Published online May 12, 2020. doi: 10.4291/wjgp.v11.i3.57
Peer-review started: October 15, 2019
First decision: December 4, 2019
Revised: February 3, 2020
Accepted: March 1, 2020
Article in press: March 1, 2020
Published online: May 12, 2020
Processing time: 209 Days and 11.1 Hours
Atherosclerosis (ATH) and non-alcoholic fatty liver disease (NAFLD) are medical conditions that straddle a communal epidemiology, underlying mechanism and a clinical syndrome that has protean manifestations, touching every organ in the body. These twin partners, ATH and NAFLD, are seemingly straightforward and relatively simple topics when considered alone, but their interdependence calls for more thought. The study of the mutual relationship of NAFLD and ATH should involve big data analytics approaches, given that they encompass a constellation of diseases and are related to several recognized risk factors and health determinants and calls to an explicit theory of change, to justify intervention. Research studies on the “association between aortic stiffness and liver steatosis in morbidly obese patients”, published recently, sparsely hypothesize new mechanisms of disease, claiming the “long shadow of NAFLD” as a risk factor, if not as a causative factor of arterial stiffness and ATH. This statement is probably overreaching the argument and harmful for the scientific credence of this area of medicine. Despite the verification that NAFLD and cardiovascular disease are strongly interrelated, current evidence is that NAFLD may be a useful indicator for flagging early arteriosclerosis, and not a likely causative factor. Greater sustainable contribution by precision medicine tools, by validated bioinformatics approaches, is needed for substantiating conjectures, assumptions and inferences related to the management of big data and addressed to intervention for behavioral changes within an explicit theory of change.
Core tip: Atherosclerosis and non-alcoholic fatty liver disease straddle a communal epidemiology, underlying mechanism and a clinical syndrome with protean manifestations, touching every organ in the body. Current therapeutic evidence supports the recommendation of addressing changes toward healthier lifestyles, including diet and physical exercise, in atherosclerosis and non-alcoholic fatty liver disease, even when defined only by non-invasive methodology. Pathway-based analysis are elucidating key molecular mechanisms underlying complex diseases addressing the joint effect and integrality as function unit of multiple genes, exploring large-scale “-omics” data. No element suggests, apart from naïve statistics, that one condition affects the other directly by any mechanism.
- Citation: Trovato GM. Non-alcoholic fatty liver disease and Atherosclerosis at a crossroad: The overlap of a theory of change and bioinformatics. World J Gastrointest Pathophysiol 2020; 11(3): 57-63
- URL: https://www.wjgnet.com/2150-5330/full/v11/i3/57.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v11.i3.57
According to World Health Organization, ICD-11 for Mortality and Morbidity Statistics (Version: 04/2019), non-alcoholic fatty liver disease (NAFLD) is characterized by fatty liver related to insulin resistance in the absence of significant alcohol consumption. It embraces a pathological spectrum from simple steatosis to steatohepatitis. 10%-20% have steatohepatitis (non-alcoholic steatohepatitis), which can progress to cirrhosis and hepatocellular carcinoma[1]. NAFLD and non-alcoholic steatohepatitis are increasingly a cause of cirrhosis and hepatocellular carcinoma globally. This burden is expected to increase as epidemics of obesity, diabetes and metabolic syndrome continue to grow[2]. Atherosclerosis (ATH) is a chronic disease of the arterial wall, and a leading cause of death and loss of productive life years worldwide. Its distinctive feature is a hardening of any artery specifically due to atheromatous plaques[3].
These conditions are increasingly recognized in primary care and specialist practice, which is largely due to the greater availability of non-invasive diagnostic tools. Nonetheless, quantifying future disease burden has always been challenging due to paucity of data in important areas, mandating an international, concerted effort to improve our understanding[4].
ATH and NAFLD are medical conditions that straddle a communal epidemiology, underlying mechanism and a clinical syndrome that has protean manifestations, touching every organ in the body[5]. Both entities stem from pathology, which seems certain and unarguable when considered alone, but when considered together, areas of uncertainty arise[6]. Interrelationship between the two conditions are many, sharing epidemiology and risk factors[7] which call for behavioral change interventions both in prevention and in therapy, but also challenging multi-factorial mechanisms by the quest of omics approaches[8], requiring computational biology analysis[9]. The conceptual milieu implies the overlap of a realistic theory of change, because implies lifestyle interventions focused on risk factors, with bioinformatics tools for the management of big data not comprehensive of all recognized risk components and indexes[10].
In the real clinical world, easy-to-assess proxies of ATH are frequently preferred: It is needed to have the awareness of using them as assumptions more than as well supported reference standards[11]. Accordingly, the present overview focuses to briefly delimit the area of the subject matter explicitly addressing which assumptions are still waiting for a demonstration, beyond frail demonstrations of association or correlation.
Arterial stiffness is deemed to occur as a consequence of both biological ageing and arteriosclerosis[12]. Stiffened arteries require a greater amount of force to permit them to accommodate the stroke volume of the heart. The main consequence is an increase in pulse pressure which damages blood vessels in target organs such as the heart, brain or kidneys[13].
Measurement of aortic pulse wave velocity (PWV) is conceptually related to arterial stiffness[13]. By this acknowledgment, PWV, as a proxy of arterial stiffness, is credited to provide statistical evidence concerning the likelihood of occurrence of cardiovascular disease, and in some cases, of all cause mortality[13]. This notion has some epidemiological support: Regretfully, and surprisingly, no PWV measurement is currently recommended for any practical and accepted general use[14].
Imaging measures of fat liver content have considerable weaknesses[15] given that they do not have complete correspondence to histology: Nonetheless, they have a key role in medical practice, which is extensive and well appreciated, providing a suitable way for monitoring liver fatty content over time and after therapeutic interventions[16].
Current therapeutic evidence supports the recommendation of addressing changes toward healthier lifestyles, including diet and physical exercise, in both ATH and NAFLD, even when defined by non-invasive methodology[15]. Although such lifestyle approaches are acknowledged as effective interventions, they are questionably demonstrated by few clinical trials[17]. Disappointingly, such studies do not appear to be fully adequate due to limitations of size, duration and methods[18]. Accordingly, seemingly, none is currently considered suitable for promoting definitive and worldwide shared guidelines[15].
Research studies on the “association between aortic stiffness and liver steatosis in morbidly obese patients” have been published in several journals recently. One of them[19], deserves greater consideration because it is based on a realistic anatomic measure of fat content, and because, despite its goal and careful design and development, it recognizes that any independent relationship between aortic stiffness and fatty liver are missing in the results achieved. Both conditions depend, as expected, on better known, and lasting, risk factors: Namely, arterial hypertension, increased body weight and diabetes[19]. Apart from these points, this study is very valuable because its reference is not only that an appropriate liver histology sampling was available, but also because the measure of aortic stiffness was done by a reliable imaging-dependent tool, using an appropriate distance-based velocity measurement. These relevant features are very well displayed and justified within the article[19], and its lack is a major flaw of previous studies. Such combined approach is an advance, since previous studies have been performed with similar purposes but with more biased, “qualitative” and “subjective” methods[20]. The effort made in better understanding and facing the challenge of these two frequently overlapping diseases, even in the specific subset of extremely obese people, as in this investigation, promotes a negative answer to the claim of a causative relationship between ATH and NAFLD, if any, and, more, to the inclusion of NAFLD as a suitable concurrent risk factor for ATH[19].
Investigations and publications, using very indirect ATH and fatty liver imaging to assess patients' risk, may have also the aim of facilitating future drug trials[20]. However, there are many pros and cons, and a matter of concern is the disproportionately big and continuous flood of scientific contributions[20]: This, by itself, may impair an appreciation of the usefulness of these procedures to be used. The core of this valuable debate is mostly concealed by a kind of implicit but not evidence-based acceptance of the diagnostic merit of such very indirect measurement tools[15]. Nonetheless, several researchers unexpectedly are converging towards some agreement for accepting them as sustainable reference and indexes of outcome[15].
Even in a relatively limited field of knowledge and science, such as medical approaches to the development of a mostly affluent disease, a warning regarding the misuse of methods, alleged paradigms and unsupported axioms is needed[21]. Actually, scientific research, both basic and applied, is a dynamic process, constantly evolving and changing perspective, with critical thinking being at the core of the scientific method. In their daily work, scientists of every field are urged to keep pace with a broad spectrum of available data[22]. Interaction and overlap between these two fields of research, basic and applied, may allow us to solve particular problems or questions, and both may enhance novel knowledge and information[22]. The twin partners, ATH and NAFLD, are only apparently straightforward and relatively simple topics, and their interdependence calls for definitions without biases. Actually, encompassing many prevalent diseases and being related to several and recognized risk factors and health determinants, the study of the mutual relationship between NAFLD and ATH should involve big data analytics approaches[23,24]. Regretfully, available studies are not sufficiently comprehensive, not including even part of the data actually available in the specific database. There is a general context that may have effects on both fatty liver- and obesity- and on arteriosclerosis and related heart, brain and kidney diseases. This context encompasses the environment at large[25], behavioral factors[26], quantity and quality of dietary intake[27], with consequent obesity or nutritional-related disturbance[28], sedentary life, stress, detrimental levels of physical activity, sleep deprivation and night shifts for work or leisure[29], and certainly many others. Despite these limitations, overall, the effects of well-addressed intervention are reported as beneficial[30-32].
In brief, regarding the mutual relationship of ATH and NAFLD, no element reasonably suggests, apart from quite naive statistics, that one condition affects the other directly, despite the attractive hypothesis that fatty liver in itself may cause vascular damage. In these matters, it is always unsafe to treat contemporaneous events as causation[33,34].
Within other backgrounds and perspectives, the scientific community is the silent bystander of determined, even unreasonable, anti-science strain and campaigns[21]. Rejection of scientific method as an objective tool that can generate universal knowledge is of great concern for scientists and health professionals[21]. This eschewal may originate from the idea that scientific reductionism is inherently limited in reaching understanding of complex problems and, namely, health and disease topics. The very relevant ongoing debate on the “misuse of statistical significance”[35], leading sometimes to discarding of genuine discoveries, may add further fuel to mistrust in science and medicine. Reciprocally, suggesting conjectural “mechanisms of disease”, such as claiming the long shadow of NAFLD as a “risk factor”, if not as a causative factor of arterial stiffness and ATH, is probably very much overreaching reality and is harmful for the scientific credence of this area of medicine. “As long as different positions are discussed scientifically, controversy has a chance to move forward”[22]. This is a very important commitment for the physician, the researcher, the research projects evaluator and the reviewer. No golden rule is available, but the use of “naive” methods, not sufficiently adequate for the purposes of the scientific questions, when detected as inappropriate or frankly biased, should be reasonably discouraged and discarded.
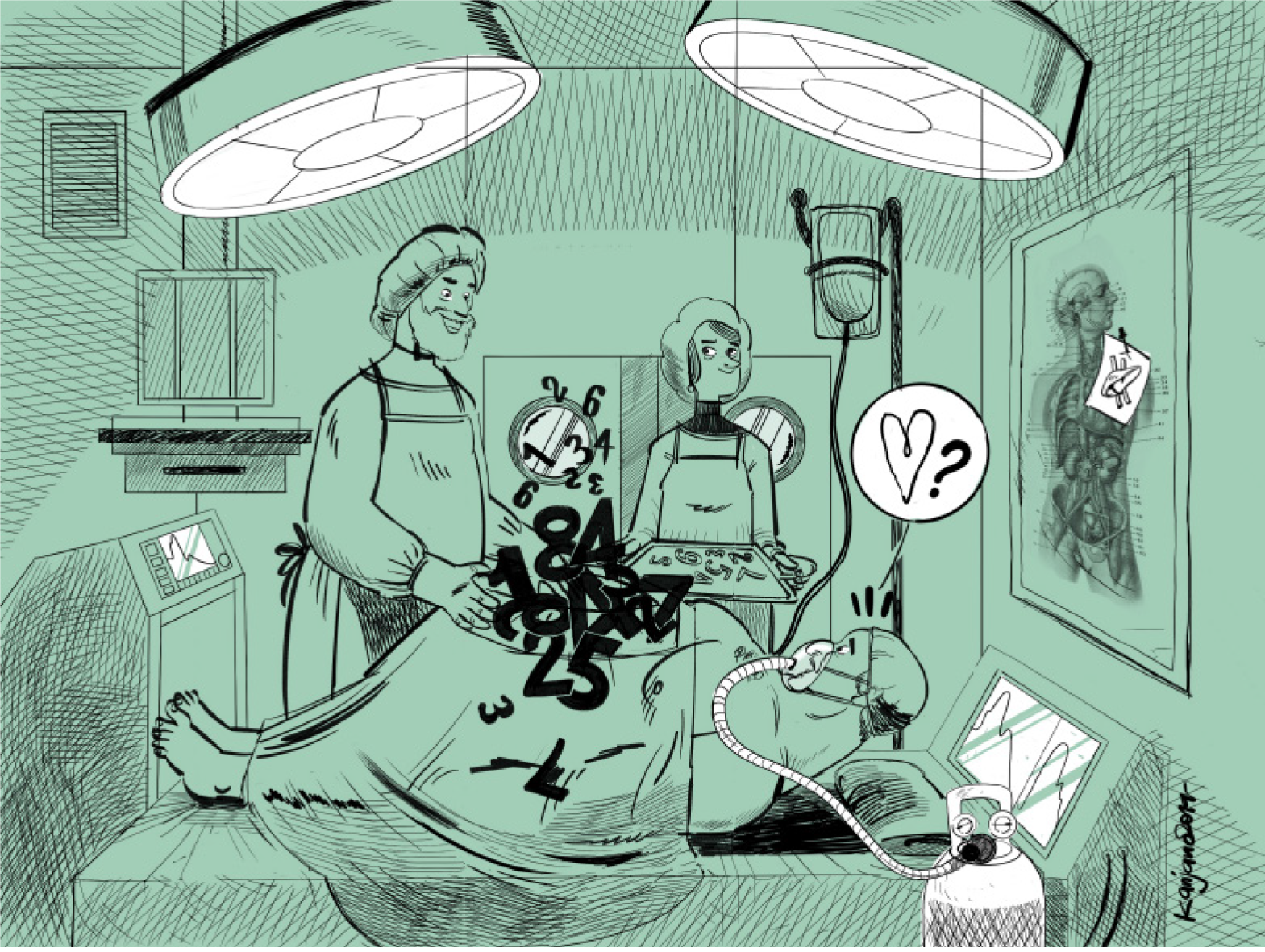
Disease study processes are often too rigid, we must agree. In fact, the aim is to collect sufficient evidence, best if coordinated in a convincing architecture, relationships and support, in ways very similar to the theory of change. In fact, the study of diseases often, as in our case, includes the quantitative observation of numerous data and of the changes that are determined with interventions, spontaneous or within clinical trials. In this sense it is acceptable that there are assumptions that are not strongly supported, but it is quite possible that these assumptions are inconsistent and misleading so that, when detected, must be included as biases or mistakes in the proposed rationale of the dependent intervention for change. Despite the verification that NAFLD and cardiovascular disease are strongly interrelated[36], current evidence is that NAFLD may be only a possibly useful indicator for flagging early arteriosclerosis[37], and not a likely causative factor. Greater sustainable contributions by precision medicine tools, i.e., by validated bioinformatics approaches and expertise, are needed to allow consideration of any role of big data and how they should be managed[38]. Very valuable investigations are already available, providing new insights into the relationship of NAFLD, fibrosis and ATH[39]. Also the shared molecular basis for ATH and vascular disease and its molecular relationships with several related diseases, namely NAFLD and Alzheimer’s disease, are the focus of frontiers research in very well planned and managed investigations[39,40]. Currently, pathway-based analysis are elucidating key molecular mechanisms underlying complex diseases addressing the joint effect and integrality as function unit of multiple genes by extensive studies exploring large-scale “-omics” data[41]. In the mind and perception of most people, what matters is if such information and measures may guide the daily choices of physicians and if they may empower the adherence of patients to prescriptions, therapeutic pathways or lifestyle choices. The answer may be yes, but this is more a real world practice affair than the conclusion of any existing or ongoing trial or of any computational statistics analysis and prediction. The methodology described above, as in most more traditional research investigating associations and relationships, alludes implicitly to the assertion that where shadows overlap, they appear darker: Which should mean better visible, if not “clearer”. However, this is not necessarily true. Actually, something is problematic in this assertion, and, more important, we may argue that it is where shadows overlap, that may matter. The need to integrate more omics data with different ones, such as epigenetic or epidemiological data, by bioinformatics, is evident when dealing with mechanisms and processes involving long cascades of multiple biological pathways[42] (Figure 1).
The unpredictability of synergy among different pathways and the possibility of over-fitting, i.e., the production of an analysis that corresponds too closely or exactly to a particular set of data, and may therefore fail to fit additional data or predict future observations reliably, must be appropriately considered when trying to illustrate the genetic, epigenetic, and environmental determinants of trigger and development of any disease[43]. Conceivably, when dealing with cross-talk of liver with ATH and fat cells[44], we should take into account what is actually overlapping, when, where, how and why. Mirroring the shadows of concepts, as we do using indirect or surrogate measures of ATH and of fatty liver, respectively, might be an unreliable and even misleading approach. Indeed, we are still waiting for high quality prospective studies in diverse racial-ethnic groups to further elucidate whether or not NAFLD is in fact causally related to ATH, while actual information provides some suggestion of limited associations[45,46]. The risk and the bias of a this clinical research tale are that, at last, some conclusion, as equally some intervention, based on uncertain assumptions might ultimately succeed in darkening or obscuring, certainly not enlightening concepts and mechanisms. The result will be weakening the strength of consequent warranted intervention which are still based on awareness and participatory behavioral changes[47] and on intervention models based on a theory of change[48], which usually is not clearly developed and monitored, as needed.
Manuscript source: Invited Manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Rezaee-Zavareh MS, Villela-Nogueira C S-Editor: Tang JZ L-Editor: A E-Editor: Liu MY
| 1. | Pimpin L, Cortez-Pinto H, Negro F, Corbould E, Lazarus JV, Webber L, Sheron N; EASL HEPAHEALTH Steering Committee. Burden of liver disease in Europe: Epidemiology and analysis of risk factors to identify prevention policies. J Hepatol. 2018;69:718-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 476] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 2. | Estes C, Anstee QM, Arias-Loste MT, Bantel H, Bellentani S, Caballeria J, Colombo M, Craxi A, Crespo J, Day CP, Eguchi Y, Geier A, Kondili LA, Kroy DC, Lazarus JV, Loomba R, Manns MP, Marchesini G, Nakajima A, Negro F, Petta S, Ratziu V, Romero-Gomez M, Sanyal A, Schattenberg JM, Tacke F, Tanaka J, Trautwein C, Wei L, Zeuzem S, Razavi H. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. 2018;69:896-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 776] [Cited by in RCA: 1308] [Article Influence: 186.9] [Reference Citation Analysis (0)] |
| 3. | Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2419] [Cited by in RCA: 2788] [Article Influence: 199.1] [Reference Citation Analysis (0)] |
| 4. | Mahady SE, George J. Predicting the future burden of NAFLD and NASH. J Hepatol. 2018;69:774-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Tana C, Ballestri S, Ricci F, Di Vincenzo A, Ticinesi A, Gallina S, Giamberardino MA, Cipollone F, Sutton R, Vettor R, Fedorowski A, Meschi T. Cardiovascular Risk in Non-Alcoholic Fatty Liver Disease: Mechanisms and Therapeutic Implications. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 6. | Oni ET, Agatston AS, Blaha MJ, Fialkow J, Cury R, Sposito A, Erbel R, Blankstein R, Feldman T, Al-Mallah MH, Santos RD, Budoff MJ, Nasir K. A systematic review: burden and severity of subclinical cardiovascular disease among those with nonalcoholic fatty liver; should we care? Atherosclerosis. 2013;230:258-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 281] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 7. | Patil R, Sood GK. Non-alcoholic fatty liver disease and cardiovascular risk. World J Gastrointest Pathophysiol. 2017;8:51-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 82] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 8. | Han J, Wang Y, Yuan Z, Liu L, Zhao M, Guan Q, Zhang H, Li Q, Xu J, Gao L, Zhao J, Zhang X. Nonalcoholic fatty liver disease represents a greater metabolic burden in patients with atherosclerosis: A cross-sectional study. Medicine (Baltimore). 2019;98:e14896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Blencowe M, Karunanayake T, Wier J, Hsu N, Yang X. Network Modeling Approaches and Applications to Unravelling Non-Alcoholic Fatty Liver Disease. Genes (Basel). 2019;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Aromatario O, Van Hoye A, Vuillemin A, Foucaut AM, Pommier J, Cambon L. Using theory of change to develop an intervention theory for designing and evaluating behavior change SDApps for healthy eating and physical exercise: the OCAPREV theory. BMC Public Health. 2019;19:1435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Trovato GM, Tamura K. The lesson of ankle-brachial index for long-term clinical outcomes: Time is not a line, but a series of now-points. Atherosclerosis. 2016;250:186-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Motau TH, Norton GR, Sareli P, Woodiwiss AJ. Aortic Pulse Pressure Does Not Adequately Index Cardiovascular Risk Factor-Related Changes in Aortic Stiffness and Forward Wave Pressure. Am J Hypertens. 2018;31:981-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler MM, Witteman JC. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006;113:657-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1350] [Cited by in RCA: 1438] [Article Influence: 75.7] [Reference Citation Analysis (0)] |
| 14. | Trovato GM. Clinical research and methodology. The paradigm of fatty liver and atherosclerosis behind the chicken or the egg dilemma. Atherosclerosis. 2016;249:228-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Buckley AJ, Thomas EL, Lessan N, Trovato FM, Trovato GM, Taylor-Robinson SD. Non-alcoholic fatty liver disease: Relationship with cardiovascular risk markers and clinical endpoints. Diabetes Res Clin Pract. 2018;144:144-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | Castera L, Friedrich-Rust M, Loomba R. Noninvasive Assessment of Liver Disease in Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2019;156:1264-1281.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 619] [Cited by in RCA: 1036] [Article Influence: 172.7] [Reference Citation Analysis (0)] |
| 17. | Karimi L, Mattace-Raso FU, van Rosmalen J, van Rooij F, Hofman A, Franco OH. Effects of combined healthy lifestyle factors on functional vascular aging: the Rotterdam Study. J Hypertens. 2016;34:853-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Hawkes C, Smith TG, Jewell J, Wardle J, Hammond RA, Friel S, Thow AM, Kain J. Smart food policies for obesity prevention. Lancet. 2015;385:2410-2421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 461] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 19. | Styczyński G, Kalinowski P, Michałowski Ł, Paluszkiewicz R, Ziarkiewicz-Wróblewska B, Zieniewicz K, Tataj E, Szmigielski C, Jędrusik P. No association between aortic stiffness and liver steatosis in morbidly obese patients. Atherosclerosis. 2019;287:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Nanchen D, Raggi P. Is atherosclerosis imaging the most sensitive way to assess patients' risk and the best way to conduct future drug trials? A pros-and-cons debate. Atherosclerosis. 2017;266:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Baron RJ, Berinsky AJ. Mistrust in Science - A Threat to the Patient-Physician Relationship. N Engl J Med. 2019;381:182-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | von Eckardstein A, Negrini S. Clinical and scientific debates on atherosclerosis: The truth lies somewhere in the middle. Atherosclerosis. 2017;266:228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Moore JB. From sugar to liver fat and public health: systems biology driven studies in understanding non-alcoholic fatty liver disease pathogenesis. Proc Nutr Soc. 2019;78:290-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Zhang Z, Salisbury D, Sallam T. Long Noncoding RNAs in Atherosclerosis: JACC Review Topic of the Week. J Am Coll Cardiol. 2018;72:2380-2390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 25. | Vlachopoulos C, Aggelakas A, Ioakeimidis N, Xaplanteris P, Terentes-Printzios D, Abdelrasoul M, Lazaros G, Tousoulis D. Music decreases aortic stiffness and wave reflections. Atherosclerosis. 2015;240:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Trovato GM, Martines GF, Trovato FM, Catalano D. Re: "Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population". Am J Epidemiol. 2013;178:661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Catalano D, Trovato GM, Pace P, Martines GF, Trovato FM. Mediterranean diet and physical activity: an intervention study. Does olive oil exercise the body through the mind? Int J Cardiol. 2013;168:4408-4409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Levin A, Tang M, Perry T, Zalunardo N, Beaulieu M, Dubland JA, Zerr K, Djurdjev O. Randomized Controlled Trial for the Effect of Vitamin D Supplementation on Vascular Stiffness in CKD. Clin J Am Soc Nephrol. 2017;12:1447-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 29. | Trovato FM, Martines GF, Brischetto D, Catalano D, Musumeci G, Trovato GM. Fatty liver disease and lifestyle in youngsters: diet, food intake frequency, exercise, sleep shortage and fashion. Liver Int. 2016;36:427-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 133] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 30. | Trovato GM, Pirri C, Martines GF, Tonzuso A, Trovato F, Catalano D. Lifestyle interventions, insulin resistance, and renal artery stiffness in essential hypertension. Clin Exp Hypertens. 