Published online May 22, 2022. doi: 10.4291/wjgp.v13.i3.85
Peer-review started: December 10, 2021
First decision: February 15, 2022
Revised: February 20, 2022
Accepted: March 27, 2022
Article in press: March 27, 2022
Published online: May 22, 2022
Processing time: 158 Days and 16.8 Hours
The prevalence of Crohn’s disease (CD) and ulcerative colitis (UC) is on the rise worldwide. This rising prevalence is concerning as patients with CD and UC may frequently relapse leading to recurrent hospitalizations and increased healthcare utilization.
To identify trends and adverse outcomes for 30 d readmissions for CD and UC.
This was a retrospective, interrupted trends study involving all adult (≥ 18 years) 30 d readmissions of CD and UC from the National Readmission Database (NRD) between 2008 and 2018. Patients < 18 years, elective, and traumatic hospitalizations were excluded from this study. We identified hospitalization characteristics and readmission rates for each calendar year. Trends of inpatient mortality, mean length of hospital stay (LOS) and mean total hospital cost (THC) were calculated using a multivariate logistic trend analysis adjusting for age, gender, insurance status, comorbidity burden and hospital factors. Furthermore, trends between CD and UC readmissions were compared using regression of the interaction coefficient after adjusting for age and gender to determine relative trends between the two populations. Stata® Version 16 software (StataCorp, TX, United States) was used for statistical analysis and P value ≤ 0.05 were considered statistically significant.
Total number of 30 d readmissions increased from 6202 in 2010 to 7672 in 2018 for CD and from 3272 in 2010 to 4234 in 2018 for UC. We noted increasing trends for 30-day all-cause readmission rate of CD from 14.9% in 2010 to 17.6% in 2018 (P-trend < 0.001), CD specific readmission rate from 7.1% in 2010 to 8.2% in 2018 (P-trend < 0.001), 30-day all-cause readmission rate of UC from 14.1% in 2010 to 15.7% in 2018 (P-trend = 0.003), and UC specific readmission rate from 5.2% in 2010 to 5.6% in 2018 (P-trend = 0.029). There was no change in the risk adjusted trends of inpatient mortality and mean LOS for CD and UC readmissions. However, we found an increasing trend of mean THC for UC readmissions. After comparison, there was no statistical difference in the trends for 30 d all-cause readmission rate, inpatient mortality, and mean LOS between CD and UC readmissions.
There was an increase in total number of 30 d readmissions for CD and UC with a trend towards increasing 30 d all-cause readmission rates.
Core Tip: This retrospective interrupted trend study analyzed 30 d readmissions of Crohn’s disease (CD) and ulcerative colitis (UC) in the United States from 2010–2018. There was a rising trend for 30 d all-cause readmission rate of CD and UC, and CD- and UC-specific readmission rate throughout the study period. However, we noted no change in the risk adjusted trends of inpatient mortality and mean length of hospital stay (LOS) for 30 d readmissions of CD and UC. Furthermore, there was no statistical difference in the trends for 30 d all-cause readmission rate, inpatient mortality, and mean LOS between CD and UC readmissions.
- Citation: Dahiya DS, Perisetti A, Kichloo A, Singh A, Goyal H, Rotundo L, Vennikandam M, Shaka H, Singh G, Singh J, Pisipati S, Al-Haddad M, Sanaka MR, Inamdar S. Increasing thirty-day readmissions of Crohn’s disease and ulcerative colitis in the United States: A national dilemma. World J Gastrointest Pathophysiol 2022; 13(3): 85-95
- URL: https://www.wjgnet.com/2150-5330/full/v13/i3/85.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v13.i3.85
Inflammatory bowel disease (IBD) is characterized by chronic inflammation of the gastrointestinal tract with a propensity of remission and relapse over time[1]. It consists of Crohn’s disease (CD) and ulcerative colitis (UC)[2]. The exact pathogenesis of IBD is relatively unknown, but researchers believe that factors such as immune response dysregulation, gut microbiota dysbiosis, environmental changes and genetic variants play a key role[3]. In 2017, there were 6.8 million patients with IBD worldwide with studies reporting continuously rising incidence and prevalence, particularly in North America[4]. The rising rates of IBD are concerning as it is associated with a poor quality of life and places significant social and economic burden on individuals and the United States healthcare system[5,6].
Despite outpatient management by gastroenterologists, patients with IBD are at increased risk of readmission due to relapse, complications of the disease or for additional interventions after index hospitalization. This further exacerbates the impact of the disease on individuals and the healthcare system. Additionally, studies have demonstrated that about 9%–50% of IBD readmissions are preventable and may be directly linked to the quality of hospital care and inadequate post-discharge care[7]. Hence, hospital systems have developed scoring systems to identify individuals at the highest risk of readmission and implemented strategies to reduce readmissions and improve the overall quality of care[8].
