Published online Jan 5, 2022. doi: 10.4292/wjgpt.v13.i1.1
Peer-review started: June 8, 2021
First decision: July 31, 2021
Revised: August 28, 2021
Accepted: January 5, 2022
Article in press: January 5, 2022
Published online: January 5, 2022
Processing time: 215 Days and 11.2 Hours
Inflammatory bowel disease (IBD) is associated with complications, frequent hospitalizations, surgery and death. The introduction of biologic drugs into the therapeutic arsenal in the last two decades, combined with an expansion of immunosuppressant therapy, has changed IBD management and may have altered the profile of hospitalizations and in-hospital mortality (IHM) due to IBD.
To describe hospitalizations from 2008 to 2018 and to analyze IHM from 1998 to 2017 for IBD in Brazil.
This observational, retrospective, ecological study used secondary data on hospitalizations for IBD in Brazil for 2008-2018 to describe hospitalizations and for 1998-2017 to analyze IHM. Hospitalization data were obtained from the Hospital Information System of the Brazilian Unified Health System and population data from demographic censuses. The following variables were analyzed: Number of deaths and hospitalizations, length of hospital stay, financial costs of hospitalization, sex, age, ethnicity and type of hospital admission.
There was a reduction in the number of IBD hospitalizations, from 6975 admissions in 1998 to 4113 in 2017 (trend: y = -0.1682x + 342.8; R2 = 0.8197; P < 0.0001). The hospitalization rate also decreased, from 3.60/100000 in 2000 to 2.17 in 2010. IHM rates varied during the 20-year period, between 2.06 in 2017 and 3.64 in 2007, and did not follow a linear trend (y = -0.0005049x + 2.617; R2 = 0,00006; P = 0.9741). IHM rates also varied between regions, increasing in all but the southeast, which showed a decreasing trend (y = -0.1122x + 4.427; R2 = 0,728; P < 0.0001). The Southeast region accounted for 44.29% of all hospitalizations. The Northeast region had the highest IHM rate (2.86 deaths/100 admissions), with an increasing trend (y = 0.1105x + 1.110; R2 = 0.6265; P < 0.0001), but the lowest hospitalization rate (1.15). The Midwest and South regions had the highest hospitalization rates (3.27 and 3.17, respectively). A higher IHM rate was observed for nonelective admissions (2.88), which accounted for 81% of IBD hospitalizations. The total cost of IBD hospitalizations in 2017 exhibited an increase of 37.5% compared to 2008.
There has been a notable reduction in the number of hospitalizations for IBD in Brazil over 20 years. IHM rates varied and did not follow a linear trend.
Core Tip: This study provides an epidemiological profile of IBD hospitalizations in Brazil from 2008 to 2018 and analyzes in-hospital mortality (IHM) between 1998 and 2017. There was a reduction from 6975 hospital admissions in 1998 to 4113 in 2017 (trend: y = -0.1682x + 342.8; R2 = 0.8197; P < 0.0001). The hospitalization rate decreased from 3.60/100000 in 2000 to 2.17 in 2010. The total cost of hospitalizations in 2017 showed an increase of 37.5% compared to 2008. IHM rates varied during the 20-year period and did not follow a linear trend, decreasing in the Southeast region but increasing in the Northeast region.
- Citation: Guedes ALV, Lorentz AL, Rios LFAR, Freitas BC, Dias AGN, Uhlein ALE, Vieira Neto FO, Jesus JFS, Torres TSN, Rocha R, Andrade VD, Santana GO. Hospitalizations and in-hospital mortality for inflammatory bowel disease in Brazil. World J Gastrointest Pharmacol Ther 2022; 13(1): 1-10
- URL: https://www.wjgnet.com/2150-5349/full/v13/i1/1.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v13.i1.1
Inflammatory bowel disease (IBD), which is characterized by a chronic and relapsing idiopathic gastrointestinal inflammatory process, includes Crohn’s disease (CD) and ulcerative colitis (UC). IBD pathogenesis is complex and involves multiple factors, such as genetic predisposition, environmental factors, intestinal microbiota and host immune response[1].Despite the unique features of CD and UC related to the extent and location of inflammation, both impact quality of life, which is remarkable considering that they affect young patients[2]. IBD can also be associated with extraintestinal complications, frequent hospitalizations, surgery and death[3]. Hospitalizations in IBD occur mainly for disease activity, diagnostic procedures and surgery. The causes of in-hospital deaths may be IBD complications or nosocomial complications, such as infections and venous thromboembolism[4].
Adequate treatment is essential to avoid complications, and the introduction of biologic drugs into the therapeutic arsenal in the last two decades, combined with an expansion of immunosuppressant therapy, has importantly altered the management of IBD[5]. In Brazil, infliximab [an antagonist of tumor necrosis factor alpha (TNFa)] was introduced as a therapeutic possibility for patients in the early 2000s[6].
