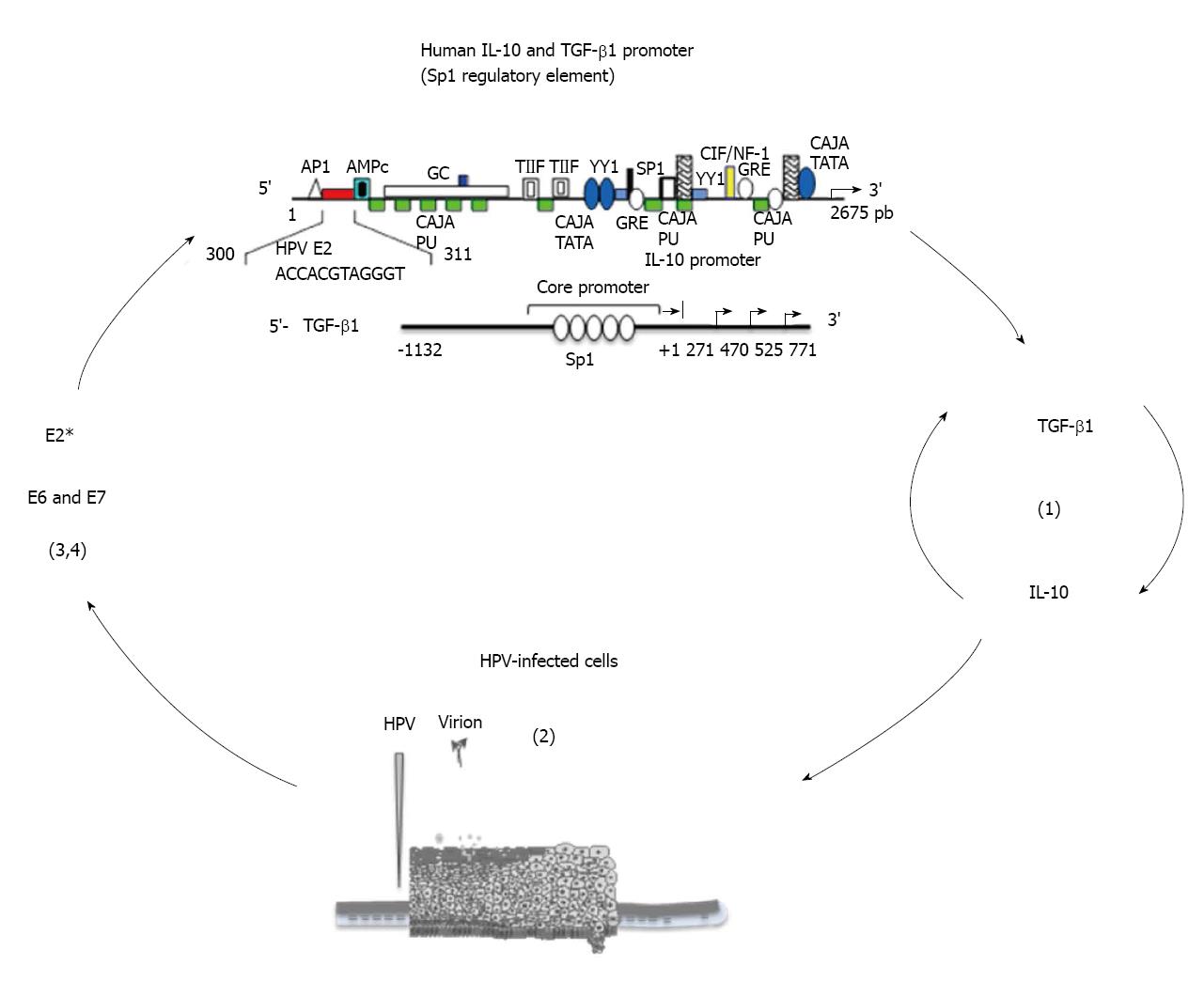
Figure 2 Vicious cycle between Interleukin-10, transforming growth factor-β1, and human papillomavirus.
(1) IL-10 enhances TGF-β1 expression and vice-versa[76]; (2) IL-10 induces transcription of HPV-16 E6 and E7[56]; (3) HPV E6 and E7 proteins induce activation of TGF-β1 promoter through Sp1 recognition sequence[21]; (4) Human gene IL-10 regulatory regions posses Sp1 regulatory elements, which suggests that HPV E6 and E7 proteins may bind to IL-10 regulatory region to activate IL-10 gene transcription, just as HPV E2* protein does[74], and may induce IL-10 expression in HPV-transformed cervical cells. HPV can enhance the expression of cytokines TGF-β1 or IL-10, which inhibit T cell functions and augment viral proteins, contributing to the persistence of HPV infection and progression of HPV-related cervix lesions to cervical cancer. The production and activity of these two cytokines, IL-10 and TGF- β1, are interrelated and likely involve a positive feedback loop in which IL-10 enhances the expression of TGF-β1 and vice-versa[76]. In fact, IL-10 not only enhances the production of TGF-β1 but also controls the ability of target cells to respond to TGF-β1. This involves the IL-10-mediated restoration of the expression of TGF-β1 receptor 2 in recently activated T cells, which usually down-regulate this receptor and become desensitized to the inhibitory effects of TGF-β1. Conversely, TGF-β1 can promote the production of IL-10[76]. IL-10: Interleukin-10; TGF-β1: Transforming growth factor-β1; HPV: Human papillomavirus.
- Citation: Torres-Poveda K, Bahena-Román M, Madrid-González C, Burguete-García AI, Bermúdez-Morales VH, Peralta-Zaragoza O, Madrid-Marina V. Role of IL-10 and TGF-β1 in local immunosuppression in HPV-associated cervical neoplasia. World J Clin Oncol 2014; 5(4): 753-763
- URL: https://www.wjgnet.com/2218-4333/full/v5/i4/753.htm
- DOI: https://dx.doi.org/10.5306/wjco.v5.i4.753