In current literature, a majority of the studies investigating readmissions of IBD have been single-center experiences or primarily focused on surgical patients[9,10]. There continues to be relative paucity of data on early (30 d) readmissions of CD and UC in the United States. Hence, this national, retrospective, interrupted trends study was designed to identify the hospitalization characteristics and estimate readmission rates of CD and UC in the United States between 2010–2018. We also identified the trends of inpatient mortality to determine improvements in therapeutic management of the disease. Furthermore, we calculated the burden of the disease on the United States healthcare system in terms of healthcare utilization and hospitalization costs.
This was a retrospective interrupted trends study involving all adult readmissions of IBD (UC and CD) in the United States between 2010–2018. Data for analysis was extracted from the Nationwide Readmissions Database (NRD) which is a part of the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases (SID)[11]. It allows for weighted analysis to obtain 100% of the United States hospitalizations within a given calendar year[11]. The data for NRD is collected using the International Classification of Diseases, Ninth/Tenth Revision, Clinical Modification (ICD-9/10-CM/PCS) codes.
The study involved all adult (≥ 18 years) 30 d readmissions of CD and UC from the NRD for the years 2010, 2012, 2014, 2016 and 2018. We used all available ICD-9-CM/PCS codes for CD (555X) and UC (556X) along with the equivalent ICD-10-CM/PCS codes K50X and K51X for CD and UC, respectively. The precedence for the utilization of these codes has been established in prior published studies[12]. Individuals < 18 years of age, elective and traumatic hospitalizations were excluded from the analysis. Using unique hospitalization identifiers, index hospitalizations of CD and UC were identified and one subsequent hospitalization within 30 d was tagged as a readmission.
The data was analyzed using Stata® Version 16 software (StataCorp, TX, United States). All analyses were conducted using weighted samples for national estimates. P value ≤ 0.05 was set as the threshold for statistical significance. We highlighted hospitalization trends and obtained the 30 d all-cause readmission rate, disease specific readmission rate and readmission proportion for specific calendar years. The comorbidity burden was assessed using Sundararajan’s adaptation of the modified Deyo’s Charlson comorbidity index[13]. Trends of inpatient mortality, mean length of stay (LOS) and mean hospital cost (THC) for CD and UC readmissions were calculated using a multivariate logistic trend analysis adjusting for age, gender, insurance status, comorbidity burden and hospital factors. The total hospital cost was obtained using the HCUP Cost-to-Charge Ratio files and adjusted for inflation using the Medical Expenditure Panel Survey index for hospital care, with 2018 as the reference point[14,15]. Additionally, trends between CD and UC readmissions were compared using regression of the interaction coefficient after adjusting for age and gender to determine relative trends between the two populations. Furthermore, we report no missing data in this study.
The NRD database lacks patient and hospital-specific identifiers. Hence, this study was exempt from Institutional Review Board (IRB) approval for analysis as per guidelines put forth by our institutional IRB for research on database studies.
The NRD is a large publicly available, multi-ethic, all-payer inpatient care database in the United States, containing data on more than 18 million hospital stays/year. The database can be accessed at: https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
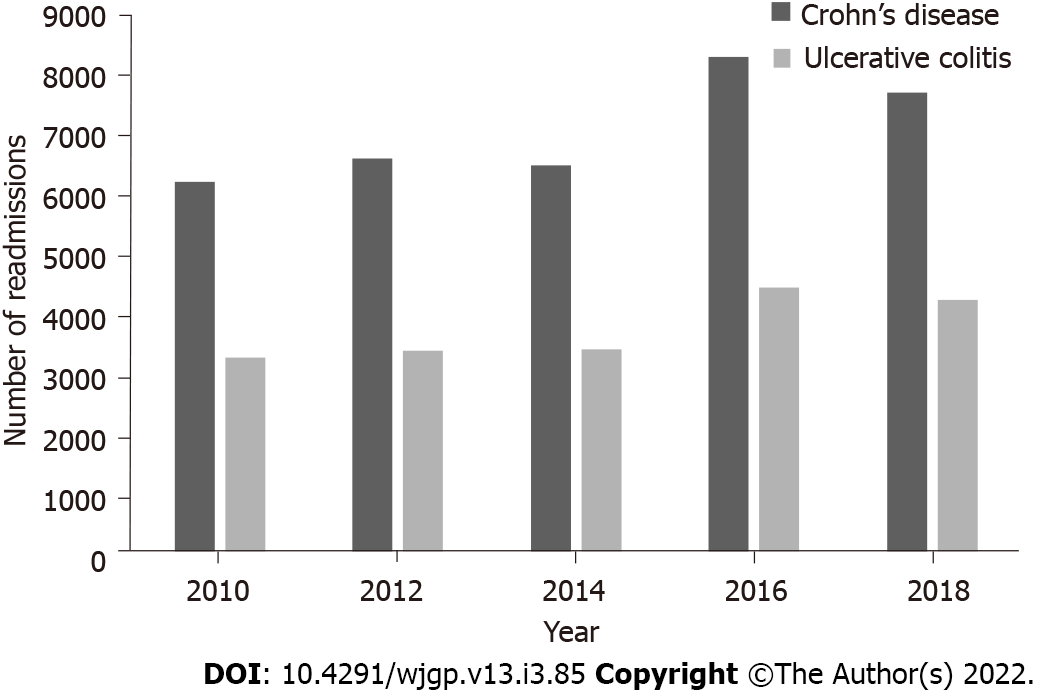
The total number of 30 d readmissions of CD increased from 6202 in 2010 to 7672 in 2018 (Figure 1). The mean age increased from 41.8 ± 0.9 in 2010 to 43.9 ± 0.7 years in 2018. A female predominance was noted throughout the study period (Table 1); however, a statistically significant trend for gender was absent. Additionally, 30 d readmissions of CD were noted to have an increasing comorbidity burden with time (Table 1). Furthermore, metropolitan teaching hospitals had the majority of the readmissions with a statistically significant trend towards increasing readmissions from 52.1% in 2010 to 77% in 2018 (Table 1).
| Variable | Year | ||||
| 2010 | 2012 | 2014 | 2016 | 2018 | |
| Number of readmissions | 6202 | 6580 | 6475 | 8278 | 7672 |
| Age (mean ± SE, yr) | 41.8 ± 0.9 | 41.6 ± 1.1 | 41.2 ± 0.8 | 42.5 ± 0.7 | 43.9 ± 0.7 |
| Gender (%) | |||||
| Males | 45.5 | 44.0 | 45.7 | 46.7 | 46.5 |
| Females | 54.5 | 56.0 | 54.3 | 53.3 | 53.5 |
| Charlson comorbidity index score (%) | |||||
| 0 | 69.7 | 72.0 | 69.9 | 64.9 | 61.3 |
| 1 | 19.2 | 15.5 | 17.3 | 19.5 | 20.0 |
| 2 | 5.9 | 6.1 | 6.7 | 7.5 | 9.0 |
| ≥ 3 | 5.2 | 6.4 | 6.1 | 8.1 | 9.7 |
| Insurance type (%) | |||||
| Medicare | 20.5 | 29.1 | 29.3 | 28.9 | 30.6 |
| Medicaid | 21.5 | 24.9 | 26.4 | 25.5 | 24.7 |
| Private | 41.2 | 37.1 | 37.0 | 40.8 | 39.0 |
| Uninsured | 8.8 | 8.9 | 7.3 | 4.8 | 5.7 |
| Household income quartile (%) | |||||
| 1st | 27.8 | 29.2 | 27.9 | 29.0 | 28.6 |
| 2nd | 23.4 | 25.6 | 28.5 | 26.8 | 30.0 |
| 3rd | 24.9 | 25.1 | 22.5 | 24.5 | 23.7 |
| 4th | 23.9 | 20.1 | 21.1 | 19.7 | 17.7 |
| Hospital characteristics | |||||
| Hospital bed size (%) | |||||
| Small | 9.9 | 9.9 | 14.2 | 13.3 | 15.0 |
| Medium | 22.4 | 22.4 | 27.3 | 26.9 | 26.3 |
| Large | 67.7 | 67.7 | 58.5 | 59.8 | 58.7 |
| Teaching status (%) | |||||
| Metropolitan non-teaching | 39.2 | 34.4 | 25.2 | 21.8 | 17.3 |
| Metropolitan teaching | 52.1 | 56.8 | 68.4 | 72.3 | 77.0 |
| Non-metropolitan | 8.7 | 8.8 | 6.4 | 5.9 | 5.7 |
| Hospital volume quintiles (%) | |||||
| Q1 | 1.8 | 1.9 | 1.5 | 1.7 | 1.3 |
| Q2 | 4.3 | 5.4 | 5.1 | 4.2 | 4.5 |
| Q3 | 10.3 | 10.0 | 10.2 | 8.4 | 10.4 |
| Q4 | 19.4 | 18.1 | 18.1 | 18.6 | 19.1 |
| Q5 | 64.2 | 64.6 | 65.1 | 67.1 | 64.7 |
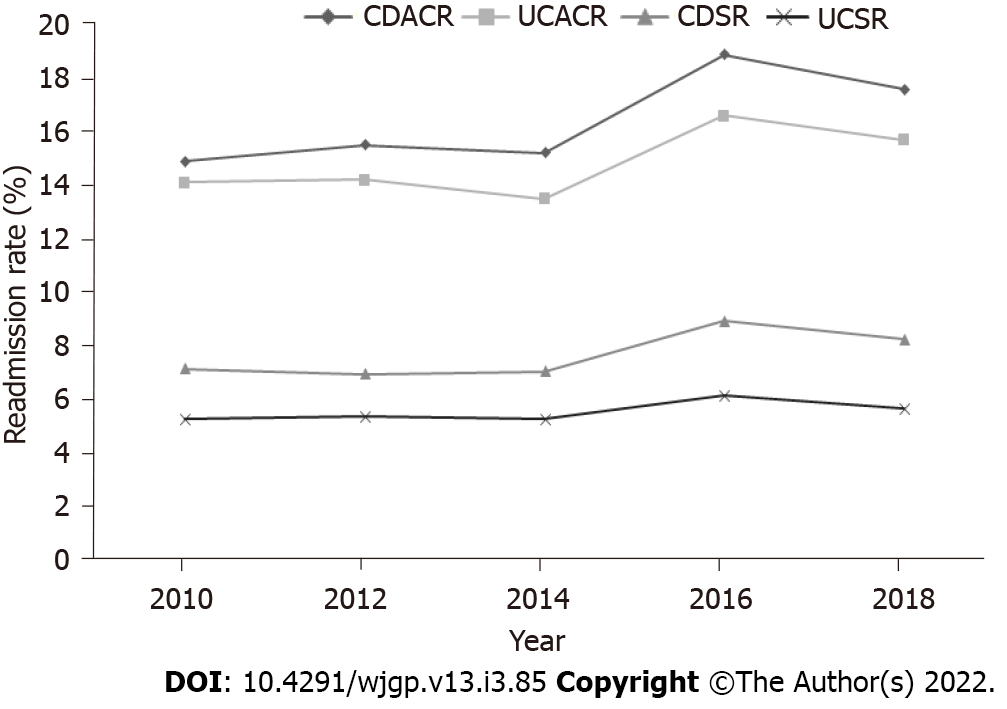
There was a statistically significant trend towards increasing 30 d all-cause readmission rate of CD from 14.9% in 2010 to 17.6% in 2018 (P-trend < 0.001) (Figure 2). The CD specific readmission rate also had a statistically significant increasing trend with an increase from 7.1% in 2010 to 8.2% in 2018 (P-trend < 0.001). However, we did not observe a significant change in the risk adjusted trends of inpatient mortality, mean LOS, and mean THC for these readmissions.