Since we have not found any nationwide population-based study on IBD in Brazil in the literature, our study is probably the first, contributing to the analysis of the impact of IBD in the country. In Brazil, there is still no integrated database of patients with IBD, limiting the development of comprehensive epidemiological studies. On the other hand, Unified Health System (SUS) has a hospital admission data collection system that allows partial analysis of the impact of IBD in the country. This article aims to describe the profile of hospitalizations and in-hospital deaths due to IBD in Brazil over 10 years and to analyze in-hospital mortality (IHM) over 20 years.
This observational, retrospective, ecological study aimed to describe the profile of hospitalizations for IBD in Brazil between 2008 and June 2018 (data available in August 2018) and to analyze IHM from 1998 to 2017. Secondary data referring to hospitalizations due to IBD were obtained from the Hospital Information System of the Brazilian SUS (SIH/SUS), Department of Informatics of the Brazilian SUS (DATASUS). Hospitalizations from 1998 to 2007 were not included because not all data were available. We carried out a survey of data from the twenty-year period to make a parallel with the introduction of infliximab in 2002 by the SUS. But the data from 1998 to 2007 are only given by year of processing, which does not include the other data, such as length of stay, costs per stay. The most detailed data in information by SIH/SUS are those from 2008, which are given by year of hospitalization.
The following variables were analyzed: Number of deaths, number of hospitalizations, length of hospital stay, financial costs of hospitalization, sex, age, ethnicity and type of hospital admission (elective or nonelective). The variables were correlated with CD and UC (ICD-10 codes K50 and K51). The database used for this research does not distinguish between CD and UC. The information was obtained from hospital admission authorization forms and cost and exit reports managed by the Ministry of Health and State and Municipal Health Secretariats. IBD was the main diagnosis on the hospital admission authorization forms. The SIH maps hospitalizations only in the public sphere and does not include those with private funding or through private health insurance.
