Copyright
©The Author(s) 2020.
World J Clin Oncol. Jul 24, 2020; 11(7): 412-427
Published online Jul 24, 2020. doi: 10.5306/wjco.v11.i7.412
Published online Jul 24, 2020. doi: 10.5306/wjco.v11.i7.412
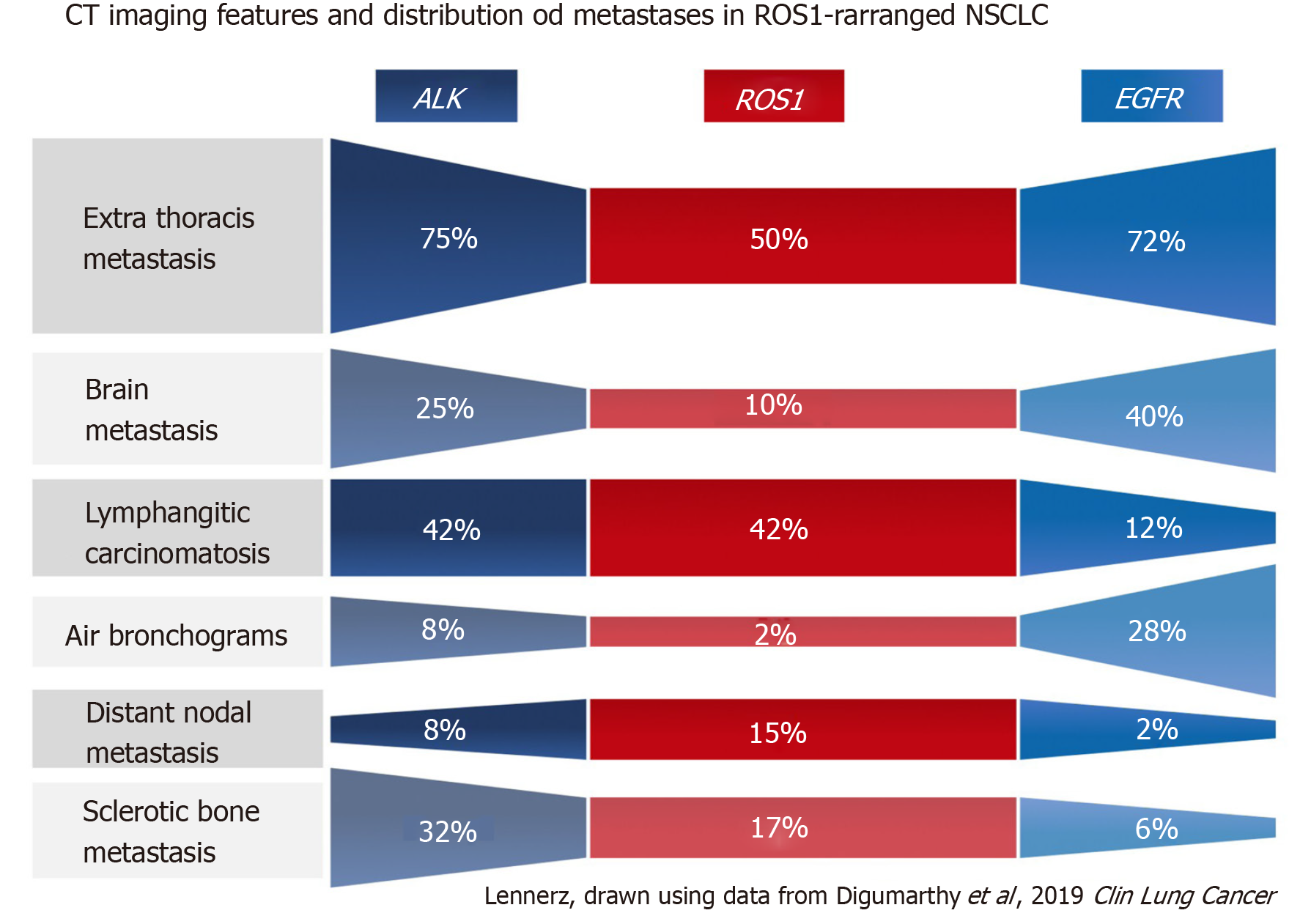
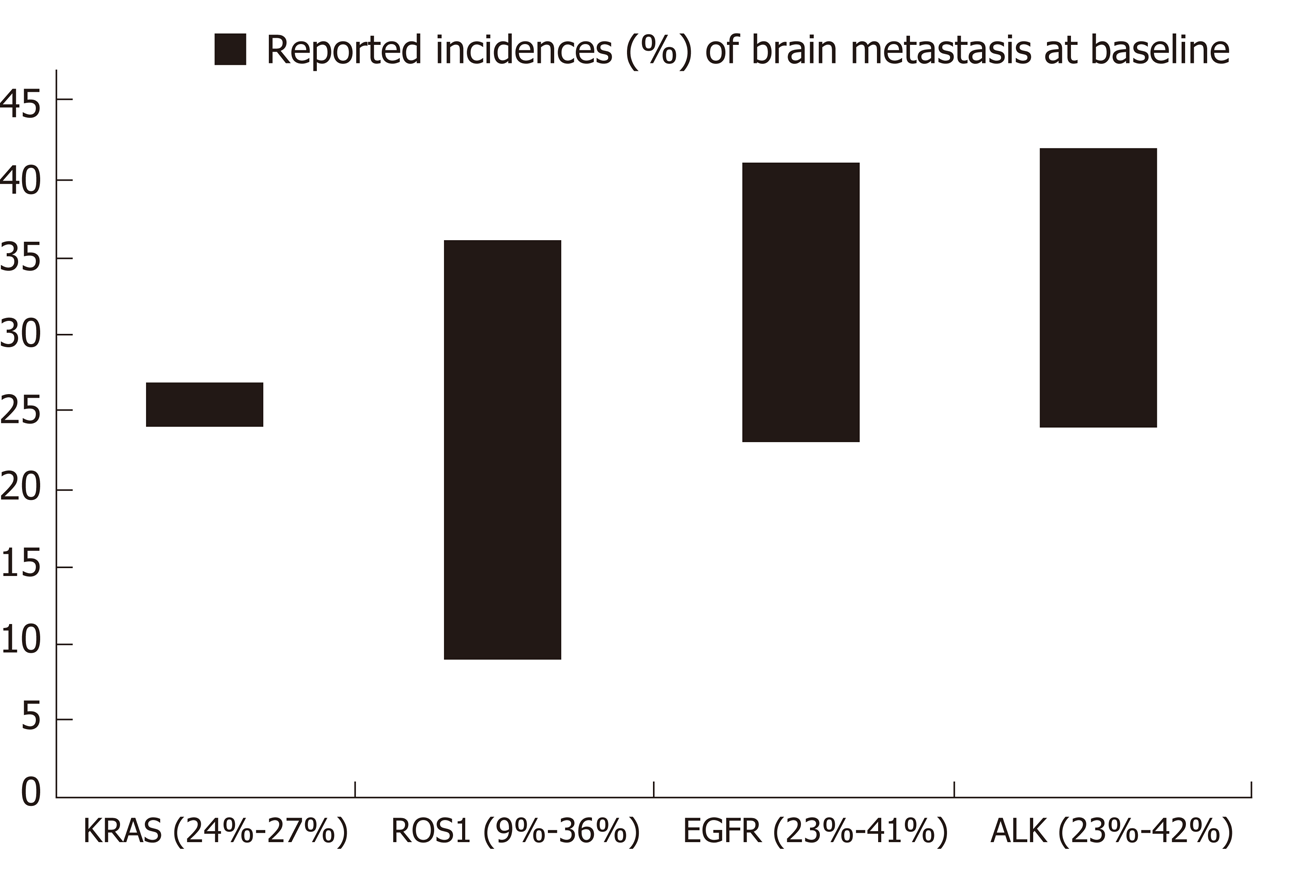
Figure 1 Comparison of select primary tumor features and metastatic patterns among patients with non-small cell lung cancer with ALK, ROS1, or EGFR alterations[71].
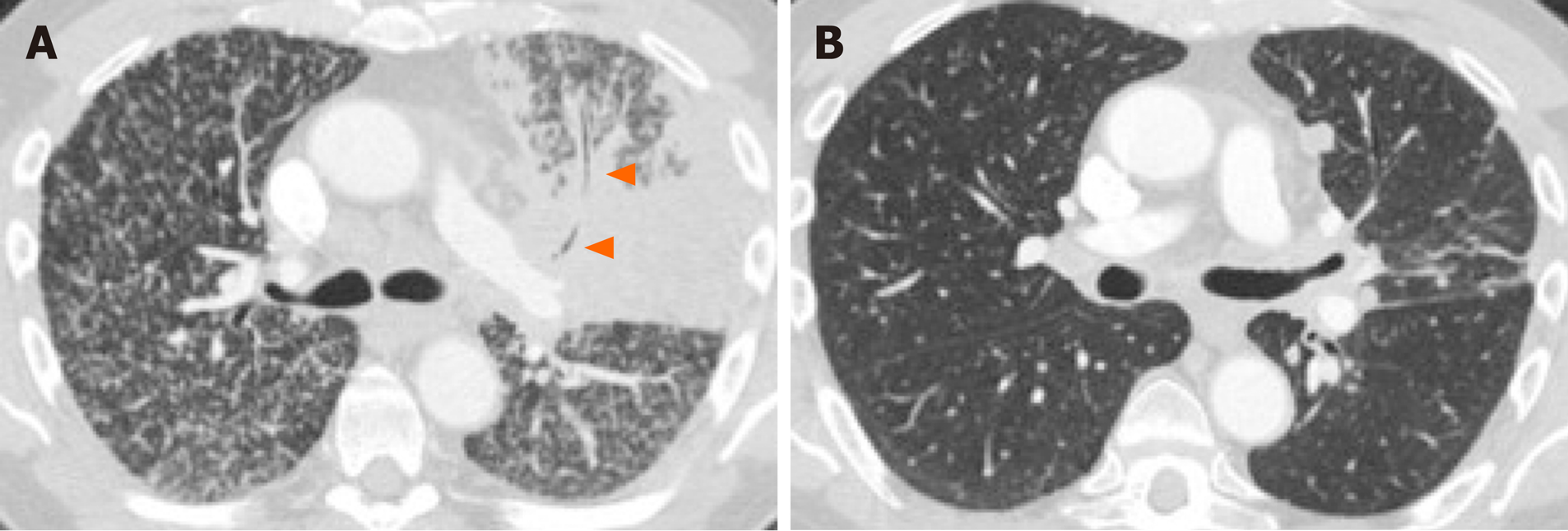
Figure 2 Primary tumor features and “miliary” type metastases in 66-year-old male non-smoker with EGFR-mutant non-small cell lung cancer.
A: Pretreatment computed tomography (CT) shows a mass-like consolidation in the left upper lobe with internal air bronchograms (arrowheads) and diffuse 1-2 mm nodules bilaterally consistent with “miliary” metastases. Consolidative, “pneumonic”, appearance of the primary tumor is associated with EGFR mutations in non-small cell lung cancer; B: Post-treatment CT shows marked treatment response to targeted therapy with mild residual scarring and nodularity in the left upper lobe and near-complete resolution of diffuse metastases.
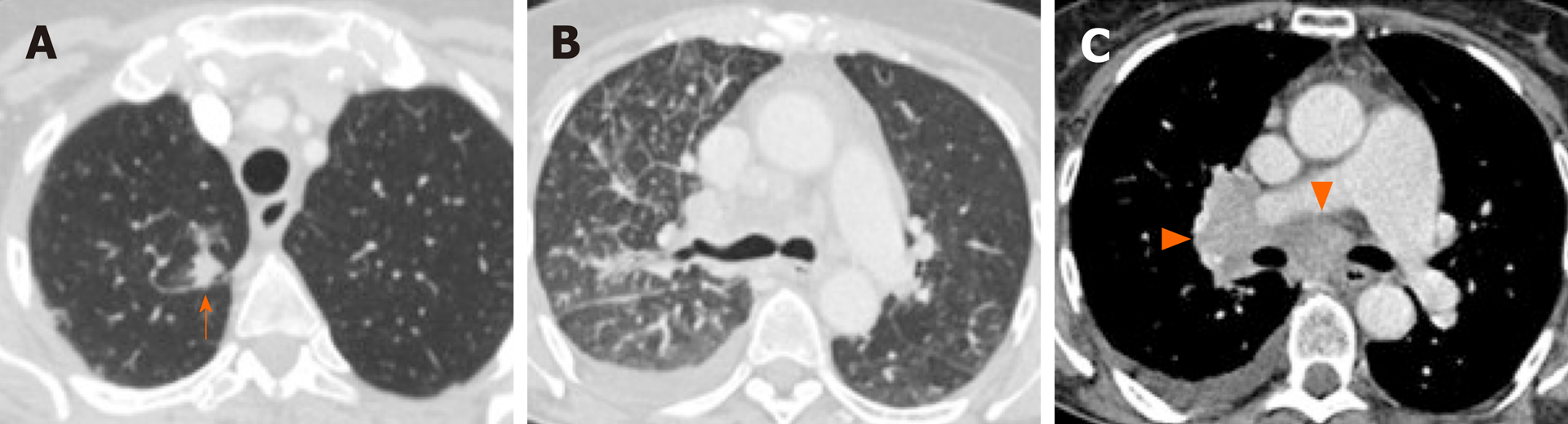
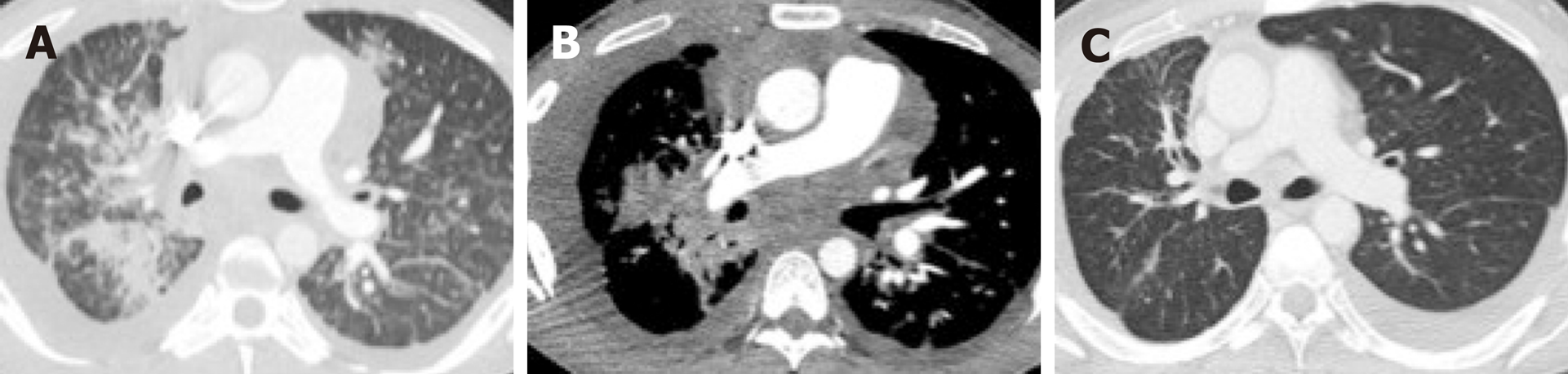
Figure 3 Lymphangitic carcinomatosis, pleural metastasis and, extensive lymphadenopathy in 64-year old female non-smoker with ALK-positive non-small cell lung cancer.
A: Pretreatment computed tomography (CT) shows a right upper lobe nodule (arrow) corresponding to the primary lung tumor; B: CT slice at the level of the carina shows extensive right sided nodular septal thickening consistent with lymphangitic carcinomatosis; C: CT (mediastinal window) shows extensive right hilar and subcarinal lymphadenopathy (arrowheads) consistent with nodal metastases. A pleural effusion, later proven to be malignant by cytology, is also noted. These features have been associated with ALK-positive non-small cell lung cancer (NSCLC). Similar features have also been described in ROS1-positive NSCLC (Figure 5).
Figure 4 Imaging features of the primary lung tumor and patterns of lung metastases in non-small cell lung cancer with driver mutations.
A: Computed tomography (CT) of a patient with EGFR-mutant non-small cell lung cancer (NSCLC) shows a dominant central left upper lobe mass with diffuse “miliary” type metastases bilaterally. Note the “consolidative” appearance of the dominant mass with air bronchograms (arrowhead), which have also been associated with EGFR-mutant NSCLC; B: CT of a patient with ALK-rearranged NSCLC shows a solid dominant peripheral right upper lobe mass (arrowhead) with nodular thickening of interstitium and ground glass opacities consistent with lymphangitic carcinomatosis, which have been associated with NSCLC with either ALK or ROS1 rearrangements; C: CT of a patient with NSCLC with MET exon 14 skipping mutation shows a part-cystic, part-solid nodule in the right upper lobe (thick arrow) with an additional ground glass nodule in the left lower lobe (arrowhead) and a smaller ground glass nodule in the left upper lobe (thin arrow), consistent with synchronous multifocal lung cancers.
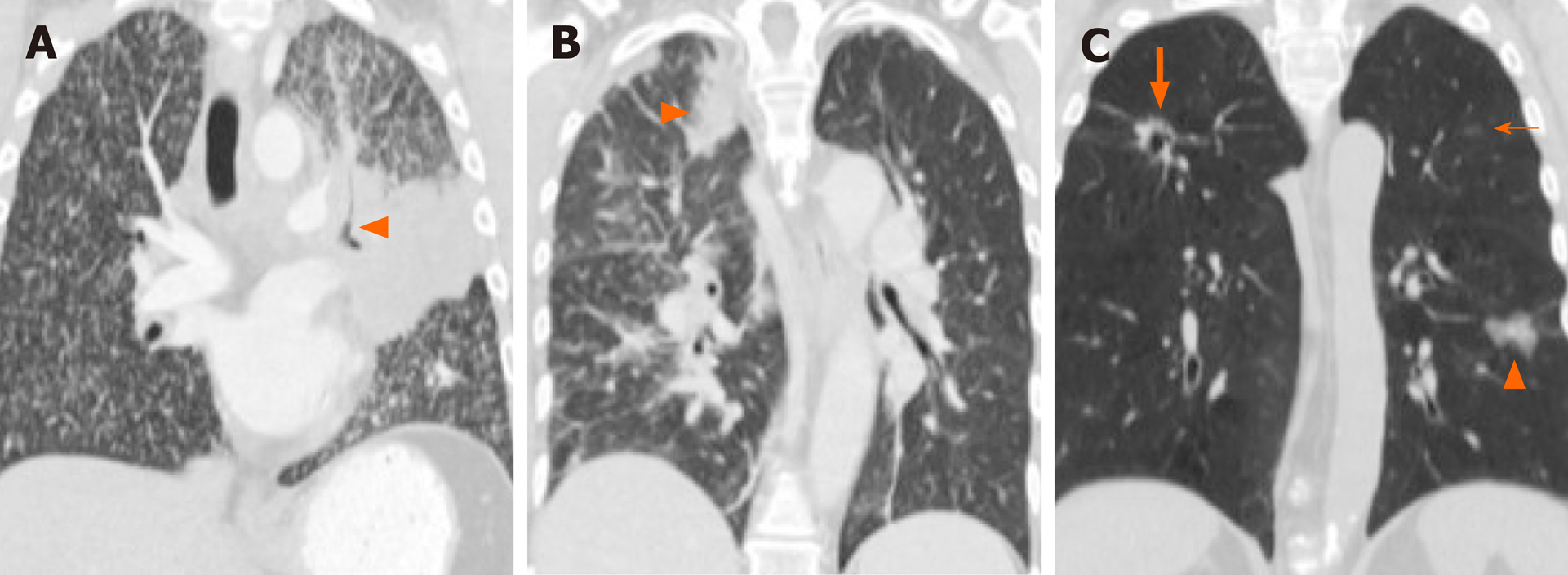
Figure 5 Lymphangitic carcinomatosis and pleural metastases in 26-year old male non-smoker with ROS1-positive non-small cell lung cancer.
A: Pre-treatment computed tomography (CT) shows a dominant right lower lobe mass with diffuse bilateral, right greater than left, lymphangitic carcinomatosis characterized by nodular interstitial thickening and ground glass opacities; B: Pre-treatment CT (mediastinal window) shows right pleural nodular thickening and pleural effusion (arrowheads) consisted with pleural metastasis; C: Initial post-treatment CT shows marked interval response to targeted therapy with near complete resolution of right lower lobe mass and of lymphangitic carcinomatosis. Increased frequencies of lymphangitic carcinomatosis and pleural metastases have also been described in ALK-positive non-small cell lung cancer (Figure 2).
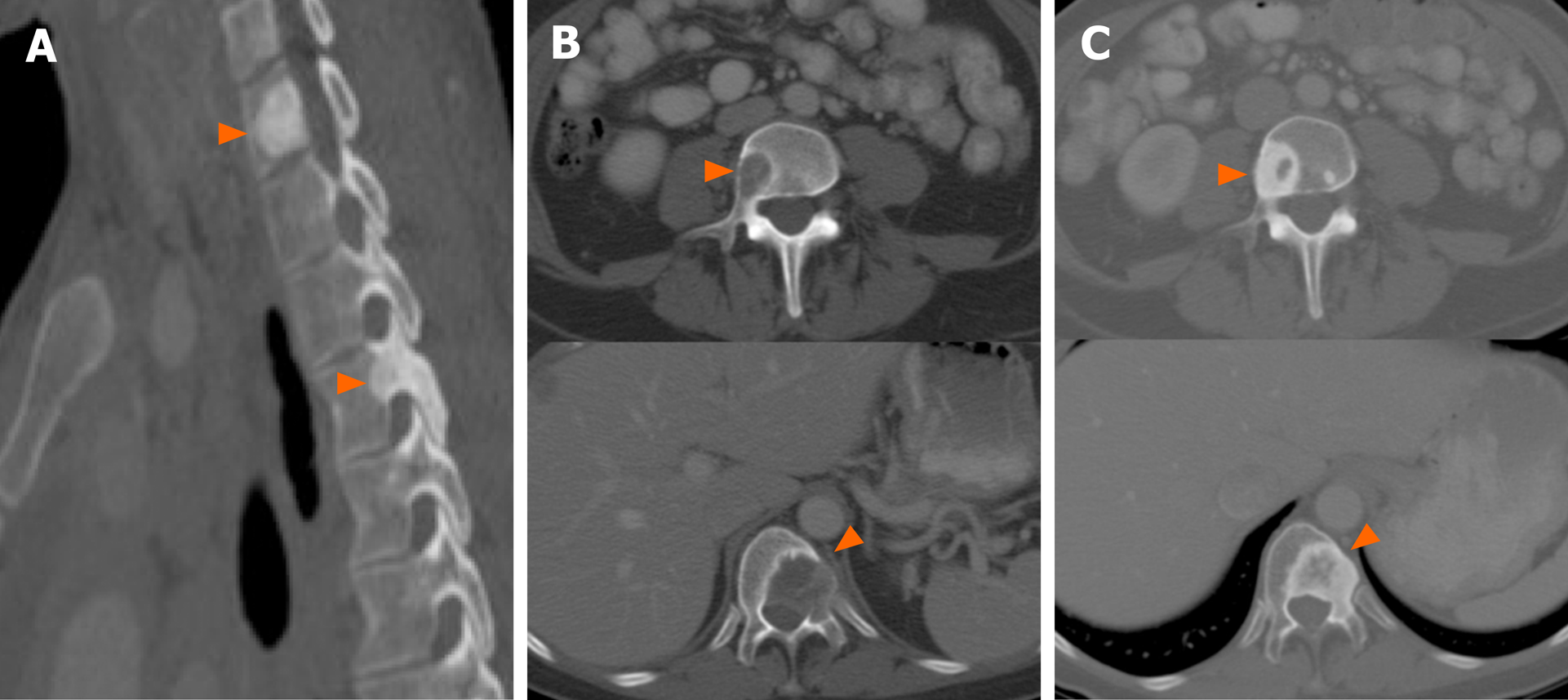
Figure 7 Patterns of bone metastases in non-small cell lung cancer with driver mutations.
A: Pretreatment computed tomography (CT) images (sagittal, bone window) show sclerotic lesions involving the cervicothoracic spine (arrowheads) consistent with osseous metastases in ROS1-positive non-small cell lung cancer (NSCLC); B: Pretreatment CT images (sagittal, bone window) show lytic lesions involving thoracic and lumbar vertebral bodies (arrowheads) in patient with EGFR-mutant NSCLC; C: Post-treatment CT of the same patient as Figure 7B shows interval sclerosis of previously lytic osseous metastases (arrowheads). In general, most NSCLC tend to have lytic lesions in contrast to those with ROS1 or ALK positive NSCLC, which tend to be more sclerotic at presentation. Sclerosis of previously lytic lesion is often seen after treatment.
- Citation: Mendoza DP, Piotrowska Z, Lennerz JK, Digumarthy SR. Role of imaging biomarkers in mutation-driven non-small cell lung cancer. World J Clin Oncol 2020; 11(7): 412-427
- URL: https://www.wjgnet.com/2218-4333/full/v11/i7/412.htm
- DOI: https://dx.doi.org/10.5306/wjco.v11.i7.412