Similar to CD, the total number of 30 d readmissions of UC increased from 3272 in 2010 to 4234 in 2018 (Figure 1). The mean age for these readmissions increased from 49.8 ± 1.6 in 2010 to 51.2 ± 0.8 years in 2018. A female predominance without a statistical trend for gender and increasing comorbidity burden with time was also noted. Furthermore, metropolitan teaching hospitals had an increasing trend of readmissions from 53.6% in 2010 to 76.3% in 2018 (Table 2), similar to that for CD.
| Variable | Year | ||||
| 2010 | 2012 | 2014 | 2016 | 2018 | |
| Number of readmissions | 3272 | 3399 | 3426 | 4449 | 4234 |
| Age (mean ± SE, yr) | 49.8 ± 1.6 | 49.6 ± 1.5 | 48.4 ± 1.1 | 49.9 ± 1.0 | 51.2 ± 0.8 |
| Gender (%) | |||||
| Males | 48.1 | 45.6 | 47.5 | 46.7 | 49.4 |
| Females | 51.9 | 54.4 | 52.5 | 53.3 | 50.6 |
| Charlson comorbidity index score (%) | |||||
| 0 | 57.8 | 59.6 | 60.6 | 55.6 | 50.9 |
| 1 | 20.3 | 20.0 | 18.6 | 19.4 | 20.7 |
| 2 | 9.4 | 9.0 | 8.5 | 10.6 | 10.3 |
| ≥ 3 | 12.5 | 11.4 | 12.3 | 14.4 | 18.1 |
| Insurance type (%) | |||||
| Medicare | 36.3 | 36.6 | 32.4 | 35.1 | 34.8 |
| Medicaid | 17.8 | 17.0 | 22.3 | 17.5 | 19.5 |
| Private | 39.4 | 37.0 | 40.1 | 42.2 | 40.4 |
| Uninsured | 6.5 | 9.4 | 5.2 | 5.2 | 5.3 |
| Household income quartile (%) | |||||
| 1st | 25.5 | 29.2 | 26.5 | 27.2 | 25.0 |
| 2nd | 22.5 | 23.1 | 25.9 | 27.5 | 26.7 |
| 3rd | 26.4 | 24.6 | 22.9 | 25.0 | 26.1 |
| 4th | 25.6 | 23.1 | 24.7 | 20.3 | 22.2 |
| Hospital characteristics | |||||
| Hospital bed size (%) | |||||
| Small | 10.2 | 9.8 | 13.2 | 13.5 | 16.8 |
| Medium | 19.8 | 22.4 | 26.8 | 25.7 | 24.3 |
| Large | 70.0 | 67.8 | 60.0 | 60.8 | 58.9 |
| Teaching status (%) | |||||
| Metropolitan non-teaching | 37.3 | 38.2 | 26.1 | 24.5 | 19.3 |
| Metropolitan teaching | 53.6 | 53.5 | 67.7 | 70.3 | 76.3 |
| Non-metropolitan | 9.1 | 8.3 | 6.2 | 5.2 | 4.4 |
| Hospital volume quintiles (%) | |||||
| Q1 | 2.4 | 2.4 | 2.5 | 2.1 | 2.0 |
| Q2 | 6.0 | 7.4 | 5.9 | 5.8 | 5.5 |
| Q3 | 11.8 | 10.5 | 11.7 | 10.3 | 12.3 |
| Q4 | 20.2 | 20.1 | 19.0 | 20.4 | 21.4 |
| Q5 | 59.6 | 59.6 | 60.9 | 61.4 | 58.8 |
A rising trend was noted for 30 d all cause readmission rate of UC from 14.1% in 2010 to 15.7% in 2018 (P-trend = 0.003) (Figure 2) and for UC specific readmission rate from 5.2% in 2010 to 5.6% in 2018 (P-trend = 0.029). Additionally, the mean THC increased from $13783 in 2010 to $15929 in 2018 (P-trend = 0.009) with a rising trend unlike CD. However, similar to CD, a significant change in the risk adjusted trends was absent for of inpatient mortality and mean LOS (Table 3).
