Published online Oct 15, 2019. doi: 10.4291/wjgp.v10.i3.36
Peer-review started: July 12, 2019
First decision: August 30, 2019
Revised: September 6, 2019
Accepted: September 22, 2019
Article in press: September 22, 2019
Published online: October 15, 2019
Processing time: 133 Days and 8.9 Hours
Neutropenic enterocolitis (NE) is a predominantly cecum-based disease with high mortality seen in patients post chemotherapy. The pathogenesis of NE is poorly understood and probably multifactorial involving mucosal injury, neutropenia, and impaired host defense to intestinal organisms. The clinical presentation is characterized as ileocolonic inflammation and bowel wall thickening in patients with neutropenia, fever, and abdominal pain. The pathological features of NE include patchy necrosis, hemorrhage, ulcer, edema, perforation, infiltrating organisms, and characteristically, depletion of inflammatory cells (neutrophils). NE should always be considered as a possible diagnosis in immunosuppressed patients, especially those receiving chemotherapy. High clinical and histological diagnostic discordance rate exists. High index of clinical suspicion and prompt appropriate personalized management are essential to achieve a lower mortality rate.
Core tip: Neutropenic enterocolitis (NE) is a predominantly cecum-based disease with high mortality seen in patients post chemotherapy. The pathogenesis of NE is still poorly understood. The clinical presentation is characterized as ileocolonic inflammation and bowel wall thickening in patients with neutropenia, fever, and abdominal pain. The pathological features of NE include patchy necrosis, hemorrhage, ulcer, edema, perforation, infiltrating organisms, and characteristically, depletion of inflammatory cells (neutrophils). High clinical and histological diagnostic discordance rate exists. High index of clinical suspicion and timely diagnosis are critical for patient appropriate treatment and improvement of survival.
- Citation: Xia R, Zhang X. Neutropenic enterocolitis: A clinico-pathological review. World J Gastrointest Pathophysiol 2019; 10(3): 36-41
- URL: https://www.wjgnet.com/2150-5330/full/v10/i3/36.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v10.i3.36
Neutropenic enterocolitis (NE) was also named as typhlitis, typhlenteritis, ileocecal syndrome, or cecitis. NE is a clinical entity described mostly in patients with hematologic malignancies, as well as other immunosuppressive causes such as acquired immune deficiency syndrome (AIDS), therapy for solid tumors, and organ transplant[1-6]. The clinical presentation is characterized as ileocolonic inflammation in patients with neutropenia, fever, and abdominal pain[5,6]. The cecum is the most commonly reported site to be involved[6,7]. The mortality of NE can reach up to 100% due to complications of malignancy, sepsis, or bowel necrosis and perforation[6,8]. In recently years, early recognition and progress in management have reduced mortality substantially[9,10]. A recent study showed a mortality rate of 32.1% in the intensive care units and a hospital mortality rate of 38.8%[11]. The clinical diagnosis of NE relies on major criteria and minor criteria. The major criteria include neutropenia, fever, and bowel wall thickening on computed tomography (CT) or ultrasound imaging. The minor criteria consist of nonspecific symptoms including abdominal pain, distension cramping, diarrhea, or lower gastrointestinal bleeding[11]. The NE patients are often in critical condition which may not permit endoscopic examination or surgical resection. Therefore, the pathologic features of NE have not been well recognized, and a high clinical and histological diagnostic discordance rate has been reported in NE cases[5].
The true occurrence rate of NE is unknown, which has been estimated at about 5% of patients hospitalized for leukemia/lymphoma, aplastic anemia or solid tumors treated with chemotherapy[12]. Neutropenia is the major risk factor for the development of NE. NE can develop in leukemia patients or patients in neutropenic condition receiving high dose chemotherapy to treat malignancies. Other conditions related to neutropenia include multiple myeloma, lymphoma, aplastic anemia, myelodysplastic syndromes, drug-induced neutropenia, cyclical neutropenia, agranulocytosis, and other immunosuppressive conditions such as AIDS and post-transplant patients[6,9]. NE patients usually present with nonspecific abdominal pain, diarrhea, nausea, vomiting, and abdominal distension[6,13]. Symptoms usually present 10-14 d post starting chemotherapy.
