Copyright
©2014 Baishideng Publishing Group Inc.
World J Clin Oncol. Aug 10, 2014; 5(3): 478-494
Published online Aug 10, 2014. doi: 10.5306/wjco.v5.i3.478
Published online Aug 10, 2014. doi: 10.5306/wjco.v5.i3.478
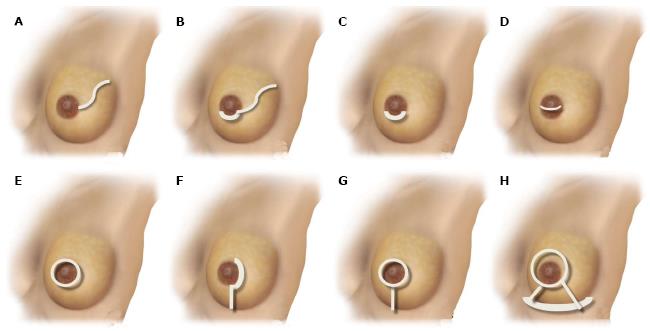
Figure 1 Schematic representation of nipple-sparing mastectomy incisions.
A: Radial lateral incision; B: Periareolar with lateral extension; C: Hemi-periareolar (superior and inferior); D: Transareolar; E: Circumareolar (periareolar total); F: Periareolar with vertical extension; G: Circumareolar (periareolar total) with vertical extension; H: Wise-pattern mastectomy.
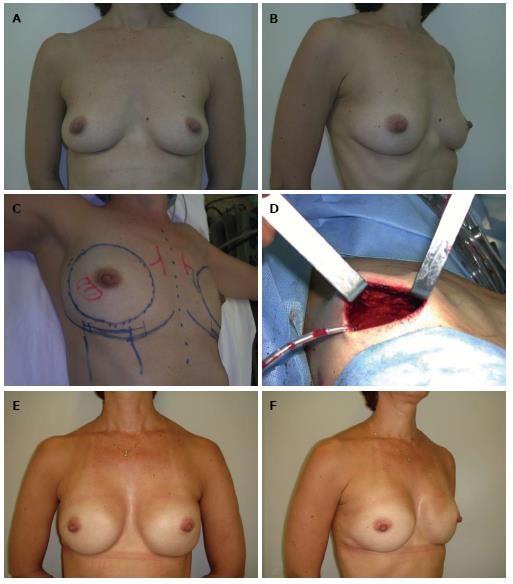
Figure 2 Nipple-sparing mastectomy/inframammary incision.
A and B: A 44-year-old patient with an invasive ductal carcinoma in the right breast (1.4 cm) and a familial history of breast cancer; C and D: Nipple-sparing mastectomy preoperative planning was based on a bilateral through a inframammary approach and immediate reconstruction with biodimensional implant-expander (Allergan 150 SH, 285 cm3). Intraoperative frozen sections demonstrated nipple-areola complex free of tumor; E and F: Five years postoperative appearance with a very good outcome.
Figure 3 Nipple-sparing mastectomy/superior periareolar incision.
A and B: A 52-year-old patient with in situ multifocal carcinoma in the right breast (4.8 cm) and atypical hyperplasia in the left breast; C and D: The patient underwent a bilateral nipple-sparing mastectomy mastectomy through a superior periareolar incision and sentinel lymph node biopsy; E and F: The oncological procedure was immediately followed by a bilateral pedicled transverse rectus abdominis myocutaneous flap reconstruction. Four years postoperative appearance with a very good outcome.
Figure 4 Nipple-sparing mastectomy/superior periareolar incision.
A and B: A 56-year-old patient with invasive ductal carcinoma of the left breast (2.3 cm); C and D: The patient underwent a left nipple-sparing mastectomy mastectomy with a superior periareolar incision and sentinel lymph node biopsy. The oncological procedure was immediately followed by a free deep inferior epigastric perforator flap reconstruction; E and F: Five years postoperative appearance with a very good outcome. The superior periareolar incision was converted to a total circumareolar incision in order to achieve a better symmetry during the second stage of reconstruction.
Figure 5 Local complications following nipple-sparing mastectomy.
A: Inferior periareolar incision with partial wound dehiscence; B: Superior periareolar incision with partial nipple areola complex necrosis; C and D: Wise pattern incision with partial mastectomy and nipple areola complex necrosis; E and F: Inframammary incision with partial mastectomy necrosis.
- Citation: Munhoz AM, Montag E, Filassi JR, Gemperli R. Immediate nipple-areola-sparing mastectomy reconstruction: An update on oncological and reconstruction techniques. World J Clin Oncol 2014; 5(3): 478-494
- URL: https://www.wjgnet.com/2218-4333/full/v5/i3/478.htm
- DOI: https://dx.doi.org/10.5306/wjco.v5.i3.478