| Outcomes | Year | P trend | ||||
| 2010 | 2012 | 2014 | 2016 | 2018 | ||
| Crohn’s disease | ||||||
| All-cause readmission rate (%) | 14.9 | 15.5 | 15.2 | 18.9 | 17.6 | < 0.001 |
| Crohn’s disease specific readmission rate (%) | 7.1 | 6.9 | 7.0 | 8.9 | 8.2 | < 0.001 |
| Crohn’s disease readmission proportion (%) | 54.9 | 51.8 | 53.0 | 55.8 | 54.6 | 0.002 |
| Inpatient mortality (%) | 0.9 | 1.4 | 0.7 | 0.7 | 1.0 | 0.059 |
| Mean length of stay (d) | 5.9 | 5.9 | 5.3 | 6.0 | 6.2 | 0.927 |
| Mean total hospital cost (USD) | 12327 | 13068 | 10988 | 13421 | 14260 | 0.210 |
| Ulcerative colitis | ||||||
| All-cause readmission rate (%) | 14.1 | 14.2 | 13.5 | 16.6 | 15.7 | 0.003 |
| Ulcerative colitis specific readmission rate (%) | 5.2 | 5.3 | 5.2 | 6.1 | 5.6 | 0.029 |
| Ulcerative colitis readmission proportion (%) | 42.6 | 42.4 | 43.4 | 43.0 | 41.0 | 0.566 |
| Inpatient mortality (%) | 2.5 | 1.8 | 2.2 | 2.0 | 2.3 | 0.912 |
| Mean length of stay (d) | 6.8 | 6.8 | 6.3 | 6.8 | 6.9 | 0.452 |
| Mean total hospital cost (USD) | 13783 | 13568 | 13790 | 15358 | 15929 | 0.009 |
Although CD had higher number of 30 d readmissions every year, we did not observe a statistically significant difference in the in the trends for 30 d all-cause readmission rate (interaction P-trend = 0.087), inpatient mortality (interaction P-trend = 0.231), and mean LOS (interaction P-trend = 0.388). However, there was a statistically significant trend towards increasing mean THC for 30 d readmissions of UC relative to 30 d readmissions of CD (interaction P-trend < 0.001).
It is essential to identify early (30 d) readmissions of IBD as they may be associated with quality of inpatient care, increased risk of adverse outcomes and place significant burden on the United States healthcare system in terms of healthcare costs and resource utilization. Additionally, as providers become aware of the magnitude of these readmissions and the patient demographics most effected, efforts could be directed at index admissions to further optimize medical therapy before discharge, promote patient education and encourage a greater degree of involvement in their care, and increase outpatient follow-up, thereby decreasing early readmissions. A single center retrospective study from 2007–2010 revealed that about 5% patients with IBD were readmitted within 1 wk of hospital discharge, 14% within 1 mo, 23% within 3 mo and about 39% within the year[16]. Another study in the United States reported similar findings with a readmission rate of 18% within 1 mo of hospital discharge[17]. In 2013, an NRD-based study estimated 3037 (7%) readmissions of IBD at 30 d[7].