The initial diagnosis of NE is usually established by detection of the characteristic CT findings in neutropenic patients presenting with fever, abdominal pain and tenderness. The most common CT findings in NE is bowel wall thickening. Other CT findings include stranding mesentery, dilated bowel, enhancement of mucosa, and intestinal pneumatosis[6]. The abnormal findings mostly involve the ascending colon and cecum[14]. Plain films of the abdomen are nonspecific, but, are useful for detecting free air[6]. Occasionally, abdominal X-ray may show diffusely distended cecum and adjacent dilated small intestine, signs of thumbprinting, or localized pneumatosis intestinalis, suggestive of NE if clinical background fits[15]. Barium enema is contradicted in potential NE patients, due to its risk to cause bowel perforation[16,17]. In addition to CT scanning, detection of micro- organisms in blood and stool cultures and Clostridioides difficile toxin assays can help identify the superposed infection and decide the management of the patients[18].
Histologic examination is the gold standard for the diagnosis of NE[19]. However, colonoscopy is relatively contraindicated in NE patients, as air insufflation may result in bowel perforation[5,20]. In patients who underwent colonoscopy examination or surgical resection of bowel segment, the gross findings in colonoscopy or surgical resection specimen include: Presence of patchy irregularity and nodularity, friable mucosa, and mass-like lesion that mimics malignancy[5,21]. Occasionally, NE causes perforation of the bowel, a leading cause of death in NE[22]. The cecum and right colon are involved in nearly all the cases (Figure 1). Other bowel segments such as terminal ileum, transverse colon and left colon can also be variably involved. However, NE lesions are not reported in the appendix or rectum so far[5].
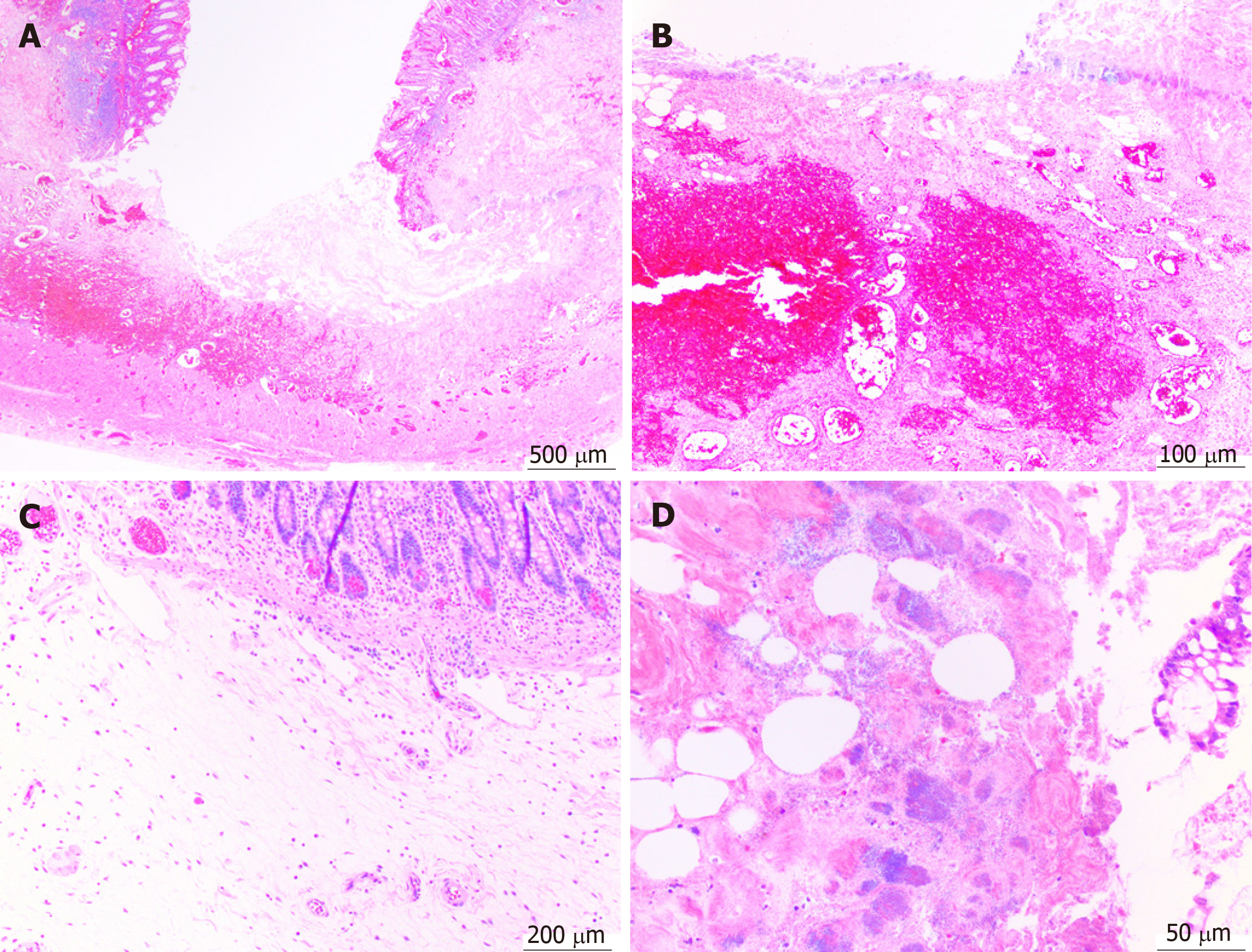
The key histopathologic features of NE are marked hemorrhagic necrosis, mucosal ulceration, extensive edema in the submucosa and laminal propria, marked congestion and even deep mural and transmural necrosis (Figure 2A-D)[5]. Most importantly, significant infiltrative inflammation should be absent in NE due to the profound neutropenia. Many cases are accompanied by infiltrating organisms like bacteria or fungus hyphae. However, inflammatory cell infiltration is still depleted despite in background of organism overgrowth[14]. Apoptotic bodies are not prominent in NE cases, distinguishing NE from the graft-versus-host disease, mycophenolate mofetil-induced injury and immune checkpoint inhibitor induced colitis[22].
The pathogenesis of NE is poorly understood and probably multifactorial involving mucosal injury, neutropenia, and impaired host defense to intestinal organisms. The initial morbidities of the patients lead to intestinal edema, engorged vessels, and mucosal surface disruption, especially of the ileocolonic segments. Chemotherapeutic agents like cytarabine can directly cause mucositis or predispose to intestinal distension and necrosis, and consequently impair the intestinal motility. The initial intestinal mucosal injury in the background of immunocompromised state of the afflicted patients leads to intestinal edema, vascular dilation, mucosal disruption, and bacterial intramural invasion[5-7]. Moreover, intestinal leukemic infiltration may be a superposed factor in the pathogenesis of NE[23]. Neutropenia and the use of steroids complicate the situation by reducing host defenses against infection. Microbes including variety of bacteria, fungi and cytomegalovirus have been implicated as causes[24-26].
Clinically and radiologically, many conditions can overlap with NE and its mimics including acute appendicitis, appendiceal abscess, ischemic enteritis, Clostridium difficile colitis, graft-versus-host disease, mycophenolate mofetil-induced injury, and enteric involvement by lymphoma/leukemia[5,6]. Recent high-dose chemotherapy along with the symptoms of fever and abdominal pain, lab finding of neutropenia, and imaging finding of bowel wall thickening will aid the diagnosis of NE. A timely diagnosis and proper management will significantly improve the prognosis[11]. Histopathological findings are the gold standard to distinguish NE from its mimics, if diagnostic tissue especially resection specimen is available for pathology examination. In a multi-institutional histological study of NE lesions, high discordance rate (35%) between clinical and pathologic diagnoses has been reported. Fifteen percent of patients with histologically confirmed NE were not clinically suspected for NE, whereas, twenty six percent of patients with clinically suspected NE were histologically evaluated as non-NE[5].
So far, there is no high-quality prospective or retrospective studies on the treatment of NE, and therefore, no recommended uniform management strategy or guidelines for NE yet. A general approach to patients with NE should be individualized depending on the complications and pre-morbidities of the patients. Treatment of NE patients without significant complications such as peritonitis, perforation, or bleeding is mainly supportive including bowel rest and intravenous fluids supplement, and use of antibiotics[11]. Neutropenia is the major risk factor for the pathogenesis of NE. Cytopenia, coagulopathy, and mucosal hemorrhage can cause coagulopathy. Therefore, coagulation should be monitored in patients with NE and be corrected promptly[7,11]. The use of granulocyte colony stimulating factor can hasten neutrophil recovery and may be beneficial in some patients[7,11]. Surgical intervention has been recommended for patients with evidence of bowel perforation, persistent bleeding even after correction of cytopenia and coagulopathy abnormalities, clinical deterioration in spite of the intensive medical intervention, and the presence of other surgical conditions, e.g., abscess and acute appendicitis[25,27]. Interestingly, patients who recovered from NE are at risk from developing NE again during subsequent chemotherapy. Patients should be fully recovered from NE before a new chemotherapy starts[25].
Neutropenic enterocolitis is a predominantly cecum-based disease with high mortality seen in patients post chemotherapy. The diagnosis of NE should always be considered in immunosuppressed patients, particularly those treated with chemotherapy when they present with appropriate symptoms. The pathogenesis of NE is still unclear and probably multifactorial involving mucosal injury, neutropenia, and impaired host defense to intestinal organisms. The clinical presentation is characterized as colonic inflammation and bowel wall thickening in patients with neutropenia, fever, and abdominal pain. The pathological features of NE include patchy necrosis, hemorrhage, ulcer, edema, perforation, infiltrating organisms, and characteristically, depletion of neutrophil infiltration. High clinical and histological diagnostic discordance rate exists. The differential diagnoses of NE include non-specific chronic and acute colitis, graft-versus-host disease associated colitis, malignancy relapse, drug-induced colitis, acute appendicitis, and bowel ischemia. Conservative treatment or surgical intervention should be tailored to the individual patient. High index of clinical suspicion and prompt appropriate treatment is essential to achieve a lower mortality rate.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cheng DY, Yuksel I S-Editor: Ma RY L-Editor: A E-Editor: Liu MY
| 1. | Miller EE, Reardon LC. Neutropenic Enterocolitis in a Pediatric Heart Transplant Recipient on Multiple Immunosuppressants. Case Rep Transplant. 2018;2018:3264921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Kaito S, Sekiya N, Najima Y, Sano N, Horiguchi S, Kakihana K, Hishima T, Ohashi K. Fatal Neutropenic Enterocolitis Caused by Stenotrophomonas maltophilia: A Rare and Underrecognized Entity. Intern Med. 2018;57:3667-3671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Pelletier JH, Nagaraj S, Gbadegesin R, Wigfall D, McGann KA, Foreman J. Neutropenic enterocolitis (typhlitis) in a pediatric renal transplant patient. A case report and review of the literature. Pediatr Transplant. 2017;21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Chow EJ, Bishop KD. Painless neutropenic enterocolitis in a patient undergoing chemotherapy. Curr Oncol. 2016;23:e514-e516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Sachak T, Arnold MA, Naini BV, Graham RP, Shah SS, Cruise M, Park JY, Clark L, Lamps L, Frankel WL, Theodoropoulos N, Arnold CA. Neutropenic Enterocolitis: New Insights Into a Deadly Entity. Am J Surg Pathol. 2015;39:1635-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Rodrigues FG, Dasilva G, Wexner SD. Neutropenic enterocolitis. World J Gastroenterol. 2017;23:42-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 97] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (2)] |
| 7. | Portugal R, Nucci M. Typhlitis (neutropenic enterocolitis) in patients with acute leukemia: a review. Expert Rev Hematol. 2017;10:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Lebon D, Biard L, Buyse S, Schnell D, Lengliné E, Roussel C, Gornet JM, Munoz-Bongrand N, Quéro L, Resche-Rigon M, Azoulay E, Canet E. Gastrointestinal emergencies in critically ill cancer patients. J Crit Care. 2017;40:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Moran H, Yaniv I, Ashkenazi S, Schwartz M, Fisher S, Levy I. Risk factors for typhlitis in pediatric patients with cancer. J Pediatr Hematol Oncol. 2009;31:630-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Machado NO. Neutropenic enterocolitis: A continuing medical and surgical challenge. N Am J Med Sci. 2010;2:293-300. [PubMed] |
| 11. | Duceau B, Picard M, Pirracchio R, Wanquet A, Pène F, Merceron S, Mokart D, Moreau AS, Lengliné E, Canet E, Lemiale V, Mariotte E, Azoulay E, Zafrani L. Neutropenic Enterocolitis in Critically Ill Patients: Spectrum of the Disease and Risk of Invasive Fungal Disease. Crit Care Med. 2019;47:668-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Gorschlüter M, Mey U, Strehl J, Ziske C, Schepke M, Schmidt-Wolf IG, Sauerbruch T, Glasmacher A. Neutropenic enterocolitis in adults: systematic analysis of evidence quality. Eur J Haematol. 2005;75:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 168] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Nesher L, Rolston KV. Neutropenic enterocolitis, a growing concern in the era of widespread use of aggressive chemotherapy. Clin Infect Dis. 2013;56:711-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 14. | Kirkpatrick ID, Greenberg HM. Gastrointestinal complications in the neutropenic patient: characterization and differentiation with abdominal CT. Radiology. 2003;226:668-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 130] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Vogel MN, Goeppert B, Maksimovic O, Brodoefel H, Faul C, Claussen CD, Horger M. CT features of neutropenic enterocolitis in adult patients with hematological diseases undergoing chemotherapy. Rofo. 2010;182:1076-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Kaste SC, Flynn PM, Furman WL. Acute lymphoblastic leukemia presenting with typhlitis. Med Pediatr Oncol. 1997;28:209-212. [PubMed] |
| 17. | Teichmann D, Cummins M, Keogh SJ, Rogers T. The complication of gastro-enteric fistulisation in neutropenic enterocolitis secondary to aplastic anaemia. Pediatr Blood Cancer. 2014;61:358-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Coleman N, Speirs G, Khan J, Broadbent V, Wight DG, Warren RE. Neutropenic enterocolitis associated with Clostridium tertium. J Clin Pathol. 1993;46:180-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Mourad N, Michel RP, Marcus VA. Pathology of Gastrointestinal and Liver Complications of Hematopoietic Stem Cell Transplantation. Arch Pathol Lab Med. 2019;143:1131-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Andreyev HJ, Davidson SE, Gillespie C, Allum WH, Swarbrick E; British Society of Gastroenterology; Association of Colo-Proctology of Great Britain and Ireland; Association of Upper Gastrointestinal Surgeons; Faculty of Clinical Oncology Section of the Royal College of Radiologists. Practice guidance on the management of acute and chronic gastrointestinal problems arising as a result of treatment for cancer. Gut. 2012;61:179-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 214] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 21. | Kulaylat M, Doerr R, Ambrus J. A case presentation and review of neutropenic enterocolitis. J Med. 1997;28:1-19. [PubMed] |
| 22. | Canbolat Ayhan A, Timur C, Bocu E, Gulcin N. Spontaneous intestinal perforation: an atypical presentation of neutropenic enterocolitis-a case report. Case Rep Hematol. 2014;2014:925078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Capria S, Vitolo D, Cartoni C, Dessanti L, Micozzi A, Mandelli F, Meloni G. Neutropenic enterocolitis in acute leukemia: diagnostic and therapeutic dilemma. Ann Hematol. 2004;83:195-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Sadullah S, Nagesh K, Johnston D, McCullough JB, Murray F, Cachia PG. Recurrent septicaemia in a neutropenic patient with typhlitis. Clin Lab Haematol. 1996;18:215-217. [PubMed] |
| 25. | Davila ML. Neutropenic enterocolitis. Curr Opin Gastroenterol. 2006;22:44-47. [PubMed] |
| 26. | Gorschlüter M, Mey U, Strehl J, Schmitz V, Rabe C, Pauls K, Ziske C, Schmidt-Wolf IG, Glasmacher A. Invasive fungal infections in neutropenic enterocolitis: a systematic analysis of pathogens, incidence, treatment and mortality in adult patients. BMC Infect Dis. 2006;6:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Castagnola E, Ruberto E, Guarino A. Gastrointestinal and liver infections in children undergoing antineoplastic chemotherapy in the years 2000. World J Gastroenterol. 2016;22:5853-5866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |