Copyright
©The Author(s) 2020.
World J Clin Oncol. Aug 24, 2020; 11(8): 655-672
Published online Aug 24, 2020. doi: 10.5306/wjco.v11.i8.655
Published online Aug 24, 2020. doi: 10.5306/wjco.v11.i8.655
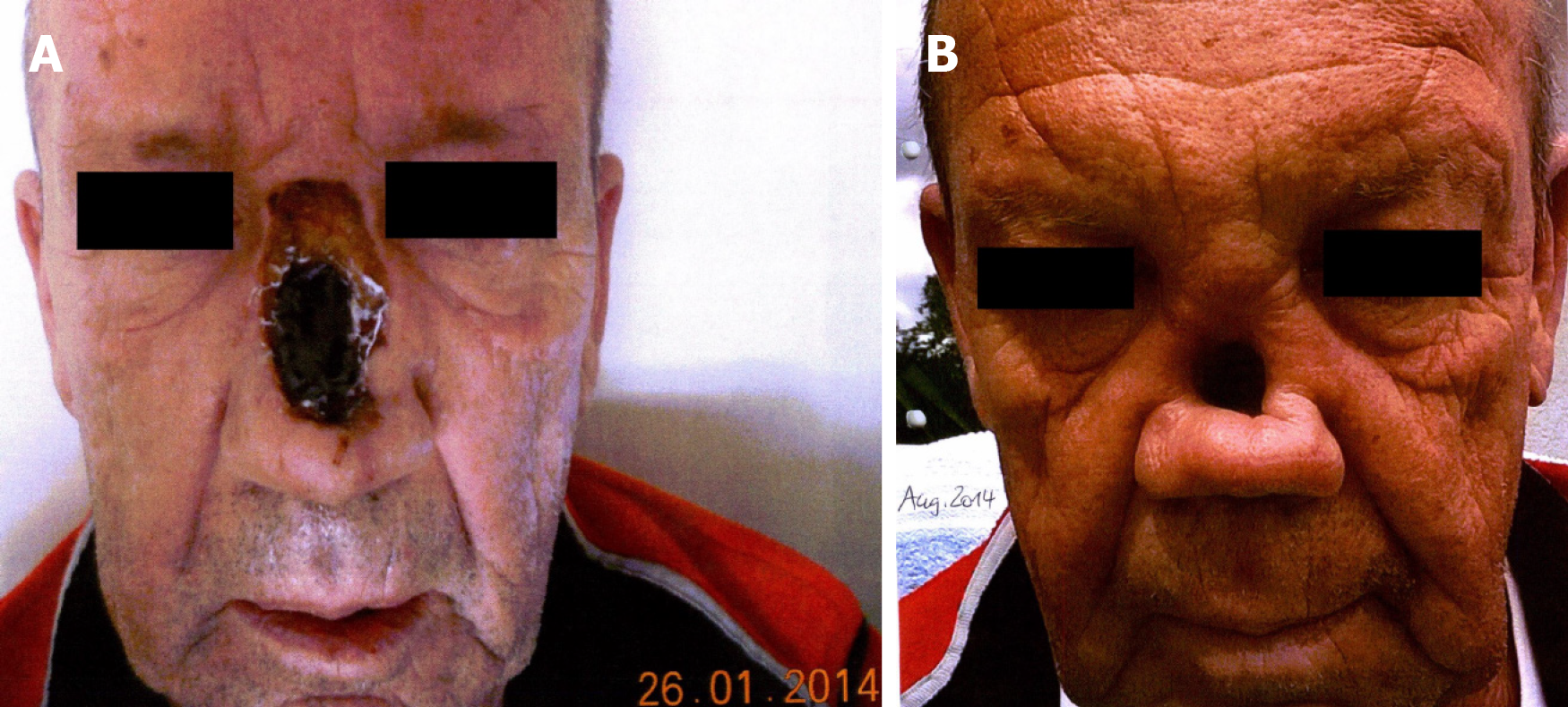
Figure 1 Patient’s images prior to proton beam therapy.
A: Partial nasal ablation in January 2014 at the initial diagnosis of a nasal squamous cell carcinoma; B: Distinct thickening in the nasal bridge, indicating local recurrence in August 2014.
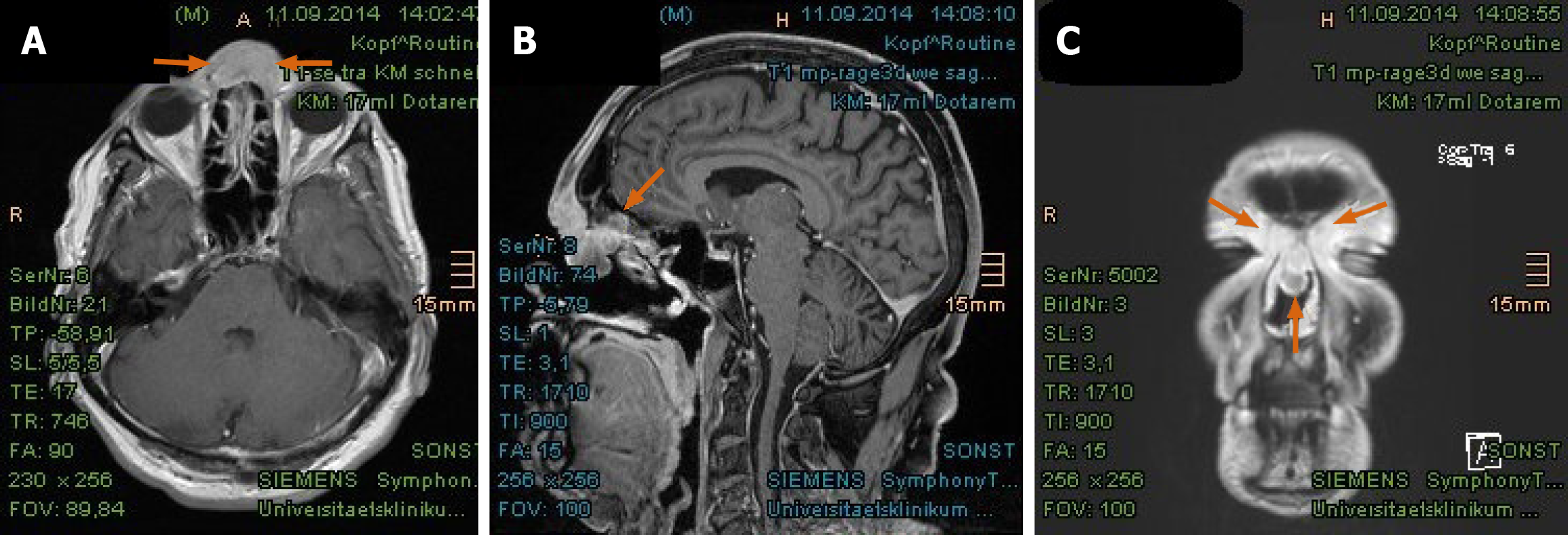
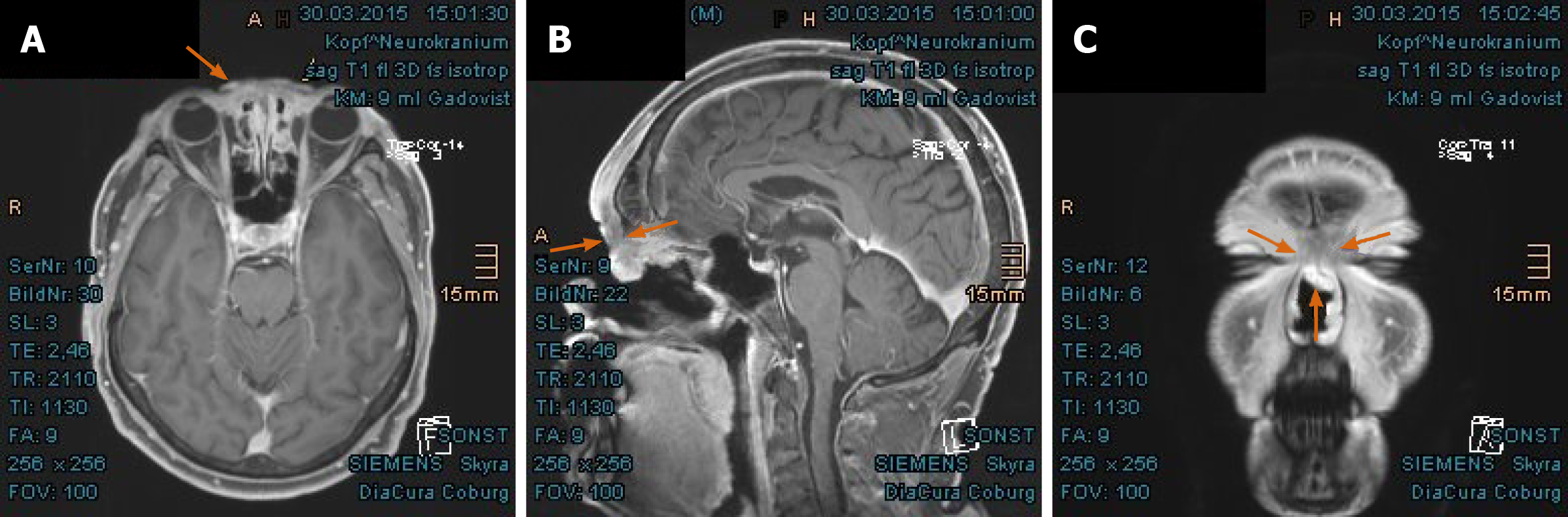
