Copyright
©2013 Baishideng Publishing Group Co.
World J Gastrointest Pathophysiol. Feb 15, 2013; 4(1): 1-11
Published online Feb 15, 2013. doi: 10.4291/wjgp.v4.i1.1
Published online Feb 15, 2013. doi: 10.4291/wjgp.v4.i1.1
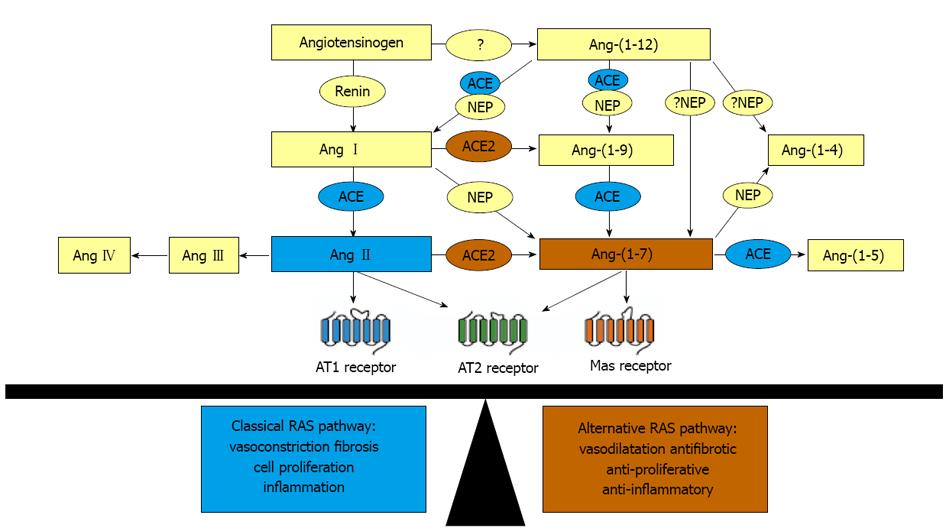
Figure 1 Overview of the renin angiotensin system.
The effects of the renin angiotensin system (RAS) are determined by the balance between the angiotensin II (Ang II)-mediated “classical” axis, depicted in blue, which is vasoconstrictive and the angiotensin-(1-7) [Ang-(1-7)]-mediated “alternate” axis, depicted in orange, which is vasodilatory. Both Ang II and Ang-(1-7) can stimulate the Ang II type 2 (AT2) receptor, depicted in green; the effects of which are often analogous to those mediated by the Ang-(1-7) receptor Mas. Recent evidence indicates that a new member, Ang-(1-12), which is cleaved from angiotensinogen, also contributes either indirectly via Ang I or directly to the pool of Ang-(1-7). NEP: Neural endopeptidase; ACE: Angiotensin converting enzyme; ACE2: Angiotensin converting enzyme 2; AT1 receptor: Angiotensin II type 1 receptor.
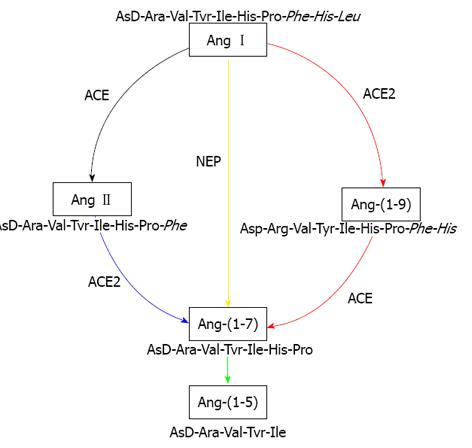
Figure 2 Intrahepatic enzymatic pathways of renin angiotensin system peptide production.
Schematic representation of the pathways responsible for the generation of vasodilator peptide angiotensin-(1-7) [Ang-(1-7)] in rat liver. The colour of the arrows represents the relative contribution of each pathway for ex vivo formation of Ang-(1-7) from the substrates angiotensin I (Ang I) and angiotensin II (Ang II) in cirrhotic rat liver. The most efficient pathway is represented by blue line, followed by green line. The black line is the least efficient pathway whilst red represents the efficiency less than green but higher than black. The yellow colour represents an efficient pathway to generate Ang-(1-7) directly from Ang I by the action of neutral endopeptidase (NEP) but it appears that this pathway is masked by angiotensin converting enzyme 2 in cirrhotic rat liver. Ang-(1-9): Angiotensin-(1-9); Ang-(1-5): Angiotensin-(1-5); ACE: Angiotensin converting enzyme; ACE2: Angiotensin converting enzyme 2; NEP: Neutral endopeptidase. Figure was adapted from our previous publication.
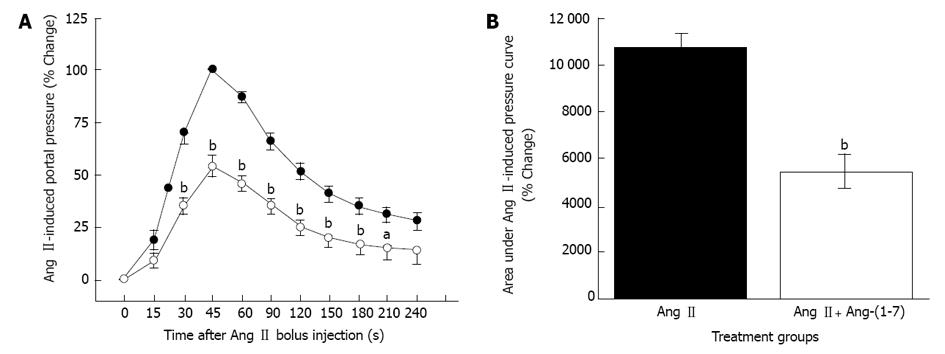
Figure 3 Angiotensin-(1-7)-induced portal pressure reduction.
Portal pressure changes in response to angiotensin II (Ang II) in cirrhotic rat liver. Portal pressure responses were measured using a vertically positioned graduated fluid-filled column open to atmospheric pressure. Ang II bolus (60 pmole) was injected into the portal vein of in-situ perfused cirrhotic rat liver preparations in the presence of an angiotensin converting enzyme (ACE) inhibitor lisinopril (0.7 μmol/L). A: Percentage increases in pressure in response to Ang II bolus in the absence (closed circles) or presence (open circles) of angiotensin-(1-7) [Ang-(1-7), 0.7 μmol/L]. The highest pressure that was recorded 45 s after the Ang II bolus injection was designated as 100% response and all other responses were calculated relative to this maximal reponse. B: The total area under Ang II response curve (AUC) in the absence (filled bar) or presence (open bar) of Ang-(1-7). Portal pressure change at each time point in panel A and AUC in B represents the mean ± SEM from 21 cirrhotic rat liver preparations. Pre-incubation with Ang-(1-7) significantly reduced the portal pressure response evoked by Ang II bolus injection. aP < 0.05, bP < 0.01 vs those with Ang II alone.
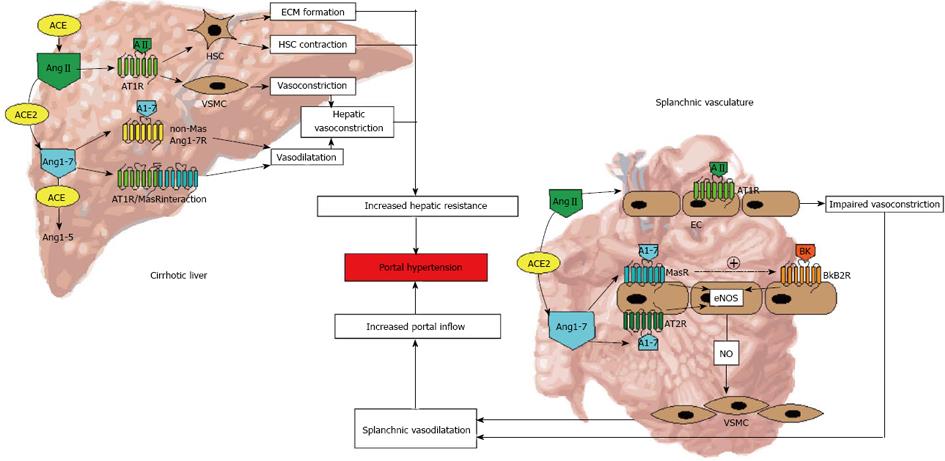
Figure 4 Overview of the renin angiotensin system-mediated pathophysiological changes in portal hypertension.
In cirrhosis, the effects of classical axis of the renin angiotensin system (RAS), mediated by its potent vasoconstrictor peptide angiotensin II (Ang II), are predominant within the hepatic vasculature, resulting in increased hepatic resistance to portal inflow. In this, apart from fixed barrier due to increased deposition of extracellular matrix (ECM) proteins, vascular tone is exacerbated by Ang II action on myofibroblastic cells (activated hepatic stellate cells-HSCs) and vascular smooth muscle cells (VSMCs). In contrast, the effects of the alternate axis of the RAS, mediated by its vasodilator peptide angiotensin-(1-7) (Ang1-7), are predominant within the splanchnic vasculature, resulting in increased nitric oxide (NO) production by vascular endothelial cells (ECs). This consequently exacerbates portal hypertension as a result of increased inflow to the portal circulation. Ang1-5: Angiotensin-(1-5); ACE: Angiotensin converting enzyme; ACE2: Angiotensin converting enzyme 2; eNOS: Endothelial nitric oxide synthase; Bk: Bradykinin; BkB2R: Bradykinin B2 receptor; AT1R: Angiotensin II type 1 receptor; AT2R: Angiotensin II type 2 receptor; MasR: Mas receptor.
- Citation: Herath CB, Grace JA, Angus PW. Therapeutic potential of targeting the renin angiotensin system in portal hypertension. World J Gastrointest Pathophysiol 2013; 4(1): 1-11
- URL: https://www.wjgnet.com/2150-5330/full/v4/i1/1.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v4.i1.1