For the geographic analysis, variables were corrected for population numbers in 2000 and 2010, according to region, using the Brazilian Institute of Geography and Statistics (IBGE) database, which provides data regarding the Brazilian population via periodic censuses. The number of available hospital beds can also be obtained from DATASUS.
The data were tabulated and subjected to statistical analysis using Excel®, 2013. The temporal trend in hospitalizations and IHM was evaluated using simple linear regression. For correlation analysis, the Spearman correlation coefficient was used through Free Statistics Software (v1.2.1), 2017. The IHM rate is given as the ratio between the number of IBD-related deaths and the number of hospitalizations due to IBD, multiplied by 100. The costs of hospitalization are presented in Brazilian reals (R$).
The DATASUS database is in the public domain. The approval of the research ethics committee was not required.
From January 2008 to June 2018, 43560 hospitalizations in Brazil were due to IBD, accounting for 0.037% of hospitalizations for all causes. The demographic data are summarized in Table 1. The number of hospitalizations was higher in women, in those of white ethnicity and in those younger than 30 years of age. The IHM rate among ethnic groups was higher in Asian Brazilian patients. In the analyzed period, although more women were hospitalized for IBD, the IHM rate was higher in males.
| Hospitalizations (n) | Hospitalizations (%) | In-hospital mortality rate (per 100 hospitalizations) | |
| Sex | |||
| Female | 23383 | 53.67 | 2.33 |
| Male | 20177 | 46.32 | 2.84 |
| Ethnicity | |||
| White | 18166 | 41.70 | 2.55 |
| Black | 1211 | 2.78 | 2.15 |
| Pardo (mixed-race) | 10432 | 23.95 | 2.37 |
| Brazilian Indian | 44 | 0.10 | 2.27 |
| Asian Brazilian | 316 | 0.72 | 5.38 |
| Unknown | 13391 | 30.74 | 2.72 |
| Age | |||
| < 30 years | 16299 | 37.41 | 0.80 |
| 30-49 years | 13127 | 30.15 | 1.61 |
| 50-64 years | 5534 | 12.70 | 5.02 |
| ≥ 65 years | 6390 | 14.67 | 7.81 |
| Hospital admission | |||
| Nonelective | 35188 | 80.78 | 2.88 |
| Elective | 8358 | 19.19 | 1.28 |
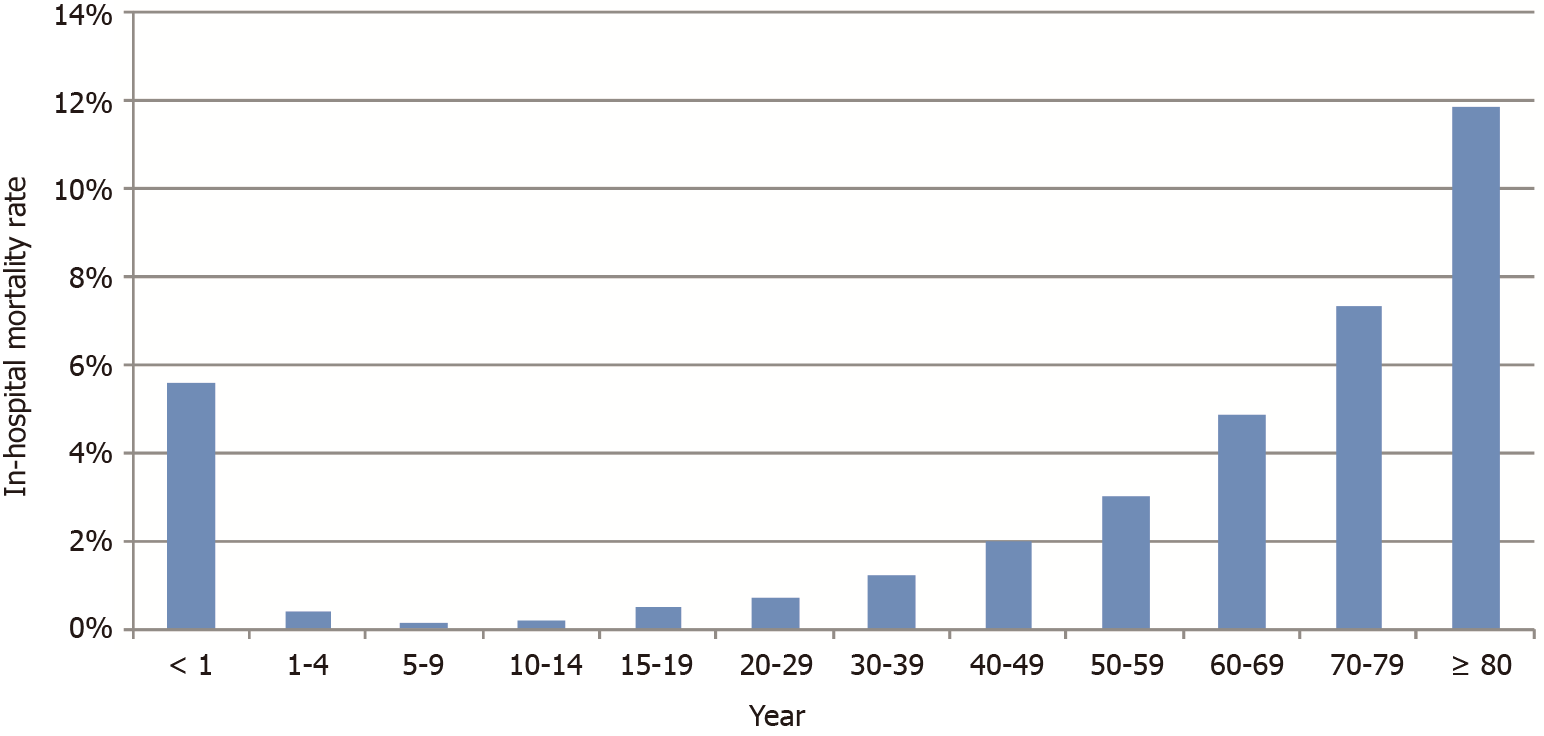
Regarding age groups, the IHM rate grew with age, except in infants younger than one year old; these patients presented an IHM rate similar to that of the elderly, at 5.61/100 hospitalizations (Figure 1).
Data on hospitalizations by region are shown in Table 2. The Southeast region had 44.29% hospitalizations. Although the Northeast region had the highest IHM rate (2.86 deaths per 100 admissions), it had the lowest hospitalization rate for IBD (1.15 hospitalizations per 100000 population). Nonetheless, this region has a small proportion of hospital beds in gastroenterology units and in training gastroenterology units, second only to the North. The Midwest and South regions, on the other hand, showed the highest hospitalization rates. Approximately 81% of hospital admissions were nonelective, and the IHM rate was higher in this type of hospitalization in all regions, except in the North. The Midwest exhibited the lowest mortality rate for elective hospitalizations.
| North | Northeast | Southeast | South | Midwest | Brazil | |
| Hospitalizations | 3364 (7.72) | 7878 (18.08) | 19292 (44.29) | 8988 (20.63) | 4038 (9.27) | 43560 (100) |
| Deaths (n) | 63 | 225 | 503 | 236 | 92 | 1119 |
| In-hospital mortality rate (per 100 hospitalizations) | 1.87 | 2.86 | 2.61 | 2.63 | 2.28 | 2.57 |
| In-hospital mortality rate for elective admissions (per 100 hospitalizations) | 4.23 | 1.38 | 0.99 | 1.37 | 0.96 | 1.28 |
| In-hospital mortality rate for nonelective admissions (per 100 hospitalizations) | 1.53 | 3.34 | 3.11 | 2.75 | 2.52 | 2.88 |
| Mean hospitalization costs (R$) | 467.33 | 663.65 | 834.19 | 736.91 | 476.42 | 721.78 |
| Mean hospitalization costs in elective admissions (R$) | 854.78 | 800.14 | 915.41 | 795.32 | 477.85 | 840.94 |
| Mean hospitalization costs for nonelective admissions (R$) | 411.15 | 618.49 | 808.99 | 731.72 | 476.15 | 693.51 |
| Mean length of hospital stay (days) | 5.4 | 8.9 | 7.3 | 6.6 | 5.9 | 7.1 |
| Mean length of hospital stay for elective admissions (days) | 7.9 | 11 | 7.4 | 6.1 | 5.8 | 8.0 |
| Mean length of hospital stay for nonelective admissions (days) | 5.0 | 8.2 | 7.2 | 6.6 | 5.9 | 6.9 |
| IBD hospitalizations/100000 population1 | 2.06 | 1.15 | 2.33 | 3.17 | 3.27 | 2.17 |
| Hospital beds in gastroenterology units/100,000 population1 | 0.87 | 0.70 | 1.21 | 1.57 | 1.49 | 1.11 |
| Hospital beds in training gastroenterology units/100,000 population1 | 0.25 | 0.20 | 0.72 | 0.77 | 0.48 | 0.53 |
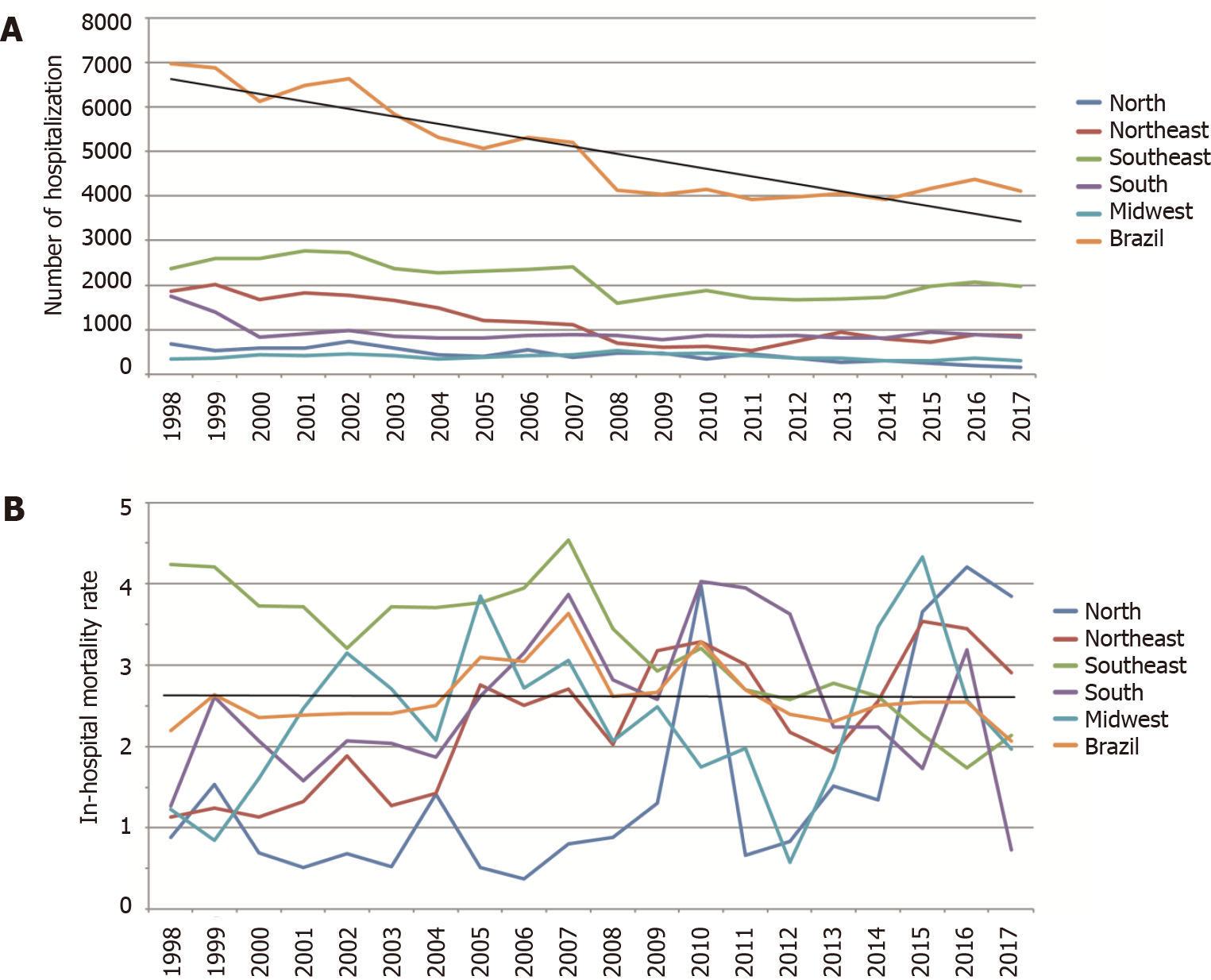
There was a reduction in the number of hospitalizations for IBD over the 20 years (Figure 2A), from 6,975 admissions in 1998 to 4,113 in 2017 (trend: y = -0.1682x + 342.8; R2 = 0.8197; P < 0.0001). The year with the lowest number of hospitalizations was 2014, at 3926. The IBD hospitalization rate was 3.60/100000 in 2000 and decreased to 2.17/100000 in 2010.
IHM rates varied during the 20-year period, between 2.06 in 2017 and 3.64 in 2007, and did not follow a linear trend (y = -0.0005049x + 2.617; R2 = 0,00006; P = 0.9741) (Figure 2B). Analyzing IHM per region, rates increased in all but the Southeast, which showed a decreasing trend (y = -0.1122x + 4.427; R2 = 0,728; P < 0.0001). Conversely, the Northeast displayed an increasing trend (y = 0.1105x + 1.110; R2 = 0.6265; P < 0.0001). In the other regions, IHM rates did not follow a linear trend (North: y = 0.1385x + 0.04941; R2 = 0.4028; P = 0.026; South: y = 0.02891x + 2.205; R2 = 0.035; P = 0.43; Midwest: y = 0.03739X + 1.936; R2 = 0.0536; P = 0.33).
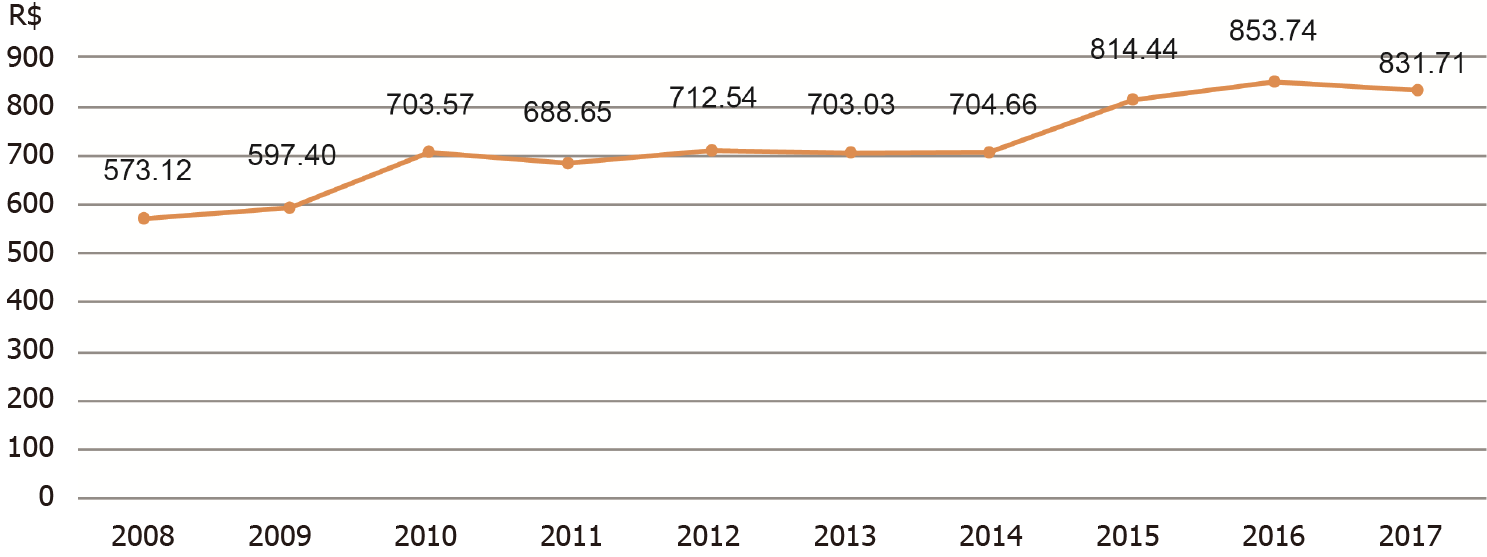
The mean national hospital length of stay was 7.1 d from 2008 to 2018 and remained steady during this period. The average cost of hospitalization exhibited an upward trend from 2008 to 2017 (y = 28.57x + 561.1; R2 = 0.867; P < 0.0001), which was more pronounced from 2009 to 2010 and from 2014 to 2016 (Figure 3), with a total increase of 45.12% from 2008 to 2017. The total cost of IBD hospitalizations in Brazil from 2008 to 2017 was R$ 29433616.56. The total cost in 2017 was R$ 3258401.28, which represents an increase of 37.5% in relation to 2008.
From January 2008 to June 2018, there was no correlation between mean hospitalization costs and IHM (ρ = 0.0107; P = 0.9) or the mean length of hospital stay and IHM (ρ = -0.1604; P = 0.072). The mean length of hospital stay correlated with mean hospitalization costs for all admissions (ρ = 0.4391; P < 0.0001) and for elective (ρ = 0.36; P = 0.0002) and non-elective hospitalizations (ρ = 0.4961, P < 0.0001).
Although our study cannot analyze the incidence and prevalence of IBD in Brazil, we have shown using nationwide IBD hospitalization data that the number of IBD admissions and hospitalization rates is decreasing. Between 1998 and 2017, there was a notable reduction in the number of hospitalizations due to IBD, probably reflecting better patient care. The epidemiology committee of ECCO considers that decreases in the frequency of hospitalization are evidence of improvement in IBD medical management[5].