In our study, the total number of 30 d readmissions of CD increased from 6202 in 2010 to 7672 in 2018 and for UC from 3,272 in 2010 to 4,234 in 2018, both with a female predominance (Tables 1 and 2). This coincides with rising prevalence of CD and UC in the general population[18]. We also noted an increasing trend for 30 d all-cause readmission rates and disease specific readmission rates for 30 d readmissions of CD and UC (Table 3). These findings may, in part, be due to a rising prevalence of IBD in the general population which increased significantly from 0.9% (2 million adults) in 1999 to 1.3% (3 million adults) in 2015, an increase in the flare-ups of IBD which may account for about 50% of the readmissions or due to non-IBD related causes such as infections secondary to the widespread use of biological agents or immunosuppressants[16,18,19]. We performed a trend comparison between 30 d all-cause readmission rate of CD and UC. It was not statistically significant and signified that all-cause readmissions for both CD and UC were increasing proportionately in the United States.
The mean age for 30 d readmissions increased for both CD and UC without a statistically significant trend. The difference in the mean age between the two groups is approximately 7 years. These finding align with current literature which reports that patients with CD tend to be younger and the mean age at the time of diagnosis of CD is usually 5–10 years earlier than that of UC[20]. From a gender standpoint, there is a lower risk of CD until puberty for females when compared to males, after which there is a reversal of this risk[21]. For UC, males and females have a similar incidence until the age of 45 after which males exhibit higher risk of incident UC than females[21]. However, for readmissions of CD and UC, a slight female predominance has been noted in literature[22]. Similarly in our study, a slight female predominance was noted for CD and UC readmissions. Furthermore, we did not find a statistically significant readmission trend for gender over time which implied that the readmission rates for both genders have remained relatively stable. Moreover, we noted an increase in the overall comorbidity burden for 30 d readmissions of CD and UC. This was expected as readmissions for individuals with multiple concurrent co-morbidities have been increasing.
From a hospital perspective, large bed-sized hospitals had the highest proportions of 30 d readmissions of CD and UC. This may be due to the fact that larger hospitals have a higher capacity of in-patient admissions. Additionally, metropolitan teaching hospitals consistently had the highest readmission rates with an increasing trend. This may be because these hospitals are usually tertiary care referral center accepting complex patients from large geographical areas and hence, are well equipped with the necessary resources and specialists to manage these readmissions and their complications. Moreover, an urban location, consisting of a greater population density which may be attributed to a demographic shift of non-urban/rural population to urban locations between 2010 and 2018, is more likely to yield higher readmissions[23].
Furthermore, IBD readmissions have been associated with significant inpatient mortality and healthcare burden. As per literature, frailty and length of intensive care unit stay is independently associated with higher rates of inpatient mortality for IBD readmissions[16,24]. From 2010–2014, a study reported that the inpatient mortality for 30 d readmissions of CD was 2.85% per year, the LOS was 6 d, and cost of hospitalization was $11402[25]. In 2017, for 30 d readmissions of UC, literature reported an inpatient mortality of 1.99% along with longer LOS and higher hospitalization costs compared to index admission[26]. In our study, despite an increasing co-morbidity burden (CCI) for the study period, inpatient mortality, and mean LOS for 30 d readmissions of CD and UC did not have a significant change in the risk adjusted trend (Table 3) over time. These stable mortality and LOS trends may reflect optimal guideline driven therapeutic management for the study period. However, the mean THC for 30 d readmission of UC increased from $13783 in 2010 to $15929 (P-trend = 0.009) with an increasing trend, while no trend in THC was identified for CD readmissions. Furthermore, a trend comparison of mean THC between CD and UC yielded a statistically significant trend towards increasing mean THC for 30 d readmissions of UC relative to 30 d readmissions of CD. The exact reason for these THC findings is unclear but may be attributed to an increased complexity and complications of UC readmission requiring immediate higher level of care, additional endoscopic interventions, and a multi-disciplinary team approach for management.
Directing our focus to individual calendar years, we noted a decrease in the total number of readmissions for both CD and UC from 2016 to 2018 (Tables 1 and 2). Similarly, the 30 d all-cause readmissions rate and disease specific readmission rate also decreased from 2016 to 2018 (Table 3). These findings may be due to an overall decrease in the readmissions for one particular calendar year and do not reflect an overall trend. In fact, as discussed earlier, when trended from 2010 to 2018, we noted an increasing trend for all-cause readmissions rate and disease specific readmission rate, and with respect to 2010, there was an overall increase in the total number of 30 d readmissions of CD and UC. Hence, future larger studies are needed to assess rate of readmissions from 2018 to evaluate the trends further.
The key strengths of this study include the study population, unique study design, and methodology which allowed for a comprehensive analysis. As the data was collected from one of the largest databases containing information on readmissions from hospitals across the United States, the results are applicable to hospitals throughout the United States. Additionally, we studied a 9-year time frame which helped us establish meaningful trends. However, important limitations exist with this study. The NRD does not contain data on the severity of the disease and therefore, we were unable to further stratify the readmissions based on the severity of CD or UC. The NRD also lacks data on the total duration of the illness and the exact duration after discharge to readmissions, limiting our ability to assess index admissions more prone to earlier readmissions. Furthermore, it does not contain information on the pharmacological treatment, hospital course and management of IBD readmissions. Hence, we could not comment on the treatment aspects of these readmissions. Moreover, this study is amenable to all biases associated with retrospective studies. Finally, the NRD is an administrative database and therefore, susceptible to coding errors. Despite these limitations, this study helps us better understand the hospitalizations characteristics and trends of 30 d readmissions for CD and UC which is critical for management of these patients.
In conclusion, the total number of 30 d readmission for CD and UC increased. UC readmissions were older than CD readmissions. We noted an increasing trend for 30 d all-cause readmission rate for CD and UC. However, there was no statistical change in the risk adjusted trends of inpatient mortality and mean LOS for these readmissions. The mean total healthcare cost for 30 d readmissions of UC had a rising trend while no trend was observed for CD readmissions. Future prospective studies are needed to further study these findings.
The prevalence of inflammatory bowel disease (IBD) continues to be on the rise around the globe. Despite outpatient management, these patients are at increased risk of relapse leading to hospitalizations and subsequent readmissions.
Through this study, we attempted to outline the magnitude, characteristics and outcomes of early (30 d) readmissions of IBD in the United States.
This national, retrospective, interrupted trends study aimed to identify hospitalization characteristics, readmission rates, adverse outcomes, and healthcare burden for 30 d readmissions of Crohn's disease (CD) and ulcerative colitis (UC) in the United States between 2010-2018.
This was a retrospective, interrupted trends which analyzed data from the National Readmission Database (NRD) on all adult 30 d readmissions of CD and UC in the United States between 2010-2018. Patients < 18 years of age, elective and traumatic hospitalizations were excluded from the analysis. Hospitalization characteristics, readmission rates, adverse outcomes and the healthcare burden was identified. P-values ≤ 0.05 were considered statistically significant.
Total number of 30 d readmissions increased from 6202 in 2010 to 7672 in 2018 for CD and from 3272 in 2010 to 4234 in 2018 for UC. There was an increase in the 30 d all-cause readmission rate of CD and UC for the study period. We did not observe a change in the risk adjusted trends of inpatient mortality and mean length of hospital stay (LOS) for CD and UC readmissions. However, there was a rising trend of mean THC for UC readmissions. After comparison, there was no statistical difference in the trends for 30 d all-cause readmission rate, inpatient mortality, and mean LOS between CD and UC readmissions.
From 2010 to 2018, there was an increase in the total number of 30 d readmissions with a trend towards increasing 30 d all-cause readmission rates for CD and UC. However, there was no change in the risk adjusted trends of inpatient mortality.
This study helps clinicians better understand the magnitude and characteristics of 30 d readmissions of CD and UC in the United States. Through this study, we also aim to encourage and promote future research on readmissions of IBD.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Gastroenterology, No. 59498; American Gastroenterological Association, No. 1550524.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Khayat AA, Saudi Arabia; Sato Y, Japan S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Ponder A, Long MD. A clinical review of recent findings in the epidemiology of inflammatory bowel disease. Clin Epidemiol. 2013;5:237-247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 118] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 2. | Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, Hayee B, Lomer MCE, Parkes GC, Selinger C, Barrett KJ, Davies RJ, Bennett C, Gittens S, Dunlop MG, Faiz O, Fraser A, Garrick V, Johnston PD, Parkes M, Sanderson J, Terry H; IBD guidelines eDelphi consensus group, Gaya DR, Iqbal TH, Taylor SA, Smith M, Brookes M, Hansen R, Hawthorne AB. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68:s1-s106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1402] [Cited by in RCA: 1532] [Article Influence: 255.3] [Reference Citation Analysis (0)] |
| 3. | Lee SH, Kwon JE, Cho ML. Immunological pathogenesis of inflammatory bowel disease. Intest Res. 2018;16:26-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 362] [Cited by in RCA: 388] [Article Influence: 55.4] [Reference Citation Analysis (0)] |
| 4. | GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:17-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1466] [Cited by in RCA: 1428] [Article Influence: 285.6] [Reference Citation Analysis (0)] |
| 5. | Knowles SR, Graff LA, Wilding H, Hewitt C, Keefer L, Mikocka-Walus A. Quality of Life in Inflammatory Bowel Disease: A Systematic Review and Meta-analyses-Part I. Inflamm Bowel Dis. 2018;24:742-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 330] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 6. | Park KT, Ehrlich OG, Allen JI, Meadows P, Szigethy EM, Henrichsen K, Kim SC, Lawton RC, Murphy SM, Regueiro M, Rubin DT, Engel-Nitz NM, Heller CA. The Cost of Inflammatory Bowel Disease: An Initiative From the Crohn's & Colitis Foundation. Inflamm Bowel Dis. 2020;26:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 260] [Cited by in RCA: 303] [Article Influence: 60.6] [Reference Citation Analysis (0)] |
| 7. | Micic D, Gaetano JN, Rubin JN, Cohen RD, Sakuraba A, Rubin DT, Pekow J. Factors associated with readmission to the hospital within 30 days in patients with inflammatory bowel disease. PLoS One. 2017;12:e0182900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | George LA, Martin B, Gupta N, Nikhil S, Mukund V, Naik AS. Predicting 30-Day Readmission Rate in Inflammatory Bowel Disease Patients: Performance of LACE Index. Crohns Colitis 360. 2019;1:otz007. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Kulaylat AN, Hollenbeak CS, Sangster W, Stewart DB Sr. Impact of smoking on the surgical outcome of Crohn's disease: a propensity-score matched National Surgical Quality Improvement Program analysis. Colorectal Dis. 2015;17:891-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Damle RN, Alavi K. Risk factors for 30-d readmission after colorectal surgery: a systematic review. J Surg Res. 2016;200:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | Overview of the Nationwide Readmissions Database (NRD). Overview of the Nationwide Readmissions Database (NRD), Rockville, MD: Healthcare Cost and Utilization Project; 2018. Available from: https://www.hcup-us.ahrq.gov/nrdoverview.jsp. |
| 12. | Barnes EL, Kochar B, Long MD, Kappelman MD, Martin CF, Korzenik JR, Crockett SD. Modifiable Risk Factors for Hospital Readmission Among Patients with Inflammatory Bowel Disease in a Nationwide Database. Inflamm Bowel Dis. 2017;23:875-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 74] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 13. | Sundararajan V, Quan H, Halfon P, Fushimi K, Luthi JC, Burnand B, Ghali WA; International Methodology Consortium for Coded Health Information (IMECCHI). Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med Care. 2007;45:1210-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 207] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 14. | Cost-to-Charge Ratio Files. Cost-to-Charge Ratio Files, Rockville, MD: Healthcare Cost and Utilization Project; 2020. Available from: https://www.hcup-us.ahrq.gov/db/ccr/costtocharge.jsp. |
| 15. | Dunn A, Grosse SD, Zuvekas SH. Adjusting Health Expenditures for Inflation: A Review of Measures for Health Services Research in the United States. Health Serv Res. 2018;53:175-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 365] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 16. | Mudireddy P, Scott F, Feathers A, Lichtenstein GR. Inflammatory Bowel Disease: Predictors and Causes of Early and Late Hospital Readmissions. Inflamm Bowel Dis. 2017;23:1832-1839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Hazratjee N, Agito M, Lopez R, Lashner B, Rizk MK. Hospital readmissions in patients with inflammatory bowel disease. Am J Gastroenterol. 2013;108:1024-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB. Prevalence of Inflammatory Bowel Disease Among Adults Aged ≥18 Years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:1166-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 470] [Article Influence: 52.2] [Reference Citation Analysis (0)] |
| 19. | Malhotra A, Mandip KC, Shaukat A, Rector T. All-cause hospitalizations for inflammatory bowel diseases: Can the reason for admission provide information on inpatient resource use? Mil Med Res. 2016;3:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Duricova D, Burisch J, Jess T, Gower-Rousseau C, Lakatos PL; ECCO-EpiCom. Age-related differences in presentation and course of inflammatory bowel disease: an update on the population-based literature. J Crohns Colitis. 2014;8:1351-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 130] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 21. | Rustgi SD, Kayal M, Shah SC. Sex-based differences in inflammatory bowel diseases: a review. Therap Adv Gastroenterol. 2020;13:1756284820915043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 22. | Cohen-Mekelburg S, Rosenblatt R, Wallace B, Shen N, Fortune B, Waljee AK, Saini S, Scherl E, Burakoff R, Unruh M. Inflammatory bowel disease readmissions are associated with utilization and comorbidity. Am J Manag Care. 2019;25:474-481. [PubMed] |
| 23. | United States Census Bureau. 2020 Census Statistics Highlight Local Population Changes and Nation’s Racial and Ethnic Diversity; 2020. Available from: https://www.census.gov/newsroom/press-releases/2021/population-changes-nations-diversity.html. |
| 24. | Qian AS, Nguyen NH, Elia J, Ohno-Machado L, Sandborn WJ, Singh S. Frailty Is Independently Associated with Mortality and Readmission in Hospitalized Patients with Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2021;19:2054-2063.e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 25. | Kruger AJ, Hinton A, Afzali A. To the Editors: Index Severity Score and Early Readmission Predicts Increased Mortality in Crohn's Disease Patients. Inflamm Bowel Dis. 2019;25:e74-e76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Weissman S, Sharma S, Fung BM, Aziz M, Feuerstein JD. Increased Mortality and Healthcare Costs upon Hospital Readmissions of Ulcerative Colitis Flares: A Large Population-based Cohort Study. Crohns Colitis 360. 2021;3:otab029. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |