Published online Oct 15, 2010. doi: 10.4291/wjgp.v1.i4.144
Revised: August 12, 2010
Accepted: August 19, 2010
Published online: October 15, 2010
Granulocytic sarcoma is an uncommon and localized extramedullary tumor composed of immature granulocytic cells. It may present in association with acute myeloid leukaemia, myelodysplastic syndrome and chronic myelogenous leukaemia. Granulocytic sarcoma may occur in any anatomical site but involvement of the gastrointestinal tract is rare, especially in the rectum. We report on the case of a 17 year old female who presented with rectal bleeding, abdominal pain and weight loss one mo prior to admission. Rectosigmoidoscopy revealed a rectal polypoid and ulcerated mass. The histological examination of the mass showed granulocytic sarcoma. Bone marrow examination was compatible with acute promyelocytic leukaemia (FAB type M3). This case report is a reminder of this peculiar sign of tumoral syndrome in acute myeloid leukaemia. We also discuss diagnostic methods and analyze the disease course.
- Citation: Benjazia E, Khalifa M, Benabdelkader A, Laatiri A, Braham A, Letaief A, Bahri F. Granulocytic sarcoma of the rectum: Report of one case that presented with rectal bleeding. World J Gastrointest Pathophysiol 2010; 1(4): 144-146
- URL: https://www.wjgnet.com/2150-5330/full/v1/i4/144.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v1.i4.144
Granulocytic sarcoma (GS), also known as one variant of myeloid sarcoma in the World Health Organization classification, is an extramedullary solid tumor composed of myeloid precursor cells. The World Health Organization classification of hematopoietic tumors divides myeloid sarcoma into 2 major categories. The more common form is GS, composed mainly of myloblasts, neutrophils and myeloid precursors. The less common form is monoblastic sarcoma[1]. This tumor occurs commonly in patients with acute myeloid leukaemia (AML) and less commonly in those with myelodysplastic syndrome or chronic myeloproliferative disorders. Incidence of GS varies from 2% to 7% in AML patients and most frequently occurs in acute myeloblastic leukaemia with maturation [French-American-British (FAB) M2][2,3]. However, other subtypes including FABM4 or M5 and M7 have also been described[3]. GS can occur in any organ but the most common sites are the skin, bone/spine and lymph nodes[1]. However, gastrointestinal tract involvement is relatively rare, especially in the rectum. We present a case of rectal GS in a patient with AML (FAB type M3) who presented with rectal bleeding.
A 17 year old female was admitted in July 2005 to our department of Internal Medicine complaining of rectal bleeding, abdominal pain especially located in the left lower quadrant and loss of appetite one month prior to admission. She had no significant medical history. On admission, she was in a stable clinical condition with normal vital signs but looked pale. No hepatosplenomegaly, lymphadenopathy, petechiae or ecchymotic areas were noted. Rectal examination confirmed the presence of blood in the stools and revealed a polypoid and ulcerated mass measuring 2 cm in great diameter budding through the anal verge.
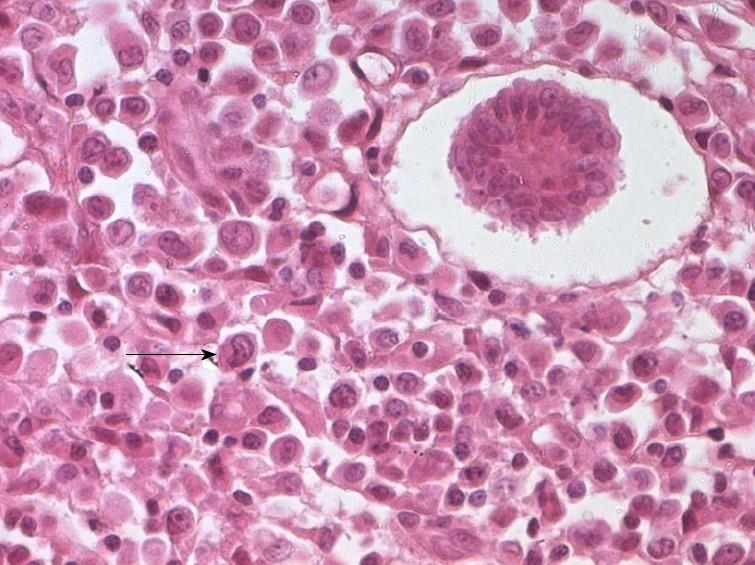
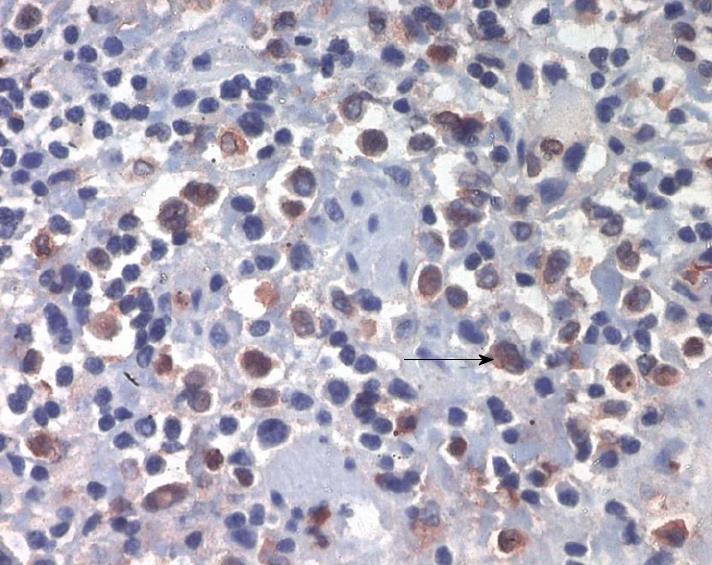
A full blood count showed a hemoglobin of 60 g/L, hematocrit of 20%, white cell count of 4 × 109/L with 20% of blasts and platelet count of 49 × 109/L. Blood chemistry profile showed levels of total protein of 53 g/L, serum albumin of 25 g/L and lactate dehydrogenase of 743 IU/L. Bone marrow examination revealed hypercellularity with an excess of myeloblasts (80%) and markedly depleted hematopoietic cells. The blasts were large with large and irregular nuclei, small basophilic cytoplasm and several azurophilic granules inside. Auer rod bodies and faggot formation were noted in some myeloblasts. Karyotype of the bone marrow cells was 46XX, t(15;17) (q22;q21). The diagnosis was acute promyelocytic leukaemia (FAB type M3). Rectosigmoidoscopy revealed a rectal polypoid and ulcerated mass measuring 2 cm in great diameter budding through the anal verge (Figure 1). Biopsy specimens of the mass showed a massive infiltration of the rectal mucosa by large atypical myeloid cells. Their cytoplasm was eosinophilic and granular. Nuclei were round or convoluted with fine chromatin and one or more fine nucleolus (Figure 2). In addition, lymphocytes, plasma cells and neutrophils were also present. Immunohistochemical stains showed that the infiltrating cells were reactive for myeloperoxidase (Figure 3), lysozyme and CD43. T- and B- cells markers (CD3, CD45) as well as CD30 were negative. These features confirmed the diagnosis of a GS infiltrating the rectum.
The patient received chemotherapy according to the AIDA protocol (All- trans Retinoic acid (ATRA) + Idarubicin). Induction treatment consisted of oral ATRA of the dose of 45 mg/m2 per day associated to intravenous idarubicin at the dose at 12 mg/m2 per day on d 2, 4, 6 and 8 until complete remission. Bone marrow examination at 1 mo follow-up revealed no blast cells and rectosigmoidoscopy showed no mass in the rectum. The patient tolerated the treatment well. After 2 wk of complete remission, treatment was consolidated with 3 courses chemotherapy. At the 4 year follow-up, the patient remained in complete clinical, cytogenetic (karyotype of the bone marrow cells was 46xx) and molecular (transcript PML/RARA was negative) remission.
GS represents an extramedullary tumor of myeloblasts and /or immature myeloid cells. It was first described by Burns in 1811 and given the name chloroma in 1853 by King because of a characteristic greenish color caused by myeloperoxidase in the tumor cells[4]. This unusual tumor can present in four clinicopathological situations: firstly, an additional manifestation in a patient known to have leukaemia; secondly, as a sign of AML in a non leukemic patient at presentation as in the present case; thirdly, as a sign of impending blast crisis in chronic myeloid leukaemia or leukemic transformation in myelodysplastic disorders; and fourthly, as an isolated event[5]. GS involves any site but most commonly affects the skin (13%-22%), bone/spine (9%-25%) and lymph nodes (15%-25%)[3]. Involvement in the gastrointestinal tract is relatively rare and occurs mostly in the small bowel. However, involvement of the colon and rectum is exceedingly rare. To our knowledge, only five patients with isolated colonic and three with rectal granulocytic sarcoma have been described in the literature[6-8].
The most common presentation of GS is abdominal pain, change in bowel habit, small bowel obstruction and less commonly, hemorrhage[9]. In a patient with AML, gastrointestinal bleeding may result from the complication of thrombocytopenia or other coagulopathy disorders caused by leukaemia, especially in FAB M3 type. But this can also be the consequence of infiltration of the gastrointestinal tract by GS.
GS may range from well differentiated tumors on histological examination to those with virtually no evidence of myeloid differentiation. Immunohistochemical study can increase the accuracy of the diagnosis[8]. In fact, the chloroacetate esterase, lysozyme, CD34 and myeloperoxidase stain confirm the granulocytic nature of the tumor cells[7]. In our patient, tumor cells were immunohistochemically positive for lysozyme, myeloperoxidase and CD43. B-cell and T cell lymphomas were excluded by negative stains for CD3 and CD20. The chromosome rearrangement in our patient was t (15;17) which has not been reported with GS previously in the literature. GS has been treated with systemic chemotherapy, surgical resection and radiation therapy. Although only a few large series comparing treatment modalities of GS are available in the literature, systemic chemotherapy seems to offer the most benefit[2]. In our patient, clinical symptoms and GS improved 3 wk after chemotherapy.
In conclusion, GS of the large intestine has seldom been described; this involvement is usually asymptomatic but patients may present with acute abdominal pain, change in bowel habit and rectal bleeding. In addition to thrombocytopenia, rectal involvement of GS must be considered in a patient with AML who presents with rectal bleeding.
Peer reviewers: Joerg Zehetner, MD, Department of Surgery, Keck School of Medicine, University of Southern California, 1510 San Pablo Street, Suite 514, Los Angeles, CA 90033, United States; Chao Qin, MD, Department of Physiology, College of Medicine, University of Oklahoma, Health Sciences Center, Oklahoma City, OK, United States
S- Editor Zhang HN L- Editor Roemmele A E- Editor Liu N
| 1. | Lin CH, Wu KH, Lin WC, Tsai JD, Peng CT, Chen AC. Granulocytic sarcoma of the colon in a child with acute myeloid leukemia presenting as hematochezia. J Pediatr Hematol Oncol. 2008;30:981-983. |
| 2. | Kohl SK, Aoun P. Granulocytic sarcoma of the small intestine. Arch Pathol Lab Med. 2006;130:1570-1574. |
| 3. | Yamauchi K, Yasuda M. Comparison in treatments of nonleukemic granulocytic sarcoma: report of two cases and a review of 72 cases in the literature. Cancer. 2002;94:1739-1746. |
| 4. | D'Alteroche L, Mor C, Durand V, De Muret A, Benbouker L, Colombat P, Danquechin Dorval E. [Gastric granulocytic sarcoma revealed by a massive digestive hemorrhage]. Gastroenterol Clin Biol. 1999;23:779-782. |
| 5. | Catalano MF, Levin B, Hart RS, Troncoso P, DuBrow RA, Estey EH. Granulocytic sarcoma of the colon. Gastroenterology. 1991;100:555-559. |
| 6. | Dabbagh V, Browne G, Parapia LA, Price JJ, Batman PA. Granulocytic sarcoma of the rectum: a rare complication of myelodysplasia. J Clin Pathol. 1999;52:865-866. |
| 7. | Lazaris AC, Papanikolaou IS, Xirou PA. Coexistence of a granulocytic sarcoma and adenocarcinoma of the rectum. Am J Gastroenterol. 2001;96:615-616. |
| 8. | Best-Aguilera CR, Vazquez-Del Mercado M, Muñoz-Valle JF, Herrera-Zarate L, Navarro-Hernandez RE, Martin-Marquez BT, Oregon-Romero E, Ruiz-Quezada S, Bonilla GM, Lomeli-Guerrero A. Massive myeloid sarcoma affecting the central nervous system, mediastinum, retroperitoneum, liver, and rectum associated with acute myeloblastic leukaemia: a case report. J Clin Pathol. 2005;58:325-327. |