2010;32:262-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Oliveira NL, Ribeiro F, Silva G, Alves AJ, Silva N, Guimarães JT, Teixeira M, Oliveira J. Effect of exercise-based cardiac rehabilitation on arterial stiffness and inflammatory and endothelial dysfunction biomarkers: a randomized controlled trial of myocardial infarction patients. Atherosclerosis. 2015;239:150-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | Laskey W, Siddiqi S, Wells C, Lueker R. Improvement in arterial stiffness following cardiac rehabilitation. Int J Cardiol. 2013;167:2734-2738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Trovato FM, Catalano D, Musumeci G, Trovato GM. 4Ps medicine of the fatty liver: the research model of predictive, preventive, personalized and participatory medicine-recommendations for facing obesity, fatty liver and fibrosis epidemics. EPMA J. 2014;5:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Cvitanović T, Reichert MC, Moškon M, Mraz M, Lammert F, Rozman D. Large-scale computational models of liver metabolism: How far from the clinics? Hepatology. 2017;66:1323-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature. 2019;567:305-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1318] [Cited by in RCA: 1515] [Article Influence: 252.5] [Reference Citation Analysis (0)] |
| 36. | Lonardo A, Ballestri S, Guaraldi G, Nascimbeni F, Romagnoli D, Zona S, Targher G. Fatty liver is associated with an increased risk of diabetes and cardiovascular disease - Evidence from three different disease models: NAFLD, HCV and HIV. World J Gastroenterol. 2016;22:9674-9693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 101] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 37. | Zhu WH, Fang LZ, Lu CR, Dai HL, Chen JH, Qiao QH, Chen LY. Correlation between non-alcoholic fatty liver with metabolic risk factors and brachial-ankle pulse wave velocity. World J Gastroenterol. 2015;21:10192-10199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Chen Y, Xu M, Wang T, Sun J, Sun W, Xu B, Huang X, Xu Y, Lu J, Li X, Wang W, Bi Y, Ning G. Advanced fibrosis associates with atherosclerosis in subjects with nonalcoholic fatty liver disease. Atherosclerosis. 2015;241:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 39. | Zhao X, Luan YZ, Zuo X, Chen YD, Qin J, Jin L, Tan Y, Lin M, Zhang N, Liang Y, Rao SQ. Identification of Risk Pathways and Functional Modules for Coronary Artery Disease Based on Genome-wide SNP Data. Genomics Proteomics Bioinformatics. 2016;14:349-356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Xu P, Zhai Y, Wang J. The Role of PPAR and Its Cross-Talk with CAR and LXR in Obesity and Atherosclerosis. Int J Mol Sci. 2018;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 41. | VanWagner LB. New insights into NAFLD and subclinical coronary atherosclerosis. J Hepatol. 2018;68:890-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 42. | Pais R, Redheuil A, Cluzel P, Ratziu V, Giral P. Relationship Among Fatty Liver, Specific and Multiple-Site Atherosclerosis, and 10-Year Framingham Score. Hepatology. 2019;69:1453-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 43. | Subramanian J, Simon R. Overfitting in prediction models - is it a problem only in high dimensions? Contemp Clin Trials. 2013;36:636-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 44. | Lim S, Taskinen MR, Borén J. Crosstalk between nonalcoholic fatty liver disease and cardiometabolic syndrome. Obes Rev. 2019;20:599-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 45. | Chang Y, Ryu S, Sung KC, Cho YK, Sung E, Kim HN, Jung HS, Yun KE, Ahn J, Shin H, Wild SH, Byrne CD. Alcoholic and non-alcoholic fatty liver disease and associations with coronary artery calcification: evidence from the Kangbuk Samsung Health Study. Gut. 2019;68:1667-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 126] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 46. | Leite NC, Villela-Nogueira CA, Ferreira MT, Cardoso CR, Salles GF. Increasing aortic stiffness is predictive of advanced liver fibrosis in patients with type 2 diabetes: the Rio-T2DM cohort study. Liver Int. 2016;36:977-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Wang C, Bowen DJ, Kardia SL. Research and practice opportunities at the intersection of health education, health behavior, and genomics. Health Educ Behav. 2005;32:686-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 48. | Asada Y, Gilmet K, Welter C, Massuda-Barnett G, Kapadia DA, Fagen M. Applying Theory of Change to a Structural Change Initiative: Evaluation of Model Communities in a Diverse County. Health Educ Behav. 2019;46:377-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |