Published online Nov 5, 2024. doi: 10.4292/wjgpt.v15.i6.99097
Revised: September 6, 2024
Accepted: September 14, 2024
Published online: November 5, 2024
Processing time: 103 Days and 12.7 Hours
Corrosive ingestion remains an important global pathology with high morbidity and mortality. Data on the acute management of adult corrosive injuries from sub-Saharan Africa is scarce, with international investigative algorithms, relying heavily on computed tomography (CT), having limited availability in this setting.
To investigate the corrosive injury spectrum in a low-resource setting and the applicability of parameters for predicting full-thickness (FT) necrosis and morta
A retrospective analysis of a prospective corrosive injury registry (March 1, 2017–October 31, 2023) was performed to include all adult patients with acute corrosive ingestion managed at a single, academic referral centre in Cape Town, South Africa. Patient demographics, corrosive ingestion details, initial investigations, management, and short-term outcomes were described using descriptive statistics while multivariate analysis with receiver operator characteristic area under the curve graphs (ROC AUC) were used to identify factors predictive of FT necrosis and 30-day mortality.
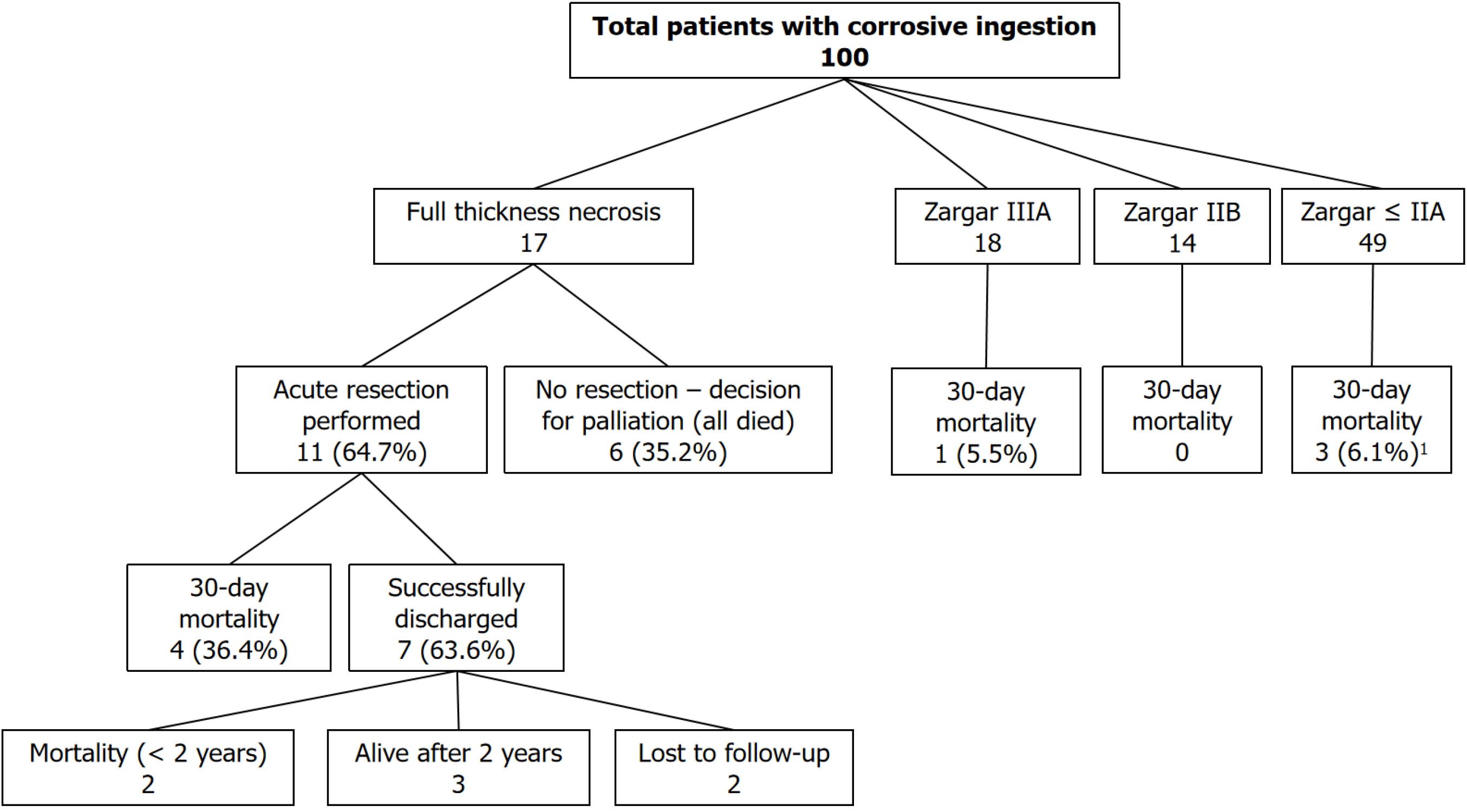
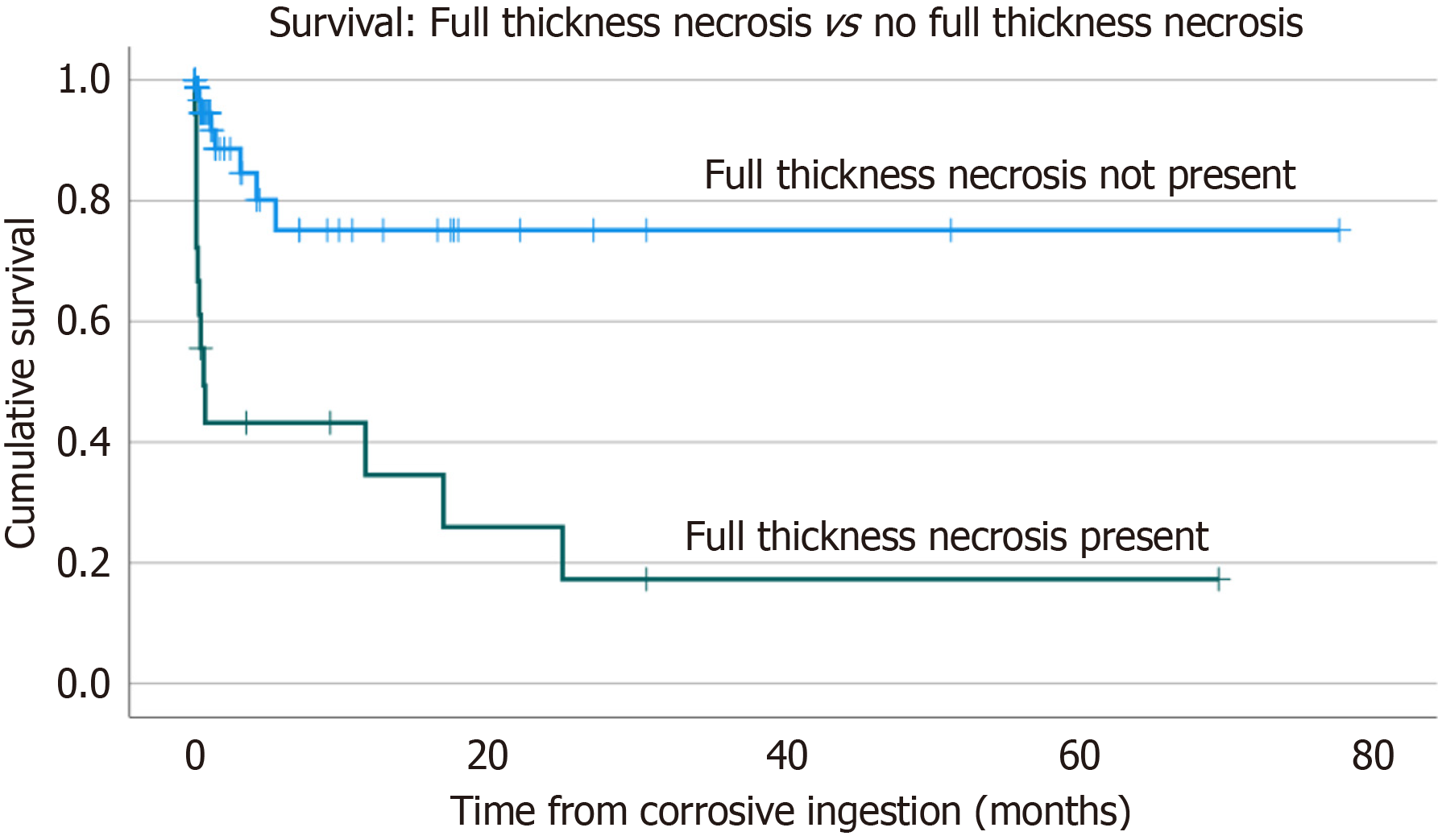
One-hundred patients were included, with a mean age of 32 years (SD: 11.2 years) and a male predominance (65.0%). The majority (73.0%) were intentional suicide attempts. Endoscopy on admission was the most frequent initial investigation performed (95 patients), while only 17 were assessed with CT. Seventeen patients had full thickness necrosis at surgery, of which eleven underwent emergency resection and six were palliated. Thirty-day morbidity and mortality were 27.0% and 14.0%, respectively. Patients with full thickness necrosis and those with an established perforation had a 30-day mortality of 58.8% and 91.0%, respectively. Full thickness necrosis was associated with a cumulative 2-year survival of only 17.6%. Multivariate analyses with ROC AUC showed admission endoscopy findings, CT findings, and blood gas findings (pH, base excess, lactate), to all have significant predictive value for full thickness necrosis, with endoscopy proving to have the best predictive value (AUC 0.850). CT and endoscopy findings were the only factors predictive of early mortality, with CT performing better than endoscopy (AUC 0.798 vs 0.759).
Intentional corrosive injuries result in devastating morbidity and mortality. Locally, early endoscopy remains the mainstay of severity assessment, but referral for CT imaging should be considered especially when blood gas findings are abnormal.
Core Tip: Management of acute adult corrosive injuries remains internationally under-reported, but specifically in sub-Saharan Africa. This large series of 100 patients highlights the high rates of morbidity and mortality, especially when full thickness necrosis is established. Predicting necrosis on admission is challenging, with international guidelines proposing computed tomography (CT) as the investigation of choice. With limited availability of CT, endoscopy still performs well in our setting. CT should be considered in patients with suspected severe corrosive injury with abnormal findings on blood gas (pH, base excess, and lactate) serving as accurate and practical markers of severity in a low-resource setting.
- Citation: Scriba MF, Jonas E, Chinnery GE. Predicting full-thickness necrosis in adult acute corrosive ingestion injuries in a sub-Saharan African setting. World J Gastrointest Pharmacol Ther 2024; 15(6): 99097
- URL: https://www.wjgnet.com/2150-5349/full/v15/i6/99097.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v15.i6.99097
Corrosive ingestion injuries remain a global problem with significant rates of associated morbidity and mortality[1]. A bimodal distribution, which includes paediatric injuries (which are mostly accidental) and adult injuries (which are mostly intentional) result in injuries of differing severity[2]. Management focuses on both the acute emergency mana
Data on corrosive injuries from sub-Saharan Africa (SSA) is limited and focuses predominantly on the management of paediatric injuries and chronic oesophageal strictures[6-12]. Management of acute adult injuries is almost completely undescribed in SSA, but one recent cohort highlights the significant challenges these injuries pose in a low resource setting, with a predominantly young, male demographic with intentional ingestion and limited use of CT imaging for acute assessment[13].
This study was performed to review the severity, management, and outcomes of acute corrosive ingestion injuries in a low resource SSA setting and to identify predictive factors of full thickness necrosis and short-term mortality.
All adult patients managed for corrosive ingestion-related gastrointestinal injuries at Groote Schuur Hospital by the Upper Gastrointestinal Surgery Unit between March 1, 2017–October 31, 2023 were analysed for inclusion. Exclusions included patients managed during this period for only the chronic sequelae of corrosive ingestion and those where acute management data was lacking (e.g. managed initially at another institution). Data were retrospectively analysed from an ethically approved prospectively maintained corrosive injury registry (HREC REF: R009/2022) with study approval by the University of Cape Town Human Research Ethics Committee (HREC REF: 347/2022)
All patients presenting after an acute corrosive ingestion are assessed and managed as per the Advanced Trauma Life Support principles[14]. Assessment of injury severity is by either endoscopy or computed tomography (this is decided by imaging availability and by the initial treating physician). Early contrast swallow assessments are not advocated in our service. Patients with suspected full thickness necrosis are expedited to theatre for operative assessment.
Groote Schuur Hospital is one of two tertiary academic referral centres for several public regional hospitals in the Western Cape province, which has an estimated population of over 7 million[15]. The hospital also accepts self-referred patients who live within the surrounding suburbs of the hospitals. CT imaging facilities are available 24 hours a day at Groote Schuur Hospital but not at all the referring hospitals, while upper gastrointestinal endoscopy is generally avai
The main outcomes analysed were 30-day mortality and morbidity (i.e. 30 days from the corrosive ingestion incident).
Endoscopic grading of acute corrosive injuries was performed using the modified Zargar classification[16]. CT grading was performed according to the CT grading published by Chirica et al[1] (Table 1).
| Modified Zargar endoscopic grading[1] | |
| Grade 0 | Normal |
| Grade I | Oedema and hyperaemia of mucosa |
| Grade IIA | Superficial localised ulcerations, friability and blisters |
| Grade IIB | Circumferential and deep ulcerations |
| Grade IIIA | Multiple and deep ulcerations and small, scattered areas of necrosis |
| Grade IIIB | Extensive necrosis |
| Grade IV | Perforation |
| CT grading[2] | |
| Grade 1 | Normal appearance |
| Grade 2 | Wall and soft tissue oedema, increased wall enhancement |
| Grade 3 | Transmural necrosis with absent wall enhancement (with or without perforation) |
Data analysis was performed using Microsoft Excel and IBM SPSS Statistics (version 29.0.0.0). Patient demographics, corrosive ingestion details, initial investigations, management, and short-term outcomes were described using simple descriptive statistics, with mean ± SD for parametric data and median with inter-quartile range for non-parametric data. Survival data of those patients with full thickness necrosis and those without were compared and presented using Kaplan-Meier curves. Multivariate analysis was performed to assess for any factors associated with full thickness necrosis and 30-day mortality using the Chi-squared test for univariate categorical data and Kruskal-Wallis test to allow for comparison of multiple groups with non-parametric data. Furthermore, post-hoc multiple comparison analyses using the Mann-Whitney U test were performed on any variables shown to be statistically significant. Performance of endoscopy, CT grading and blood gas parameters (pH, base excess, and lactate) were further analysed to assess specificity, sen
During the 80-month study period a total of 126 patients with corrosive ingestion-related injuries were treated, of which 100 patients met the inclusion criteria. The mean age was 32 years (SD: 11.2 years) with most being male (65.0%). Two-thirds had no known medical comorbidities, with 15% known with a prior psychiatric history. Forty-one patients re
| Baseline demographics (n = 100) | n | % |
| Gender | ||
| Female | 35 | 35.0 |
| Male | 65 | 65.0 |
| Comorbidities | ||
| No | 67 | 67.0 |
| Yes | 33 | 33.0 |
| Specified comorbidities | ||
| Known psychiatric history | 15 | 15.0 |
| HIV positive | 12 | 12.0 |
| Hypertension | 2 | 2.0 |
| Obesity | 3 | 3.0 |
| Diabetes mellitus | 1 | 1.0 |
| Other comorbidity | 7 | 7.0 |
| Substance use | ||
| No | 59 | 59.0 |
| Yes | 41 | 41.0 |
| Substance use specified | ||
| Smoking | 31 | 31.0 |
| Alcohol - regular use | 21 | 21.0 |
| Marijuana | 10 | 10.0 |
| Methamphetamine | 8 | 8.0 |
| Methaqualone | 7 | 7.0 |
| Opioids | 1 | 1.0 |
| Prior corrosive ingestion/suicide attempt | ||
| Yes | 11 | 11.0 |
| No | 89 | 89.0 |
| Corrosive ingestion incident (n = 100) | ||
| Intentional/accidental | ||
| Intentional (suicidal) | 73 | 73.0 |
| Accidental | 20 | 20.0 |
| Forced ingestion (assault) | 5 | 5.0 |
| Unknown | 2 | 2.0 |
| Substance ingested | ||
| Acid | 32 | 32.0 |
| Sulphuric acid | 22 | |
| Hydrochloric acid | 3 | |
| Other acid | 7 | |
| Alkali | 58 | 58.0 |
| Sodium hypochlorite (bleach) | 30 | |
| Sodium hydroxide | 27 | |
| Other alkali | 3 | |
| Other corrosive substance | 10 | 10.0 |
| Unknown corrosive substance | 5 | 5.0 |
Most of the ingested substances were alkaline solutions, with bleach (30%) being the most common (Table 3). Almost three quarters (73%) of patients ingested the corrosive in a suicide attempt, 20% were accidental ingestions while five patients were forced to drink corrosive ingestions during assaults. In 20 patients additional non-corrosive substances were ingested, which included toxins in 13 patients, painkillers, and medication in five patients, washing powder, and a non-corrosive cleaning agent. Ingested toxins included alcohol, rat poison, mercury, and organophosphate.
| Imaging/endoscopy during acute admission (n = 100) | n | % | n | % | n | % |
| Endoscopy | 95 | 95.0 | ||||
| Chest X-ray | 82 | 82.0 | ||||
| Lateral neck X-ray | 31 | 31.0 | ||||
| CT | 17 | 17.0 | ||||
| Contrast swallow | 1 | 1.0 | ||||
| None | 1 | 1.0 | ||||
| Endoscopy findings (n = 95) | n | % | n | % | n | % |
| Oesophagus | Stomach | Duodenum | ||||
| Not entered | 1 | 1.1 | 3 | 3.2 | 32 | 33.7 |
| Zargar 0 | 23 | 24.2 | 14 | 14.7 | 42 | 44.2 |
| Zargar I | 11 | 11.6 | 25 | 26.3 | 9 | 9.5 |
| Zargar IIA | 20 | 21.1 | 14 | 14.7 | 7 | 7.4 |
| Zargar IIB | 26 | 27.4 | 8 | 8.4 | 1 | 1.1 |
| Zargar IIIA | 6 | 6.3 | 16 | 16.8 | 1 | 1.1 |
| Zargar IIIB | 8 | 8.4 | 14 | 14.7 | 3 | 3.2 |
| Zargar IV | 0 | 0.0 | 1 | 1.1 | 0 | 0.0 |
| CT findings (n = 17) | n | % | n | % | ||
| Oesophagus | Stomach | |||||
| Grade 1 - normal | 2 | 11.8 | 5 | 29.4 | ||
| Grade 2 - oedematous only | 11 | 64.7 | 8 | 47.1 | ||
| Grade 3 - lack of contrast enhancement | ||||||
| Without perforation | 3 | 17.6 | 2 | 11.8 | ||
| With perforation | 1 | 5.9 | 2 | 11.8 | ||
Early endoscopy was the most prevalent investigation performed with 95 patients assessed at a median time of 24 (IQR 15-40) hours post ingestion. In 7 patients (7.4%) the initial endoscopy was performed more than 72 hours post corrosive ingestion. There were no documented perforations occurring during endoscopy in our cohort. Only 17 patients were assessed using CT, of which 14 also had an endoscopy. In only three patients was the injury severity assessed on CT findings only. A chest X-ray (CXR) was performed on admission in 82 patients with 78 (95.1%) being normal and the other four showing non-specific lung changes. No CXR showed features confirming a perforation and no CXR directly influenced the acute corrosive management. Only one patient underwent a contrast swallow study as part of the acute severity assessment, which was reported as normal.
Twenty-three patients (23.0%) required emergency resuscitation on initial presentation, nineteen of whom necessitated endotracheal intubation for a threatened airway (Table 4). Initial management prior to referral included prophylactic antibiotics in 7.0%, activated charcoal in four patients (of which only one had an actual concomitant toxin overdose warranting the use of activated charcoal). No patient was managed with a pH neutralizing agent. One-fifth (20 patients) required acute surgery, of which 17 were found to have full thickness necrosis. The remaining three patients included two patients needing surgical feeding access (gastrostomy or jejunostomy) and one patient with a negative laparotomy. Eleven underwent an emergency resection, while the remaining six patients had such extensive injuries that an intra-operative decision was made to palliate (Figure 1). Resections performed included oesophagogastrectomy in five patients and total gastrectomy in five. One patient had an oesophagectomy without gastrectomy. In two patients extended resections were performed (additional to gastric or oesophageal resections), which included pancreas-preserving duode
| Management | ||
| Median (IQR) time from ingestion to first healthcare assessment | 6 (2-13) hours | |
| Emergency resuscitation | n | % |
| Required emergency resuscitation | 23 | 23.0 |
| Specified | ||
| Endotracheal intubation | 19 | 19.0 |
| Chest compressions | 1 | 1.0 |
| Inotropes | 3 | 3.0 |
| Other1 | 2 | 2.0 |
| Other management initiated in the emergency department | ||
| Proton pump inhibitor therapy | 35 | 35.0 |
| Prophylactic antibiotics | 7 | 7.0 |
| Therapeutic antibiotics | 4 | 4.0 |
| Nasogastric tube insertion (for drainage, not feeding) | 4 | 4.0 |
| Activated charcoal administration | 4 | 4.0 |
| Steroids | 1 | 1.0 |
| Neutralizing agent | 0 | 0.0 |
| Surgery | ||
| Required acute surgery | 20 | 20.0 |
| Decision for needing surgery (n = 20) | ||
| Based on endoscopy findings | 13 | 65.0 |
| Based on CT findings | 5 | 25.0 |
| Based on clinical findings only | 2 | 10.0 |
| Type of surgery (n = 20) | ||
| Emergency resection performed | 11 | 55.0 |
| Oesophagectomy only | 1 | |
| Oesophagogastrectomy | 5 | |
| Gastrectomy only | 5 | |
| Extended resections2 | 2 | |
| Exploration only - decision for palliation | 6 | 30.0 |