There was a tendency of reductions in IBD hospitalization rates after the introduction of biologic drugs, with a consequent switch of hospitalization expenses for high-cost medications[3]. However, despite the reduction in the number of hospitalizations in Brazil, total expenditures with hospitalizations for IBD increased by 30% from 2008 to 2018. Perhaps this reflects greater access to exams, procedures or even the need for hospitalization for the application of anti-TNFa. DATASUS data do not differentiate 1-d hospitalizations. The average cost of hospitalization for IBD in USA increased from 2003 to 2008, but remained stable from 2008 to 2014, on the other hand, in Canada, the cost remained increasing from 2000 to 2009[7,8]
European studies show that IBD is one of the most expensive chronic diseases, and it is important to analyze the costs involved with patient care[9]. The difference in hospitalization costs between regions in Brazil is important: while the average cost of hospitalizations in the North is R$ 467.33, it is R$ 834.19 in the Southeast, probably reflecting the greater amount of diagnostic and therapeutic resources available in the latter region.
Hospitalization costs were higher for elective hospitalizations, perhaps reflecting patients admitted for surgical procedures. It may also explain why the average length of hospital stay was longer for elective hospitalizations. As it was expected, the length of hospital stay correlated with average hospitalization costs. The length of stay for elective and nonelective admissions was higher in the Northeast, which may reflect a difficulty in obtaining diagnostic procedures and surgery. The mean length of hospital stay in our study was 7.1, slightly higher than that found in the United States (5.8 d for CD and 6.8 d for UC)[10] and lower than that found in Canada (8.1 d for CD and 10.2 d for UC)[4] and Scotland (9.0 d for CD)[11].
We found a predominance of IBD hospitalizations in women and in the young. This is consistent with several studies from different countries, such as the United States and Canada, and the known incidence of IBD in the second and third decades of life[4,12,13]. Although more women were hospitalized for IBD, the IHM rate was higher in men, as was found in the Ananthakrishnan et al[12] study in the United States.
The Brazil is a country with racial miscegenation and regional differences in racial composition. In our study, IBD hospitalizations predominated among white patients, followed by mixed-race, with a small percentage of blacks, Brazilian Indians and Asian Brazilians. This might be explained by the fact that the white ethnic group is the most prevalent group in the South and Southeast regions, which have the highest number of hospitalizations. Victoria et al[2] also demonstrated a predominance of IBD in whites in the Midwest of São Paulo State during 1986-2005. However, in a study of CD patients in Bahia State in the Northeast, Santana et al[13] found a predominance of mixed-race (43.1%), followed by white (32.3%) and Afro-Brazilians (24.6%). Another study from the Northeast also demonstrated a predominance of mixed-race IBD in 67.9% of IBD patients[14].
The mortality rates due to UC in the 21 different countries from 1951 to 2005 were initially higher than those due to CD but that CD death rates increased until they reached a rate similar to that of UC. Since then, both mortality rates followed a parallel declining course[15].
It is believed that the introduction of anti-TNFa into the therapeutic arsenal has modified the natural course of IBD. Although the findings show an increased risk of death in patients taking immunomodulators, up to 2-fold mortality in patients with CD taking infliximab compared to a general population, there is no consensus regarding any change in mortality[5]. In Brazil, infliximab became a therapeutic possibility in the early 2000s[6].
In Brazil, we found an IHM rate of 7.81% in those ≥ 65 years of age, 2-fold higher than that in Canada and almost 10-fold higher than that among Brazilians under 30 years of age[4]. In our database, IBD was the main diagnosis on hospital admission authorization forms and not the cause of death; thus, our study was unable to elucidate whether the increasing IHM with older age is related to IBD.
It is interesting to note that the IHM rate was much higher (2-fold) in Asian Brazilian patients. The prevalence of IBD in Asia is still lower than that in Western countries, but it is possibly increasing with the westernization of lifestyle[16]. By sharing a western lifestyle, Asian Brazilians would be more likely to develop IBD. Some studies have shown that CD in Asia is as severe or even worse than that in Western countries, with complicated and penetrating diseases[16]. If this is related to a genetic component, it may partially explain the higher rate of IHM in Asian Brazilians.
Nonelective hospitalizations accounted for 81% of all IBD hospitalizations, with an IHM rate higher than 2-fold that of electives, which is expected considering the severity of cases admitted as urgent or emergent. A Scottish study also demonstrated predominance in nonelective admissions in patients with CD (62.5%)[11].
Our analysis of the IHM rate by region revealed an increase in all regions, except in the Southeast, which showed a decreasing trend and where nearly half of hospitalizations occurred. Appropriate treatment of IBD involves specialized knowledge, familiarity with therapeutic options, early recognition of complications, and the need for surgical interventions[12]. Thus, it is expected that geographic regions with higher resources will have lower hospital mortality rates. The main Brazilian regions in descending order by per capita gross domestic product are the Southeast, South, Northeast, Midwest and North[17]. From this perspective, we can initially highlight that the difference in resources between Brazilian regions, as an isolated factor, does not fully explain the contrast between IHM rates.
The Northern region, which includes the greatest part of the Brazilian Amazon forest and is one of the poorest regions, had the lowest IHM rate. Perhaps this occurs because of underreporting or patient transference to other regions. For elective hospitalizations, the North showed a high IHM rate, unlike the rest of the country. The issue of underreporting should be taken into account when using DATASUS. One study analyzed the relevance of the use of the SIH/SUS in the evaluation of quality of care for acute myocardial infarction, observing underreporting in the procedures performed, which interferes with hospitalization cost analyses. There was also underreporting for the number of days of hospitalization[18]. Another study of myocardial infarction reported a higher number of intrahospital deaths registered in the Information System on Mortality than in the SIH/SUS. This occurred due to the absence of the hospital admission authorization form for 32.9% and to underreporting of death in 3.3%[19].
A Canadian study analyzed the mortality of UC patients admitted under specialist care compared to care by other providers, demonstrating that the primary in-hospital care provided by gastroenterologists was associated with lower IHM[20]. In our study, we found that the Midwest and South regions have the largest number of hospital beds in gastroenterology units but that the South and Southeast have the greatest number of hospital beds in training gastroenterology units. This may help to explain the lower IHM compared to the Northeast region.
In Brazil, the South and Southeast regions have the highest IBD hospitalization rates, whereas less industrialized areas (the North, Northeast and Midwest) have the lowest rates. Victoria et al[2] in a study in São Paulo state and Parente et al[14] in a study in Piauí state also reported that most IBD patients live in urban districts. The Northeast region had the highest IHM rate and an upward trend, despite being the region with the lowest IBD hospitalizations per 100000 inhabitants. This may reflect difficulty in accessing health resources or underreporting. Another possibility to explain this is related to environmental factors, as the Northeast region is less developed[14].
The Southeast region is the richest, most industrialized and populous region of the country, with more hospital beds and more resources, and it often receives patients from other regions[17]. This region accounted for 44.29% of all IBD hospitalizations. Despite having a low mortality rate for elective hospitalizations, this rate increased and was lower only than the Northeast region rate for nonelective hospitalizations. This may reflect more severe patients coming to the Southeast states, mainly São Paulo and Rio de Janeiro, from all over the country.
There has been a notable reduction in the number of hospitalizations for IBD in Brazil over 20 years. IHM rates varied and did not follow a linear trend. To date, there are a small number of epidemiological studies in Brazil on IBD. Considering that the majority of the population depends on SUS and that DATASUS involves nationwide data, this study is an important contribution to greater knowledge of the impact of IBD in Brazil. Nevertheless, the data analyzed only involved hospitalized patients and did not cover part of the patients cared for by private health insurance. In addition, there was no distinction between CD and UC and no data on the reason for admission, procedures performed or readmissions. Because we used secondary data, much of it collected from hospital admission authorization forms, such information is prone to errors. To carry out a more comprehensive and reliable study, it is necessary to create a national IBD database.
Inflammatory bowel disease (IBD) is associated with complications, frequent hospitalizations, surgery and death. The major causes of hospitalizations are disease activity, diagnostic procedures and surgery. The introduction of biologic drugs into the therapeutic arsenal in the last two decades, combined with an expansion of immunosuppressant therapy, has changed IBD management and may have altered the profile of hospitalizations and in-hospital mortality (IHM) due to IBD.
In Brazil, there is still no integrated database of patients with IBD, limiting the development of comprehensive epidemiological studies. On the other hand, the Brazilian Unified Health System (SUS) has a hospital admission data collection system that allows partial analysis of the impact of IBD in the country.
We aim to describe the profile of hospitalizations and in-hospital deaths due to IBD in Brazil over 10 years and to analyze IHM over 20 years.
This observational, retrospective, ecological study used secondary data on hospitalizations for IBD in Brazil for 2008-2018 to describe hospitalizations and for 1998-2017 to analyze IHM. Hospitalization data were obtained from the Hospital Information System of the Brazilian SUS and population data from demographic censuses. The temporal trend in hospitalizations and IHM was evaluated using simple linear regression.
There was a reduction in the number of IBD hospitalizations, from 6,975 admissions in 1998 to 4113 in 2017 (trend: y = -0.1682x +342.8; R2 = 0.8197; P < 0.0001). The hospitalization rate also decreased, from 3.60/100000 in 2000 to 2.17 in 2010. IHM rates varied during the 20-year period, between 2.06 in 2017 and 3.64 in 2007, and did not follow a linear trend (y = -0.0005049x + 2.617; R2 = 0.00006; P = 0.9741). IHM rates also varied between regions, increasing in all but the southeast, which showed a decreasing trend (y = -0.1122x +4.427; R2 = 0.728; P < 0.0001). The Northeast region had the highest IHM rate (2.86 deaths/100 admissions), with an increasing trend (y = 0.1105x +1.110; R2 = 0.6265; P < 0.0001). A higher IHM rate was observed for nonelective admissions (2.88), which accounted for 81% of IBD hospitalizations. The total cost of IBD hospitalizations in 2017 exhibited an increase of 37.5% compared to 2008.
There has been a notable reduction in the number of hospitalizations for IBD in Brazil over 20 years. Because we used secondary data, such information is prone to errors. To carry out a more comprehensive and reliable study, it is necessary to create a national IBD database.
For the future perspective, the creation of a national IBD database will allow more comprehensive and reliable studies.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gisbert JP S-Editor: Liu M L-Editor: A P-Editor: Liu M
| 1. | Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. 2007;369:1627-1640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1299] [Cited by in RCA: 1509] [Article Influence: 83.8] [Reference Citation Analysis (2)] |
| 2. | Victoria CR, Sassak LY, Nunes HR. Incidence and prevalence rates of inflammatory bowel diseases, in midwestern of São Paulo State, Brazil. Arq Gastroenterol. 2009;46:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | van der Valk ME, Mangen MJ, Leenders M, Dijkstra G, van Bodegraven AA, Fidder HH, de Jong DJ, Pierik M, van der Woude CJ, Romberg-Camps MJ, Clemens CH, Jansen JM, Mahmmod N, van de Meeberg PC, van der Meulen-de Jong AE, Ponsioen CY, Bolwerk CJ, Vermeijden JR, Siersema PD, van Oijen MG, Oldenburg B; COIN study group and the Dutch Initiative on Crohn and Colitis. Healthcare costs of inflammatory bowel disease have shifted from hospitalisation and surgery towards anti-TNFa therapy: results from the COIN study. Gut. 2014;63:72-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 418] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 4. | Nguyen GC, Bollegala N, Chong CA. Factors associated with readmissions and outcomes of patients hospitalized for inflammatory bowel disease. Clin Gastroenterol Hepatol. 2014;12:1897-1904.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Annese V, Duricova D, Gower-Rousseau C, Jess T, Langholz E. Impact of New Treatments on Hospitalisation, Surgery, Infection, and Mortality in IBD: a Focus Paper by the Epidemiology Committee of ECCO. J Crohns Colitis. 2016;10:216-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 6. | Brasil Ministério da Saúde. “Protocolo Clínico e Diretrizes Terapêuticas para tratamento da Retocolite Ulcerativa”. Portaria SAS/MS no 861, de 04 de novembro de 2002. [cited 10 August 2018]. Available from: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_diretrizes_terapeuticas_retocolite_ulcerativa.pdf. |
| 7. | Xu F, Liu Y, Wheaton AG, Rabarison KM, Croft JB. Trends and Factors Associated with Hospitalization Costs for Inflammatory Bowel Disease in the United States. Appl Health Econ Health Policy. 2019;17:77-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 8. | Coward S, Heitman SJ, Clement F, Hubbard J, Proulx MC, Zimmer S, Panaccione R, Seow C, Leung Y, Datta I, Ghosh S, Myers RP, Swain M, Kaplan GG. Ulcerative colitis-associated hospitalization costs: a population-based study. Can J Gastroenterol Hepatol. 2015;29:357-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | de S B Fróes R, Carvalho ATP, de V Carneiro AJ, de Barros Moreira AMH, Moreira JPL, Luiz RR, de Souza HS. The socio-economic impact of work disability due to inflammatory bowel disease in Brazil. Eur J Health Econ. 2018;19:463-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Nguyen GC, Tuskey A, Dassopoulos T, Harris ML, Brant SR. Rising hospitalization rates for inflammatory bowel disease in the United States between 1998 and 2004. Inflamm Bowel Dis. 2007;13:1529-1535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 122] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Kennedy NA, Clark DN, Bauer J, Crowe AM, Knight AD, Nicholls RJ, Satsangi J. Nationwide linkage analysis in Scotland to assess mortality following hospital admission for Crohn's disease: 1998-2000. Aliment Pharmacol Ther. 2012;35:142-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalized for inflammatory bowel disease? Am J Gastroenterol. 2008;103:2789-2798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 99] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Santana GO, Lyra LG, Santana TC, Dos Reis LB, Guedes JC, Toralles MB, Lyra AC. Crohn's disease in one mixed-race population in Brazil. World J Gastroenterol. 2007;13:4489-4492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Parente JM, Coy CS, Campelo V, Parente MP, Costa LA, da Silva RM, Stephan C, Zeitune JM. Inflammatory bowel disease in an underdeveloped region of Northeastern Brazil. World J Gastroenterol. 2015;21:1197-1206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 60] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 15. | Sonnenberg A. Time trends of mortality from Crohn's disease and ulcerative colitis. Int J Epidemiol. 2007;36:890-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Ng SC. Emerging leadership lecture: Inflammatory bowel disease in Asia: emergence of a "Western" disease. J Gastroenterol Hepatol. 2015;30:440-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Instituto Brasileiro de Geografia e Estatística. Contas Regionais do Brasil 2012. Série Contas Nacionais v. 42. Rio de Janeiro: IBGE, 2014. [cited 23 October 2018]. Available from: ftp://ftp.ibge.gov.br/Contas_Regionais/2012/pdf/contas_regionais_2012.pdf. |
| 18. | Escosteguy CC, Portela MC, Medronho Rde A, de Vasconcellos MT. [The Brazilian Hospital Information System and the acute myocardial infarction hospital care]. Rev Saude Publica. 2002;36:491-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Melo EC, Travassos C, Carvalho MS. [Quality of data on myocardial infarction deaths, Brazil]. Rev Saude Publica. 2004;38:385-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Murthy SK, Steinhart AH, Tinmouth J, Austin PC, Nguyen GC. Impact of gastroenterologist care on health outcomes of hospitalised ulcerative colitis patients. Gut. 2012;61:1410-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |