Copyright
©The Author(s) 2025.
World J Clin Oncol. Aug 24, 2025; 16(8): 109217
Published online Aug 24, 2025. doi: 10.5306/wjco.v16.i8.109217
Published online Aug 24, 2025. doi: 10.5306/wjco.v16.i8.109217
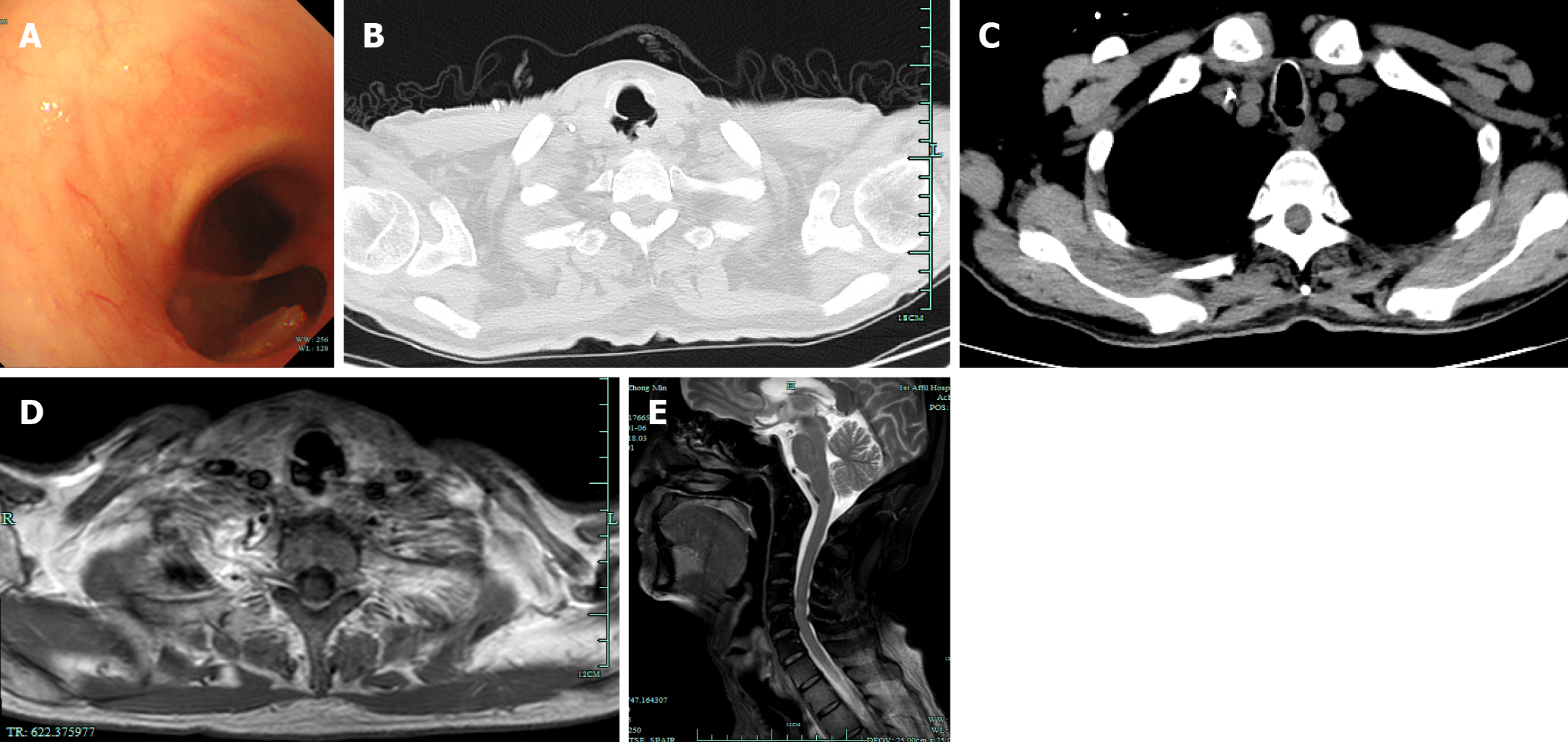
Figure 1 Tracheoesophageal fistula in the cervical trachea and esophagus.
A: Flexible bronchoscopy examination showed a tracheoesophageal fistula (TEF) 0.8 cm from the glottis and about 1.5 cm in length; C and B: TEF was found on computed tomography; D and E: TEF was found on magnetic resonance imaging.
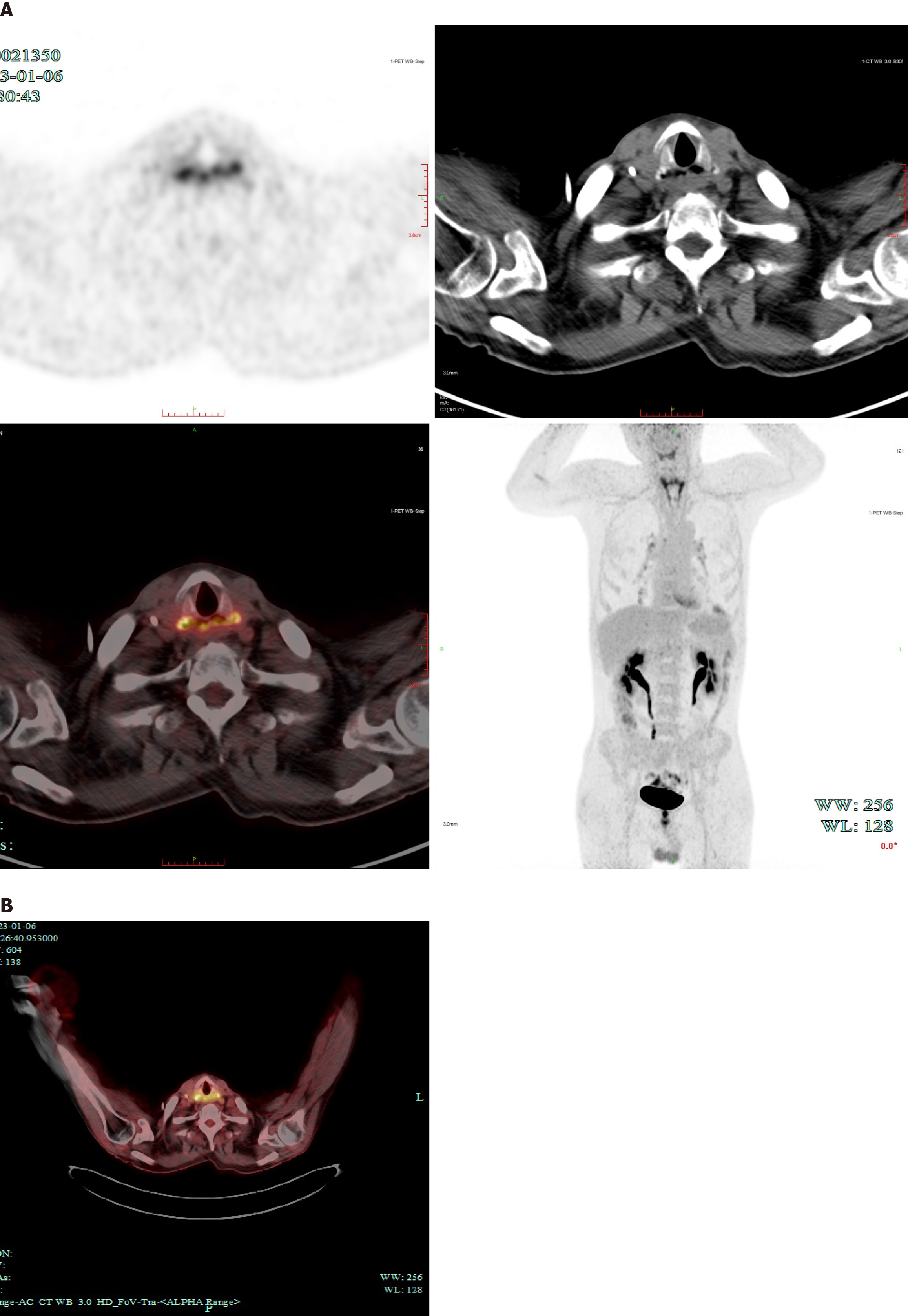
Figure 2 Positron emission tomography/computed tomography showed potential tumor recurrence.
A: Imaging analysis showed increased uptake in the anterior esophageal wall and excluded systemic metastasis; B: Increased uptake in the anterior esophageal wall.
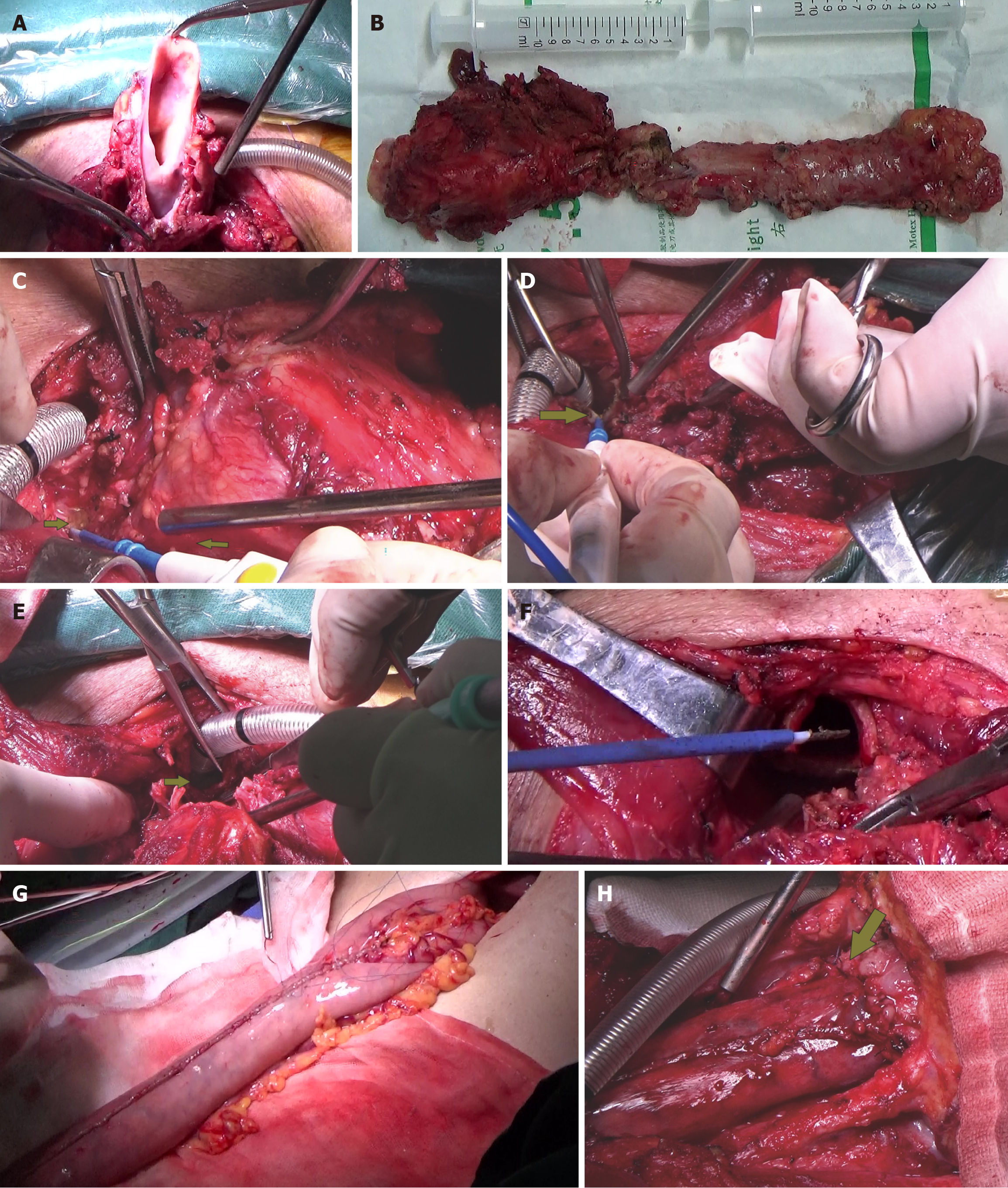
Figure 3 Pharyngolaryngoesophagectomy, left thyroidectomy, and removal of about 5 cm (at the second thoracic spine level) of the tracheal membrane.
A: Total pharyngolaryngectomy; B: Total pharyngolaryngoesophagectomy; C: Left thyroidectomy (the arrow near the suction tube indicates the left thyroid); D: Resection of the invaded tracheal membrane; E and F: View after removal of the invaded tracheal membrane; G: Preparation of the gastric tube; H: The gastric tube was sutured to the base of the tongue (the arrow indicates the base of the tongue).
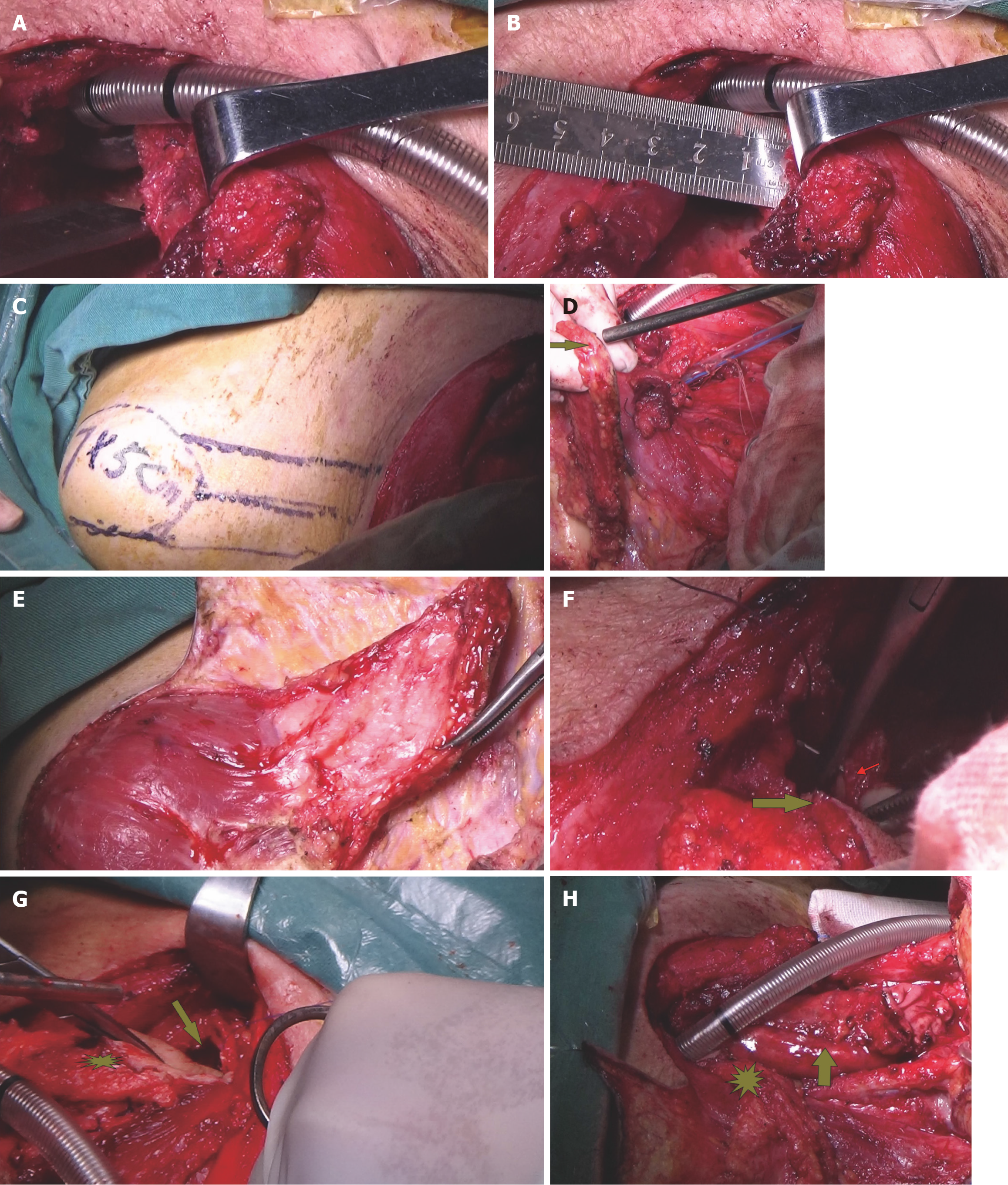
Figure 4 The lower residual tracheal defect was repaired with a supraclavicular artery island flap.
A and B: Size of the defect; C: A 7 cm × 5 cm SCAIF was harvested from the left shoulder; D: Examination of the blood supply of the SCAIF; E: Preparation of the SCAIF; F and G: The SCAIF was sutured to the tracheal membrane (F) arrow: SCAIF; small red arrow: Tracheal membrane, (G) asterisk: SCAIF; arrow: Thoracic tracheal cavity; H: Repair of the SCAIF (asterisk) and gastric tube (arrow).
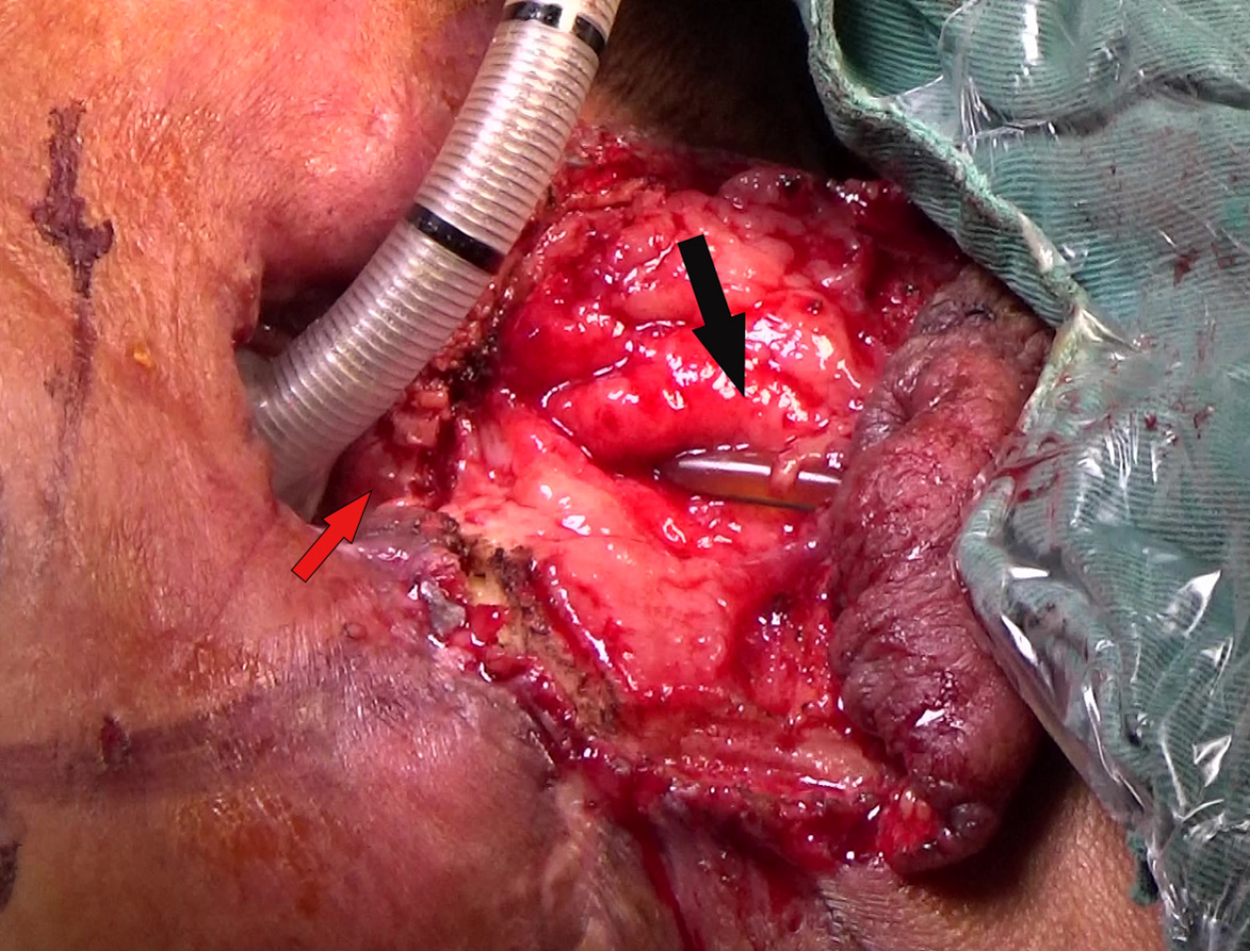
Figure 5 A 3 cm × 5 cm circumferential defect was found in the neck after partial gastric conduit necrosis.
Neck (black arrow: Defect; red arrow: Surviving SCAIF).
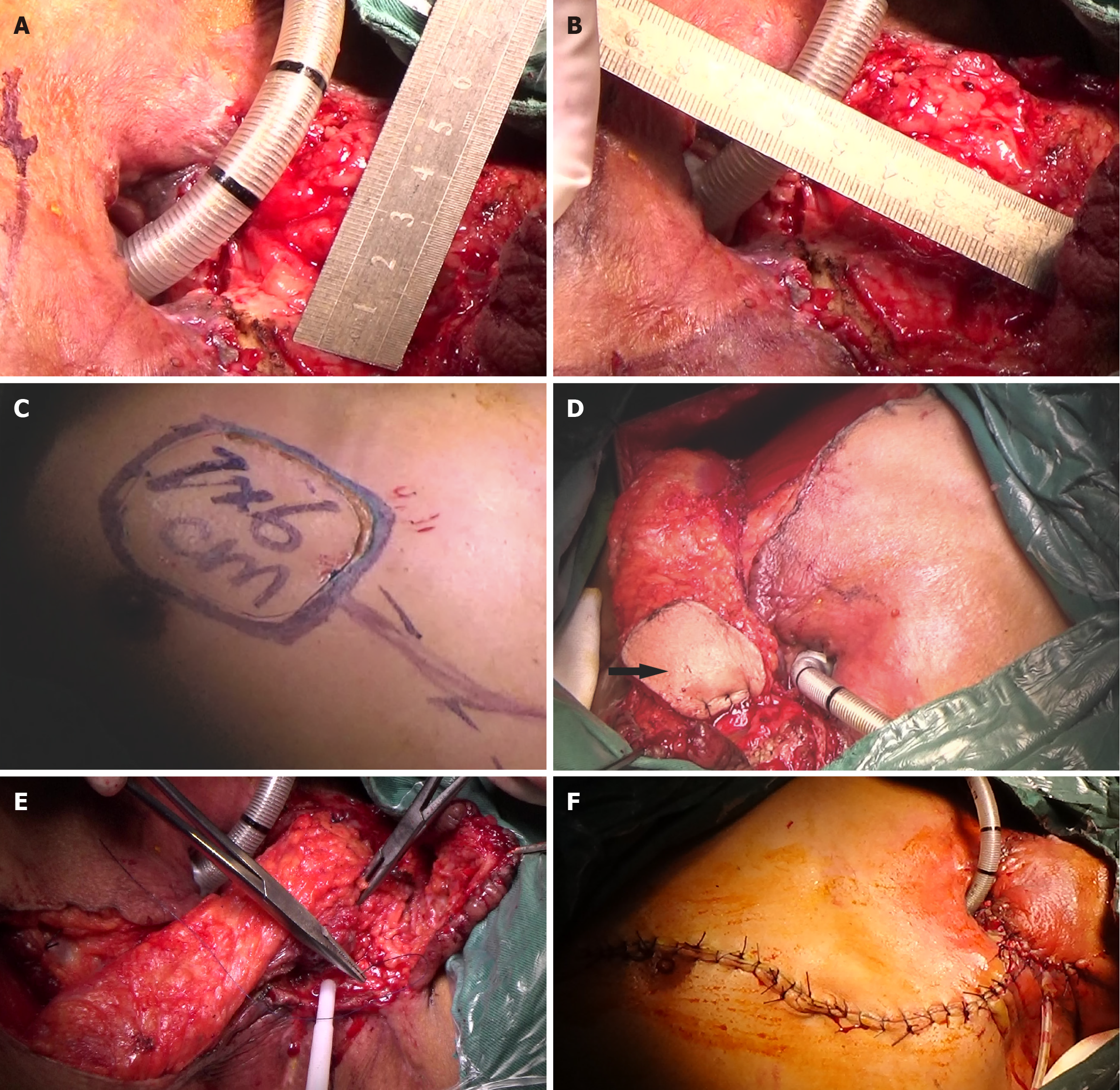
Figure 6 A 7 cm × 6 cm pectoralis major myocutaneous flap (PMMF) was used to repair the defect caused by partial gastric conduit necrosis in the neck.
A and B: The 3 cm × 5 cm circumferential defect; C: The 7 cm × 6 cm pectoralis major myocutaneous flap (PMMF); D: The U-shaped PMMF (black arrow); E and F: The circumferential defect was repaired with the U-shaped PMMF.
Figure 7 The patient recovered after treatment and during the follow-up, there was no recurrence or metastasis observed in this patient.
A: The patient recovered; B: Tracheostomy stoma after supraclavicular artery island flap repair after 112 days in hospital; C and D: At follow-up on March 20, 2025 (follow-up period, 27 months), the patient had no recurrence or metastasis, skin flaps were successful, and the patient could consume a semi-fluid diet and had gained significant weight; D: Stoma.
- Citation: Waheed HZ, Huang CQ, Bao YY, Chen Z, Chen HC, Cao ZZ, Zhong JT, Ye P, Fu SQ, Zhou SH. Successful cure of a patient with tracheoesophageal fistula in cervical esophageal cancer: A case report and review of literature. World J Clin Oncol 2025; 16(8): 109217
- URL: https://www.wjgnet.com/2218-4333/full/v16/i8/109217.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i8.109217