| Feeding jejunostomy (only) | 1 | 5.0 |
| Gastrojejunostomy & gastrostomy | 1 | 5.0 |
| Negative laparotomy | 1 | 5.0 |
Thirty-day mortality was 14.0%, with 27.0% having a documented morbidity within 30 days of the corrosive ingestion (Table 5). Nosocomial pneumonia, acute kidney injury and unexpected cardiac arrest were the most common morbidities. One quarter (26.0%) of patients required intensive care admission within 30 days of the corrosive ingestion. Patients found to have full thickness necrosis had a 30-day mortality of 58.8% (including patients selected for palliation) while those who underwent an acute resection had a 30-day mortality of 36.4%. Eleven patients were found to have an already-established perforation at surgery. Of these, 10 (91.0%) died, with the only survivor being a patient who initially had a reassuring CT with modified Zagar grade IIB caustic injury on endoscopy. Following increasing septic markers and pyrexia an oesophagectomy on day 7 after the ingestion was performed for delayed full-thickness perforation, with localized mediastinitis. Patients who underwent an acute resection had a median length of hospital stay for their primary admission of 28 (IQR 19-137.5) days. Kaplan-Meier survival curves show a significant survival difference between those patients with full thickness necrosis and those without. Full thickness necrosis was associated with a cumulative survival of only 17.6% at 2 years (Figure 2).
| Outcomes (n = 100) | n | % |
| 30-day mortality | 14 | 14.0 |
| 30-day morbidity | 27 | 27.0 |
| Required ICU management | 26 | 26.0 |
| Median (IQR) ICU stay | 2.5 (2-3.25) days | |
| Median (IQR) length of hospital stay | 6 (2-15.5) days | |
| Acute morbidities specified (n = 39) | ||
| Pneumonia (nosocomial) | 7 | 17.9 |
| Acute kidney injury | 5 | 12.8 |
| Cardiac arrest (unexpected) | 4 | 10.3 |
| Refeeding syndrome | 3 | 7.7 |
| Systemic sepsis | 2 | 5.1 |
| Unplanned extubation | 2 | 5.1 |
| Surgical site infection | 2 | 5.1 |
| Other | 14 | 35.9 |
Multivariate analysis with ROC AUC as predictive of necrosis and mortality, showed that Zargar IIIB findings, grade 3 CT findings, pH, base excess, and lactate to all have good predictive performance for full thickness necrosis, with endoscopy proving to have the best predictive performance (AUC 0.850) (Table 6). CT and endoscopy findings were the only factors predictive of short-term mortality, with CT performing better than endoscopy (AUC 0.798 vs 0.759). Blood gas parameters (pH, base excess and lactate) were further analysed in the whole cohort, but also separately in patients without concomitant toxin ingestion (where blood gas findings may be falsely abnormal due to the toxin and not the corrosive substance). After excluding patients with additional toxin ingestion, both pH and base excess had a 100% negative predictive value for full thickness necrosis. In addition, an abnormal base excess (< 2 mEq/L) had excellent predictive value for full thickness necrosis with a ROC AUC of 0.821 (Table 7).
| Variables | Predicting full thickness necrosis | Predicting acute mortality | ||||||||||||
| Total, n | No FT necrosis | FT necrosis | P value | ROC AUC | No mortality | Mortality | P value | ROC AUC | ||||||
| Gender | Female | 35 | 31 | 88.6 | 4 | 11.4 | 0.279 | 28 | 80.0 | 7 | 20.0 | 0.207 | ||
| Male | 65 | 52 | 80 | 13 | 20 | 58 | 89.2 | 7 | 10.8 | |||||
| At least one comorbidity | No | 67 | 58 | 86.6 | 9 | 13.4 | 0.178 | 56 | 83.6 | 11 | 16.4 | 0.323 | ||
| Yes | 33 | 25 | 75.8 | 8 | 24.2 | 30 | 90.9 | 3 | 9.1 | |||||
| Known psychiatric history | No | 85 | 71 | 83.5 | 14 | 16.5 | 0.739 | 72 | 84.7 | 13 | 15.3 | 0.377 | ||
| Yes | 15 | 12 | 80 | 3 | 20 | 14 | 93.3 | 1 | 6.7 | |||||
| Known HIV positive | No | 88 | 75 | 85.2 | 13 | 14.8 | 0.11 | 74 | 84.1 | 14 | 15.9 | 0.138 | ||
| Yes | 12 | 8 | 66.7 | 4 | 33.3 | 12 | 100.0 | 0 | 0.0 | |||||
| Prior corrosive/suicide attempt | No | 89 | 75 | 84.3 | 14 | 15.7 | 0.339 | 77 | 86.5 | 12 | 13.5 | 0.673 | ||
| Yes | 11 | 8 | 72.7 | 3 | 27.3 | 9 | 81.8 | 2 | 18.2 | |||||
| Needing endotracheal intubation | No | 82 | 71 | 86.6 | 11 | 13.4 | 0.043 | 0.604 | 69 | 84.1 | 13 | 15.9 | 0.257 | |
| Yes | 18 | 12 | 66.7 | 6 | 33.3 | 17 | 94.4 | 1 | 5.6 | |||||
| Needing chest compressions | No | 99 | 83 | 83.8 | 16 | 16.2 | 0.027 | 0.529 | 85 | 85.9 | 14 | 14.1 | 0.687 | |
| Yes | 1 | 0 | 0 | 1 | 100 | 1 | 100.0 | 0 | 0.0 | |||||
| Needing inotropes/vasopressors | No | 97 | 81 | 83.5 | 16 | 16.5 | 0.447 | 83 | 85.6 | 14 | 14.4 | 0.480 | ||
| Yes | 3 | 2 | 66.7 | 1 | 33.3 | 3 | 100.0 | 0 | 0.0 | |||||
| ≥ Zargar IIIB endoscopic findings | No | 79 | 75 | 94.9 | 4 | 5.1 | < 0.001 | 0.85 | 74 | 93.7 | 5 | 6.3 | < 0.001 | 0.759 |
| Yes | 16 | 4 | 25 | 12 | 75 | 8 | 50.0 | 8 | 50.0 | |||||
| Grade 3 CT Findings | No | 12 | 10 | 83.3 | 2 | 16.7 | 0.016 | 0.788 | 11 | 91.7 | 1 | 8.3 | 0.026 | 0.798 |
| Yes | 5 | 1 | 20 | 4 | 80 | 2 | 40.0 | 3 | 60.0 | |||||
| Age (years) | 100 | 31 (24-38) | 39 (30-50) | 0.015 | 0.687 | 32 (24-40) | 31 (25-40) | 0.917 | ||||||
| Systolic BP (mmHg) | 48 | 134 (114-143) | 129 (113-149) | 0.926 | 130 (113-144) | 134 (120-137) | 0.919 | |||||||
| Diastolic BP (mmHg) | 48 | 80 (73-90) | 83 (75-97) | 0.309 | 82 (73-90) | 79 (64-91) | 0.520 | |||||||
| Heart rate (beats per minute) | 48 | 94 (79-109) | 86 (72-105) | 0.405 | 93 (76-110) | 94 (82-107) | 0.965 | |||||||
| Urea (mmol/L) | 79 | 4.6 (3.3-5.9) | 5.1 (2.7-7.1) | 0.686 | 4.7 (3.2-6.5) | 3.9 (3.4-5.4) | 0.432 | |||||||
| Creatinine (umol/L) | 88 | 70 (57-81) | 84 (68-102) | 0.038 | 0.666 | 72 (58-85) | 72 (66-84) | 0.892 | ||||||
| WCC (× 109/L) | 85 | 14.07 (9.58-18.31) | 13.80 (9.76-19.16) | 0.695 | 13.79 (9.59-18.31) | 15.75 (10.63-20.50) | 0.605 | |||||||
| Platelets (× 109/L) | 81 | 253 (210-326) | 206 (171-266) | 0.045 | 0.666 | 245 (194-308) | 263 (232-375) | 0.142 | ||||||
| Calcium (mmol/L) | 12 | 2.21 (2.00-2.35) | 1.99 (199-1.99) | 0.31 | 2.15 (1.99-2.35) | 2.21 (2.21-2.21) | 0.885 | |||||||
| pH | 41 | 7.37 (7.31-7.42) | 7.13 (7.07-7.35) | 0.003 | 0.823 | 7.35 (7.17-7.40) | 7.36 (7.27-7.43) | 0.593 | ||||||
| Base excess (mEq/L) | 40 | -0.50 (-5.50-2.10) | -14.20 (-17.00 to -4.60) | 0.004 | 0.819 | -3.2 (-12.1-0.65) | 2.45 (-0.58-5.38) | 0.020 | 0.199 | |||||
| Lactate (mmol/L) | 40 | 1.80 (1.20-3.30) | 3.20 (2.60-4.45) | 0.026 | 0.746 | 2.45 (1.20-3.55) | 1.55 (1.18-3.48) | 0.677 | ||||||
| Ingestion to first assessment (hours) | 94 | 6.0 (2.5-14.5) | 4.0 (2.0-8.5) | 0.209 | 6.0 (3.0-15.5) | 3.0 (1.5-6.5) | 0.052 | |||||||
| Total | FT necrosis | Not FT necrosis | Sensitivity, % | Specificity, % | PPV, % | NPV, % | P value | ROC AUC | |
| Endoscopy performance (n = 95) | |||||||||
| Zargar IIIB | 16 | 12 | 4 | 75.0 | 94.9 | 75.0 | 94.5 | < 0.001 | 0.850 |
| CT performance (n = 17) | |||||||||
| CT grade 3 | 5 | 4 | 1 | 66.7 | 90.9 | 80.0 | 83.3 | 0.026 | 0.788 |
| Blood gas performance (n = 40) | |||||||||
| pH < 7.35 | 20 | 7 | 13 | 77.8 | 58.1 | 35.0 | 90.0 | 0.062 | 0.679 |
| BE < -2 mEq/L | 18 | 7 | 11 | 77.8 | 64.5 | 38.9 | 90.9 | 0.027 | 0.711 |
| Lactate > 2.0 mmol/L | 21 | 8 | 13 | 88.9 | 58.1 | 38.1 | 94.7 | 0.014 | 0.735 |
| Blood gas performance (Patients with concomitant toxin ingestion removed) (n = 35) | |||||||||
| pH < 7.35 | 19 | 7 | 12 | 77.8 | 58.1 | 35.0 | 100.0 | 0.007 | 0.786 |
| BE < -2 mEq/L | 17 | 7 | 10 | 77.8 | 58.1 | 35.0 | 100.0 | 0.003 | 0.821 |
| Lactate > 2.0 mmol/L | 18 | 6 | 12 | 77.8 | 58.1 | 35.0 | 94.1 | 0.046 | 0.714 |
Corrosive ingestion injuries remain a difficult clinical problem in our setting. Demographics in this series closely resemble those reported by Mthethwa et al[13] also from South Africa, with a low mean age and significant male predominance. Case series from Europe (United Kingdom and France) show a different demographic with a median age approximately 10 years older than in the South African setting and a more equal gender distribution[2,5,17]. As seen in most studies on adult corrosive injuries, intentional suicide attempts remain the most common reason for the ingestion. The majority of patients in this series were not known with a prior psychiatric history, unlike results from international series, such as Challine et al[17] who reported 71.8% of patients having been known with a prior psychiatric history. Five patients in our series were forced to drink a corrosive substance as part of an assault, one of which resulted in severe corrosive pneumonitis and the need for extracorporeal membrane oxygenation. Corrosive assault is not well described and pro
Decision-making in the emergency setting revolves around the need for surgical resection. Patient selection is crucial and remains difficult. Delays to resection result in significantly worse outcomes, while unnecessary resections, especially oesophagectomy, carry a significant morbidity and even mortality. CT is now considered in many centres, and by international guidelines, to be superior in selecting patients for resection[1,4,19-21]. Some centres now rely on CT grading only in the emergency setting with endoscopy considered obsolete[5]. Management of severe corrosive injuries may require extended foregut resections and in patients with staged procedures technically demanding delayed reconstructions with high complication rates and poor eventual quality of life[1]. Improving outcomes in these patients is best achieved by management in centralised high-volume centres with access to not only surgery but also minimally invasive interventions[2,17].
CT utilisation in our study, as well as the study by Mthethwa et al[13], was low. This is likely due to a combination of lack of emergency 24-hour access to CT imaging, but also a lack of awareness of the usefulness of CT grading for acute corrosives. It is not clear how many acute corrosive injures were seen within the drainage area during the study period in total, as minor cases have been managed at peripheral hospitals and are not included in this study. Most of these hospitals have 24-hour access to endoscopy but not CT imaging. Non-selective referrals of all corrosive ingestion patients will result in significant strain to an already overburdened tertiary facility. Selective referral of patients with suspected full thickness necrosis is crucial and should be expedited to allow resection before foregut perforation occurs. Perforation prior to surgery in our setting is invariably fatal.
Although plain radiography (CXR or lateral neck X-rays) and basic admission blood tests (full blood count and renal function with electrolytes) are routinely performed the results are of limited value in the acute management. Blood gas parameters (pH, base excess, and serum lactate) were the most useful blood tests to predict necrosis while endoscopy and CT both performed well as imaging modalities. Locally, a blood gas (which is relatively cheap, easy to perform and readily available at almost all emergency centres) can aid in selecting patients for referral for CT assessment.
Although not used for the acute injury severity assessment in some international centres, we still consider endoscopy to be a very useful investigation (especially in patients without necrosis). We recommend that early endoscopy should be considered in all patients who do not have evidence of full thickness necrosis on CT. It must be highlighted that initial reassuring CT and endoscopic findings in severe corrosive cases do not replace close clinical observation, as delayed perforation can still occur, as was evident in one patient in our series who had an oesophageal perforation diagnosed one week after the ingestion incident[22,23].
The limitations of this study include the retrospective nature of the data analysis and the low patient numbers who had CT imaging compared to endoscopy which may have compromised the accuracy of ROC curves and predictive models for CT grading. Lack of data on these injuries in SSA hampers preventive health strategies and even in our setting it is unclear how many of these injuries are seen within the catchment area, but outside of our centre. Further research with multi-centre collaboration would generate larger patient numbers and give a more robust assessment of the full extent of this problem.
Acute corrosive ingestion in adults may result in devastating injuries and remains a condition poorly described in SSA. Acute management success hinges on accurate and timeous identification of full thickness necrosis and early surgical resection. CT is the most accurate tool to achieve this, but in resource-constrained environments is not readily available. Endoscopy thus remains an important and invaluable tool. We propose using blood gas findings to select patients who should be acutely referred to an academic centre for emergency CT imaging and assessment for surgical resection.
| 1. | Chirica M, Bonavina L, Kelly MD, Sarfati E, Cattan P. Caustic ingestion. Lancet. 2017;389:2041-2052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 102] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 2. | Di Maggio F, Vergani V, Tomasi I, Zhang C, Gossage J, Botha A, Baker C. Assessment and management after corrosive ingestion: when is specialist centre referral needed? A 10-year UK experience. Surg Endosc. 2022;36:5753-5765. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Zargar SA, Kochhar R, Nagi B, Mehta S, Mehta SK. Ingestion of corrosive acids. Spectrum of injury to upper gastrointestinal tract and natural history. Gastroenterology. 1989;97:702-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 115] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Chirica M, Kelly MD, Siboni S, Aiolfi A, Riva CG, Asti E, Ferrari D, Leppäniemi A, Ten Broek RPG, Brichon PY, Kluger Y, Fraga GP, Frey G, Andreollo NA, Coccolini F, Frattini C, Moore EE, Chiara O, Di Saverio S, Sartelli M, Weber D, Ansaloni L, Biffl W, Corte H, Wani I, Baiocchi G, Cattan P, Catena F, Bonavina L. Esophageal emergencies: WSES guidelines. World J Emerg Surg. 2019;14:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 139] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 5. | Assalino M, Resche-Rigon M, Corte H, Maggiori L, Zagdanski AM, Goere D, Sarfati E, Cattan P, Chirica M. Emergency computed tomography evaluation of caustic ingestion. Dis Esophagus. 2022;35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Seydou T, Abdoulaye OM, Xing L, Zi SZ, Sekou K, Wen YS, Ibrahim S, Sekou TC, Boubacar MI, Saye J, Jerome DD, Dantoumé TO, Sadio Y. [Endoscopic contribution in the dilatation of caustic esophagus stenosis]. Pan Afr Med J. 2016;23:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Contini S, Scarpignato C, Rossi A, Strada G. Features and management of esophageal corrosive lesions in children in Sierra Leone: lessons learned from 175 consecutive patients. J Pediatr Surg. 2011;46:1739-1745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Contini S, Tesfaye M, Picone P, Pacchione D, Kuppers B, Zambianchi C, Scarpignato C. Corrosive esophageal injuries in children. A shortlived experience in Sierra Leone. Int J Pediatr Otorhinolaryngol. 2007;71:1597-1604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Weldon E, Martey PM. Caustic soda poisoning in Ghana--an alarming increase. Paediatr Int Child Health. 2012;32:158-160. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Botwe BO, Anim-Sampong S, Sarkodie BD, Antwi WK, Obeng-Nkansah J, Ashong GG. Caustic soda ingestion in children under-5 years presenting for fluoroscopic examinations in an Academic Hospital in Ghana. BMC Res Notes. 2015;8:684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Adedeji TO, Tobih JE, Olaosun AO, Sogebi OA. Corrosive oesophageal injuries: a preventable menace. Pan Afr Med J. 2013;15:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Okugbo SU, Anyanhun GA, Efobi CA, Okugbo OT. Presentation and management outcome of childhood corrosive oesophageal injury in Benin City. Afr J Paediatr Surg. 2020;17:74-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 13. | Mthethwa AN, Govender M, Clarke DL. Adult corrosive ingestions in the Pietermaritzburg Metropolitan Surgical Service. S Afr J Surg. 2023;61:144-149. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Galvagno SM Jr, Nahmias JT, Young DA. Advanced Trauma Life Support(®) Update 2019: Management and Applications for Adults and Special Populations. Anesthesiol Clin. 2019;37:13-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 160] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 15. | Statistics South Africa. South African National Census 2022. Available from: https://census.statssa.gov.za/#/. |
| 16. | Zargar SA, Kochhar R, Mehta S, Mehta SK. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc. 1991;37:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 278] [Article Influence: 8.2] [Reference Citation Analysis (2)] |
| 17. | Challine A, Maggiori L, Katsahian S, Corté H, Goere D, Lazzati A, Cattan P, Chirica M. Outcomes Associated With Caustic Ingestion Among Adults in a National Prospective Database in France. JAMA Surg. 2022;157:112-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Matzopoulos R, Prinsloo MR, Mhlongo S, Marineau L, Cornell M, Bowman B, Mamashela TA, Gwebushe N, Ketelo A, Martin LJ, Dekel B, Lombard C, Jewkes R, Abrahams N. South Africa's male homicide epidemic hiding in plain sight: Exploring sex differences and patterns in homicide risk in a retrospective descriptive study of postmortem investigations. PLOS Glob Public Health. 2023;3:e0002595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Chirica M, Resche-Rigon M, Pariente B, Fieux F, Sabatier F, Loiseaux F, Munoz-Bongrand N, Gornet JM, Brette MD, Sarfati E, Azoulay E, Zagdanski AM, Cattan P. Computed tomography evaluation of high-grade esophageal necrosis after corrosive ingestion to avoid unnecessary esophagectomy. Surg Endosc. 2015;29:1452-1461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Chirica M, Resche-Rigon M, Zagdanski AM, Bruzzi M, Bouda D, Roland E, Sabatier F, Bouhidel F, Bonnet F, Munoz-Bongrand N, Marc Gornet J, Sarfati E, Cattan P. Computed Tomography Evaluation of Esophagogastric Necrosis After Caustic Ingestion. Ann Surg. 2016;264:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 21. | Kluger Y, Ishay OB, Sartelli M, Katz A, Ansaloni L, Gomez CA, Biffl W, Catena F, Fraga GP, Di Saverio S, Goran A, Ghnnam W, Kashuk J, Leppäniemi A, Marwah S, Moore EE, Bala M, Massalou D, Mircea C, Bonavina L. Caustic ingestion management: world society of emergency surgery preliminary survey of expert opinion. World J Emerg Surg. 2015;10:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 22. | Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013;19:3918-3930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 273] [Cited by in RCA: 208] [Article Influence: 17.3] [Reference Citation Analysis (7)] |
| 23. | Hall AH, Jacquemin D, Henny D, Mathieu L, Josset P, Meyer B. Corrosive substances ingestion: a review. Crit Rev Toxicol. 2019;49:637-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |