Published online Nov 6, 2015. doi: 10.4292/wjgpt.v6.i4.253
Peer-review started: May 12, 2015
First decision: August 19, 2015
Revised: September 11, 2015
Accepted: October 12, 2015
Article in press: October 13, 2015
Published online: November 6, 2015
Processing time: 184 Days and 19.2 Hours
A 53-year-old woman underwent a 2-stage right hepatectomy for bilobar metastasis of an ileal neuroendocrine carcinoma. Preoperative three-dimensional computed tomography reconstruction helped to diagnose an intrahepatic venovenous shunts from the right and middle hepatic veins to the left hepatic vein, which could cause a intraoperative bleeding. Hemostasis was performed by means of precoagulation with microwave-assisted coagulation.
Core tip: Detection of anomalies in hepatic vascularization before liver surgery is crucial in order to prevent intraoperative difficulties such as massive bleeding, which needs to be controlled. Surgical planning is now well-known as a major step in liver surgery. From a general standpoint, three-dimensional computed tomography (3D-CT) is not used to this purpose but can be very useful to identify vascular structures. We report a case where intrahepatic venovenous shunts were preoperatively diagnosed by means of 3D-CT reconstruction and were managed with precoagulation microwave-assisted coagulation.
- Citation: Delhorme JB, Méméo R, Marescaux J, Pessaux P. Preoperative detection of intrahepatic venovenous shunt treated by microwave precoagulation during right hepatectomy. World J Gastrointest Pharmacol Ther 2015; 6(4): 253-256
- URL: https://www.wjgnet.com/2150-5349/full/v6/i4/253.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v6.i4.253
Detection of anomalies in hepatic vascularization before liver surgery is crucial in order to prevent intraoperative difficulties such as massive bleeding, which needs to be controlled. Surgical planning is now well-known as a major step in liver surgery[1], and the absence of agreement between a preoperative planning and the realized operating techniques has been shown as risk factor of morbidity. From a general standpoint, three-dimensional computed tomography (3D-CT) is not used to this purpose but can be very useful to identify vascular structures. As blood loss represents a major complication prognostic factor in liver surgery, several bloodless techniques are available. In case of persistent bleeding, tissue precoagulation with microwave energy can be a very attractive tool to achieve tissue hemostasis.
We report a case where intrahepatic venovenous shunts were preoperatively diagnosed by means of 3D-CT reconstruction and were managed with precoagulation microwave-assisted coagulation.
Lower limb edema made it possible to detect a voluminous intrahepatic lesion compressing the retrohepatic vena cava in a 53-year-old woman. This lesion located in segments IV and VII of the liver measured 16 by 13 by 15 cm. The patient’s past medical history included thyroidectomy, appendectomy, arterial hypertension and hypercholesterolemia. Percutaneous liver biopsy confirmed the diagnosis of liver metastasis of a grade 2 neuroendocrine tumor (Ki-67 index = 5%). Preoperative examination including CT-scan, MRI, and a somatostatin receptor scintigraphy showed a primitive tumor at the last ileal loop with bilobar synchronous liver metastasis (voluminous lesion in the right liver and another one in liver segment II). After discussion in our oncological multidisciplinary committee, a 2-stage surgical strategy was put forward.
The first step consisted in a right colectomy with radiofrequency ablation of the liver metastasis in liver segment II. The postoperative outcome was uneventful. Histopathological examination confirmed an ileal grade 2 well-differentiated neuroendocrine carcinoma, classified pT3N1 (11 lymph nodes involved out of 21 retrieved) M1 according to the 7th edition of the AJCC/UICC system TNM classification (Ki-67 index = 5% and the mitotic index was less than 1 mitosis/10HPF).
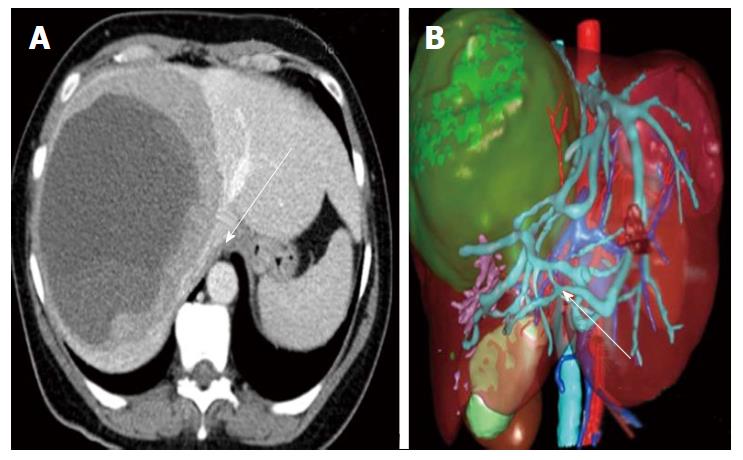
One month later, a percutaneous right portal embolization was performed in order to induce left liver hypertrophy. Six weeks later, the future remnant liver (segments I, II, III and IVb) represented 29.5% of the total liver (vs 22.5% prior to embolization). The 3D virtual anatomical model was obtained from thoraco-abdominal CT-scanning using a customary software [VR-RENDER®, IRCAD (Institut de Recherche contre les Cancers de l’Appareil Digestifs)]. The 3D modeling confirmed the compression of the right and middle supra-hepatic veins as well as the presence of intrahepatic venovenous shunts from the right and middle hepatic veins to the left hepatic vein crossing through segments IV and V of the liver (Figure 1). The model was then processed using a VR-RENDER® plug-in application, the Virtual Surgical Planning (VSP®, IRCAD), in order to delineate surgical resection planes, including elective ligature of vascular structures and precoagulation of venovenous shunts. We discussed the possibility of a preoperative endovascular embolization of the shunt, but it was retained due to the risks of the procedure.
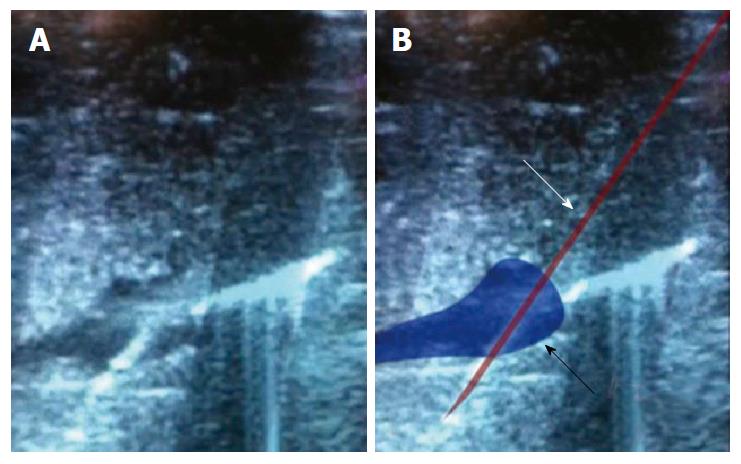
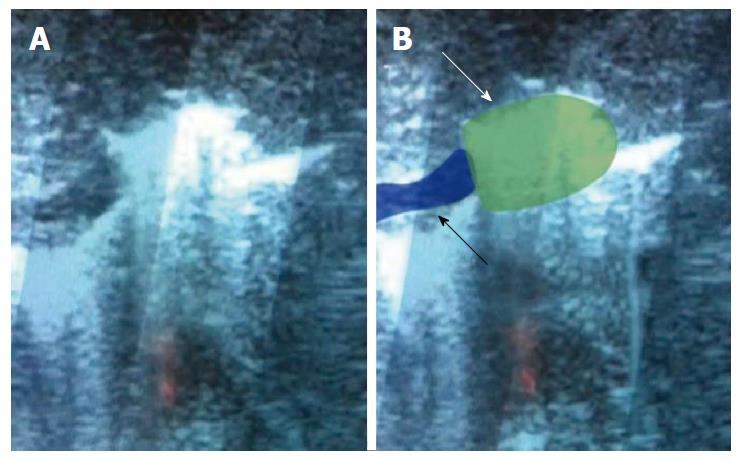
A right hepatectomy was initiated with an intraoperative ultrasound examination, which corroborated the presence of venovenous shunts. The right branch of the portal vein and the hepatic artery were dissected, clamped, and then ligatured. As anticipated, parenchymal transection using ultrasonic tissue ablation system (CUSA®) induced bleeding, caused by the difficulty to control the venovenous shunts. We decided to completely isolate the liver from blood flow by clamping hepatoduodenal ligament, infrahepatic vena cava, and suprahepatic cava. Despite this total liver vascular exclusion, bleeding was still difficult to control. Consequently, as preoperatively planned, it was decided to perform a precoagulation of the multiple shunts by means of a microwave-assisted coagulation. We used a 2 cm microwave needle applied onto the shunts crossing through liver segment IV transection line (Figure 2). This maneuver allowed to control bleeding and right hepatectomy was then completed in adequate conditions (Figure 3). The postoperative outcome was uneventful and the patient was discharged on postoperative day 12.
Histopathological examination confirmed the completeness of resection of two right liver metastases from a G2 well-differentiated neuroendocrine carcinoma with Ki-67 index comprised between 5% and 10% and less than 1 mitosis/10HPF. The multidisciplinary committee opted for an oncological follow-up. At one year, the patient was disease-free.
Preoperative evaluation of hepatic vascularization can be very useful in order to anticipate potential intraoperative difficulties, in particular when hepatic vein resection is required. Several detection techniques have been described in the literature in order to analyze intrahepatic venovenous shunts. Sakaguchi et al[2] showed that hepatic occlusion venography allowed for the detection of venovenous shunt in half of patients while it was unpredictable from CT-scan or laboratory data. The main drawback of this technique lies in its invasiveness. Intrahepatic venous anastomosis has also been evaluated in living donor liver transplantation with Doppler ultrasonography and pulse-inversion ultrasonography by Kaneko et al[3]. This procedure seems to be efficient for detection of venovenous shunts between the middle and the right hepatic vein but it is operator-dependent and not often available. Detection of venovenous shunts is also efficient with 3D-venography reconstructed from multidetector-row computed tomography during angiography[4]. Three-dimensional computed tomography, as shown in our case report, appears to be an appropriate tool to evaluate hepatic vascularization prior to surgery. As demonstrated by Kamiyama et al[5] in a cohort, 3D-CT provided key information that could not be obtained with two-dimensional computed tomography (2D-CT).
From CT or MRI images, it’s often difficult for the surgeon to plan precisely the technical procedure. These imaging exams provide images in 2D, but surgeons work in 3D. It seems fundamental to offer surgeons patient-specific 3D model of the liver for easy interpretation of the anatomy. Volume rendering available on all radiology consoles does not make independent each organ, and therefore does not allow performing a virtual surgery. To overcome this limitation, we created a software allowing the identification and delimitation of each anatomical and pathological structure with different colours (Figure 1). This 3D model is optimal to obtain preoperative surgical planning and intraoperative guidance. In our case report, the venovenous shunt was known before surgery and difficulties to perform hemostasis were anticipated.
In our case, microwave was successfully used not to obtain tissue coagulation but to achieve elective precoagulation of the shunt. The needle was electively and precisely inserted with ultrasound control into the shunt to obtain a thrombus. Microwave coagulation is also less time-consuming as compared to radiofrequency coagulation. In case of difficulty to control bleeding during hepatectomy and to limit blood loss, especially in cirrhotic liver, it might be better to perform tissue precoagulation using microwave coagulation.
In conclusion, the presentation of this case report underscores two major key topics concerning liver surgery. First and foremost, a thorough knowledge of liver anatomy preoperatively is essential as it gives the surgeon the opportunity to anticipate hemostatic difficulties in liver surgery where blood loss is a major complication and prognostic factor. This can be easily evaluated by means of preoperative 3D-CT. Secondly, tissue precoagulation using radiofrequency or microwave coagulation should remain available for the surgeon as they can be important tools to control persistent bleeding in spite of conventional bloodless hepatectomy techniques.
This manuscript has been extensively revised linguistically by a native English speaker (Christopher Burel), with 4 years of professional experience in medical translation; and by two non-native speakers (Mathilde Raux-Defossez and Guy Temporal) with a postgraduate degree in medical translation.
Authors are grateful to Christopher Burel, Mathilde Raux-Defossez, and Guy Temporal for their linguistic proofreading.
A 53-year-old woman underwent a 2-stage right hepatectomy for bilobar metastasis of an ileal neuroendocrine carcinoma.
Lower limb edema made it possible to detect a voluminous intrahepatic lesion compressing the retrohepatic vena cava.
Malignant tumors (hepatocarcinoma or other liver metastases) and benign lesions (focal nodular hyperplasia, hemangioma and adenoma).
Preoperative examination including computed tomography (CT)-scan, magnetic resonance imaging, and a somatostatin receptor scintigraphy showed a primitive tumor at the last ileal loop with bilobar synchronous liver metastasis. The 3D virtual anatomical model was obtained from thoraco-abdominal CT-scanning using a customary software (VR-RENDER®, IRCAD).
Percutaneous liver biopsy confirmed the diagnosis of liver metastasis of a grade 2 neuroendocrine tumor (Ki-67 index = 5%).
Right hepatectomy with precoagulation and microwave.
Few papers report the preoperative detection and intraoperative management of intrahepatic veno-venous shunt.
The precoagulation of the shunt avoided major bleeding during the parenchymal transection.
First and foremost, a thorough knowledge of liver anatomy preoperatively is essential as it gives the surgeon the opportunity to anticipate hemostatic difficulties in liver surgery where blood loss is a major complication and prognostic factor. This can be easily evaluated by means of preoperative 3D-CT. Secondly, tissue precoagulation using radiofrequency or microwave coagulation should remain available for the surgeon as they can be important tools to control persistent bleeding in spite of conventional bloodless hepatectomy techniques.
This video clip and the case report are well presented.
P- Reviewer: Chok KSH, Uchiyama H S- Editor: Qiu S
L- Editor: A E- Editor: Li D
| 1. | Gauss T, Merckx P, Brasher C, Kavafyan J, Le Bihan E, Aussilhou B, Belghiti J, Mantz J. Deviation from a preoperative surgical and anaesthetic care plan is associated with increased risk of adverse intraoperative events in major abdominal surgery. Langenbecks Arch Surg. 2013;398:277-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Sakaguchi T, Suzuki S, Inaba K, Fukumoto K, Takehara Y, Nasu H, Kamiya M, Yamashita S, Ushio T, Nakamura S. Analysis of intrahepatic venovenous shunt by hepatic venography. Surgery. 2010;147:805-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Kaneko T, Sugimoto H, Hirota M, Kure S, Kiuchi T, Nakao A. Intrahepatic venous anastomosis formation of the right liver in living donor liver transplantation: evaluations by Doppler ultrasonography and pulse-inversion ultrasonography with Levovist. Surgery. 2005;138:21-27. [PubMed] |
| 4. | Sakaguchi T, Suzuki S, Hiraide T, Shibasaki Y, Morita Y, Suzuki A, Fukumoto K, Inaba K, Takehara Y, Nasu H. Detection of intrahepatic veno-venous shunts by three-dimensional venography using multidetector-row computed tomography during angiography. Surg Today. 2014;44:662-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Kamiyama T, Nakagawa T, Nakanishi K, Kamachi H, Onodera Y, Matsushita M, Todo S. Preoperative evaluation of hepatic vasculature by three-dimensional computed tomography in patients undergoing hepatectomy. World J Surg. 2006;30:400-409. [PubMed] |