Figure 2 Magnetic resonance imaging from September 2014 revealed tumorous enhancement in the nasal bridge abutting frontal sinus and skull base.
A: Axial plane; B: Sagittal plane; C: Coronal plane. Local recurrence marked with arrows.
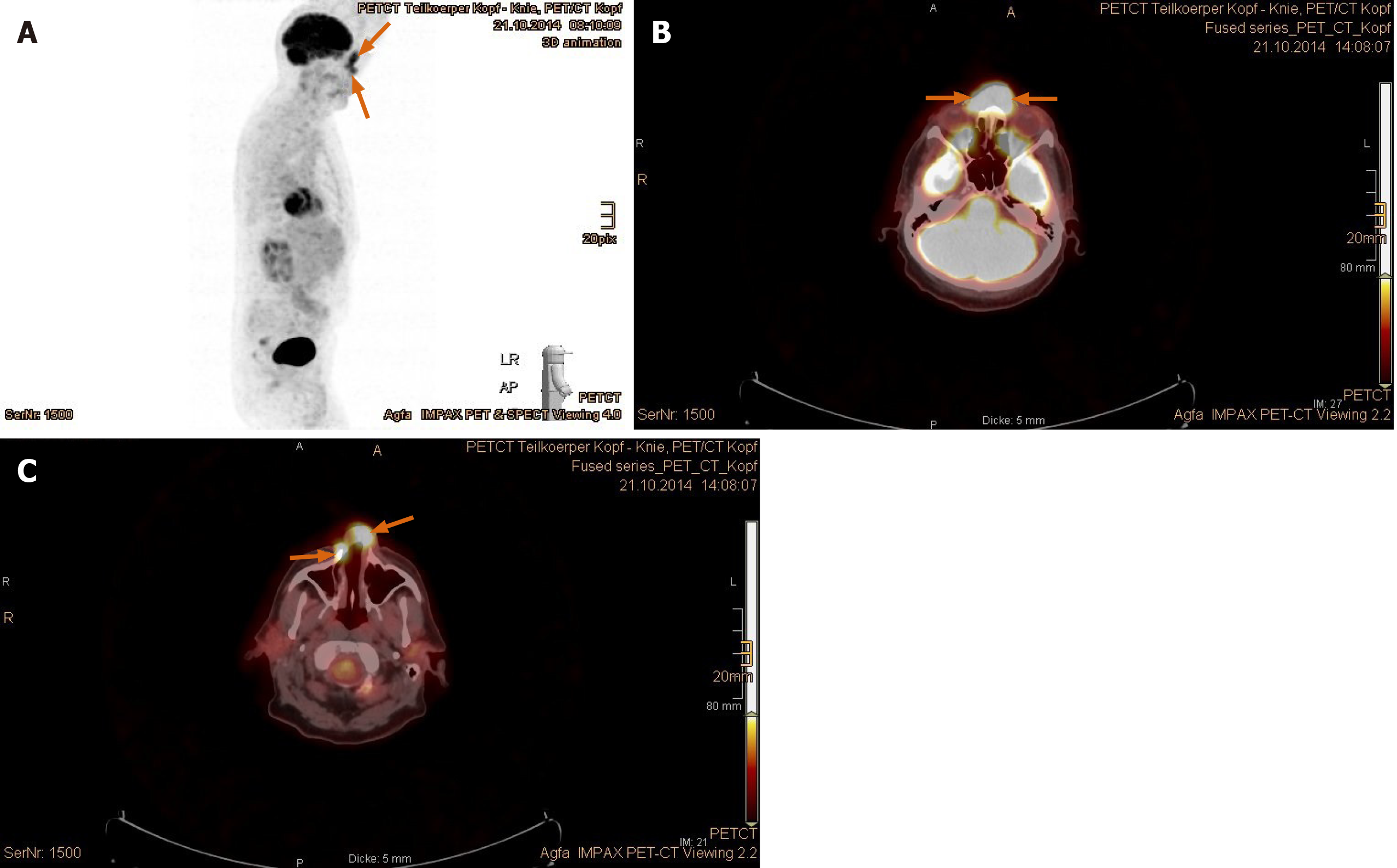
Figure 3 Positron emission tomography with 2-deoxy-2-fluorine-18-fluoro-D-glucose/computed tomography validated tumor recurrence in the nasal bridge and left parotid gland.
A: Positron emission tomography overview image; B: Increased uptake in the nasal bridge; C: Fluoro-D-glucose-avid tumor in the nostrils (recurrent tumor marked with arrows).
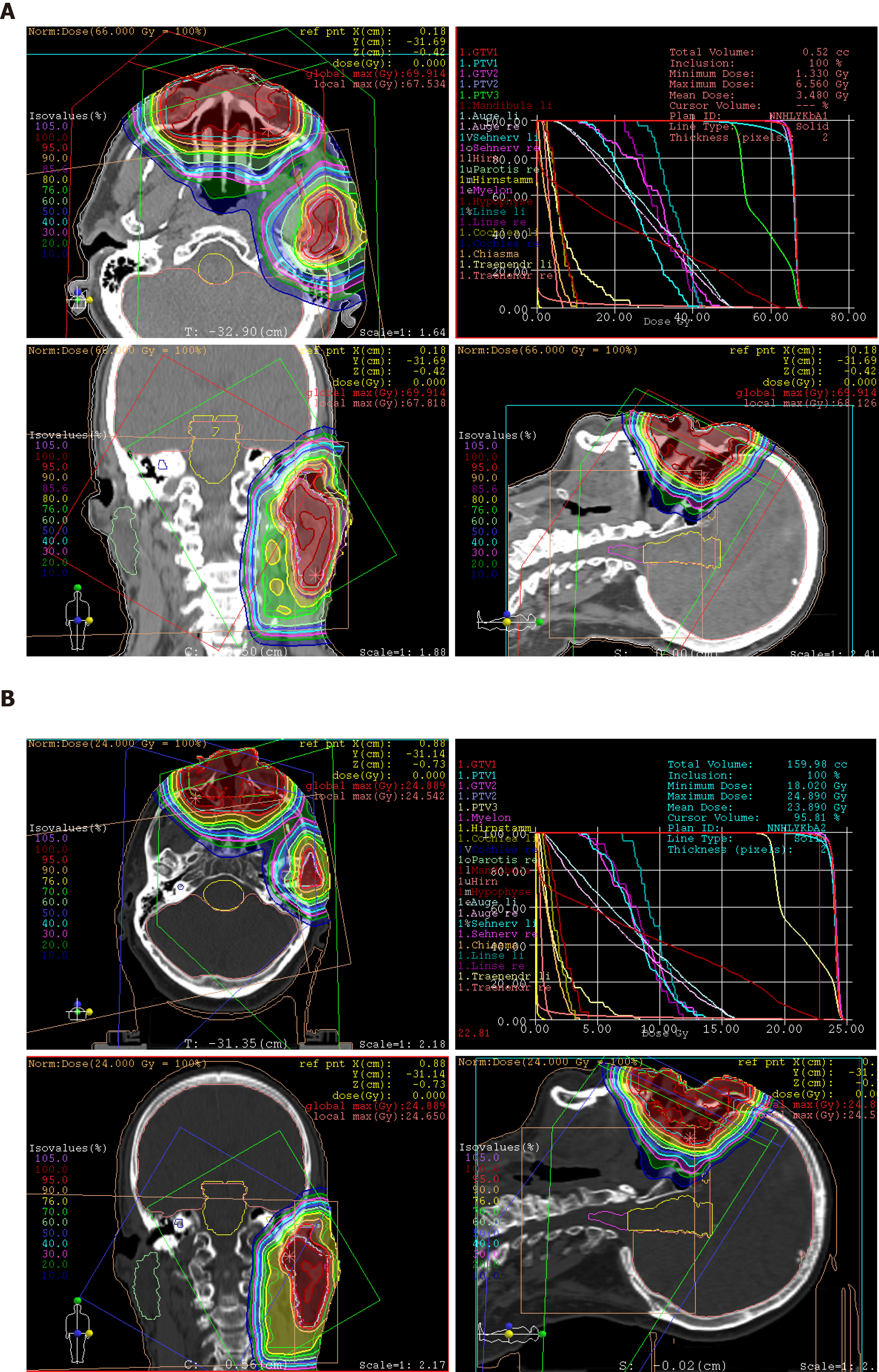
Figure 4 Treatment plans of proton beam therapy with isodose distributions in all three planes and dose-volume-histogram.
A: The first section, until the 28th fraction; B: Plan adaptation, with more eye sparing for the remaining 16 fractions.
Figure 5 Significant shrinkage of recurrent tumor in the nasal bridge with mucosal swelling in the first follow-up at 3 mo after proton beam therapy.
A: Unequivocal reduction of tumor thickening in the nasal bridge, presented in axial plane; B: Pronounced tumor regression abutting the frontal skull base, presented in sagittal plane; C: Coronal presentation of shrinking tumor in the nasal bridge. Local recurrence marked with arrows.
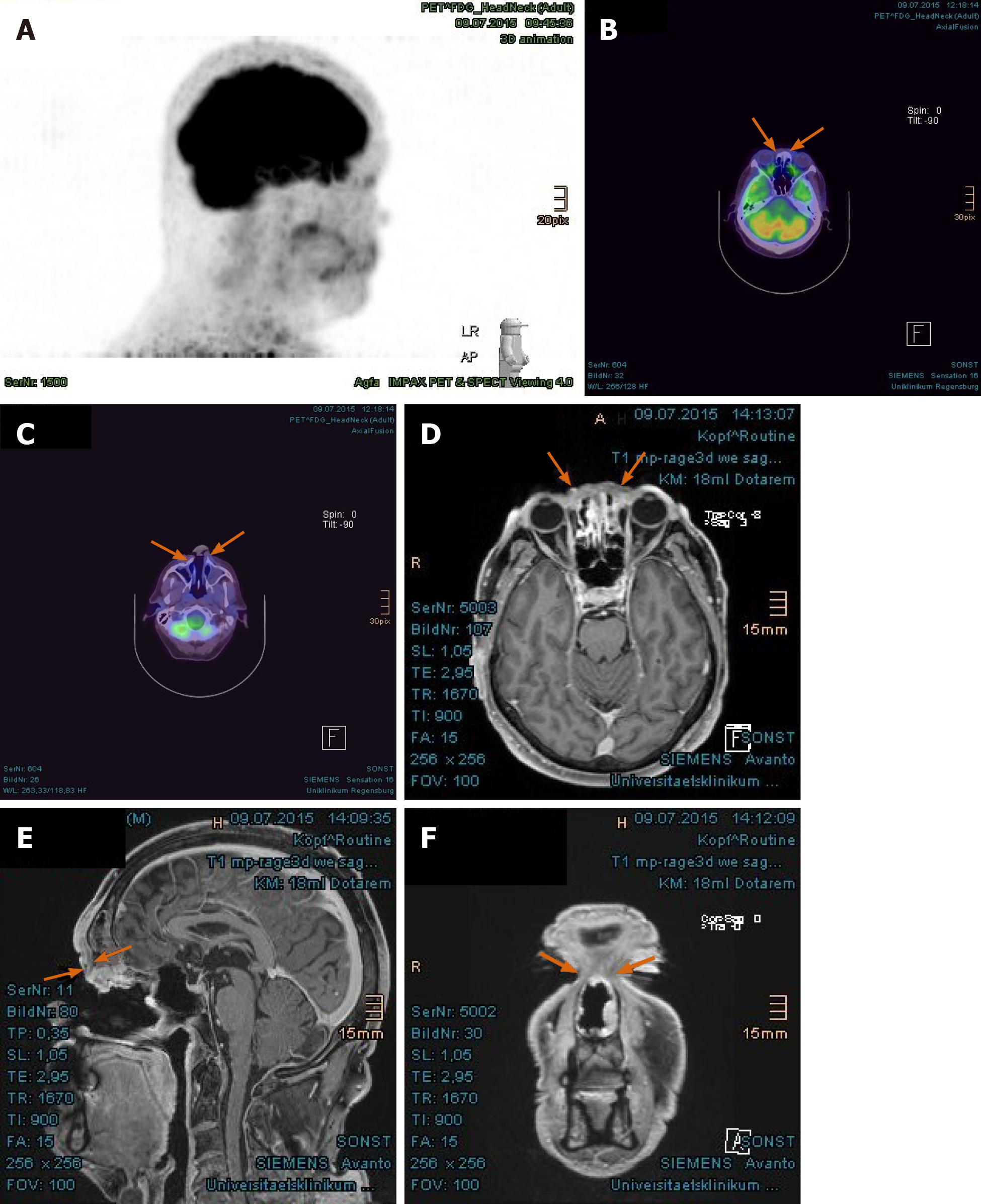
Figure 6 Complete tumor remission demonstrated in the positron emission tomography with 2-deoxy-2--fluorine-18-fluoro-D-glucose/computed tomography and magnetic resonance imaging at 8 mo after proton beam therapy.
A: No pathologically increased activity in the positron emission tomography, overview image; B: Absence of increased fluoro-D-glucose avidity in the nasal bridge (arrow-marked in positron emission tomography/computed tomography); C: Absence of metabolically active tumor in the nostrils; D: Corresponding area in the nasal bridge in magnetic resonance imaging, presented in axial plane; E: Corresponding area in the frontal skull base, presented in sagittal plane; F: Coronal presentation of tumor remission in the nasal bridge. Previously enhancing tumors marked with arrows.
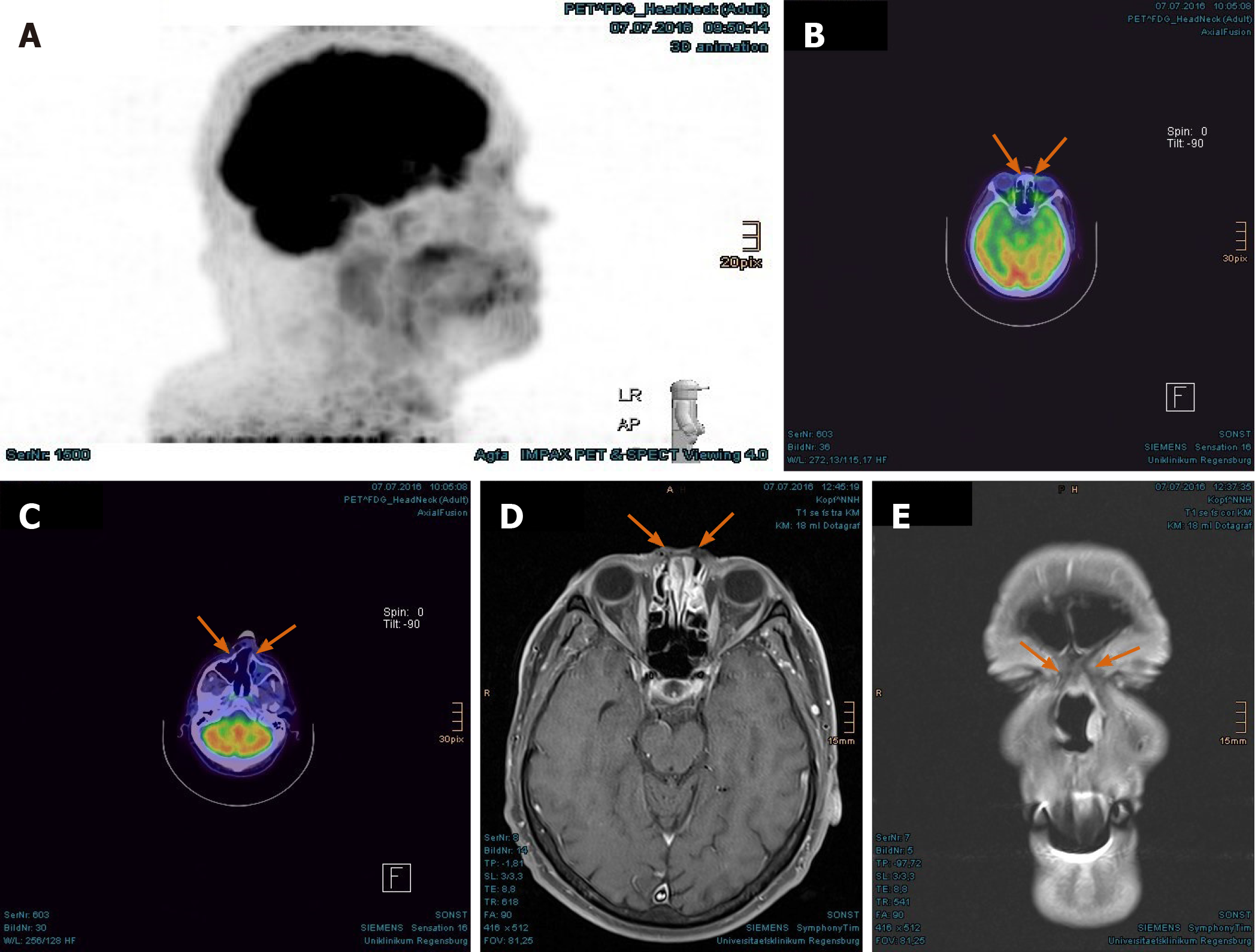
Figure 7 Persisting tumor remission evidenced in the positron emission tomography with 2-deoxy-2--fluorine-18-fluoro-D-glucose/computed tomography and magnetic resonance imaging at 20 mo after proton beam therapy.
A: No pathologically increased activity in the positron emission tomography, overview image; B: Absence of increased fluoro-D-glucose avidity in the nasal bridge (arrow-marked in positron emission tomography/computed tomography); C: Absence of metabolically active tumor in the nostrils; D: Flat surface above the nasal bridge in the magnetic resonance imaging; E: No evidence of tumor enhancement in the nasal bridge, presented in coronal plane.
Figure 8 “Case 1” patient’s images after a nasal reconstruction in five sessions between 2016-2017.
A: Taken in November 2016; B: Taken in February 2017; C: Taken after the last surgery in May 2017; D: Current image in March 2020.
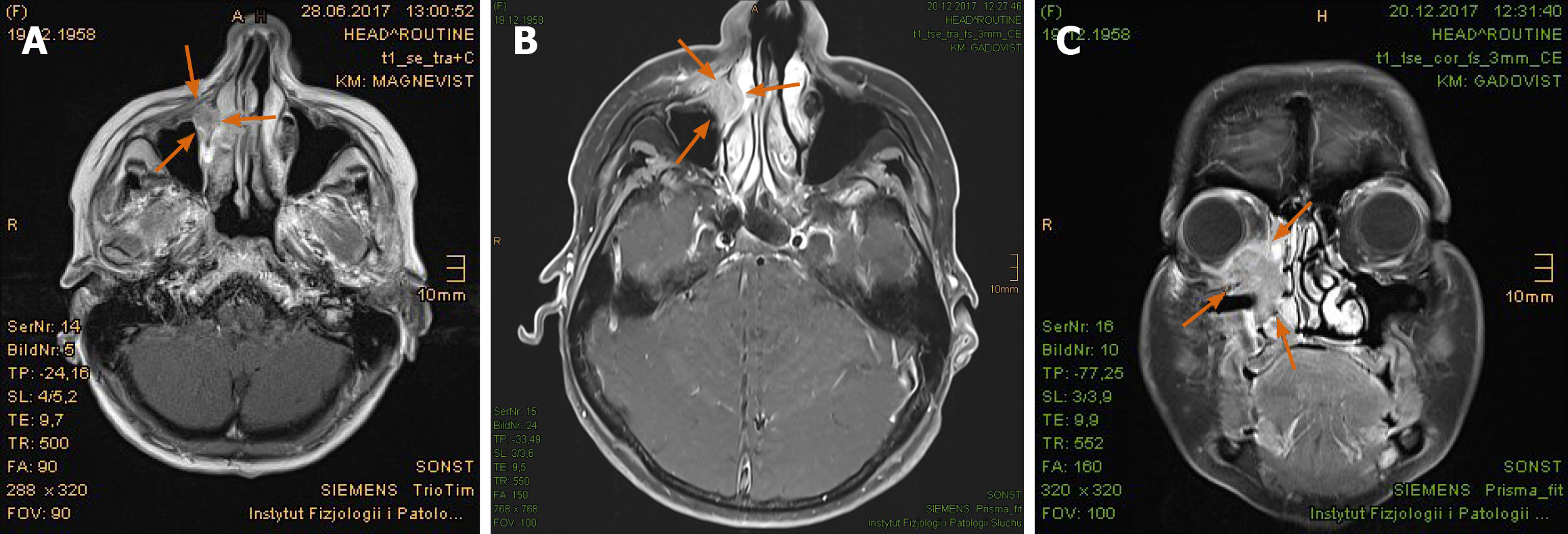
Figure 9 Continuously growing tumor lesion in the right lacrimal sac invading the adjacent orbit and sinonasal spaces, presented as magnetic resonance imaging.
A: Initial tumor extent in the antero-medial recess of the right maxillary sinus in June 2017; B: Size progression in December 2017, presented in axial plane; C: Distinct tumor invasion of the right orbit and neighboring sinonasal spaces, presented in coronal plane. Tumor marked with arrows.
Figure 10 “Case 2” patient’s image showing a tumorous nodule beneath the medial canthus of the right eye.
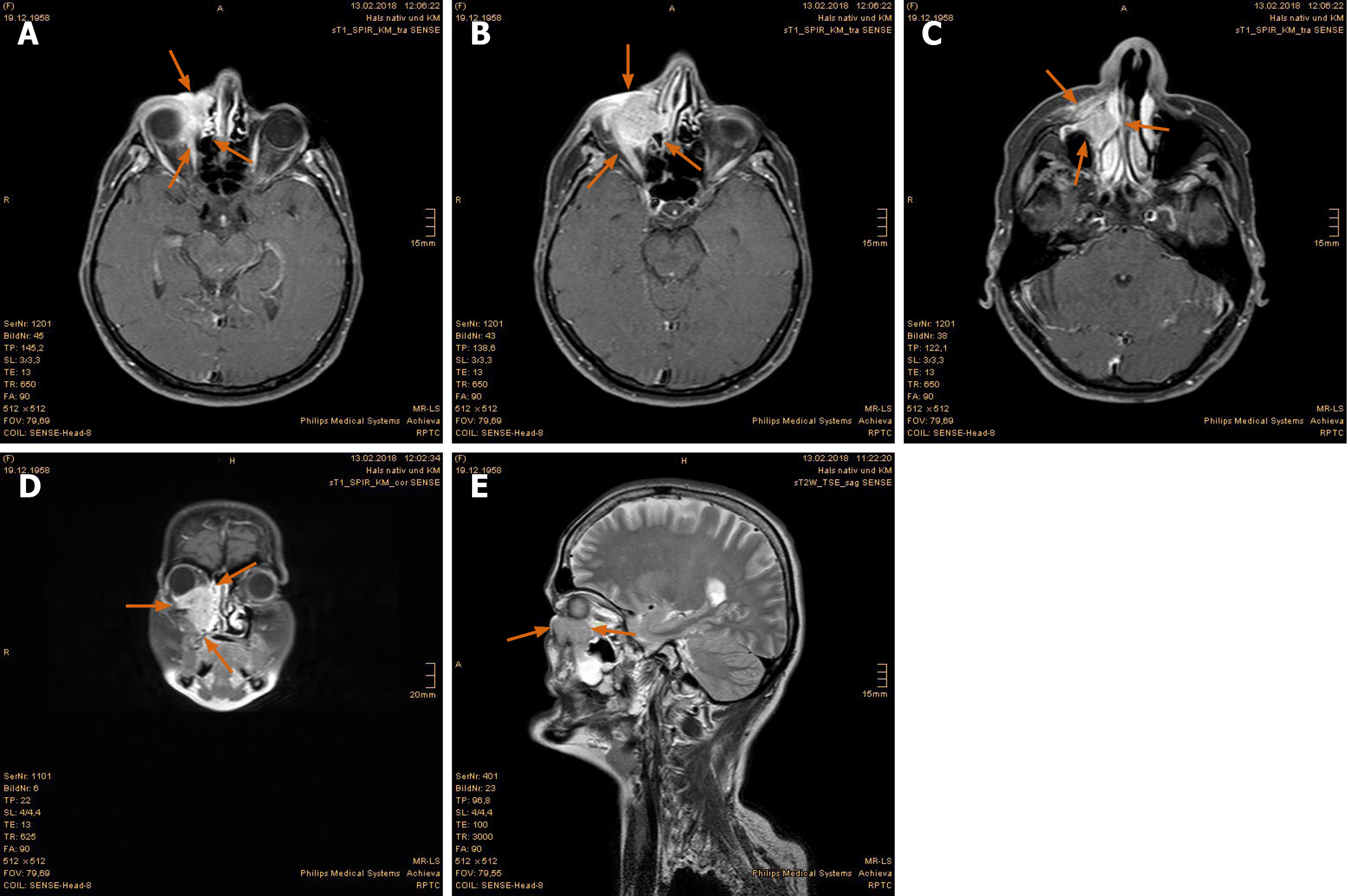
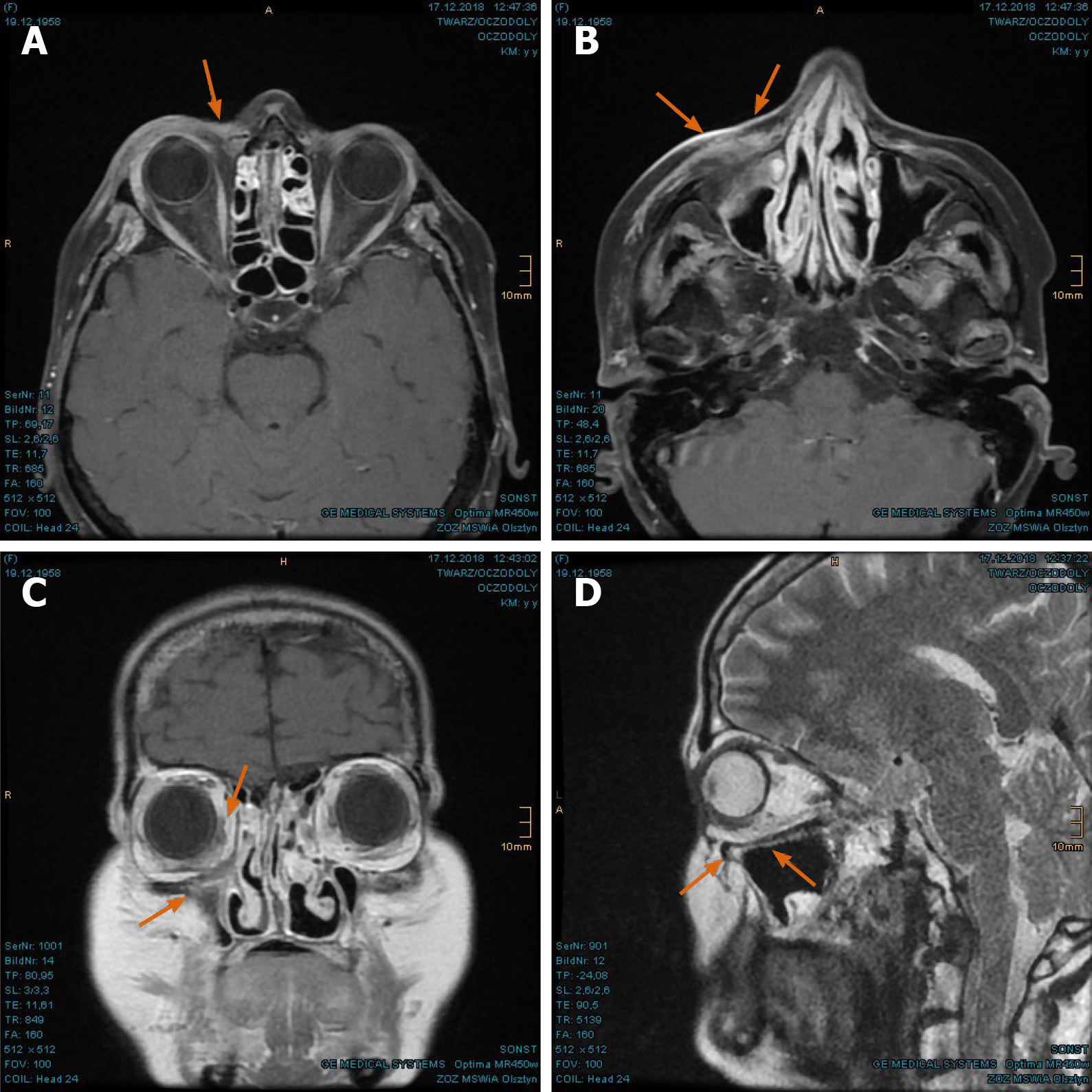
Figure 11 Magnetic resonance imaging prior to proton beam therapy.
A: Naso-orbital nodular enhancement with lacking delimitation to the right eyeball; B: Tumor displacement of the right eye; C: Growing tumor invasion of the right maxillary sinus, turbinates and adjoining facial soft tissue; D: Coronal presentation of the right periorbital sinonasal cancer; E: Sagittal presentation of the sinonasal cancer with shift of the right eyeball upwards. Tumor marked with arrows.
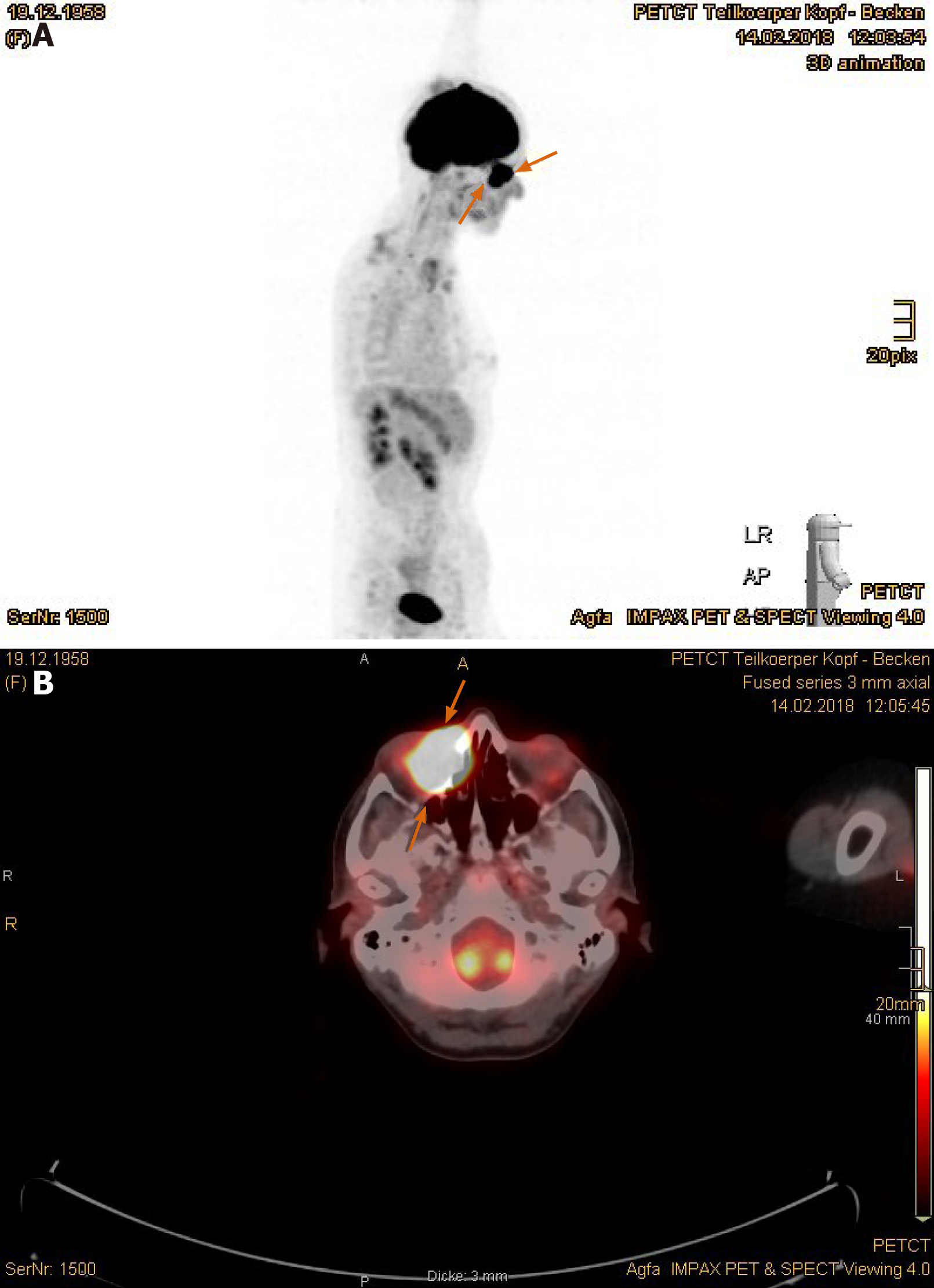
Figure 12 Positron emission tomography with 2-deoxy-2--fluorine-18-fluoro-D-glucose/computed tomography exhibited remarkably increased uptake in the right periorbital sinonasal squamous cell carcinoma.
A: Positron emission tomography overview image; B: Axial plane (tumor marked with arrows).
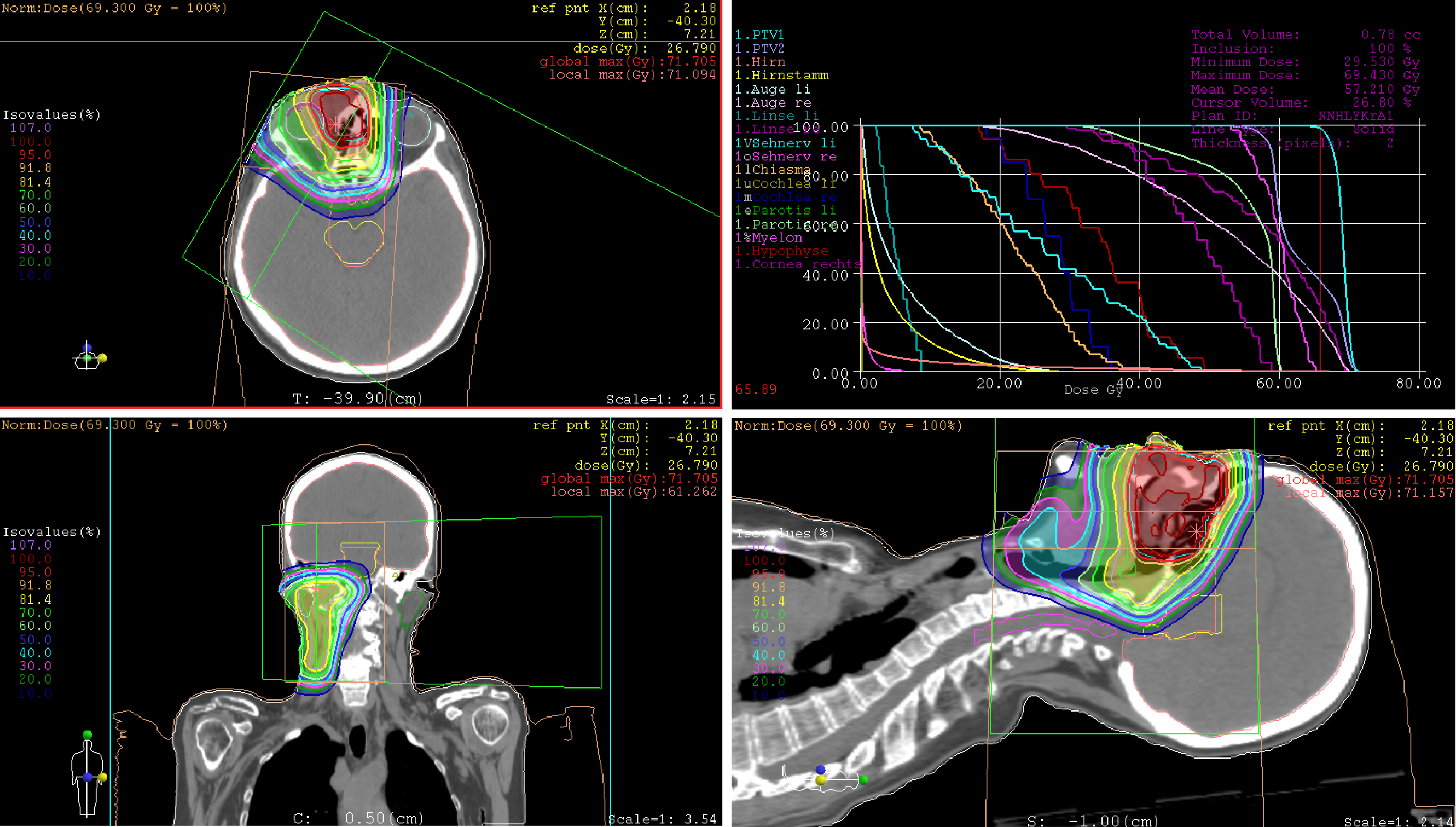
Figure 13 Treatment plan of proton beam therapy with isodose distributions in all three planes and dose-volume-histogram.
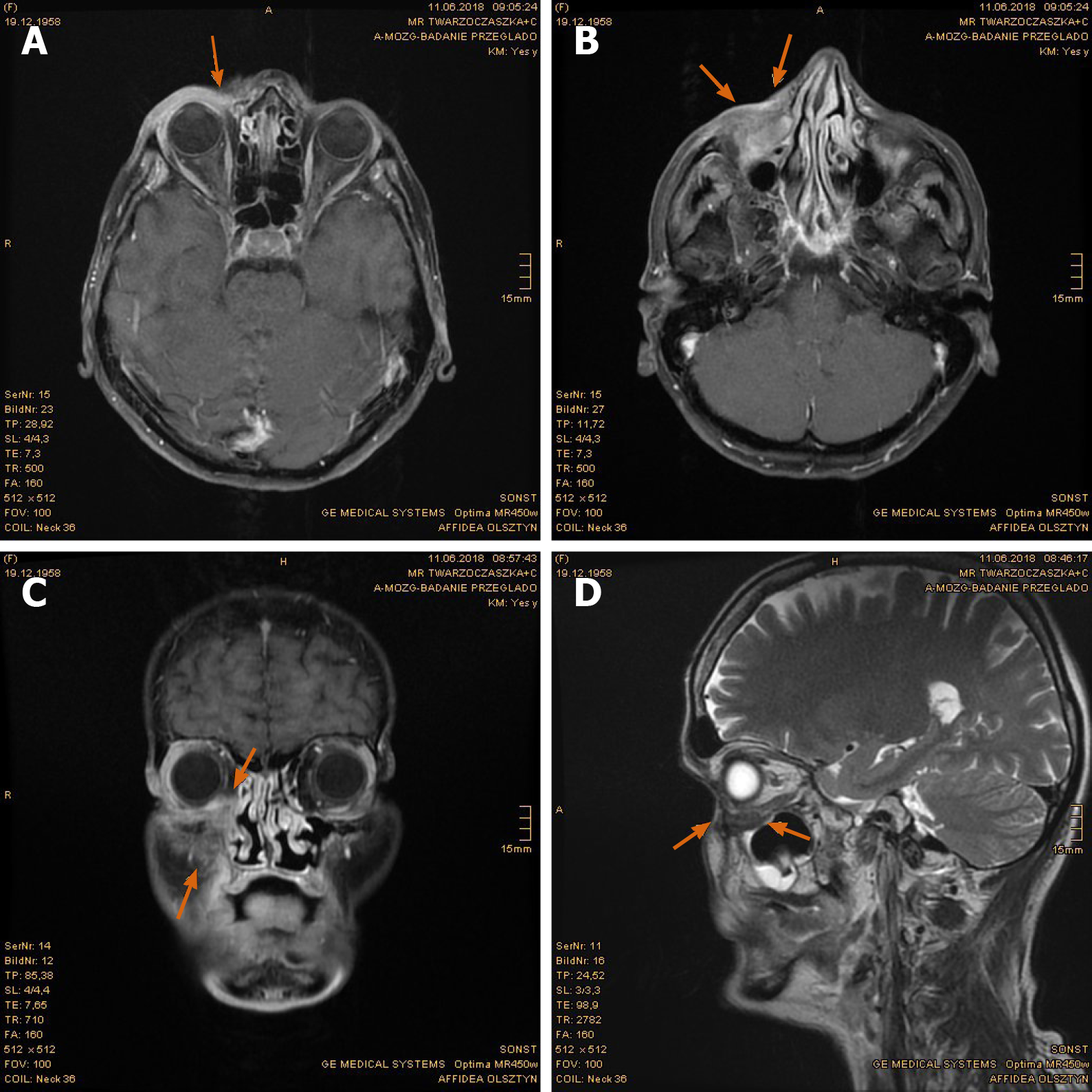
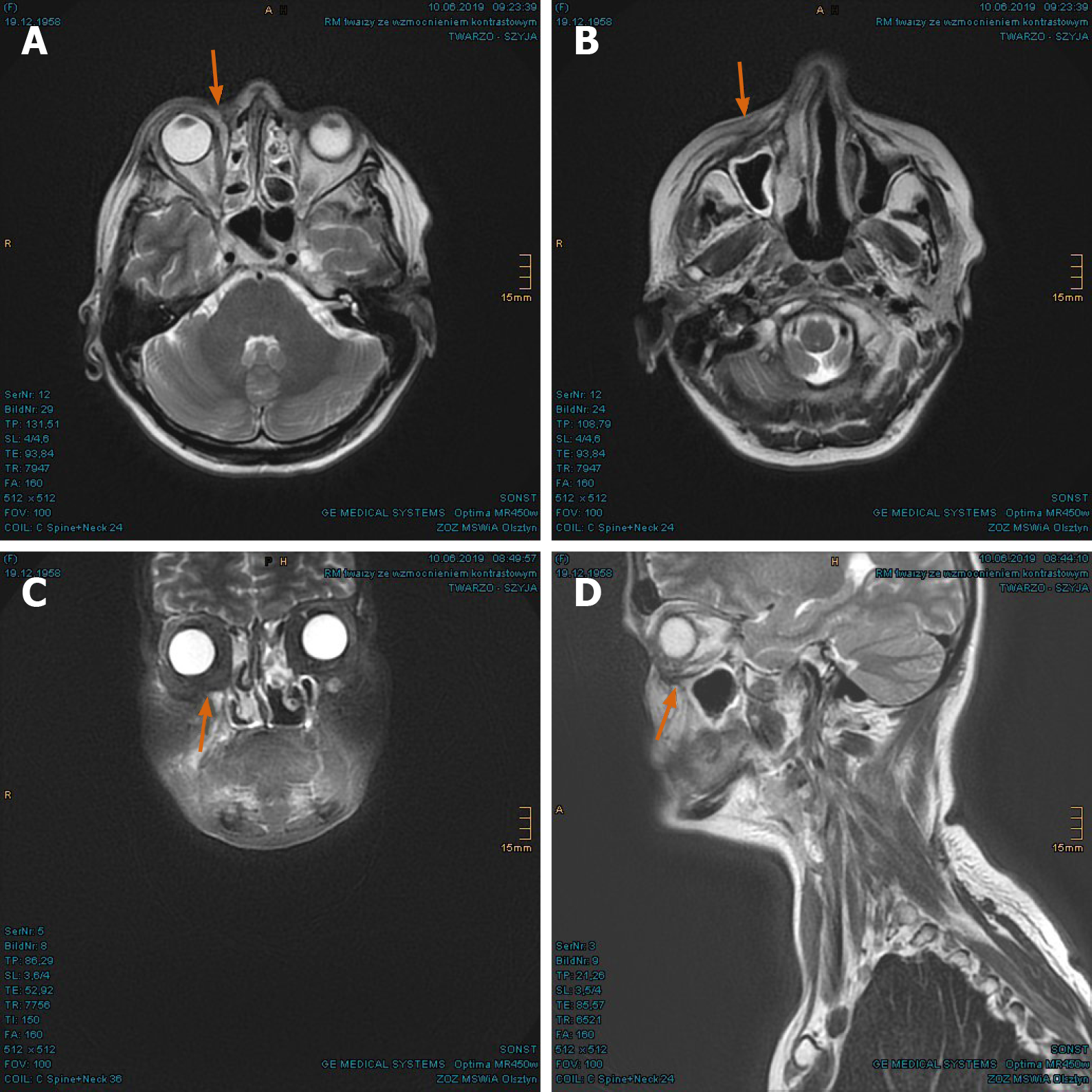
Figure 14 Pronounced tumor reduction in the first follow-up magnetic resonance imaging scan.
A: Dwindling of enhancing tumor nodules at the right naso-orbital corner; B: Decreased enhancement in the soft tissue of the naso-labial fold and zygomatic area; C: Significant regression of the right periorbital sinonasal cancer, presented in coronal plane; D: Restored delimitation of the right orbital floor, presented in sagittal plane. Former tumor extent marked with arrows.
Figure 15 Complete tumor remission verified in the magnetic resonance imaging at 8 mo after proton beam therapy.
A: Further regression of the tumorous enhancement in the right lacrimal sac marked with arrows; B: Postradiogenic changes of the right facial soft tissue with no evidence of residual tumor; C: Coronal presentation of the fully regressed right periorbital sinonasal cancer; D: Clearly defined orbital floor with normal position of the right eye.
Figure 16 Sustained full remission in the magnetic resonance imaging at 14 mo after proton beam therapy.
A: Right naso-orbital corner; B: Maxillary sinus and naso-labial fold; C and D: In coronal and sagittal plane, respectively.
Figure 17 “Case 2” patient’s current image at 2 years after proton beam therapy.
- Citation: Lin YL. Proton beam therapy of periorbital sinonasal squamous cell carcinoma: Two case reports and review of literature. World J Clin Oncol 2020; 11(8): 655-672
- URL: https://www.wjgnet.com/2218-4333/full/v11/i8/655.htm
- DOI: https://dx.doi.org/10.5306/wjco.v11.i8.655